Well-Being in Family Caregivers of Dementia Patients in Romania
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Instruments
2.2. Participants and Data Collection
2.3. Statistical Analysis
2.4. Classification of Well-Being Status
3. Results
Descriptive Statistics
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Disability Language/Terminology Positionality Statement
Abbreviations
| BCa | Bias-Corrected and Accelerated Bootstrap Confidence Interval |
| C.F.2 | Railway Clinical Hospital No. 2, managed by the Ministry of Transport of Romania |
| Ryff’s Scale | Scale for Assessing Well-Being |
| WHO | World Health Organization |
References
- Nichols, E.; Szoeke, C.E.I.; Vollset, S.E.; Abbasi, N.; Abd-Allah, F.; Abdela, J.; Aichour, M.T.E.; Akinyemi, R.O.; Alahdab, F.; Asgedom, S.W.; et al. Global, Regional, and National Burden of Alzheimer’s Disease and Other Dementias, 1990–2016: A Systematic Analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 88–106. [Google Scholar] [CrossRef] [PubMed]
- Nichols, E.; Steinmetz, J.D.; Vollset, S.E.; Fukutaki, K.; Chalek, J.; Abd-Allah, F.; Abdoli, A.; Abualhasan, A.; Abu-Gharbieh, E.; Akram, T.T.; et al. Estimation of the Global Prevalence of Dementia in 2019 and Forecasted Prevalence in 2050: An Analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125. [Google Scholar] [CrossRef] [PubMed]
- Schulz, R.; Sherwood, P.R. Physical and Mental Health Effects of Family Caregiving. Am. J. Nurs. 2008, 108, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Chiao, C.-Y.; Wu, H.-S.; Hsiao, C.-Y. Caregiver Burden for Informal Caregivers of Patients with Dementia: A Systematic Review. Int. Nurs. Rev. 2015, 62, 340–350. [Google Scholar] [CrossRef]
- European Commission; Directorate General for Employment, Social Affairs and Inclusion; London School of Economics and Political Science (LSE). Informal Care in Europe: Exploring Formalisation, Availability and Quality; Publications Office: Luxembourg, 2018. [Google Scholar]
- Fonareva, I.; Oken, B.S. Physiological and Functional Consequences of Caregiving for Relatives with Dementia. Int. Psychogeriatr. 2014, 26, 725–747. [Google Scholar] [CrossRef]
- Brodaty, H.; Donkin, M. Family Caregivers of People with Dementia. Dialogues Clin. Neurosci. 2009, 11, 217–228. [Google Scholar] [CrossRef]
- Bressan, V.; Visintini, C.; Palese, A. What Do Family Caregivers of People with Dementia Need? A Mixed-method Systematic Review. Health Soc. Care Community 2020, 28, 1942–1960. [Google Scholar] [CrossRef] [PubMed]
- Gallagher-Thompson, D.; Choryan Bilbrey, A.; Apesoa-Varano, E.C.; Ghatak, R.; Kim, K.K.; Cothran, F. Conceptual Framework to Guide Intervention Research Across the Trajectory of Dementia Caregiving. Gerontologist 2020, 60, S29–S40. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Zhang, F. A Comprehensive Meta-Review of Systematic Reviews and Meta-Analyses on Nonpharmacological Interventions for Informal Dementia Caregivers. BMC Geriatr. 2020, 20, 137. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Au, A.; Losada, A.; Thompson, L.W.; Gallagher-Thompson, D. Psychological Interventions for Dementia Caregivers: What We Have Achieved, What We Have Learned. Curr. Psychiatry Rep. 2019, 21, 59. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness Is Everything, or Is It? Explorations on the Meaning of Psychological Well-Being. J. Personal. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Ryff, C.D.; Keyes, C.L.M. The Structure of Psychological Well-Being Revisited. J. Personal. Soc. Psychol. 1995, 69, 719–727. [Google Scholar] [CrossRef]
- Ryff, C.D. Psychological Well-Being Revisited: Advances in the Science and Practice of Eudaimonia. Psychother. Psychosom. 2014, 83, 10–28. [Google Scholar] [CrossRef]
- Abbott, R.A.; Ploubidis, G.B.; Huppert, F.A.; Kuh, D.; Wadsworth, M.E.; Croudace, T.J. Psychometric Evaluation and Predictive Validity of Ryff’s Psychological Well-Being Items in a UK Birth Cohort Sample of Women. Health Qual. Life Outcomes 2006, 4, 76. [Google Scholar] [CrossRef] [PubMed]
- Van Dierendonck, D.; Lam, H. Interventions to Enhance Eudaemonic Psychological Well-being: A Meta-analytic Review with Ryff’s Scales of Psychological Well-being. Appl. Psych. Health Well 2023, 15, 594–610. [Google Scholar] [CrossRef]
- Lindfors, P. Positive health in a group of swedish white-collar workers. Psychol. Rep. 2002, 91, 839. [Google Scholar] [CrossRef] [PubMed]
- Huppert, F.A. Challenges in Defining and Measuring Well-Being and Their Implications for Policy. In Future Directions in Well-Being; White, M.A., Slemp, G.R., Murray, A.S., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 163–167. ISBN 978-3-319-56888-1. [Google Scholar]
- Ryff, C.D.; Singer, B. Psychological Weil-Being: Meaning, Measurement, and Implications for Psychotherapy Research. Psychother. Psychosom. 1996, 65, 14–23. [Google Scholar] [CrossRef]
- Van Dierendonck, D. The Construct Validity of Ryff’s Scales of Psychological Well-Being and Its Extension with Spiritual Well-Being. Personal. Individ. Differ. 2004, 36, 629–643. [Google Scholar] [CrossRef]
- Pinquart, M.; Sorensen, S. Correlates of Physical Health of Informal Caregivers: A Meta-Analysis. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2007, 62, P126–P137. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Differences between Caregivers and Noncaregivers in Psychological Health and Physical Health: A Meta-Analysis. Psychol. Aging 2003, 18, 250–267. [Google Scholar] [CrossRef]
- Gallagher, M.W.; Lopez, S.J.; Preacher, K.J. The Hierarchical Structure of Well-Being. J. Personal. 2009, 77, 1025–1050. [Google Scholar] [CrossRef]
- Chang, S.O.; Kim, E.Y. Rediscovering One’s Identity: A Qualitative Meta-Synthesis Study on the Resilience Experiences of Family Caregivers of Patients with Dementia. Available online: https://www.researchsquare.com/article/rs-1260102/v1 (accessed on 10 February 2022).
- Cheng, C.; Lau, H.-P.B.; Chan, M.-P.S. Coping Flexibility and Psychological Adjustment to Stressful Life Changes: A Meta-Analytic Review. Psychol. Bull. 2014, 140, 1582–1607. [Google Scholar] [CrossRef]
- Alexandrova, A. Well-Being as an Object of Science. Philos. Sci. 2012, 79, 678–689. [Google Scholar] [CrossRef]
- Alexandrova, A. A Philosophy for the Science of Well-Being; Oxford University Press: Oxford, UK, 2017; Volume 1, ISBN 978-0-19-930051-8. [Google Scholar]
- Ryan, R.M.; Deci, E.L. On Happiness and Human Potentials: A Review of Research on Hedonic and Eudaimonic Well-Being. Annu. Rev. Psychol. 2001, 52, 141–166. [Google Scholar] [CrossRef]
- World Health Organization. Dementia: A Public Health Priority; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 18 September 2025).
- World Health Organization. Country Case Study on the Integrated Delivery of Long-Term Care: Romania. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2022-5261-45025-64131 (accessed on 18 September 2025).
- Alzheimer’s Association. 2022 Alzheimer’s Disease Facts and Figures; Alzheimer’s Association: Chicago, IL, USA, 2022. [Google Scholar]
- Wimo, A.; Guerchet, M.; Ali, G.; Wu, Y.; Prina, A.M.; Winblad, B.; Jönsson, L.; Liu, Z.; Prince, M. The Worldwide Costs of Dementia 2015 and Comparisons with 2010. Alzheimer’s Dement. 2017, 13, 1–7. [Google Scholar] [CrossRef]
- Philipp, J. Mental Health in Romania: Issues and Solutions. The Borgen Project 2023. Available online: https://borgenproject.org/mental-health-in-romania/ (accessed on 19 September 2025).
- Jönsson, L.; Tate, A.; Frisell, O.; Wimo, A. The Costs of Dementia in Europe: An Updated Review and Meta-Analysis. PharmacoEconomics 2023, 41, 59–75. [Google Scholar] [CrossRef] [PubMed]
- Onetiu, V.; Aurelian, S.M.; Capisizu, A.; Cristescu, F.; Zus, I.C.; Kissimova-Skarbek, K. Cost of Dementia in Romania: A Cross-Sectional Cost-of-Illness Study Undertaken in Bucharest. Zesz. Nauk. Ochr. Zdrowia 204 Zdr. Publiczne Zarządzanie 2016, 14, 204–226. [Google Scholar]
- National Institute of Statistics, Romania. Romanian Statistical Yearbook 2024; National Institute of Statistics: Washington, DC, USA, 2025. [Google Scholar]
- Reform of Long-Term Care Services for Older People—European Commission. Available online: https://commission.europa.eu/projects/reform-long-term-care-services-older-people_en (accessed on 18 September 2025).
- Costea-Bărluțiu, C.; Bălaș-Baconschi, C.; Hathazi, A. Romanian Adaptation of the Ryff’s Psychological Well-Being Scale: Brief Report of the Factor Structure and Psychometric Properties. J. Evid.-Based Psychot. 2018, 18, 21–34. [Google Scholar] [CrossRef]
- Bradburn, N. The Structure of Psychological Well-Being; Aldine Publishing Company: Chicago, IL, USA, 1969. [Google Scholar]
- Babnik, K.; Benko, E.; Von Humboldt, S. Ryff’s Psychological Well-Being Scale. In Encyclopedia of Gerontology and Population Aging; Gu, D., Dupre, M.E., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 4344–4349. ISBN 978-3-030-22008-2. [Google Scholar]
- Baltes, P.B.; Baltes, M.M. (Eds.) Successful Aging: Perspectives from the Behavioral Sciences, 1st ed.; Cambridge University Press: Cambridge, UK, 1990; ISBN 978-0-521-37454-5. [Google Scholar]
- Arnett, J.J. Emerging Adulthood: A Theory of Development from the Late Teens through the Twenties. Am. Psychol. 2000, 55, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, L. The Influence of Neuroscience on US Supreme Court Decisions about Adolescents’ Criminal Culpability. Nat. Rev. Neurosci. 2013, 14, 513–518. [Google Scholar] [CrossRef]
- Blakemore, S.-J.; Robbins, T.W. Decision-Making in the Adolescent Brain. Nat. Neurosci. 2012, 15, 1184–1191. [Google Scholar] [CrossRef]
- DiCiccio, T.J.; Efron, B. Bootstrap Confidence Intervals. Statist. Sci. 1996, 11, 189–228. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; SAGE Publications Ltd.: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- Altman, D.G.; Royston, P. The Cost of Dichotomising Continuous Variables. BMJ 2006, 332, 1080. [Google Scholar] [CrossRef]
- Agresti, A.; Finlay, B. Statistical Methods for the Social Sciences, 4th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2009; ISBN 978-0-13-713150-1. [Google Scholar]
- OECD. OECD Guidelines on Measuring Subjective Well-Being; OECD: Paris, France, 2013; ISBN 978-92-64-19164-8. [Google Scholar]
- Cumming, G. The New Statistics: Why and How. Psychol. Sci. 2014, 25, 7–29. [Google Scholar] [CrossRef]
- Greenland, S.; Senn, S.J.; Rothman, K.J.; Carlin, J.B.; Poole, C.; Goodman, S.N.; Altman, D.G. Statistical Tests, P Values, Confidence Intervals, and Power: A Guide to Misinterpretations. Eur. J. Epidemiol. 2016, 31, 337–350. [Google Scholar] [CrossRef]
- Tatomirescu, L.F.; Glavce, C.S.; Prada, G.I.; Borosanu, A.; Turcu, S. Socio-Demographic Factors Linked to Psychological Well-Being in Dementia Caregivers. Healthcare 2025, 13, 2235. [Google Scholar] [CrossRef] [PubMed]
- Tatomirescu, L.F.; Prada, G.-I.; Glavce, C.S.; David-Rus, R.; Borosanu, A. Well-Being Profiles of Family Caregivers of Patients with Dementia from Romania: A Latent Profile Analysis. Cureus 2025, 17, e83103. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.K.; Adluru, N.; Finley, A.J.; Gresham, L.K.; Skinner, S.E.; Alexander, A.L.; Davidson, R.J.; Ryff, C.D.; Schaefer, S.M. Purpose in Life as a Resilience Factor for Brain Health: Diffusion MRI Findings from the Midlife in the U.S. Study. Front. Psychiatry 2024, 15, 1355998. [Google Scholar] [CrossRef]
- Ryff, C.D.; Singer, B.H. Know Thyself and Become What You Are: A Eudaimonic Approach to Psychological Well-Being. J. Happiness Stud. 2008, 9, 13–39. [Google Scholar] [CrossRef]
- Ryff, C.D. A New Direction in Mental Health: Purposeful Life Engagement. In Encyclopedia of Mental Health; Elsevier: Amsterdam, The Netherlands, 2023; pp. 629–637. ISBN 978-0-323-91498-7. [Google Scholar]
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the Stress Process: An Overview of Concepts and Their Measures. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef]
- Hammell, K.W. Opportunities for Well-Being: The Right to Occupational Engagement. Can. J. Occup. Ther. 2017, 84, 209–222. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Association. 2023 Alzheimer’s Disease Facts and Figures. Alzheimers Dement. 2023, 19, 1598–1695. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%) |
|---|---|
| Gender of dementia patient | |
| Male | 21 (30.0%) |
| Female | 49 (70.0%) |
| Gender of Contact Caregiver | |
| Male | 18 (25.7%) |
| Female | 52 (74.3%) |
| Occupational Status of Contact Caregiver | |
| Employed | 52 (74.3%) |
| Retired | 18 (25.7%) |
| Place of Residence of Contact Caregiver | |
| Rural | 23 (32.9%) |
| Urban | 47 (67.1%) |
| Caregiving Structure | |
| Family-based caregiving | 45 (64.3%) |
| Assisted by a female caregiver | 22 (31.4%) |
| Single caregiver | 3 (4.3%) |
| Education Level of Contact Caregiver | |
| Secondary education | 5 (7.1%) |
| High school education | 38 (54.3%) |
| Higher education | 27 (38.6%) |
| Declared Household Income/per month | |
| Up to 400 EUR | 14 (20%) |
| 400 ≤ income < 1000 EUR | 45 (64.3%) |
| Equal to or above 1000 EUR | 11 (15.7%) |
| state-provided financial support | |
| Received | 70 (100.0%) |
| Dimension | Mean | SD | Skewness | Kurtosis | Shapiro–Wilk |
|---|---|---|---|---|---|
| Self-Acceptance | 37.67 | 7.97 | 0.29 | −0.78 | 0.98 (p = 0.22) |
| Positive Relations | 37.41 | 7.57 | −0.17 | −0.08 | 0.99 (p = 0.96) |
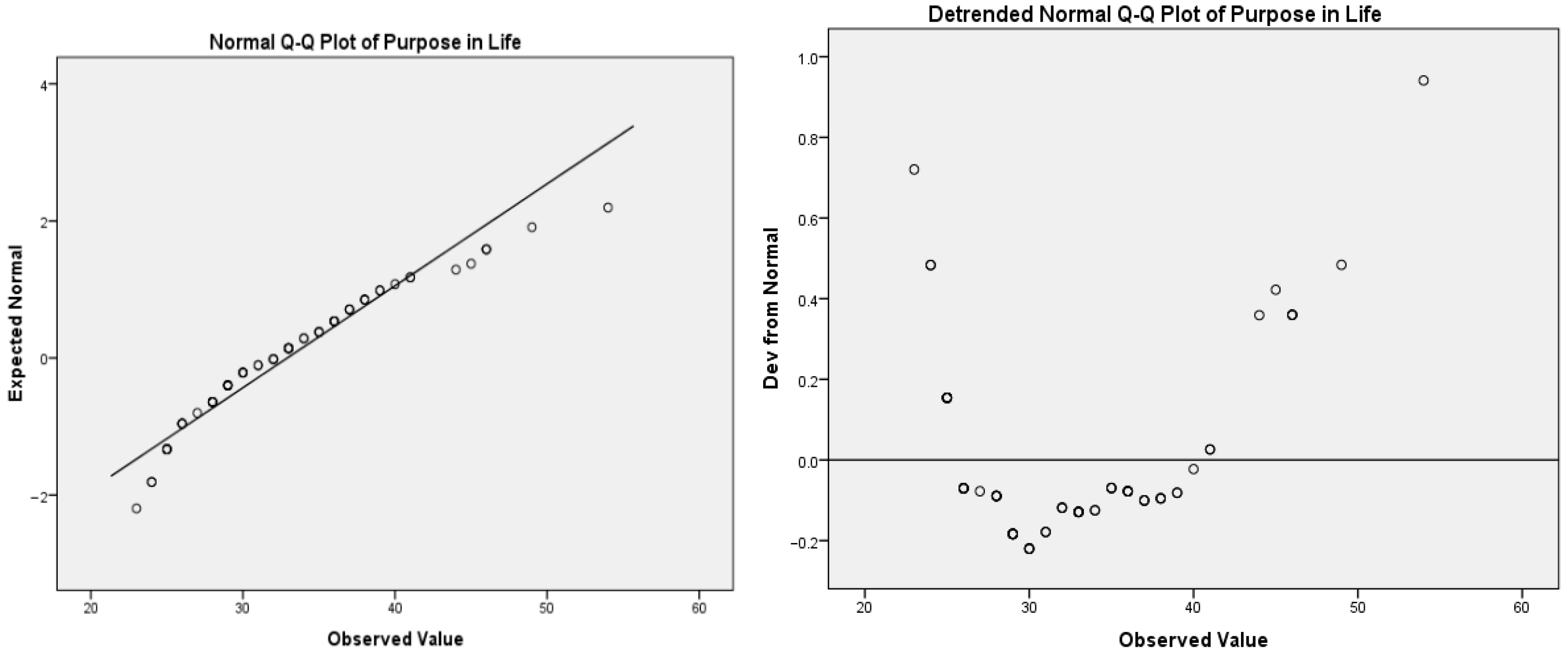
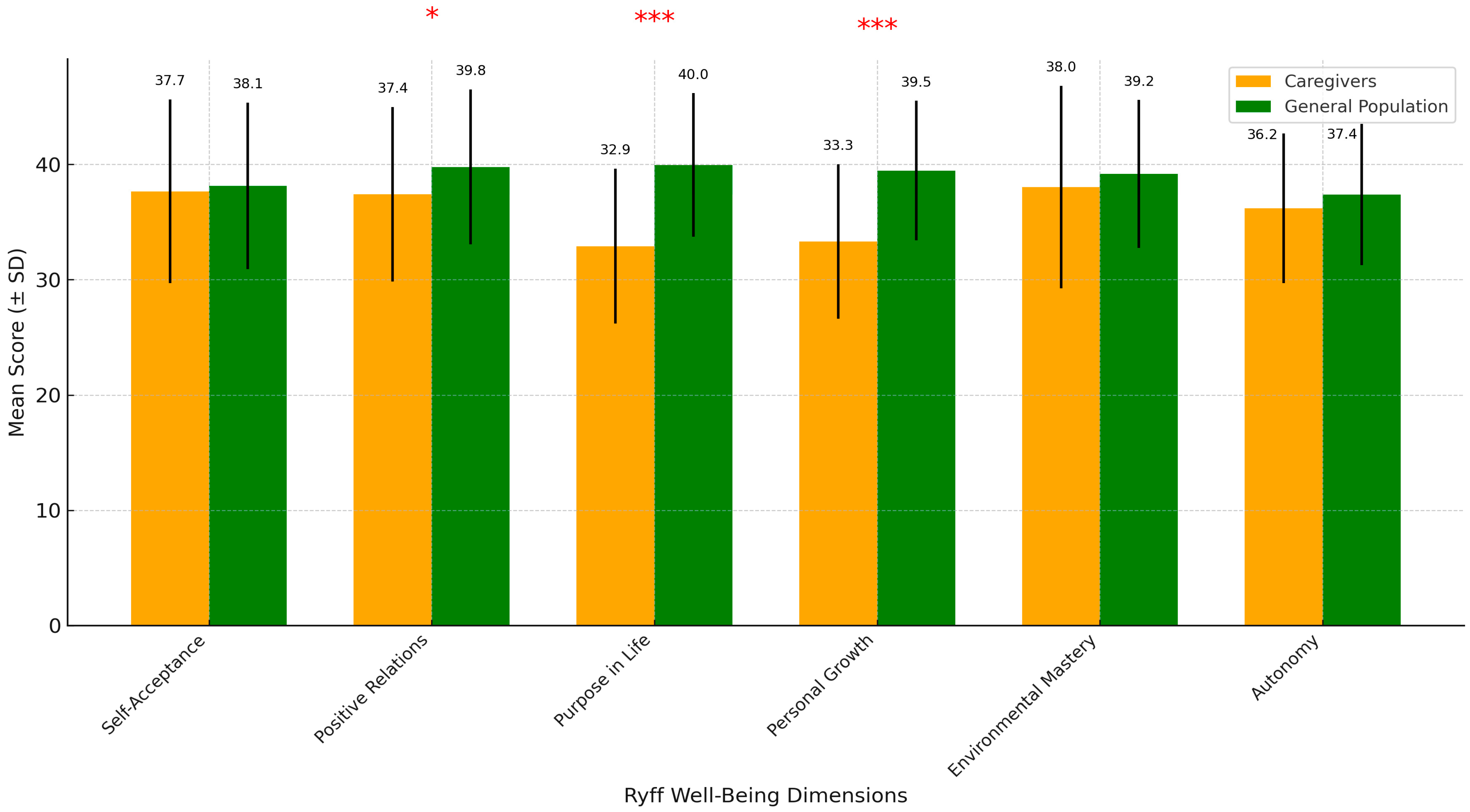
| Purpose in Life | 32.91 | 6.72 | 0.86 | 0.50 | 0.98 (p = 0.01) |
| Personal Growth | 33.31 | 6.71 | 0.13 | 1.02 | 0.97 (p = 0.12) |
| Environmental Mastery | 38.03 | 8.78 | −0.32 | −0.14 | 0.98 (p = 0.45) |
| Autonomy | 36.21 | 6.49 | 0.48 | −0.33 | 0.97 (p = 0.09) |
| Dimension | Dementia Family Caregivers’ Sample | Reference Population | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Minimum | Maximum | Mean | SD | Minimum | Maximum | |
| Self-Acceptance | 37.67 | 7.97 | 21 | 54 | 38.14 | 7.21 | 14 | 54 |
| Positive Relations | 37.41 | 7.57 | 16 | 54 | 39.78 | 6.72 | 19 | 53 |
| Purpose in Life | 32.91 | 6.72 | 23 | 54 | 39.96 | 6.22 | 23 | 54 |
| Personal Growth | 33.31 | 6.71 | 13 | 54 | 39.47 | 6.05 | 24 | 54 |
| Environmental Mastery | 38.03 | 8.78 | 13 | 54 | 39.17 | 6.42 | 16 | 53 |
| Autonomy | 36.21 | 6.49 | 23 | 52 | 37.39 | 6.14 | 20 | 53 |
| Dimension | Self- Acceptance | Positive Relations | Purpose in Life | Environmental Mastery | Personal Growth | Autonomy |
|---|---|---|---|---|---|---|
| Self-Acceptance | 1 | |||||
| Positive Relations | 0.74 ** | 1 | ||||
| Purpose in Life | 0.66 ** | 0.64 ** | 1 | |||
| Environmental Mastery | 0.83 ** | 0.83 ** | 0.69 ** | 1 | ||
| Personal Growth | 0.67 ** | 0.79 ** | 0.61 ** | 0.73 ** | 1 | |
| Autonomy | 0.62 ** | 0.55 ** | 0.51 ** | 0.55 ** | 0.52 ** | 1 |
| Variable | Sample Mean | Reference Mean | Mean Difference | t-Value | Df | p-Value | 95% BCa Bootstrap CI | |
|---|---|---|---|---|---|---|---|---|
| Self-Acceptance | 37.67 | 38.14 | −0.47 | −0.49 | 69 | 0.62 | −2.37 | 1.43 |
| Positive Relations | 37.41 | 39.78 | −2.37 | −2.62 | 69 | 0.01 | −4.17 | −0.56 |
| Purpose in Life | 32.91 | 39.96 | −6.82 | −8.77 | 69 | <0.001 | −8.65 | −5.44 |
| Personal Growth | 33.31 | 39.47 | −6.05 | −7.68 | 69 | <0.001 | −7.75 | −4.56 |
| Environmental Mastery | 38.03 | 39.17 | −1.14 | −1.09 | 69 | 0.26 | −3.24 | 0.95 |
| Autonomy | 36.21 | 37.39 | −1.18 | −1.52 | 69 | 0.13 | −2.72 | 0.37 |
| Sociodemographic and Contextual Variable | Pearson’s χ2 (df) | Pearson’s p-Value | Fisher’s Exact p-Value | Interpretation |
|---|---|---|---|---|
| Gender of Contact Caregiver | — | — | 0.54 | Not significant |
| Gender of patient | — | — | 0.63 | Not significant |
| Occupational Status of Contact Caregiver | 4.04 (1) | 0.04 | 0.05 | Significant/Marginal |
| Education Level of Contact Caregiver | — | — | 0.28 | Not significant |
| Place of Residence of Contact Caregiver | — | — | 0.28 | Not significant |
| Caregiving Structure | — | — | 0.23 | Not significant |
| Declared Household Income | — | — | 0.14 | Marginally significant |
| Patient sleeps in separate room | — | — | 0.15 | Marginally significant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tatomirescu, L.F.; Glavce, C.S.; Prada, G.-I.; Turcu, S.; Borosanu, A. Well-Being in Family Caregivers of Dementia Patients in Romania. Disabilities 2025, 5, 90. https://doi.org/10.3390/disabilities5040090
Tatomirescu LF, Glavce CS, Prada G-I, Turcu S, Borosanu A. Well-Being in Family Caregivers of Dementia Patients in Romania. Disabilities. 2025; 5(4):90. https://doi.org/10.3390/disabilities5040090
Chicago/Turabian StyleTatomirescu, Liviu Florian, Cristiana Susana Glavce, Gabriel-Ioan Prada, Suzana Turcu, and Adriana Borosanu. 2025. "Well-Being in Family Caregivers of Dementia Patients in Romania" Disabilities 5, no. 4: 90. https://doi.org/10.3390/disabilities5040090
APA StyleTatomirescu, L. F., Glavce, C. S., Prada, G.-I., Turcu, S., & Borosanu, A. (2025). Well-Being in Family Caregivers of Dementia Patients in Romania. Disabilities, 5(4), 90. https://doi.org/10.3390/disabilities5040090







