Continuity of Care in Adults Aging with Cerebral Palsy and Spina Bifida: The Importance of Community Healthcare and Socioeconomic Context
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Analytical Cohort
2.2. Measuring Continuity of Care
2.3. Measures of Community Characteristics
2.4. Statistical Analyses
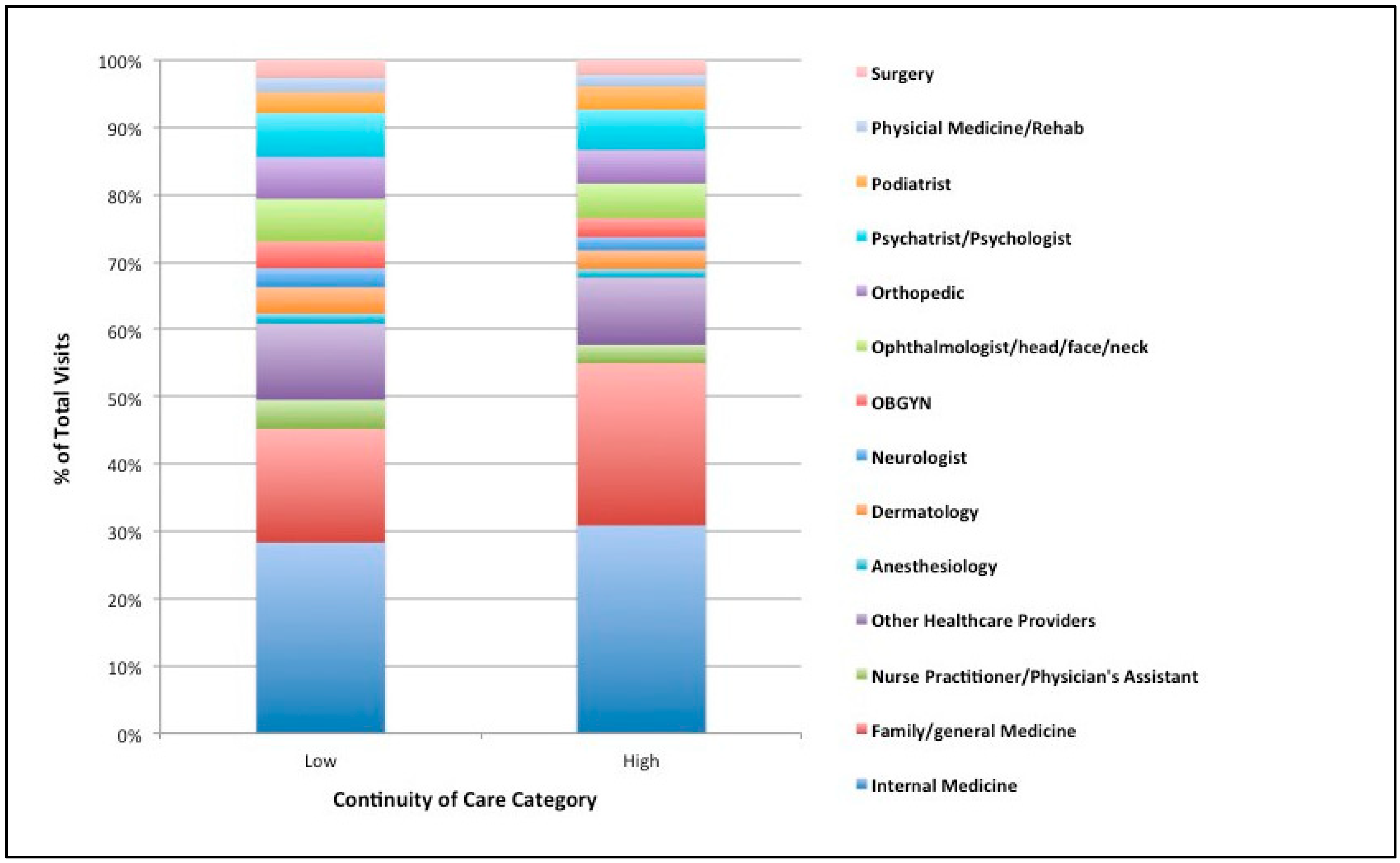
3. Results
4. Discussion
4.1. Continuity of Care in Adults Aging with CP/SB
4.2. Community Resources and Care Continuity
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Campbell, M.L.; Putnam, M. Reducing the shared burden of chronic conditions among persons aging with disability and older adults in the United States through bridging aging and disability. Healthcare 2017, 5, 56. [Google Scholar] [CrossRef]
- Molton, I.R.; Ordway, A. Aging with Disability: Populations, Programs, and the New Paradigm an Introduction to the Special Issue. J. Aging Health 2019, 31, 3S–20S. [Google Scholar] [CrossRef]
- Molton, I.R.; Yorkston, K.M. Growing Older with a Physical Disability: A Special Application of the Successful Aging Paradigm. J. Gerontol. Ser. B 2017, 72, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, L.M.; Latham, K.; Clarke, P.J. Aging with disability for midlife and older adults. Res. Aging 2017, 39, 741–777. [Google Scholar] [CrossRef] [PubMed]
- Field, M.; Jette, A. Secondary conditions and aging with disability. In The Future of Disability in America; Field, M., Jette, A., Eds.; National Academies Press: Washington, DC, USA, 2007; pp. 136–161. [Google Scholar]
- Clarke, P.; Latham, K. Life course health and socioeconomic profiles of Americans aging with disability. Disabil. Health J. 2014, 7, S15–S23. [Google Scholar] [CrossRef] [PubMed]
- Groah, S.L.; Charlifue, S.; Tate, D.; Jensen, M.P.; Molton, I.R.; Forchheimer, M. Spinal cord injury and aging: Challenges and recommendations for future research. Am. J. Phys. Med. Rehabil. 2012, 91, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.E.; Molton, I.R.; Jensen, M.P. Self-reported incidence and age of onset of chronic comorbid medical conditions in adults aging with long-term physical disability. Disabil. Health J. 2016, 9, 533–538. [Google Scholar] [CrossRef]
- Peterson, M.D.; Lin, P.; Kamdar, N.; Mahmoudi, E.; Schmidt, M.M.; Haapala, H.J.; Hurvitz, E.A. Cardiometabolic morbidity in adults with cerebral palsy and spina bifida. Am. J. Med. 2020, 133, e695–e705. [Google Scholar] [CrossRef] [PubMed]
- Tate, D.G.; Forchheimer, M.; Reber, L.; Meade, M.; Tan, N.; Clarke, P. Factors enabling comorbidities and secondary conditions in older adults with spinal cord injury. J. Spinal Cord Med. 2022, 1–12. [Google Scholar] [CrossRef]
- Li, C.; Clark, J.M.; Krause, J.S. Twenty-five-year cross-sequential analysis of self-reported problems: Findings from 5 cohorts from the spinal cord injury longitudinal aging study. Arch. Phys. Med. Rehabil. 2021, 102, 888–894. [Google Scholar] [CrossRef]
- Cook, K.F.; Molton, I.R.; Jensen, M.P. Fatigue and aging with a disability. Arch. Phys. Med. Rehabil. 2011, 92, 1126–1133. [Google Scholar] [CrossRef] [PubMed]
- Yi, Y.G.; Jung, S.H.; Bang, M.S. Emerging Issues in Cerebral Palsy Associated with Aging: A Physiatrist Perspective. Arm 2019, 43, 241–249. [Google Scholar] [CrossRef]
- Iezzoni, L.I.; McCarthy, E.P.; Davis, R.B.; Siebens, H. Mobility impairments and use of screening and preventive services. Am. J. Public Health 2000, 90, 955–961. [Google Scholar] [PubMed]
- Meltzer, D.O.; Ruhnke, G.W. Redesigning care for patients at increased hospitalization risk: The comprehensive care physician model. Health Aff. 2014, 33, 770–777. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, D.; Ryan, J.; Klein, S. Models of Care for High-Need, High-Cost Patients: An Evidence Synthesis; Commonwealth Fund: New York, NY, USA, 2015. [Google Scholar]
- Hirschman, K.; Shaid, E.; McCauley, K.; Pauly, M.; Naylor, M. Continuity of care: The transitional care model. Online J. Issues Nurs. 2015, 20, 13–27. [Google Scholar] [CrossRef]
- Long, P.; Abrams, M.; Milstein, A.; Anderson, G.; Apton, K.; Dahlberg, M.; Whicher, D. Effective Care for High-Need Patients; National Academy of Medicine: Washington, DC, USA, 2017. [Google Scholar]
- Shortell, S.M. Continuity of medical care: Conceptualization and measurement. Med. Care 1976, 14, 377–391. [Google Scholar] [CrossRef]
- Lagu, T.; Haywood, C.; Reimold, K.; DeJong, C.; Walker Sterling, R.; Iezzoni, L.I. ‘I Am Not the Doctor for You’: Physicians’ Attitudes about Caring for People with Disabilities: Study Examines Physician Attitudes about Caring for People with Disabilities. Health Aff. 2022, 41, 1387–1395. [Google Scholar] [CrossRef]
- Iezzoni, L.I. Eliminating Health and Health Care Disparities among The Growing Population of People with Disabilities. Health Aff. 2011, 30, 1947–1954. [Google Scholar] [CrossRef]
- Iezzoni, L.I.; Davis, R.B.; Soukup, J.; O’Day, B. Satisfaction with quality and access to health care among people with disabling conditions. Int. J. Qual. Health Care 2002, 14, 369–381. [Google Scholar] [CrossRef]
- Iezzoni, L.I.; Rao, S.R.; Ressalam, J.; Bolcic-Jankovic, D.; Agaronnik, N.D.; Donelan, K.; Lagu, T.; Campbell, E.G. Physicians’ Perceptions of People with Disability and Their Health Care: Study Reports the Results of a Survey of Physicians’ Perceptions of People with Disability. Health Aff. 2021, 40, 297–306. [Google Scholar] [CrossRef]
- McCarthy, E.P.; Ngo, L.H.; Roetzheim, R.G.; Chirikos, T.N.; Li, D.; Drews, R.E.; Iezzoni, L.I. Disparities in breast cancer treatment and survival for women with disabilities. Ann. Intern. Med. 2006, 145, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Dillaway, H.E.; Lysack, C.L. “Most of them are amateurs”: Women with spinal cord injury experience the lack of education and training among medical providers while seeking gynecological care. Disabil. Stud. Q. 2015, 35, 1–25. [Google Scholar] [CrossRef]
- Wolfe, M.K.; McDonald, N.C.; Holmes, G.M. Transportation barriers to health care in the United States: Findings from the national health interview survey, 1997–2017. Am. J. Public Health 2020, 110, 815–822. [Google Scholar] [CrossRef]
- Matin, B.K.; Williamson, H.J.; Karyani, A.K.; Rezaei, S.; Soofi, M.; Soltani, S. Barriers in access to healthcare for women with disabilities: A systematic review in qualitative studies. BMC Women’s Health 2021, 21, 44. [Google Scholar] [CrossRef]
- Remillard, E.T.; Campbell, M.L.; Koon, L.M.; Rogers, W.A. Transportation challenges for persons aging with mobility disability: Qualitative insights and policy implications. Disabil. Health J. 2022, 15, 101209. [Google Scholar] [CrossRef]
- Ryvicker, M.; Russell, D. Individual and environmental determinants of provider continuity among Urban older adults with heart failure: A retrospective cohort study. Gerontol. Geriatr. Med. 2018, 4, 2333721418801027. [Google Scholar] [CrossRef]
- Amjad, H.; Carmichael, D.; Austin, A.M.; Chang, C.-H.; Bynum, J.P.W. Continuity of Care and Health Care Utilization in Older Adults With Dementia in Fee-for-Service MedicareContinuity of Care in Older Adults With Dementia Continuity of Care in Older Adults With Dementia. JAMA Intern. Med. 2016, 176, 1371–1378. [Google Scholar] [CrossRef]
- Fontanella, C.A.; Guada, J.; Phillips, G.; Ranbom, L.; Fortney, J.C. Individual and contextual-level factors associated with continuity of care for adults with schizophrenia. Adm. Policy Ment. Health Ment. Health Serv. Res. 2014, 41, 572–587. [Google Scholar] [CrossRef]
- Forducey, P.G.; Glueckauf, R.L.; Bergquist, T.F.; Maheu, M.M.; Yutsis, M. Telehealth for persons with severe functional disabilities and their caregivers: Facilitating self-care management in the home setting. Psychol. Serv. 2012, 9, 144. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Parmanto, B. Reaching people with disabilities in underserved areas through digital interventions: Systematic review. J. Med. Internet Res. 2019, 21, e12981. [Google Scholar] [CrossRef] [PubMed]
- Bezyak, J.L.; Sabella, S.A.; Gattis, R.H. Public transportation: An investigation of barriers for people with disabilities. J. Disabil. Policy Stud. 2017, 28, 52–60. [Google Scholar] [CrossRef]
- Peterson, M.D.; Hurvitz, E.A. Cerebral palsy grows up. Mayo Clin. Proc. 2021, 96, 1404–1406. [Google Scholar] [CrossRef] [PubMed]
- Lidal, I.B.; Lundberg Larsen, K.; Hoff, M. 50 Years and older–born with spina bifida: Participation, health issues and physical function. Disabil. Rehabil. 2021, 43, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Cremer, N.; Hurvitz, E.A.; Peterson, M.D. Multimorbidity in middle-aged adults with cerebral palsy. Am. J. Med. 2017, 130, e9–e15. [Google Scholar] [CrossRef] [PubMed]
- Pollack, C.E.; Hussey, P.S.; Rudin, R.S.; Fox, D.S.; Lai, J.; Schneider, E.C. Measuring care continuity: A comparison of claims-based methods. Med. Care 2016, 54, e30. [Google Scholar] [CrossRef]
- Cohen-Mekelburg, S.; Saini, S.D.; Krein, S.L.; Hofer, T.P.; Wallace, B.I.; Hollingsworth, J.M.; Bynum, J.P.W.; Wiitala, W.; Burns, J.; Higgins, P.D.R.; et al. Association of continuity of care with outcomes in US veterans with inflammatory bowel disease. JAMA Netw. Open 2020, 3, e2015899. [Google Scholar] [CrossRef]
- Khan, A.; Li, M.; Finlay, J.; Esposito, M.; Gomez-Lopez, I.; Clarke, P.; Chenoweth, M. National Neighborhood Data Archive (NaNDA): Health Care Services by ZIP Code Tabulation Area, United States, 2003–2017; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2022. [Google Scholar] [CrossRef]
- Li, M.; Gomez-Lopez, I.; Khan, A.; Clarke, P.; Chenoweth, M. National Neighborhood Data Archive (NaNDA): Internet Access by ZIP Code Tabulation Area, United States, 2015–2019; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2021. [Google Scholar] [CrossRef]
- Melendez, R.; Li, M.; Khan, A.; Gomez-Lopez, I.; Clarke, P.; Chenoweth, M. National Neighborhood Data Archive (NaNDA): Public Transit Stops by ZIP Code Tabulation Area, United States, 2016–2018; Inter-University Consortium for Political and Social Research: Ann Arbor, MI, USA, 2021. [Google Scholar] [CrossRef]
- Naylor, K.B.; Tootoo, J.; Yakusheva, O.; Shipman, S.A.; Bynum, J.P.; Davis, M.A. Geographic variation in spatial accessibility of US healthcare providers. PLoS ONE 2019, 14, e0215016. [Google Scholar] [CrossRef] [PubMed]
- Wen, M.; Browning, C.R.; Cagney, K.A. Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Soc. Sci. Med. 2003, 57, 843–860. [Google Scholar] [CrossRef] [PubMed]
- Do, D.P.; Wang, L.; Elliott, M.R. Investigating the relationship between neighborhood poverty and mortality risk: A marginal structural modeling approach. Soc. Sci. Med. 2013, 91, 58–66. [Google Scholar] [CrossRef]
- Krause, N. Neighborhood deterioration and self-rated health in later life. Psychol. Aging 1996, 11, 342. [Google Scholar] [CrossRef]
- Moore, B.J.; White, S.; Washington, R.; Coenen, N.; Elixhauser, A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data. Med. Care 2017, 55, 698–705. [Google Scholar] [CrossRef]
- Whitney, D.G.; Kamdar, N.S.; Ng, S.; Hurvitz, E.A.; Peterson, M.D. Prevalence of high-burden medical conditions and health care resource utilization and costs among adults with cerebral palsy. Clin. Epidemiol. 2019, 11, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.D.; Lin, P.; Kamdar, N.; Hurvitz, E.A.; Mahmoudi, E. Psychological, cardiometabolic, and musculoskeletal morbidity and multimorbidity among adults with cerebral palsy and spina bifida: A retrospective cross-sectional study. Am. J. Phys. Med. Rehabil. 2021, 100, 940–945. [Google Scholar] [CrossRef] [PubMed]
- Hussey, P.S.; Schneider, E.C.; Rudin, R.S.; Fox, D.S.; Lai, J.; Pollack, C.E. Continuity and the costs of care for chronic disease. JAMA Intern. Med. 2014, 174, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Bynum, J.P.; Chang, C.H.; Austin, A.; Carmichael, D.; Meara, E. Outcomes in older adults with multimorbidity associated with predominant provider of care specialty. J. Am. Geriatr. Soc. 2017, 65, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Bayliss, E.A.; Ellis, J.L.; Shoup, J.A.; Zeng, C.; McQuillan, D.B.; Steiner, J.F. Effect of continuity of care on hospital utilization for seniors with multiple medical conditions in an integrated health care system. Ann. Fam. Med. 2015, 13, 123–129. [Google Scholar] [CrossRef]
- Taouk, L.H.; Fialkow, M.F.; Schulkin, J.A. Provision of reproductive healthcare to women with disabilities: A survey of obstetrician–gynecologists’ training, practices, and perceived barriers. Health Equity 2018, 2, 207–215. [Google Scholar] [CrossRef]
- Williams, M.D.; Asiedu, G.B.; Finnie, D.; Neely, C.; Egginton, J.; Finney Rutten, L.J.; Jacobson, R.M. Sustainable care coordination: A qualitative study of primary care provider, administrator, and insurer perspectives. BMC Health Serv. Res. 2019, 19, 92. [Google Scholar] [CrossRef]
- Doty, M.M.; Fryer, A.-K.; Audet, A.-M. The role of care coordinators in improving care coordination: The patient’s perspective. Arch. Intern. Med. 2012, 172, 587–588. [Google Scholar]
- Hostetter, M.; Klein, S. Creating Better Systems of Care for Adults with Disabilities: Lessons for Policy and Practice; The Commonwealth Fund: New York, NY, USA, 2018; pp. 147–148. [Google Scholar]
- Brault, M. Disability Status and the Characteristics of People in Group Quarters: A Brief Analysis of Disability Prevalence among the Civilian Noninstitutionalized and Total Populations in the American Community Survey; US Census Bureau: Washington, DC, USA, 2008.
- Browning, C.R.; Cagney, K.A. Moving beyond Poverty: Neighborhood Structure, Social Processes, and Health. J. Health Soc. Behav. 2003, 44, 552–571. [Google Scholar] [CrossRef]
- Davis, M.A.; Anthopolos, R.; Tootoo, J.; Titler, M.; Bynum, J.P.; Shipman, S.A. Supply of healthcare providers in relation to county socioeconomic and health status. J. Gen. Intern. Med. 2018, 33, 412–414. [Google Scholar] [CrossRef] [PubMed]
- Bynum, J.P. The long reach of alzheimer’s disease: Patients, practice, and policy. Health Aff. 2014, 33, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Gudzune, K.A.; Bennett, W.L.; Cooper, L.A.; Clark, J.M.; Bleich, S.N. Prior doctor shopping resulting from differential treatment correlates with differences in current patient-provider relationships. Obesity 2014, 22, 1952–1955. [Google Scholar] [CrossRef] [PubMed]
- Iezzoni, L.I. Assessing quality using administrative data. Ann. Intern. Med. 1997, 127, 666–674. [Google Scholar] [CrossRef]
- Buajitti, E.; Chiodo, S.; Rosella, L.C. Agreement between area-and individual-level income measures in a population-based cohort: Implications for population health research. SSM Popul. Health 2020, 10, 100553. [Google Scholar] [CrossRef]
- Stange, K.C. The problem of fragmentation and the need for integrative solutions. Ann. Fam. Med. 2009, 7, 100–103. [Google Scholar] [CrossRef] [PubMed]
| Overall | High COC | Low COC | |
|---|---|---|---|
| N | 8596 | 4221 | 4375 |
| Continuity of Care, mean (SD) | 0.3 (0.19) | 0.52 (0.24) | 0.14 (0.06) |
| Individual Characteristics | |||
| Age (years), mean (SD) | 48.6 (13.6) | 49.9 (14.2) | 47.3 (13.9) |
| Sex, % | |||
| Female | 61.6 | 59.1 | 64.0 |
| Male | 38.4 | 41.0 | 36.0 |
| Comorbidity, mean (SD) | 2.7 (2.0) | 2.6 (2.1) | 2.7 (2.0) |
| Community Characteristics (%) | |||
| Density of Healthcare Resources | |||
| Hospitals | |||
| Low | 33.9 | 32.8 | |
| Medium | 32.2 | 34.5 | |
| High | 34.0 | 32.7 | |
| Residential Care/Skilled Nursing Facilities | |||
| Low | 33.0 | 33.7 | |
| Medium | 32.3 | 34.3 | |
| High | 34.7 | 32.0 | |
| Ambulatory Care Services | |||
| Low | 33.8 | 32.8 | |
| Medium | 33.4 | 33.4 | |
| High | 32.9 | 33.8 | |
| Spatial Accessibility of Healthcare Providers | |||
| Family Medicine/Nurse Practitioners | |||
| Low | 42.0 | 36.6 | |
| Medium | 21.1 | 22.4 | |
| High | 37.0 | 40.9 | |
| Medical Specialists | |||
| Low | 34.6 | 32.1 | |
| Medium | 33.8 | 33.0 | |
| High | 31.6 | 35.0 | |
| Chiropractors | |||
| Low | 35.8 | 30.9 | |
| Medium | 32.8 | 34.0 | |
| High | 31.5 | 35.1 | |
| Socioeconomic Structure | |||
| Affluence | |||
| Low | 37.4 | 29.4 | |
| Medium | 33.9 | 32.8 | |
| High | 28.7 | 37.8 | |
| Disadvantage | |||
| Low | 29.6 | 36.9 | |
| Medium | 34.8 | 32.0 | |
| High | 35.6 | 31.1 | |
| Public Infrastructure | |||
| Density of Public Transit stops | |||
| Low | 45.9 | 45.6 | |
| Medium | 20.5 | 21.4 | |
| High | 33.6 | 33.0 | |
| Density of Broadband Internet Connections | |||
| Low | 37.1 | 29.7 | |
| Medium | 33.0 | 33.7 | |
| High | 30.0 | 36.6 |
| Density of Community Characteristics (Ref = High) | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Ambulatory Care | ||
| Low | 1.10 | (0.87, 1.38) |
| Medium | 1.11 | (0.95, 1.31) |
| Hospitals | ||
| Low | 0.89 | (0.74, 1.07) |
| Medium | 0.84 | (0.72, 0.98) |
| Residential Care/Skilled Nursing | ||
| Low | 0.72 | (0.59, 0.88) |
| Medium | 0.84 | (0.73, 0.96) |
| Family Medicine/Nurse Practitioners | ||
| Low | 1.26 | (1.09, 1.46) |
| Medium | 1.05 | (0.92, 1.21) |
| Medical Specialists | ||
| Low | 1.07 | (0.91, 1.27) |
| Medium | 1.10 | (0.96, 1.25) |
| Chiropractors | ||
| Low | 1.08 | (0.95, 1.23) |
| Medium | 1.00 | (0.89, 1.12) |
| Public Transit Stops | ||
| Low | 1.09 | (0.96, 1.25) |
| Medium | 1.15 | (0.99, 1.34) |
| Broadband Internet | ||
| Low | 1.11 | (0.94, 1.31) |
| Medium | 0.99 | (0.87, 1.13) |
| Socioeconomic Disadvantage | ||
| Low | 0.96 | (0.82, 1.13) |
| Medium | 1.15 | (0.99, 1.34) |
| Socioeconomic Affluence | ||
| Low | 1.55 | (1.29, 1.86) |
| Medium | 1.26 | (1.10, 1.45) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khan, A.M.; Lin, P.; Kamdar, N.; Mahmoudi, E.; Clarke, P. Continuity of Care in Adults Aging with Cerebral Palsy and Spina Bifida: The Importance of Community Healthcare and Socioeconomic Context. Disabilities 2023, 3, 295-306. https://doi.org/10.3390/disabilities3020019
Khan AM, Lin P, Kamdar N, Mahmoudi E, Clarke P. Continuity of Care in Adults Aging with Cerebral Palsy and Spina Bifida: The Importance of Community Healthcare and Socioeconomic Context. Disabilities. 2023; 3(2):295-306. https://doi.org/10.3390/disabilities3020019
Chicago/Turabian StyleKhan, Anam M., Paul Lin, Neil Kamdar, Elham Mahmoudi, and Philippa Clarke. 2023. "Continuity of Care in Adults Aging with Cerebral Palsy and Spina Bifida: The Importance of Community Healthcare and Socioeconomic Context" Disabilities 3, no. 2: 295-306. https://doi.org/10.3390/disabilities3020019
APA StyleKhan, A. M., Lin, P., Kamdar, N., Mahmoudi, E., & Clarke, P. (2023). Continuity of Care in Adults Aging with Cerebral Palsy and Spina Bifida: The Importance of Community Healthcare and Socioeconomic Context. Disabilities, 3(2), 295-306. https://doi.org/10.3390/disabilities3020019







