1. Introduction
Over the past two decades, spinal cord injury, both traumatic and non-traumatic, has seen a progressive increase in incidence [
1]. The likelihood of mobility recovery from spinal cord injury with complete lesion above thoracic level ten is low [
2]. Individuals with spinal cord injury with complete lesions have poor motor recovery prognosis after 9 months of injury [
3]. Kirshblum et al. [
3] suggested that recovery during the acute and post-acute period of spinal cord injury is likely due to edema reduction or diaschisis. Spinal cord injury poses a significant burden globally, which is even higher for those with complete lesion in the cervical spine levels [
4]. Whilst wheelchair advancement has promoted the quality of life among individuals with spinal cord injuries, the use of exoskeleton may further enhance their quality of life in partly adapted environments. To complement technological advancement, biomedical research in cellular regrowth provides a promising treatment for spinal cord injury [
5], but the approach is still in early stage of research and thus not readily available for clinical implementation. Recently, spinal cord stimulation using an implant followed by seven months of physical rehabilitation showed improvements in motor function for three individuals with complete lesions in their thoracic spinal cords, but not sensory function [
6]. However, not all individuals with spinal cord injury are suitable for the surgical implant procedure.
In the absence of recent novel interventions in managing individuals with spinal cord injury, the recommended management remains conservative. The recent literature has identified three useful conservative interventions for functional improvements among individuals with spinal cord injury, which are transcranial magnetic stimulation, functional electrical stimulation, and robotic-assisted treadmill training [
7]. That said, Duan et al. [
7] found the use of transcranial magnetic stimulation promising only for incomplete spinal cord lesion. This is because the mechanism acts through the corticospinal tract [
8,
9]. Thus, in complete spinal cord lesion, the only stimulation mechanism possible is through the reflex arc [
10]. Whilst the use of functional electrical stimulation is similarly useful in managing individuals with incomplete spinal cord lesions as compared to those with complete spinal cord lesions, knowledge, cost, and time were barriers perceived by healthcare professionals in its adoption for clinical practice [
11]. In the last recommendation, which is robotic-assisted treadmill training, the use of exoskeleton is increasingly popular not just out of novelty, but because of the potential to activate the central pattern generator [
7]. However, evidence in the recovery of walking ability using supportive technology is limited. Overall, there is a lack of consensus on which rehabilitation intervention will be more effective [
12], especially for those with complete spinal cord lesions.
Considering the challenges in the management of individuals with spinal cord injury, particularly those with complete lesions, this study presents a rehabilitation approach using traditional and robotic exoskeletons for physical rehabilitation. This case study is aimed at demonstrating the possibility of evoking sensorimotor changes despite a loss in corticospinal tract connectivity in complete spinal cord lesion. The rehabilitation strategy presented could then be considered by other clinicians.
2. Materials and Methods
In view of the scarcity and difficulty in recruiting spinal cord injury participants, a case study approach is used. This case study is presented in accordance with the Case Report (CARE) guidelines. The case has been sufficiently masked to maintain anonymity and written informed consent is obtained from the patient.
2.1. Case Demographics and Clinical History
The patient is 48 years old, female, and Asian, who was involved in a road traffic accident 10 years ago, resulting in spinal cord injury—complete lesion. She has no medical conditions prior to the spinal cord injury and has been a homemaker. She was an active triathlete who participated in races annually. Her radiological report from the accident and emergency department showed multiple fractures at the posterior aspects of thoracic spine levels six and seven, and stable hyaline fractures at spinous processes of lower cervical spine level seven. In addition to the spinal fractures, she was diagnosed with right pneumothorax and bilateral hemothorax. Subsequently, she underwent spinal decompression surgery and interbody fusion to stabilize thoracic spine levels six and seven. There was no post-surgical complication reported. Prior to leaving the hospital for home, she was categorized as low rehabilitation potential, so she was counseled to adapt with her available physical ability after six months of outpatient rehabilitation. Her function above thoracic spine level six is preserved, which means her bladder and bowel control are impaired. She was also reviewed by the psychiatrist for emotional wellbeing back then and considered to be well, likely associated with her acceptance of her present physical condition and social support from family.
2.2. Therapeutic Interventions
Hospital B rehabilitation did not include her in robotics therapy as she was deemed to be of poor rehabilitation outcome in the past year. Hence, the patient decided to give private rehabilitation robotics therapy a trial in March 2025, 10 years after her spinal cord injury. On initial assessment, based on the American Spinal Injury Association (ASIA) impairment classification, the patient is classified as ‘A’, complete spinal cord lesion below thoracic level six. Although she understands that the prognosis is poor, she hopes that robotics training and physical rehabilitation will provide stimulation to her lower limb muscles. She attends a two-hour rehabilitation session, once a week. The first hour involves physical therapy with core strengthening exercises and fitness exercises assisted using the traditional exoskeleton—standing Thoracic-Hip-Knee-Ankle-Foot Orthosis (THKAFO).
In her initial sessions, the patient was guided in quadruped position to transit into kneeling as a form of core training. Apart from donning the THKAFO to walk with a forearm rollator frame, her rehabilitation exercises incorporated the element of fun with the aims of muscle strengthening and flexibility, aerobics training, and movement coordination. These exercises included overhead ball lift and throw, battle rope, stepping, trampoline jump, boxing, and lunges (
Table 1). The patient maintains perceived exertion within four to six points on the Borg’s ten-point rate of perceived exertion scale [
13]. Each session ends with ambulation on the advanced exoskeleton for about 45 min. To ensure her safety during the exercises, all exercise movements were performed within her available joint range of motion.
2.3. Thematic Synthesis
The patient was interviewed with four open-ended questions, (1) “How is life after the incident?” (2) “What are your goals back in 2015 versus now [2025], ie. past versus present?” (3) How did you find out about exoskeleton rehabilitation in Singapore?” (4) “What are your future plans?” We employed a few common strategies to mitigate potential bias in data extraction and interpretation. The interview was recorded by author R.X.L.C. Two authors (J.L.O and B.C.K.) independently extracted and coded qualitative data, with discrepancies resolved through discussion to achieve consensus. Reflexive discussions were used to minimize subjective bias in theme development. The authors (J.L.O and B.C.K.) maintained reflexive notes to acknowledge their preconceptions and minimize interpretive bias. We triangulated interpretations with author interpretations (J.L.O. and B.C.K.), participant quotes (patient), and provider observations (R.X.L.C.) to ensure consistency.
3. Results
The patient expressed satisfaction with her rehabilitation program because she reported muscle pulls in the calf muscle during lunges exercise and cramps in the quadriceps and hamstrings during and after trampoline, lunges, and walking exercises. She has not had such feelings or sensations prior to the current rehabilitation program. Commonly, these new symptoms could be due to a stretch fracture evoked by the intensive training. In this case, her new symptoms were not adverse and improved with rest. She has been reviewed in Hospital B in September 2025 for consideration as a clinical trial participant for stem cell transplant, and in her medical review, there were neither osteoporotic fractures nor other injuries detected. In terms of functioning, her functional independence measure score on admission was high, so rehabilitation outcome is expected to be limited by ceiling effect (
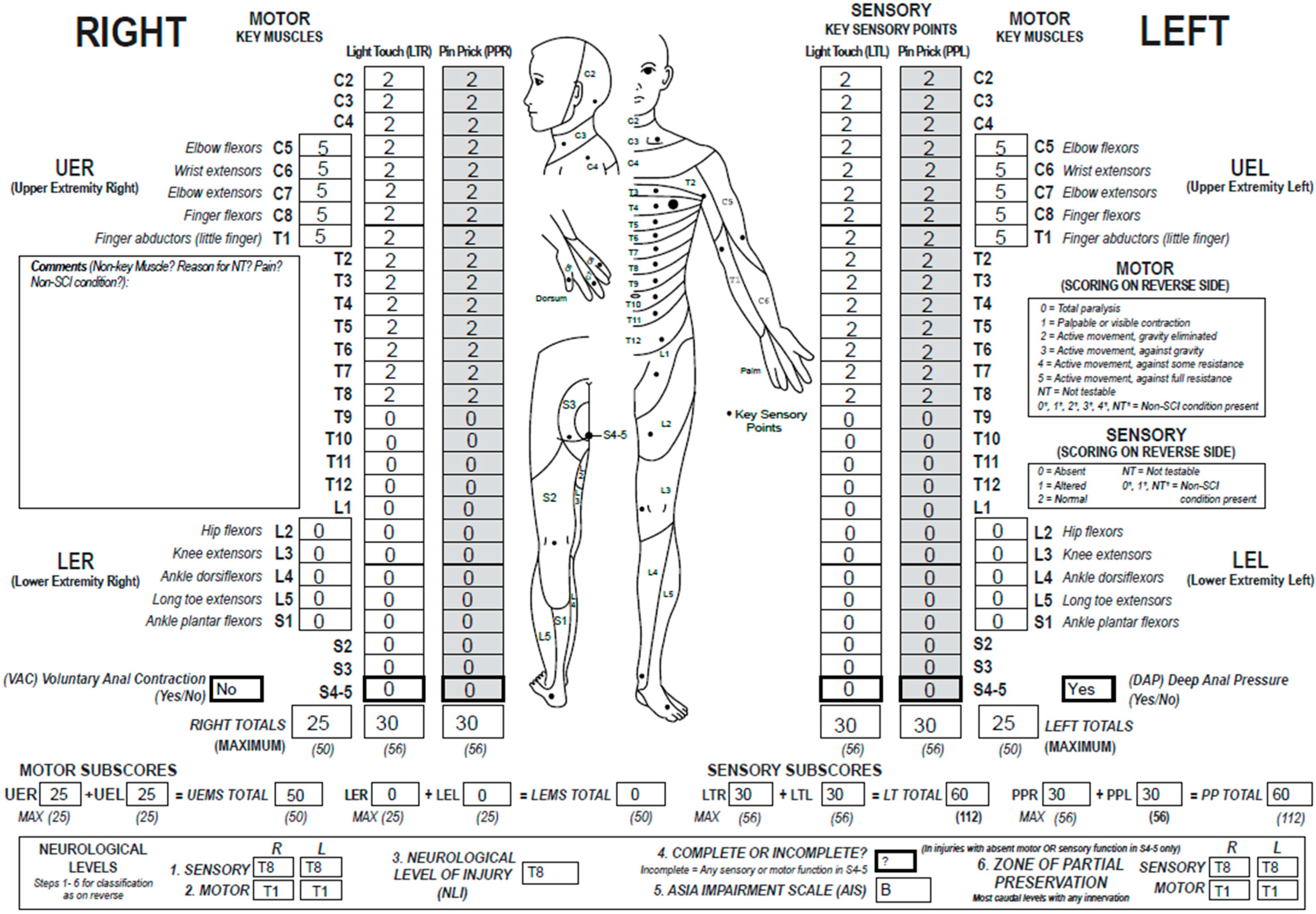
Table 2). As compared to baseline ASIA score and classification (
Figure A1), the 6th month follow-up assessment showed improvements in sensory from thoracic spinal cord levels six to eight, and she reported feeling deep anal pressure that was previously absent (
Figure A2).
3.1. Patient Perspectives
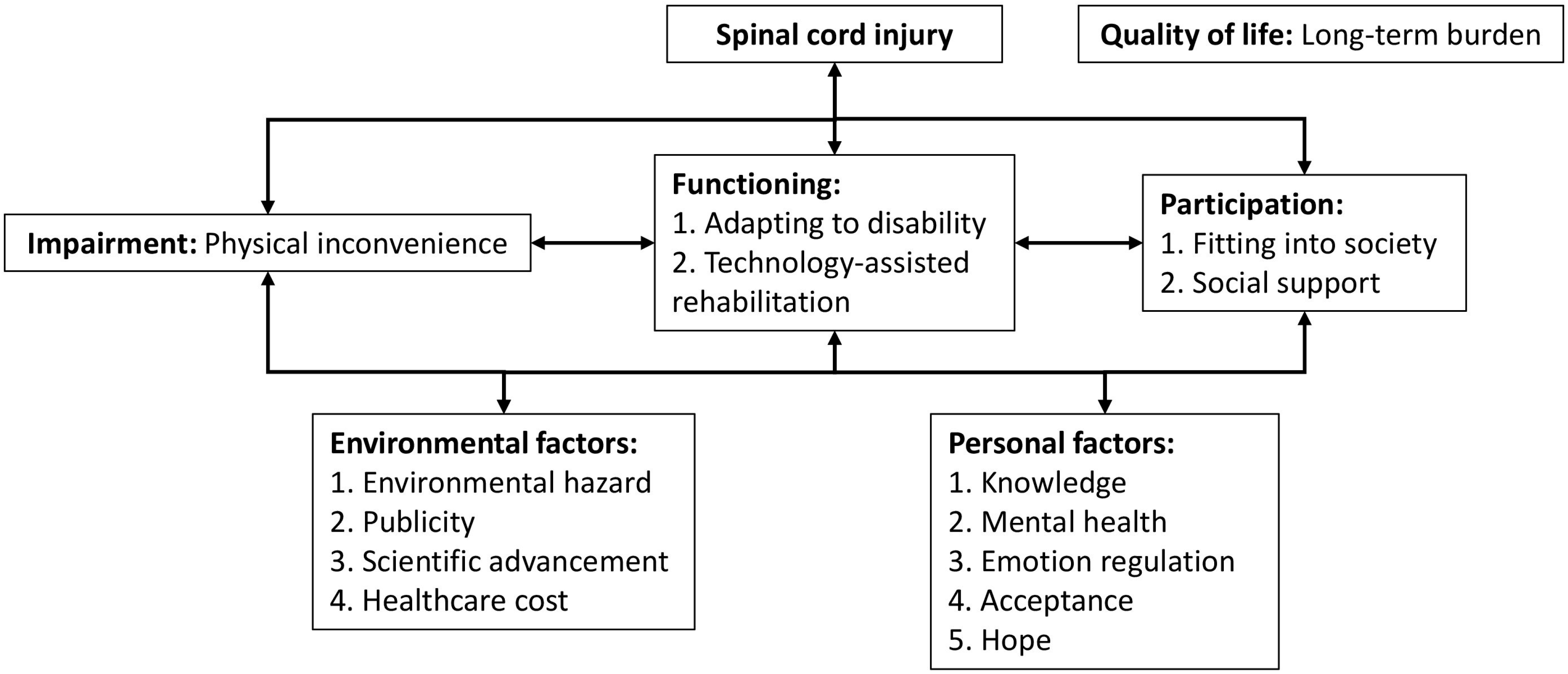
The themes synthesized from the patient’s perspective were mapped onto the International Classification of Functioning and Disability framework of the World Health Organization for ease of interpretation (
Figure 1).
3.1.1. Life After the Incident
Patient started the interview with, “[There are] a lot of inconveniences especially when the environment is [designed] for people without disability. So even [when] my home was renovated for my convenience, it can never fully cater to my personal needs because there are other able people living in the same environment. Examples of physical inconveniences are like toilet flushing system, how things are kept in the storeroom/cupboards, and the method to cook in the kitchen. Therefore, much effort and time is required for even a small gesture.” In this segment, the themes ‘physical inconvenience’ and ‘adapting to disability’ were thematically synthesized.
Followed by, “Another aspect of inconveniences is the loss of skin sensation, which accidents can happen [frequently]. Examples are shower water too hot for the skin, thighs got scalded by hot objects leading to pressure sores and broken skin due to impaired sensation after the incident.” The emerging theme in this segment of interview is ‘environmental hazard’.
In continuation, “Apart from the physical inconveniences, I find both mental and emotional health are a big change in me. I put these two domains together because I find that both aspects are closely related. My perspective of mental is about spinal cord injury knowledge, previously challenging, but easy these days to attain certain knowledge about spinal cord injury. However, how to translate that knowledge to help people like us still live a life meaningfully and purposefully can be quite challenging. Because we have many things to juggle and limited by our physical abilities, we often must spend more time nurturing our emotions and make mental adjustments to our expectations. This can be seen as non-productive because it lacks quantifiable element. For example, our standard measure of productivity is based on the house we live in and the amount of money we earn. Having said this, I find myself fortunate because I don’t have to worry too much about livelihood because to start off with, I have been a homemaker before the accident. But I believe many out there have much to juggle. I mean for an able person to climb the ladder of success in a corporate world is already a huge challenge, what’s more for spinal cord injury persons. I am just contented to have food on the table and be with my loved ones. These have been quite overlooked before the accident.” The key themes synthesized in this segment of the interview are ‘knowledge’, ‘mental health’, ‘emotion regulation’, ‘fitting into society’ and ‘social support’.
And ending the first question with, “I tend to worry less these days compared to before the accident. Perhaps in my unconscious mind is that this is the worst I can get in life. What could be even worse than this? Then just live a day as it is, living in the present. Don’t look too far to the future and what’s the past is already past. There’s nothing I can do to change the past.” A single theme was synthesized from this segment—‘acceptance’.
3.1.2. Past Versus Present Goals
The patient shared, “I think not much difference because I have always wanted to stand and walk again. In fact, I feel even more hopeful now because of advanced technology.” The themes that emerged from this question are ‘hope’ and ‘technology-assisted rehabilitation’.
3.1.3. Awareness of Exoskeleton
In this question, she shared, “Initially from Hospital A and then from social media.” The single theme that emerged from this response is ‘publicity’.
3.1.4. Future
She concluded the interview with, “I am planning to go for the stem cell clinical trial in Hospital B. I will still be going for rehab as long as my financials allow me to do so.” The emerging themes are ‘scientific advancement’, ‘long-term burden’, and ‘healthcare cost’.
4. Discussion
This case study showed that even though corticospinal tract connectivity is lost in complete spinal cord lesion, it is still possible to evoke sensory changes through lower limb weightbearing exercises. However, motor changes were not found after six months of rehabilitation. Nonetheless, the interview with the patient showed that private rehabilitation settings that incorporate traditional and advanced exoskeletons have benefits beyond physical functioning for those with spinal cord injuries below thoracic spine level six.
Literature demonstrating some signs of recovery in spinal cord injury is scarce. It is evident that robot-assisted rehabilitation benefits individuals with incomplete spinal cord lesions [
14]. In our case study of complete spinal cord lesion, we offer a few possible reasons for the lower limb sensation felt by the patient. First, the symptoms could be triggered via spinal stretch reflex, an involuntary and overly active muscle contraction as observed in the muscle spasms during exercise. This altered reflex pathway occurs because the inhibitory signals from the brain to the spinal cord are lost in complete spinal cord lesion. Thus, there is a possibility for the patient to perceive a pulling sensation at the calf muscle during lunges exercise. Second, while the spinal cord lesion is diagnosed as complete, there could be a chance that some sensory fibers are spared, thus allowing some signals through the spinothalamic tract. Third, similar to amputees, the sensation felt could be a phantom sensation. However, this is unlikely as the patient reports of the calf pulling sensation only during the lunges exercise for the rear foot, which she did not expect to have any feelings. Her muscle cramps during rehabilitation were also exercise-specific. With regard to her regaining of deep anal pressure, it is an unusual phenomenon that warrants future investigation. Overall, superficial sensation is not significantly regained, and this case shows the possibility of regaining some sensation through physical rehabilitation.
The thematic synthesis mapped to the International Classification of Functioning and Disability framework of the World Health Organization provided an overview of the multi-disciplinary care needs of an individual with spinal cord injury. It is not surprising that physical inconvenience emerged as a theme because of the loss of motor function in spinal cord injury. In view that the motor impairments are difficult to reverse, a patient with spinal cord injury will need to adapt to available physical function. It is possible that advancement in technology can support physical rehabilitation and daily functioning. Advanced technology could support the patient in social activity participation. Social support plays an important role in supporting patients with spinal cord injuries [
15]. The environment of patients with spinal cord injuries matters a lot as their loss of thermal sensitivity could lead to burns. The environmental safety of spinal cord injuries might be an overlooked care issue based on our patient’s perspective.
Awareness of rehabilitation advancement, which relates to knowledge, is important in keeping updated with the possibility of recovery. Advancement in science keeps hope alive but can also be a barrier to physical rehabilitation or advanced care because of the rising healthcare cost. The acceptance of one’s health condition is vital in regulating emotion and maintaining mental health. Overall, these themes reflect the long-term burden of spinal cord injury on quality of life. The themes highlight the importance of an inclusive society by improving accessibility for patients with spinal cord injuries and considering long-term healthcare subsidies. The patient’s perspective thus provides information for clinicians and policymakers to consider in developing an inclusive society.
Whilst this case study provides the genuine experience of a patient, it is possible that other patients, younger or older adults, with complete spinal cord lesions may have different life experience and expectations. Hence, generalizing the intervention plan of this case study to other patients requires careful consideration. Patients with higher levels of spinal cord lesions such as at the cervical spine or higher thoracic spine levels would likely have more physical impairments, which include reduced upper limb functioning. The novelty of robotic-assisted therapy may provide hope to individuals with spinal cord injuries. This case study shows the importance of weightbearing exercises and making exercise sessions fun, especially when the exercises cannot be performed in the gymnasium by patients independently. Future research using case series or large cohort studies will be useful in confirming if such intensive training protocol yields similar results without adverse events.
5. Conclusions
In this case study, a patient with complete spinal cord lesion at thoracic spine level six showed deep sensory improvement with weightbearing exercises assisted with traditional and advanced exoskeletons. To achieve this progress, moderate exercise intensity and two hours of rehabilitation session are necessary. The use of robotic-assisted walking can reduce the physical strain on allied health professionals, as well as provide extended rehabilitation care in view of limited allied health professional manpower.
Author Contributions
Conceptualization, all authors; methodology, all authors; validation, B.C.K.; formal analysis, R.X.L.C., J.L.O. and B.C.K.; investigation, R.X.L.C., J.L.O. and B.C.K.; resources, R.X.L.C. and H.Y.; data curation, R.X.L.C., H.Y. and B.C.K.; writing—original draft preparation, R.X.L.C. and B.C.K.; writing—review and editing, J.L.O., H.Y. and B.C.K.; visualization, R.X.L.C. and B.C.K.; supervision, H.Y. and B.C.K.; project administration, R.X.L.C. and H.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the nature of the study, a case report that is sufficiently masked to maintain anonymity.
Informed Consent Statement
Written informed consent has been obtained from the patient and therapy staff to participate in the study and publish the paper.
Data Availability Statement
All data pertaining to the case study has been reported.
Conflicts of Interest
R.X.L.C. is an employee of Kang Jia Therapy, while H.Y. is the owner of Kang Jia Therapy. Clinical Pilates Family Physiotherapy is not an organization that serves the clients, and J.L.O. and B.C.K. are not paid for this piece of work. Hence, J.L.O. and B.C.K. serve as an independent party in this work. The authors declare no conflicts of interest.
Disability Language/Terminology Positionality Statement
The authorship team comprises health researchers and clinicians with continuous interests in collaboration with people with lived experience. Our case study adopts person-first language (e.g., “patient with spinal cord injury” and “patient with complete spinal cord lesion”), which reflects a commitment to inclusive and respectful communication. Person-first language emphasizes the individual before the condition, recognizing that their condition is only one aspect of a person’s identity, rather than a defining characteristic. In this manuscript, we adopt the patients’ perspective to define successful healthcare interventions for people with spinal cord injury. We acknowledge the voluntary contributions of the patient and express our respect for her diverse opinions, beliefs, and lived experiences.
Appendix A
Figure A1.
American Spinal Injury Association March 2025 Admission Scoring.
Figure A1.
American Spinal Injury Association March 2025 Admission Scoring.
Figure A2.
American Spinal Injury Association September 2025 Follow-Up Scoring.
Figure A2.
American Spinal Injury Association September 2025 Follow-Up Scoring.
References
- Lu, Y.; Shang, Z.; Zhang, W.; Pang, M.; Hu, X.; Dai, Y.; Shen, R.; Wu, Y.; Liu, C.; Luo, T. Global incidence and characteristics of spinal cord injury since 2000–2021: A systematic review and meta-analysis. BMC Med. 2024, 22, 285. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.A.; Leiby, B.E.; Marino, R.J. Neurological and functional recovery after thoracic spinal cord injury. J Spinal Cord Med. 2016, 39, 67–76. [Google Scholar] [CrossRef]
- Kirshblum, S.; Snider, B.; Eren, F.; Guest, J. Characterizing natural recovery after traumatic spinal cord injury. J. Neurotrauma 2021, 38, 1267–1284. [Google Scholar] [CrossRef]
- Ding, W.; Hu, S.; Wang, P.; Kang, H.; Peng, R.; Dong, Y.; Li, F. Spinal cord injury: The global incidence, prevalence, and disability from the global burden of disease study 2019. Spine 2022, 47, 1532–1540. [Google Scholar] [CrossRef] [PubMed]
- Zipser, C.M.; Cragg, J.J.; Guest, J.D.; Fehlings, M.G.; Jutzeler, C.R.; Anderson, A.J.; Curt, A. Cell-based and stem-cell-based treatments for spinal cord injury: Evidence from clinical trials. Lancet Neurol. 2022, 21, 659–670. [Google Scholar] [CrossRef] [PubMed]
- Wee, S.K.; Valerie, Z.Y.N.; Phua, M.W.; Lui, W.L.; Misbaah, F.; Ker, R.X.J.; Ng, W.H.; Rui Wan, K. Synergistic integration of epidural spinal cord stimulation with robotic therapy and neurorehabilitation to facilitate functional recovery in chronic sensorimotor complete spinal cord injury: A case series. Adv. Rehabil. Sci. Pract. 2025, 14, 27536351251343738. [Google Scholar] [CrossRef] [PubMed]
- Duan, R.; Qu, M.; Yuan, Y.; Lin, M.; Liu, T.; Huang, W.; Gao, J.; Zhang, M.; Yu, X. Clinical benefit of rehabilitation training in spinal cord injury: A systematic review and meta-analysis. Spine 2021, 46, E398–E410. [Google Scholar] [CrossRef] [PubMed]
- Cortes, M.; Medeiros, A.H.; Gandhi, A.; Lee, P.; Krebs, H.I.; Thickbroom, G.; Edwards, D. Improved grasp function with transcranial direct current stimulation in chronic spinal cord injury. Neurorehabilit. 2017, 41, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Kuppuswamy, A.; Balasubramaniam, A.V.; Maksimovic, R.; Mathias, C.J.; Gall, A.; Craggs, M.D.; Ellaway, P.H. Action of 5 hz repetitive transcranial magnetic stimulation on sensory, motor and autonomic function in human spinal cord injury. Clin. Neurophysiol. 2011, 122, 2452–2461. [Google Scholar] [CrossRef] [PubMed]
- Martin, R.; Sadowsky, C.; Obst, K.; Meyer, B.; McDonald, J. Functional electrical stimulation in spinal cord injury: From theory to practice. Top. Spinal Cord Inj. Rehabil. 2012, 18, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Tedesco Triccas, L.; Donovan-Hall, M.; Dibb, B.; Burridge, J.H. A nation-wide survey exploring the views of current and future use of functional electrical stimulation in spinal cord injury. Disabil. Rehabil. Assist. Technol. 2023, 18, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Arienti, C.; Patrini, M.; Negrini, S.; Kiekens, C. Overview of cochrane systematic reviews for rehabilitation interventions in persons with spinal cord injury: A mapping synthesis. Arch. Phys. Med. Rehabil. 2023, 104, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Borg, E.; Kaijser, L. A comparison between three rating scales for perceived exertion and two different work tests. Scand. J. Med. Sci. Sports 2006, 16, 57–69. [Google Scholar] [CrossRef]
- Shin, J.C.; Jeon, H.R.; Kim, D.; Cho, S.I.; Min, W.K.; Lee, J.S.; Oh, D.S.; Yoo, J. Effects on the motor function, proprioception, balance, and gait ability of the end-effector robot-assisted gait training for spinal cord injury patients. Brain Sci. 2021, 11, 1281. [Google Scholar] [CrossRef] [PubMed]
- Carrard, V.; Kunz, S.; Peter, C. Mental health, quality of life, self-efficacy, and social support of individuals living with spinal cord injury in switzerland compared to that of the general population. Spinal Cord 2021, 59, 398–409. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).