Experiences of Social Participation for Canadian Wheelchair Users with Spinal Cord Injury during the First Wave of the COVID-19 Pandemic
Abstract
:1. Introduction
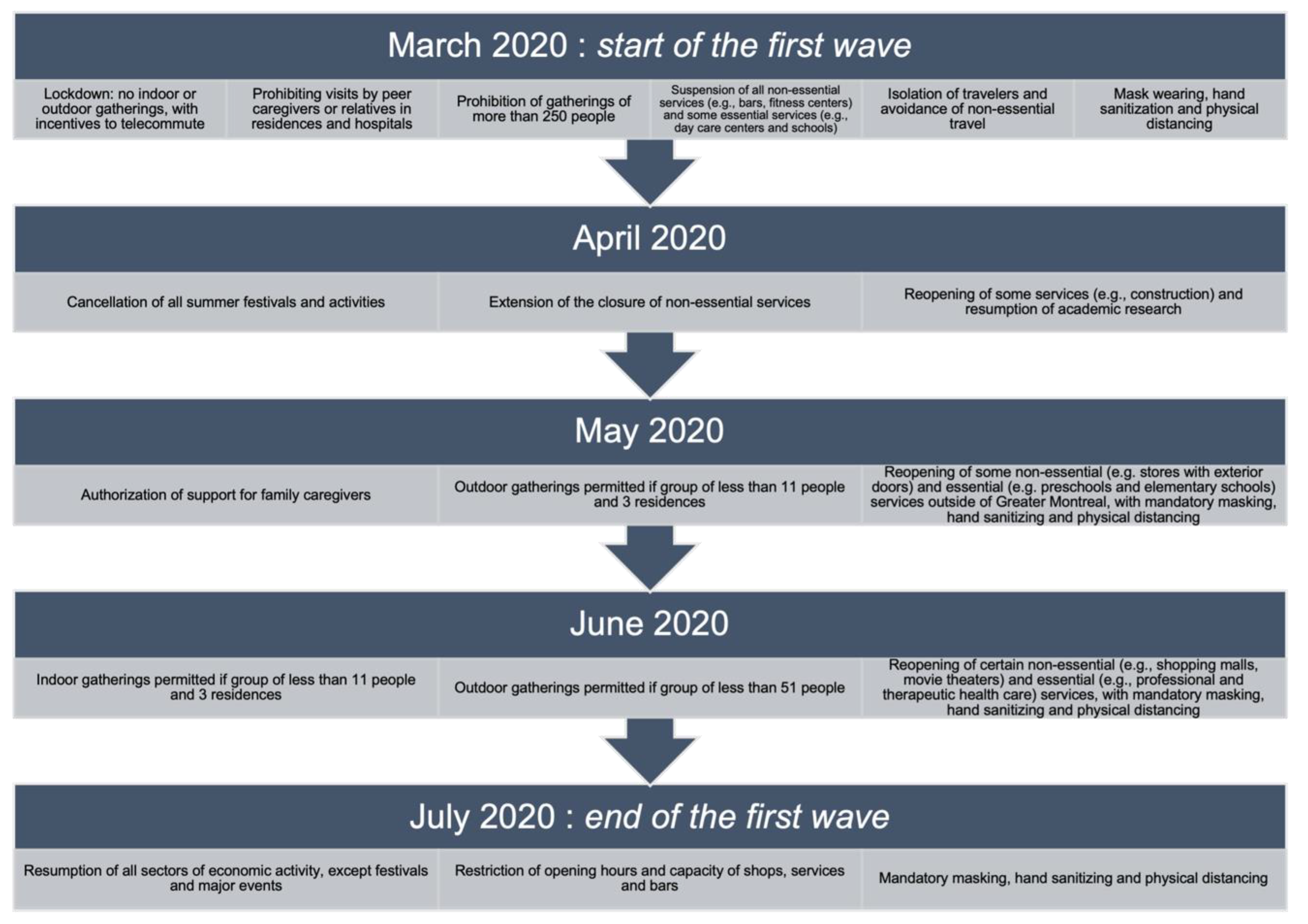
2. Materials and Methods
2.1. Design
2.2. Participants and Recruitment
2.3. Procedures
2.4. Data Collection
2.5. Assessment of Life Habits (LIFE-H 4.0)
2.6. Measure of Quality of the Environment (MQE)
2.7. Data Analysis
3. Results
3.1. Demographics
3.2. Qualitative Findings
3.2.1. Theme 1: “Perceived Participation Restrictions for People with SCI and Their Loved Ones during COVID-19”
“Regarding my services, the only thing that I lost is the house cleaning, so my son does some (housecleaning) as well as my wife.”(Participant 10)
“It’s only for the rehab, for the wheelchair, it’s harder. You can’t take appointments. And some appointments of the doctors, for example, the radiology and something like that, it’s all cancelled.”(Participant 3)
“Grocery shopping was as usual, I used to do all my shopping online before, it didn’t change much in this regard either.”(Participant 10)
“Well, when you need a hand, that’s for sure… it just blows up all over the place. I mean, they’re all ready to help us. (…) the three of us were able to organize. So, everyone was helping…”(Participant 7)
“I think that phone consultations are useful, I think it is great that we do not have to go on-site.”(Participant 6)
“The pandemic and the lockdown is like putting myself on the ground, in a state of inertia. (…) During the whole period, I do nothing. (…) The (activity) must be physical, sensory, all of that. But right now, I’m really not into it, it worried me and still worries me. (…) It affects my self-esteem because I really don’t feel capable.”(Participant 8)
“Not that we are more independent, but people are less willing to help you with contamination. (…) So, every day, I still pay more attention to what I’m doing so that I don’t need help.”(Participant 8)
“The association between sick people and disabled people is quite strong.”(Participant 10)
“I think it puts us, the people who have dependencies on services or technical assistance, it puts us in the position of a person where we are asked to not make things worse. (…) through the pandemic, we were unintentionally labelled as people who had a good potential to do damage, to get sick, (…) so our situation wasn’t very good.”(Participant 8)
“Technology helped (kept) independence during COVID-19.”(Participant 5)
“It (facetime with health professionals) was good. Yeah. You just phoned in, and then they set up a time, and then the doctor would phone you back and do everything over the phone.”(Participant 4)
3.2.2. Theme 2: There Was No Change in Life Habits (But Found New Ways to Do Some Things)
“(Lockdown) did not have much influence, because I am in a wheelchair, sometimes I am a little bit restricted in advance. And it gets worse in winter.”(Participant 12)
“Well, I didn’t have a problem with that (lockdown). It didn’t bother me, it was winter. And then in the winter I am not going out, I am less out in the winter than in the summer. It didn’t affect me too much.”(Participant 13)
“I’ve been using my phone and internet a lot more that I used to.”(Participant 2)
“Well, I think I’ll be a lot more appreciative of my friend, the community, and just more appreciative about the fact that I’m able to get out and enjoy my life. So just an increase in appreciation of the enjoyment that’s available.”(Participant 3)
3.2.3. Theme 3: “Future Hopes and Concerns”
(…) Like the water pumps with the feet, it is a little difficult when you are in a wheelchair, or the openers with the feet because they have deactivated the automatic opening.(participant 5)
“It will get worse. The thing that they are … for example a lot of them was doing their workout and their moving, and now they lost all what they had from the strain and injury because (…) the spinal cord injury people stop work out, they will lose what they have.”(Participant 9)
“I think people will be more cautious about maybe handshakes and hugging people. Yeah, I think people will just be a little bit more paranoid about the possibility of another infection.”(Participant 3)
“People who have that (SCI), they understand our situation and they have tips, that’s what helps.”(Participant 12)
“(About) the virtual long-distance way of offering services. I don’t think you can replace a human experience itself, so maybe have that as an option, or as an add-on, (…) I think the idea of having a choice, rather than having to do things one way.”(Participant 1)
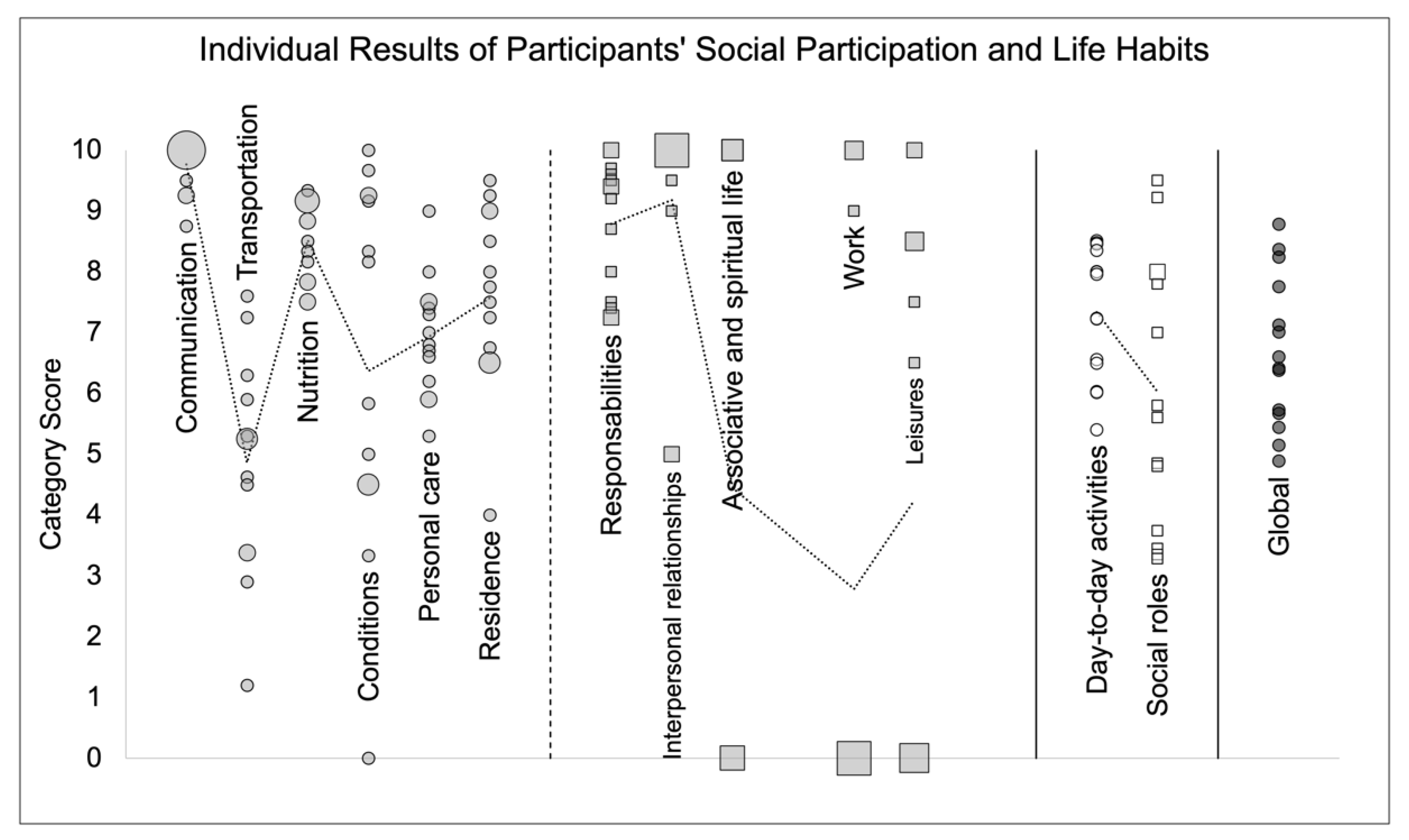
3.3. Quantitative Findings
3.3.1. Social Participation
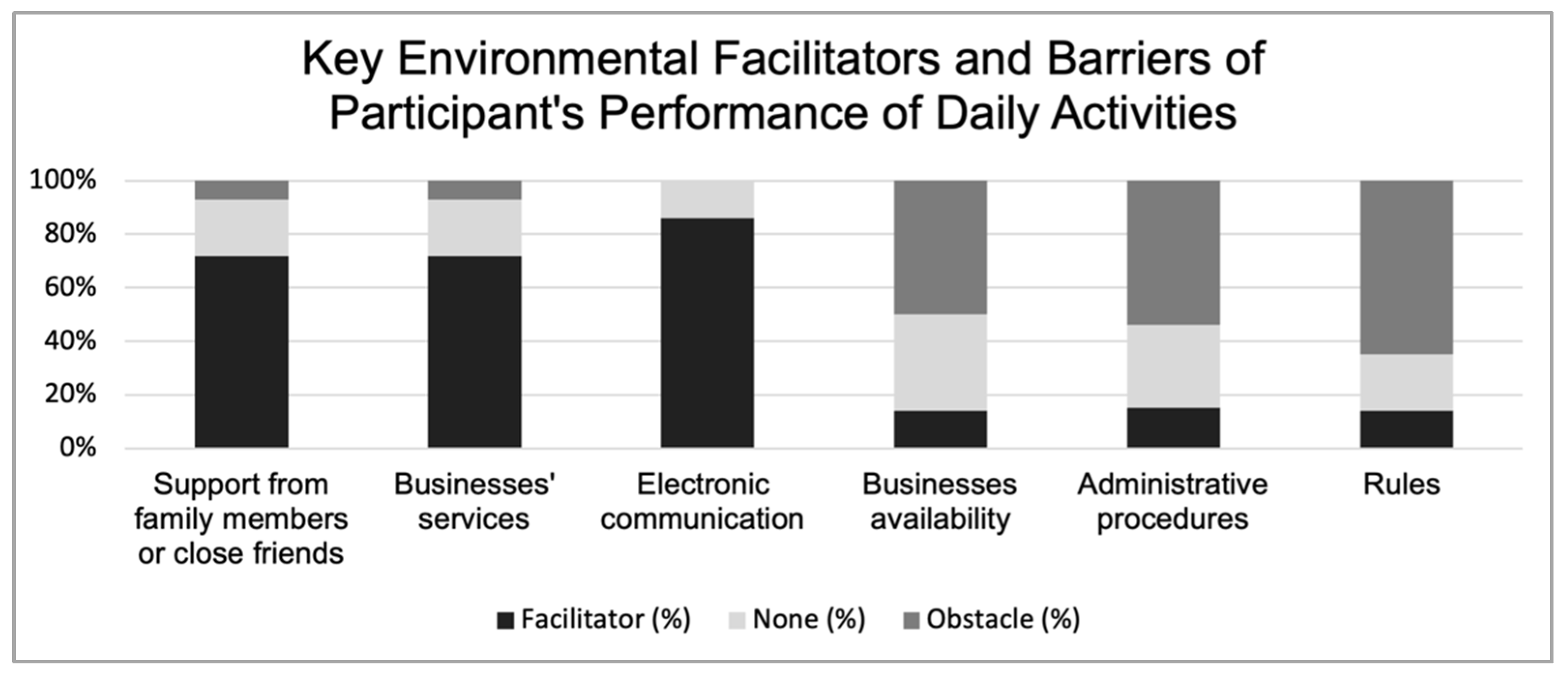
3.3.2. Quality of the Social and Physical Environment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Disability Considerations during the COVID-19 Outbreak; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Munster, V.J.; Koopmans, M.; van Doremalen, N.; van Riel, D.; de Wit, E. A Novel Coronavirus Emerging in China—Key Questions for Impact Assessment. N. Engl. J. Med. 2020, 382, 692–694. [Google Scholar] [CrossRef] [PubMed]
- El-Zoghby, S.M.; Soltan, E.M.; Salama, H.M. Impact of the COVID-19 Pandemic on Mental Health and Social Support among Adult Egyptians. J. Community Health 2020, 45, 689–695. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized Anxiety Disorder, Depressive Symptoms and Sleep Quality During COVID-19 Outbreak in China: A Web-Based Cross-Sectional Survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and Associated Psychological Problems. Asian J. Psychiatr. 2020, 51, 102092. [Google Scholar] [CrossRef] [PubMed]
- Madani, A.; Boutebal, S.E.; Bryant, C.R. The Psychological Impact of Confinement Linked to the Coronavirus Epidemic COVID-19 in Algeria. Int. J. Environ. Res. Public Health 2020, 17, 3604. [Google Scholar] [CrossRef] [PubMed]
- Constant, A.; Conserve, D.F.; Gallopel-Morvan, K.; Raude, J. Socio-Cognitive Factors Associated with Lifestyle Changes in Response to the COVID-19 Epidemic in the General Population: Results from a Cross-Sectional Study in France. Front. Psychol. 2020, 11, 579460. [Google Scholar] [CrossRef] [PubMed]
- Kocevska, D.; Blanken, T.F.; van Someren, E.J.W.; Rosler, L. Sleep Quality During the COVID-19 Pandemic: Not One Size Fits All. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef] [PubMed]
- International Network on the Disability Creation Process. The Human Development Model—Disability Creation Process—Key Concepts. 2021. Available online: https://ripph.qc.ca/en/hdm-dcp-model/key-concepts/ (accessed on 10 January 2021).
- Barker, R.N.; Kendall, M.D.; Amsters, D.I.; Pershouse, K.J.; Haines, T.P.; Kuipers, P. The Relationship between Quality of Life and Disability across the Lifespan for People with Spinal Cord Injury. Spinal Cord 2009, 47, 149–155. [Google Scholar] [CrossRef] [Green Version]
- Carpenter, C.; Forwell, S.J.; Jongbloed, L.E.; Backman, C.L. Community Participation after Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2007, 88, 427–433. [Google Scholar] [CrossRef]
- Cimino, S.R.; Hitzig, S.L.; Craven, B.C.; Bassett-Gunter, R.L.; Li, J.; Guilcher, S.J.T. An Exploration of Perceived Social Isolation among Persons with Spinal Cord Injury in Ontario, Canada: A Qualitative Study. Disabil. Rehabil. 2020, 1–10. [Google Scholar] [CrossRef]
- Guilcher, S.J.T.; Craven, B.C.; Bassett-Gunter, R.L.; Cimino, S.R.; Hitzig, S.L. An Examination of Objective Social Disconnectedness and Perceived Social Isolation among Persons with Spinal Cord Injury/Dysfunction: A Descriptive Cross-Sectional Study. Disabil. Rehabil. 2021, 43, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Dijkers, M.P. Quality of Life of Individuals with Spinal Cord Injury: A Review of Conceptualization, Measurement, and Research Findings. J. Rehabil. Res. Dev. 2005, 42 (Suppl. 1), 87–110. [Google Scholar] [CrossRef] [PubMed]
- Lebrasseur, A.; Fortin-Bedard, N.; Lettre, J.; Bussieres, E.L.; Best, K.; Boucher, N.; Hotton, M.; Beaulieu-Bonneau, S.; Mercier, C.; Lamontagne, M.E.; et al. Impact of COVID-19 on People with Physical Disabilities: A Rapid Review. Disabil. Health J. 2021, 14, 101014. [Google Scholar] [CrossRef]
- de Sousa, D.A.; van der Worp, H.B.; Caso, V.; Cordonnier, C.; Strbian, D.; Ntaios, G.; Schellinger, P.D.; Sandset, E.C.; Organisation European Stroke. Maintaining Stroke Care in Europe During the COVID-19 Pandemic: Results from an International Survey of Stroke Professionals and Practice Recommendations from the European Stroke Organisation. Eur. Stroke J. 2020, 5, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Piano, C.; di Stasio, E.; Primiano, G.; Janiri, D.; Luigetti, M.; Frisullo, G.; Vollono, C.; Lucchini, M.; Brunetti, V.; Monforte, M.; et al. An Italian Neurology Outpatient Clinic Facing Sars-Cov-2 Pandemic: Data from 2167 Patients. Front. Neurol. 2020, 11, 564. [Google Scholar] [CrossRef]
- Zhao, J.; Li, H.; Kung, D.; Fisher, M.; Shen, Y.; Liu, R. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke 2020, 51, 1996–2001. [Google Scholar] [CrossRef]
- Capozzo, R.; Zoccolella, S.; Musio, M.; Barone, R.; Accogli, M.; Logroscino, G. Telemedicine Is a Useful Tool to Deliver Care to Patients with Amyotrophic Lateral Sclerosis During COVID-19 Pandemic: Results from Southern Italy. Amyotroph Lateral Scler Front. Degener 2020, 21, 542–548. [Google Scholar] [CrossRef]
- Radulovic, L.; Erakovic, J.; Roganovic, M. Attitudes of Patients with Relapsing-Remitting Form of Multiple Sclerosis Using Disease-Modifying Drugs in Montenegro Regarding COVID-19 Pandemic. Mult. Scler. Relat. Disord. 2020, 45, 102380. [Google Scholar] [CrossRef]
- Stojanov, A.; Malobabic, M.; Milosevic, V.; Stojanov, J.; Vojinovic, S.; Stanojevic, G.; Stevic, M. Psychological Status of Patients with Relapsing-Remitting Multiple Sclerosis During Coronavirus Disease-2019 Outbreak. Mult. Scler. Relat. Disord. 2020, 45, 102407. [Google Scholar] [CrossRef]
- Di Stefano, V.; Battaglia, G.; Giustino, V.; Gagliardo, A.; D’Aleo, M.; Giannini, O.; Palma, A.; Brighina, F. Significant Reduction of Physical Activity in Patients with Neuromuscular Disease During COVID-19 Pandemic: The Long-Term Consequences of Quarantine. J. Neurol. 2021, 268, 20–26. [Google Scholar] [CrossRef]
- Lopez-Sanchez, G.F.; Lopez-Bueno, R.; Gil-Salmeron, A.; Zauder, R.; Skalska, M.; Jastrzebska, J.; Jastrzebski, Z.; Schuch, F.B.; Grabovac, I.; Tully, M.A.; et al. Comparison of Physical Activity Levels in Spanish Adults with Chronic Conditions before and During COVID-19 Quarantine. Eur. J. Public Health 2021, 31, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Capuano, R.; Altieri, M.; Bisecco, A.; d’Ambrosio, A.; Docimo, R.; Buonanno, D.; Matrone, F.; Giuliano, F.; Tedeschi, G.; Santangelo, G.; et al. Psychological Consequences of COVID-19 Pandemic in Italian Ms Patients: Signs of Resilience? J. Neurol. 2021, 268, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.B.; Groomes, T.E. Incidence of Respiratory Complications Following Spinal Cord Injury. Arch. Phys. Med. Rehabil. 1994, 75, 270–275. [Google Scholar] [CrossRef]
- Whiteneck, G.; Meade, M.A.; Dijkers, M.; Tate, D.G.; Bushnik, T.; Forchheimer, M.B. Environmental Factors and Their Role in Participation and Life Satisfaction after Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2004, 85, 1793–1803. [Google Scholar] [CrossRef]
- Kennedy, P.; Rogers, B.A. Anxiety and Depression after Spinal Cord Injury: A Longitudinal Analysis. Arch. Phys. Med. Rehabil. 2000, 81, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. Whatever Happened to Qualitative Description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Best, K.L.; Routhier, F.; Sweet, S.N.; Arbour-Nicitopoulos, K.P.; Borisoff, J.F.; Noreau, L.; Ginis, K.A.M. The Smartphone Peer Physical Activity Counseling (Sppac) Program for Manual Wheelchair Users: Protocol of a Pilot Randomized Controlled Trial. JMIR Res. Protoc. 2017, 6, e69. [Google Scholar] [CrossRef] [Green Version]
- Martin Ginis, K.A.; van der Scheer, J.W.; Latimer-Cheung, A.E.; Barrow, A.; Bourne, C.; Carruthers, P.; Bernardi, M.; Ditor, D.S.; Gaudet, S.; de Groot, S.; et al. Evidence-Based Scientific Exercise Guidelines for Adults with Spinal Cord Injury: An Update and a New Guideline. Spinal Cord 2018, 56, 308–321. [Google Scholar] [CrossRef] [Green Version]
- Institut National de Santé Publique du Québec. Ligne du Temps COVID-19 au Québec. Available online: https://www.inspq.qc.ca/Covid-19/donnees/ligne-du-temps (accessed on 31 May 2021).
- Control, BC Centre for Disease. Bc COVID-19 Data. Available online: http://www.bccdc.ca/health-info/diseases-conditions/Covid-19/data#Covid-19Dashboard (accessed on 31 May 2021).
- Fougeyrollas, P.; Noreau, L. La Mesure des Habitudes de Vie (Life-H 4.0): Guide D’utilisation, Version Pour Adolescents, Adultes Et Aînés; Réseau International sur le Processus de Production du Handicap: Quebec City, QC, Canada, 2014. [Google Scholar]
- Fougeyrollas, P.; Noreau, L.; St Michel, G.; Boschen, K. Mesure de la Qualité de L’environnement, (Mqe), Version 2.0; RIPPH: Québec, QC, Canada, 2008. [Google Scholar]
- Fereday, J.; Muir-Cochrane, E. Demonstrating Rigor Using Thematic Analysis: A Hybrid Approach of Inductive and Deductive Coding and Theme Development. Int. J. Qual. Methods 2006, 5, 80–92. [Google Scholar] [CrossRef]
- Roberts, K.; Dowell, A.; Nie, J.-B. Attempting Rigour and Replicability in Thematic Analysis of Qualitative Research Data; a Case Study of Codebook Development. BMC Med. Res. Methodol. 2019, 19, 66. [Google Scholar] [CrossRef] [Green Version]
- Nowell, L.; Jill, S.; Norris, M.; White, D.E.; Moules, J. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Robinson-Whelen, S.; Taylor, H.B.; Feltz, M.; Whelen, M. Loneliness among People with Spinal Cord Injury: Exploring the Psychometric Properties of the 3-Item Loneliness Scale. Arch. Phys. Med. Rehabil. 2016, 97, 1728–1734. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.H.; Liu, C.H.; Hung, H.P. An in-Depth Understanding of the Impact of the Environment on Participation among People with Spinal Cord Injury. Disabil. Rehabil. 2018, 40, 2192–2199. [Google Scholar] [CrossRef] [PubMed]
- Monden, K.R.; Trost, Z.; Catalano, D.; Garner, A.N.; Symcox, J.; Driver, S.; Hamilton, R.G.; Warren, A.M. Resilience Following Spinal Cord Injury: A Phenomenological View. Spinal Cord 2014, 52, 197–201. [Google Scholar] [CrossRef] [Green Version]
- Muller, R.; Peter, C.; Cieza, A.; Geyh, S. The Role of Social Support and Social Skills in People with Spinal Cord Injury—A Systematic Review of the Literature. Spinal Cord 2012, 50, 94–106. [Google Scholar] [CrossRef] [Green Version]
- Cardol, M.; de Jong, B.A.; Ward, C.D. On Autonomy and Participation in Rehabilitation. Disabil. Rehabil. 2002, 24, 970–974. [Google Scholar] [CrossRef]
- Stillman, M.D.; Capron, M.; Alexander, M.; di Giusto, M.L.; Scivoletto, G. COVID-19 and Spinal Cord Injury and Disease: Results of an International Survey. Spinal Cord Ser. Cases 2020, 6, 21. [Google Scholar] [CrossRef] [Green Version]
- Babamohamadi, H.; Negarandeh, R.; Dehghan-Nayeri, N. Coping Strategies Used by People with Spinal Cord Injury: A Qualitative Study. Spinal Cord 2011, 49, 832–837. [Google Scholar] [CrossRef] [Green Version]
- Migliorini, C.; Tonge, B.; Taleporos, G. Spinal Cord Injury and Mental Health. Aust. N. Z. J. Psychiatry 2008, 42, 309–314. [Google Scholar] [CrossRef]
- Kehn, M.; Kroll, T. Staying Physically Active after Spinal Cord Injury: A Qualitative Exploration of Barriers and Facilitators to Exercise Participation. BMC Public Health 2009, 9, 168. [Google Scholar] [CrossRef] [Green Version]
- Jick, T. Mixing Qualitative and Quantitative Methods: Triangulation in Action. Adm. Sci. Q. 1979, 24, 602. [Google Scholar] [CrossRef] [Green Version]
| Participant Number | Sex | Age, Years | Province of Origin 1 | Employment Status | Highest Education Level | Annual Household Income, $ | Diagnosis | Time Using any WC 2, Years |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 30–39 | BC | Employed | College/University | <30,000 | Transverse myelitis | 6–10 |
| 2 | F | 30–39 | BC | Unemployed | Post Graduate studies | <30,000 | Paraplegia | 21–25 |
| 3 | M | 70–79 | BC | Retired | Post Graduate studies | ≥60,000 | Paraplegia | 41–45 |
| 4 | M | 30–39 | BC | Employed | College/University | <30,000 | Paraplegia | 6–10 |
| 5 | M | 20–29 | QC | Unemployed | High school or no diploma | 30,000–59,999 | Paraplegia | 0–5 |
| 6 | F | 50–59 | QC | Unemployed | College/University | 30,000–59,999 | Paraplegia | 11–15 |
| 7 | M | 30–39 | QC | Unemployed | Other | 30,000–59,999 | Paraplegia | 0–5 |
| 8 | F | 60–69 | QC | Retired | College/University | ≥60,000 | Paraplegia | 41–45 |
| 9 | F | 20–29 | QC | Unemployed | College/University | <30,000 | Paraplegia | 0–5 |
| 10 | M | 60–69 | QC | Retired | High school or no diploma | <30,000 | Paraplegia | 11–15 |
| 11 | M | 40–49 | QC | Unemployed | High school or no diploma | <30,000 | Tetraplegia | 6–10 |
| 12 | M | 50–59 | QC | Retired | College/University | 30,000–59,999 | Paraplegia | 0–5 |
| 13 | M | 40–49 | QC | Retired | High school or no diploma | 30,000–59,999 | Paraplegia | 16–20 |
| 14 | F | 50–59 | QC | Unemployed | College/University (started) | Missing | Paraplegia | 0–5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fortin-Bédard, N.; de Serres-Lafontaine, A.; Best, K.L.; Rahn, C.; Turcotte, E.; Borisoff, J.; Sweet, S.N.; Arbour-Nicitopoulos, K.P.; Routhier, F. Experiences of Social Participation for Canadian Wheelchair Users with Spinal Cord Injury during the First Wave of the COVID-19 Pandemic. Disabilities 2022, 2, 398-414. https://doi.org/10.3390/disabilities2030028
Fortin-Bédard N, de Serres-Lafontaine A, Best KL, Rahn C, Turcotte E, Borisoff J, Sweet SN, Arbour-Nicitopoulos KP, Routhier F. Experiences of Social Participation for Canadian Wheelchair Users with Spinal Cord Injury during the First Wave of the COVID-19 Pandemic. Disabilities. 2022; 2(3):398-414. https://doi.org/10.3390/disabilities2030028
Chicago/Turabian StyleFortin-Bédard, Noémie, Annabelle de Serres-Lafontaine, Krista L. Best, Caroline Rahn, Elizabeth Turcotte, Jaimie Borisoff, Shane N. Sweet, Kelly P. Arbour-Nicitopoulos, and François Routhier. 2022. "Experiences of Social Participation for Canadian Wheelchair Users with Spinal Cord Injury during the First Wave of the COVID-19 Pandemic" Disabilities 2, no. 3: 398-414. https://doi.org/10.3390/disabilities2030028
APA StyleFortin-Bédard, N., de Serres-Lafontaine, A., Best, K. L., Rahn, C., Turcotte, E., Borisoff, J., Sweet, S. N., Arbour-Nicitopoulos, K. P., & Routhier, F. (2022). Experiences of Social Participation for Canadian Wheelchair Users with Spinal Cord Injury during the First Wave of the COVID-19 Pandemic. Disabilities, 2(3), 398-414. https://doi.org/10.3390/disabilities2030028








