Physical Activity Levels during Therapeutic Camp Activities in Youth with Disabilities in the United States
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
Camp Setting
2.2. Study Design
2.2.1. Accelerometry
2.2.2. Data Analysis
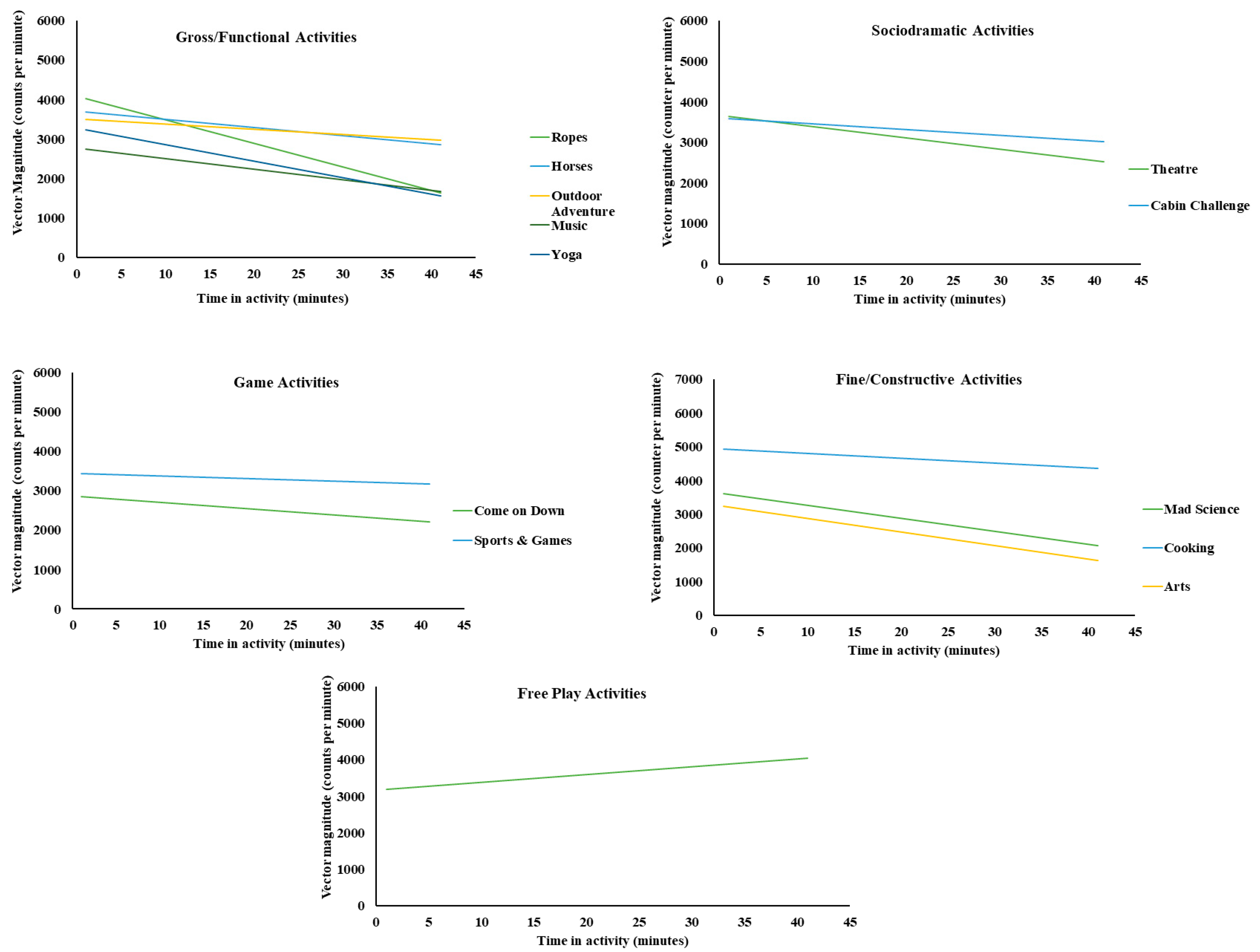
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bize, R.; Johnson, J.A.; Plotnikoff, R.C. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev. Med. 2007, 45, 401–415. [Google Scholar] [CrossRef] [PubMed]
- Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Scientific Report; US Department of Health and Human Services: Washington, DC, USA, 2018.
- Boyle, C.A.; Boulet, S.; Schieve, L.A.; Cohen, R.A.; Blumberg, S.J.; Yeargin-Allsopp, M.; Visser, S.; Kogan, M.D. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics 2011, 127, 1034–1042. [Google Scholar] [CrossRef] [PubMed]
- Lobenius-Palmer, K.; Sjoqvist, B.; Hurtig-Wennlof, A.; Lundqvist, L.O. Accelerometer-Assessed physical activity and sedentary time in youth with disabilities. Adapt. Phys. Activ. Q. 2018, 35, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.P.; Tremblay, M.S. Systematic review of sedentary behaviour and health indicators in school-aged children and youth: An update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Carson, V.; Chaput, J.P.; Connor Gorber, S.; Dinh, T.; Duggan, M.; Zehr, L. Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2016, 41, S311–S327. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Kodish, S.; Kulinna, P.H.; Martin, J.; Pangrazi, R.; Darst, P. Determinants of physical activity in an inclusive setting. Adapt. Phys. Activ. Q. 2006, 23, 390–409. [Google Scholar] [CrossRef]
- Darrah, J.; Wessel, J.; Nearingburg, P.; O'Connor, M. Evaluation of a community fitness program for adolescents with cerebral palsy. Pediatric. Phys. Ther. 1999, 11, 18–23. [Google Scholar] [CrossRef]
- Schreiber, J.; Marchetti, G.; Crytzer, T. The implementation of a fitness program for children with disabilities: A clinical case report. Pediatric. Phys. Ther. 2004, 16, 173–179. [Google Scholar] [CrossRef]
- Allsop, J.; Negley, S.; Sibthorp, J. Assessing the social effect of Therapeutic Recreation summer camp for adolescents with chronic illness. Ther. Recreat. J. 2013, 47, 35–46. [Google Scholar]
- Wozencroft, A.J.; Scott, J.L.; Waller, S.N.; Parsons, M.D. Positive youth development for youth with disabilities in a therapeutic camp setting. J. Youth Dev. 2019, 14, 182–197. [Google Scholar] [CrossRef]
- Moxham, L.; Liersch-Sumskis, S.; Taylor, E.; Patterson, C.; Brighton, R. Preliminary outcomes of a pilot Therapeutic Recreation camp for people with a mental illness. Ther. Recreat. J. 2015, 49, 61–75. [Google Scholar]
- Cotton, S.M.; Butselaar, F.J. Adventure Camps for young adults and adults with mental illness. Psychiatr. Serv. 2012, 63, 1154. [Google Scholar]
- Sarkin, J.A.; McKenzie, T.L.; Sallis, J.F. Gender differences in physical activity during fifth-grade physical education and recess periods. J. Teach. Phys. Educ. 1997, 17, 99–106. [Google Scholar] [CrossRef]
- MacDonald, M.; Esposito, P.; Ulrich, D. The physical activity patterns of children with autism. BMC Res. Notes 2011, 4, 422. [Google Scholar] [CrossRef] [PubMed]
- Yogman, M.; Garner, A.; Hutchinson, J.; Hirsh-Pasek, K.; Golinkoff, R.M. The Power of Play: A Pediatric Role in Enhancing Development in Young Children. Pediatrics 2018, 142, e20182058. [Google Scholar] [CrossRef] [PubMed]
- Welk, G.; Morrow, J.; Saint-Maurice, P. Measures Registry User Guide: Individual Physical Activity; National Collaborative on Childhood Obesity Research: Washington, DC, USA, 2017; Available online: https://nccor.org/tools-mruserguides/wp-content/uploads/2017/NCCOR_MR_User_Guide_Individual_PA-FINAL.pdf (accessed on 23 November 2022).
- Trost, S.G.; Ward, D.S.; Moorehead, S.M.; Watson, P.D.; Riner, W.; Burke, J.R. Validity of the computer science and applications (CSA) activity monitor in children. Med. Sci. Sports Exerc. 1998, 30, 629–633. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; McIver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37, S531–S543. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.; Pober, D.; Janz, K.F. Calibration of accelerometer output for children. Med. Sci. Sports Exerc. 2005, 37, S523–S530. [Google Scholar] [CrossRef]
- Troiano, R.P.; McClain, J.J.; Brychta, R.J.; Chen, K.Y. Evolution of accelerometer methods for physical activity research. Br. J. Sports Med. 2014, 48, 1019–1023. [Google Scholar] [CrossRef] [PubMed]
- Herrington, W.G.; Goldsack, J.C.; Landray, M.J. Increasing the use of mobile technology-derived endpoints in clinical trials. Clin. Trials 2018, 15, 313–315. [Google Scholar] [CrossRef] [PubMed]
- Belcher, B.R.; Wolff-Hughes, D.L.; Dooley, E.E.; Staudenmayer, J.; Berrigan, D.; Eberhardt, M.S.; Troiano, R.P. US Population-referenced Percentiles for Wrist-Worn Accelerometer-derived Activity. Med. Sci. Sports Exerc. 2021, 53, 2455–2464. [Google Scholar] [CrossRef] [PubMed]
- Millard, L.A.C.; Tilling, K.; Gaunt, T.R.; Carslake, D.; Lawlor, D.A. Correction: Association of physical activity intensity and bout length with mortality: An observational study of 79,503 UK Biobank participants. PLoS Med. 2022, 19, e1004020. [Google Scholar] [CrossRef] [PubMed]
- Chiew, T.K.; Khoo, S.; Ansari, P.; Kiruthika, U. Mobile and wearable technologies for persons with disabilities: A bibliometric analysis (2000–2021). Disabil. Rehabil. Assist. Technol. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; Noonan, R.J.; Rowlands, A.V.; van Hees, V.; Knowles, Z.R.; Boddy, L.M. Wear Compliance and Activity in Children Wearing Wrist and Hip-Mounted Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 245–253. [Google Scholar] [CrossRef]
- Crouter, S.E.; Flynn, J.I.; Bassett, D.R., Jr. Estimating physical activity in youth using a wrist accelerometer. Med. Sci. Sports Exerc. 2015, 47, 944–951. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Bassett, D.R. The technology of accelerometry-based activity monitors: Current and future. Med. Sci. Sports Exerc. 2005, 37, S490–S500. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Hibbing, P.; Saint-Maurice, P.F.; Ellingson, L.D.; Hennessy, E.; Wolff-Hughes, D.L.; Perna, F.M.; Welk, G.J. Surveillance of Youth Physical Activity and Sedentary Behavior with Wrist Accelerometry. Am. J. Prev. Med. 2017, 52, 872–879. [Google Scholar] [CrossRef] [PubMed]
- Arteaga, D.; Donnelly, T.; Crum, K.; Markham, L.; Killian, M.; Burnette, W.B.; Soslow, J.; Buchowski, M.S. Assessing Physical Activity Using Accelerometers in Youth with Duchenne Muscular Dystrophy. J. Neuromuscul. Dis. 2020, 7, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Hulst, R.Y.; Gorter, J.W.; Obeid, J.; Voorman, J.M.; van Rijssen, I.M.; Gerritsen, A.; Visser-Meily, J.M.A.; Pillen, S.; Verschuren, O. Accelerometer-measured physical activity, sedentary behavior, and sleep in children with cerebral palsy and their adherence to the 24-hour activity guidelines. Dev. Med. Child Neurol. 2022. ahead of print. [Google Scholar] [CrossRef]
- Choi, L.; Liu, Z.; Matthews, C.E.; Buchowski, M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sport Exerc. 2011, 43, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Ruch, N.; Rumo, M.; Mader, U. Recognition of activities in children by two uniaxial accelerometers in free-living conditions. Eur. J. Appl. Physiol. 2011, 111, 1917–1927. [Google Scholar] [CrossRef] [PubMed]
- Howie, E.K.; Brown, W.H.; Dowda, M.; McIver, K.L.; Pate, R.R. Physical activity behaviours of highly active preschoolers. Pediatric. Obes. 2013, 8, 142–149. [Google Scholar] [CrossRef]
- Gao, Z.; Podlog, L.; Huang, C. Associations among children's situational motivation, physical activity participation, and enjoyment in an active dance video game. J. Sport. Health Sci. 2013, 2, 122–128. [Google Scholar] [CrossRef]
- Lyden, K.; Keadle, S.K.; Staudenmayer, J.; Freedson, P.; Alhassan, S. Energy cost of common activities in children and adolescents. J. Phys. Act. Health 2013, 10, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, J.L.; Sallis, J.F.; Saelens, B.E.; Cain, K.L.; Black, J.B. The association of neighborhood design and recreational environments with physical activity. Am. J. Health Promot. 2005, 19, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Ward, J.A.; Richardson, D.; Orgs, G.; Hunter, K.; Hamilton, A. Sensing interpersonal synchrony between actors and autistic children in theatre using wrist-worn accelerometers. In Proceedings of the 2018 ACM International Symposium on Wearable Computers, Singapore, 8–12 October 2018; pp. 148–155. [Google Scholar]
- Hickerson, B.D.; Henderson, K.A. Opportunities for promoting youth physical activity: An examination of youth summer camps. J. Phys. Act. Health 2014, 11, 199–205. [Google Scholar] [CrossRef]
- Jago, R.; Baranowski, T. Non-curricular approaches for increasing physical activity in youth: A review. Prev. Med. 2004, 39, 157–163. [Google Scholar] [CrossRef]
- Leung, W.; Siebert, E.A.; Yun, J. Measuring physical activity with accelerometers for individuals with intellectual disability: A systematic review. Res. Dev. Disabil. 2017, 67, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Marin Ginnis, K.A.; van der Ploeg, H.P.; Foster, C.; Lai, B.; McBride, C.B.; Ng, K.; Pratt, M.P.; Shirazipour, C.H.; Smith, B.; Vazquez, P.M.; et al. Participation of people living with disabilities in physical activity: A global perspective. Lancet 2021, 398, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Khursid, S.; Weng, L.-C.; Nauffal, V.; Pirruccello, J.P.; Venn, R.A.; Al-Alusi, M.A.; Benjamin, E.J.; Ellinor, P.T.; Lubitz, S.A. Wearable accelerometer-derived physical activity and incident disease. NPJ Digit. Med. 2022, 5, 131. [Google Scholar] [CrossRef]
- Ekkekakis, P.; Hall, E.E.; Petruzzello, S.J. Variation and homogeneity in affective responses to physical activity of varying intensities: An alternative perspective on dose–response based on evolutionary considerations. J. Sports Sci. 2005, 23, 477–500. [Google Scholar] [CrossRef] [PubMed]
- Richard, M.; Christina, M.F.; Deborah, L.S.; Rubio, N.; Kennon, M.S. Intrinsic motivation and exercise adherence. Int. J. Sport Exerc. Psychol. 1997, 28, 335–354. [Google Scholar]
- McConnell, S.R. Interventions to facilitate social interaction for young children with autism: Review of available research and recommendations for educational intervention and future research. J. Autism. Dev. Disord. 2002, 32, 351–372. [Google Scholar] [CrossRef]
- Morrison, R.S.; Sainato, D.M.; Benchaaban, D.; Endo, S. Increasing play skills of children with autism using activity schedules and correspondence training. J. Early Interv. 2002, 25, 58–72. [Google Scholar] [CrossRef]
- Wolery, M.; Wilbers, J.S. (Eds.) Including Children with Special Needs in Early Childhood Programs: Research Monograph of the National Association for the Education of Young Children; National Association for the Education of Young Children: Washington, DC, USA, 1994; Volume 6. [Google Scholar]
- Rimmer, J.A.; Rowland, J.L. Physical activity for youth with disabilities: A critical need in an underserved population. Dev. Neurorehabil. 2008, 11, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Y.; Liu, C.W.; Chung, I.C.; Hsu, P.J. Physical activity levels of adolescents with and without intellectual disabilities during physical education and recess. Res. Dev. Disabil. 2014, 36, 579–586. [Google Scholar] [CrossRef]
- Ridgers, N.D.; Salmon, J.; Parrish, A.M.; Stanley, R.M.; Okely, A.D. Physical activity during school recess: A systematic review. Am. J. Prev. Med. 2012, 43, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Sit, C.H.; McKenzie, T.L.; Cerin, E.; Chow, B.C.; Huang, W.Y.; Yu, J. Physical Activity and Sedentary Time among Children with Disabilities at School. Med. Sci. Sports Exerc. 2017, 49, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Dowda, M.; Brown, W.H.; Mitchell, J.; Addy, C. Physical activity in preschool children with the transition to outdoors. J. Phys. Act. Health 2013, 10, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.Y.; Frey, G.C. Physical activity patterns in youth with autism spectrum disorders. J. Autism Dev. Disord. 2006, 36, 597–606. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Barreira, T.V.; Schuna, J.M. Comparison of step outputs for waist and wrist accelerometer attachment sites. Med. Sci. Sports Exerc. 2015, 47, 839–842. [Google Scholar] [CrossRef]
- Hildebrand, M.; van Hees, V.T.; Hansen, B.H.; Ekelund, U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med. Sci. Sports Exerc. 2014, 46, 1816–1824. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, M.E.; Haskell, W.L.; Albinali, F.; Mota, S.; Nawyn, J.; Intille, S. Estimating activity and sedentary behavior from an accelerometer on the hip or wrist. Med. Sci. Sports Exerc. 2013, 45, 964–975. [Google Scholar] [CrossRef]
- Butte, N.F.; Watson, K.B.; Ridley, K.; Zakeri, I.F.; Mcmurray, R.G.; Pfeiffer, K.A.; Berhane, Z. A youth compendium of physical activities: Activity codes and metabolic intensities. Med. Sci. Sports Exerc. 2018, 50, 246–256. [Google Scholar] [CrossRef]
- Haley, L.; McKay, E.A. ‘Baking gives you confidence’: Users' views of engaging in the occupation of baking. Br. J. Occup. Ther. 2004, 67, 125–128. [Google Scholar] [CrossRef]
- Thompson, W.R. Worldwide survey of fitness trends for 2021. ACSMs Health Fit. J. 2020, 24, 10–18. [Google Scholar] [CrossRef]
| Age | 14.6 ± 3.9 |
| Mass (kg) | 59.3 ± 24.6 |
| Height (cm) | 152.8 ± 18.0 |
| BMI (kg/m2) | 24.5 ± 6.7 |
| Sex | |
| Male | 45% |
| Female | 55% |
| Autism (n = 6) | Genetic disorder (n = 1) |
| Cerebral Palsy (n = 1) | Global Apraxia (n = 1) |
| Developmental Delay (n = 1) | Global Developmental Delays (n = 1) |
| Disgenisis of the Corpus Callosum (n = 1) | Intellectual Disability (n = 4) |
| Down Syndrome (n = 9) | Prader–Willi Syndrome (n = 1) |
| Dup15q Syndrome (n = 1) | Spina Bifida (n = 1) |
| Tetrasomy X (n = 1) | |
| Activity | Description |
|---|---|
| Gross/Functional | |
| Ropes | Movement at a self-selected pace through a tight rope like obstacle course. Movement would primarily be classified as balancing and walking. |
| Horses | Engagement in actual horseback riding with assistance. Activity would be limited to upper body movement with the lower body providing stability on the horses. |
| Outdoor Adventure | Learn and execute basic survival skills such as movement though obstacle courses at a self-selected pace, typically walking. |
| Music and Movement | Learn and execute dance movements. |
| Yoga | Learn and execute basic yoga movements. |
| Canoeing * | Ride in a canoe while counselors paddle. Movement is restricted during this activity for safety reasons. |
| Game | |
| Come on Down | An interactive game that tests the knowledge of popular culture in a game show format, participants alternate between seated and standing positions. |
| Sports and Games | A variety of sports and games played within a controlled and inclusive environment. |
| Sociodramatic | |
| Theatre | Development and performance of pretend play on stage. The participants alternated between seated and standing positions. |
| Cabin Challenge | Challenging tasks that stimulate cognitive functioning. Participants were seated for the majority of this activity. |
| Fine/Constructive | |
| Arts | Consisting of various artistic projects. Participants were seated for the majority of this activity. |
| Cooking | Learn and execute basic cooking skills and techniques. Participants were seated for the majority of this activity. |
| Mad Science | Participate in a variety of scientific experiments. Participants were seated for the majority of this activity. |
| Free Period | |
| Unstructured free time | A free period of time with no planned activities. Activities varied during this time. |
| Activity Category (Activity) | Vector Magnitude (Counts per Minute) | Activity Intensity (%; Min during the 41-min Activity Session) | ||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Median (IQR) | Sedentary | Light | Moderate | |
| Gross/Functional | 3690 | 2807.2 (2383.7) | 2363.6 (1145.2–3831.4) | |||
| Ropes | 779 | 2698.5 (2130.7) | 2239.4 (1192.0–3691.3) | 75.6 (31 min) | 19.5 (8 min) | 4.9 (2 min) |
| Horses | 738 | 3409.2 (2458.5) | 3073.8 (1719.6–4444.1) | 58.5 (24 min) | 41.5 (17 min) | 0 (0 min) |
| Outdoor Adventure | 779 | 3234.6 (2700.4) | 2710.9 (1584.0–4168.7) | 53.78 (22 min) | 46.3 (19 min) | 0 (0 min) |
| Music & Movement | 697 | 2208.2 (1880.1) | 1813.7 (865.8–3128.6) | 92.7 (38 min) | 7.3 (3 min) | 0 (0 min) |
| Yoga | 697 | 2412.2 (2416.1) | 1872.4 (800.1–3326.4) | 87.8 (36 min) | 12.2 (5 min) | 0 (0 min) |
| Game | 1558 | 2938.9 (2461.4) | 2481.9 (1198.2–4050.9) | |||
| Come on Down | 738 | 2527.6 (2074.9) | 2119.5 (998.4–3555.1) | 90.2 (37 min) | 9.8 (4 min) | 0 (0 min) |
| Sports & Games | 820 | 3309.1 (2715.5) | 2752.8 (1412.8–4498.11) | 58.5 (24 min) | 41.5 (17 min) | 0 (0 min) |
| Sociodramatic | 1599 | 3155.0 (2580.6) | 2650.4 (1446.3–4304.1) | |||
| Theatre | 861 | 3080.6 (2715.5) | 2538.3 (1373.9–4176.1) | 68.3 (28 min) | 29.3 (12 min) | 2.4 (1 min) |
| Cabin Challenge | 738 | 3241.9 (2412.7) | 2882.4 (1535.7–4485.0) | 63.4 (26 min) | 36.6 (15 min) | 0 (0 min) |
| Fine/Constructive | 2127 | 3225.8 (3393.1) | 2295.4 (1036.4–4157.6) | |||
| Art | 738 | 2876.0 (2742.8) | 2183.0 (1339.0–3351.0) | 80.5 (33 min) | 19.5 (8 min) | 0 (0 min) |
| Cooking | 697 | 4379.8 (4403.4) | 3281.0 (1046.5–6371.9) | 2.4 (1 min) | 65.9 (27 min) | 31.7 (13 min) |
| Mad Science | 692 | 2436.7 (2402.3) | 1887.0(669.3–3425.4) | 87.8 (36 min) | 12.2 (5 min) | 0 (0 min) |
| Free Period | 697 | 3610.2 (3518.8) | 2914.2 (933.9–5334.2) | |||
| Unstructured Free Time | 697 | 3610.2 (3518.8) | 2914.2 (933.9–5334.2) | 31.7 (13 min) | 68.3 (28 min) | 0 (0 min) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nocera, V.G.; Kybartas, T.J.; Wozencroft, A.J.; Coe, D.P. Physical Activity Levels during Therapeutic Camp Activities in Youth with Disabilities in the United States. Disabilities 2022, 2, 764-777. https://doi.org/10.3390/disabilities2040053
Nocera VG, Kybartas TJ, Wozencroft AJ, Coe DP. Physical Activity Levels during Therapeutic Camp Activities in Youth with Disabilities in the United States. Disabilities. 2022; 2(4):764-777. https://doi.org/10.3390/disabilities2040053
Chicago/Turabian StyleNocera, Vincenzo G., Tyler J. Kybartas, Angela J. Wozencroft, and Dawn P. Coe. 2022. "Physical Activity Levels during Therapeutic Camp Activities in Youth with Disabilities in the United States" Disabilities 2, no. 4: 764-777. https://doi.org/10.3390/disabilities2040053
APA StyleNocera, V. G., Kybartas, T. J., Wozencroft, A. J., & Coe, D. P. (2022). Physical Activity Levels during Therapeutic Camp Activities in Youth with Disabilities in the United States. Disabilities, 2(4), 764-777. https://doi.org/10.3390/disabilities2040053







