Biomechanics and Performance of Single-Leg Vertical and Horizontal Hop in Adolescents Post-Anterior Cruciate Ligament Reconstruction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Protocol
2.3. Data Analysis
3. Results
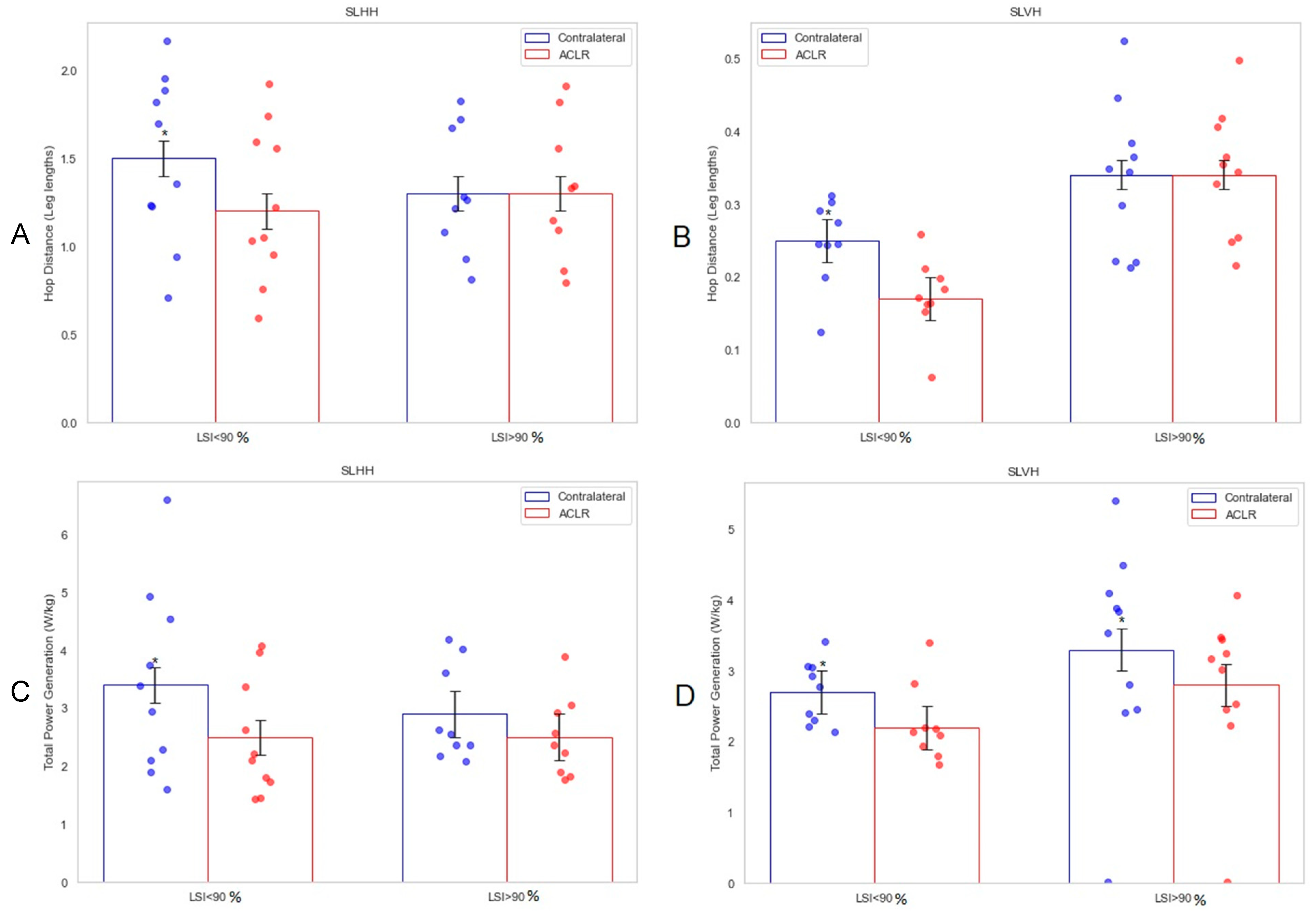
3.1. Performance and LSI
3.2. Takeoff
3.3. Landing
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Burgi, C.R.; Peters, S.; Ardern, C.L.; Magill, J.R.; Gomez, C.D.; Sylvain, J.; Reiman, M.P. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br. J. Sports Med. 2019, 53, 1154–1161. [Google Scholar] [CrossRef] [PubMed]
- Matsuzaki, Y.; Chipman, D.E.; Perea, S.H.; Green, D.W. Unique Considerations for the Pediatric Athlete During Rehabilitation and Return to Sport After Anterior Cruciate Ligament Reconstruction. Arthrosc. Sports Med. Rehabil. 2022, 4, e221–e230. [Google Scholar] [CrossRef]
- Korakakis, V.; Kotsifaki, A.; Korakaki, A.; Karanasios, S.; Whiteley, R. Current perspectives and clinical practice of physiotherapists on assessment, rehabilitation, and return to sport criteria after anterior cruciate ligament injury and reconstruction. An online survey of 538 physiotherapists. Phys. Ther. Sport 2021, 52, 103–114. [Google Scholar] [CrossRef]
- Grindem, H.; Snyder-Mackler, L.; Moksnes, H.; Engebretsen, L.; Risberg, M.A. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: The Delaware-Oslo ACL cohort study. Br. J. Sports Med. 2016, 50, 804–808. [Google Scholar] [CrossRef]
- Beischer, S.; Gustavsson, L.; Senorski, E.H.; Karlsson, J.; Thomeé, C.; Samuelsson, K.; Thomeé, R. Young Athletes Who Return to Sport Before 9 Months After Anterior Cruciate Ligament Reconstruction Have a Rate of New Injury 7 Times That of Those Who Delay Return. J. Orthop. Sports Phys. Ther. 2020, 50, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Ekås, G.; Grindem, H.; Moksnes, H.; Anderson, A.; Chotel, F.; Cohen, M.; Forssblad, M.; Ganley, T.J.; Feller, J.A.; et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 989–1010. [Google Scholar] [CrossRef]
- Nagelli, C.V.; Hewett, T.E. Should Return to Sport be Delayed Until 2 Years After Anterior Cruciate Ligament Reconstruction? Biological and Functional Considerations. Sports Med. 2016, 47, 221–232. [Google Scholar] [CrossRef]
- Nagai, T.; Schilaty, N.D.; Laskowski, E.R.; Hewett, T.E. Hop tests can result in higher limb symmetry index values than isokinetic strength and leg press tests in patients following ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2019, 28, 816–822. [Google Scholar] [CrossRef]
- Wren, T.A.L.; Mueske, N.M.; Brophy, C.H.; Pace, J.L.; Katzel, M.J.; Edison, B.R.; Vandenberg, C.D.; Zaslow, T.L. Hop Distance Symmetry Does Not Indicate Normal Landing Biomechanics in Adolescent Athletes With Recent Anterior Cruciate Ligament Reconstruction. J. Orthop. Sports Phys. Ther. 2018, 48, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Sueyoshi, T.; Nakahata, A.; Emoto, G.; Yuasa, T. Single-Leg Hop Test Performance and Isokinetic Knee Strength After Anterior Cruciate Ligament Reconstruction in Athletes. Orthop. J. Sports Med. 2017, 5, 2325967117739811. [Google Scholar] [CrossRef] [PubMed]
- Capin, J.J.; Snyder-Mackler, L.; Risberg, M.A.; Grindem, H. Keep calm and carry on testing: A substantive reanalysis and critique of ‘what is the evidence for and validity of return-to-sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis’. Br. J. Sports Med. 2019, 53, 1444–1446. [Google Scholar] [CrossRef]
- Roe, C.; Jacobs, C.; Hoch, J.; Johnson, D.L.; Noehren, B. Test Batteries After Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review. Sports Health 2021, 14, 205–215. [Google Scholar] [CrossRef] [PubMed]
- Astur, D.C.; Cachoeira, C.M.; Vieira, T.d.S.; Debieux, P.; Kaleka, C.C.; Cohen, M. Increased incidence of anterior cruciate ligament revision surgery in paediatric verses adult population. Knee Surg. Sports Traumatol. Arthrosc. 2017, 26, 1362–1366. [Google Scholar] [CrossRef] [PubMed]
- Snaebjörnsson, T.; Senorski, E.H.; Sundemo, D.; Svantesson, E.; Westin, O.; Musahl, V.; Alentorn-Geli, E.; Samuelsson, K. Adolescents and female patients are at increased risk for contralateral anterior cruciate ligament reconstruction: A cohort study from the Swedish National Knee Ligament Register based on 17,682 patients. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3938–3944. [Google Scholar] [CrossRef]
- Barber-Westin, S.; Noyes, F.R. One in 5 Athletes Sustain Reinjury Upon Return to High-Risk Sports After ACL Reconstruction: A Systematic Review in 1239 Athletes Younger Than 20 Years. Sports Health 2020, 12, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Boykin, R.E.; McFeely, E.D.; Shearer, D.; Frank, J.S.; Harrod, C.C.; Nasreddine, A.Y.; Kocher, M.S. Correlation Between the Child Health Questionnaire and the International Knee Documentation Committee Score in Pediatric and Adolescent Patients With an Anterior Cruciate Ligament Tear. J. Pediatr. Orthop. 2013, 33, 216–220. [Google Scholar] [CrossRef]
- Romanchuk, N.J.; Livock, H.; Lukas, K.J.; Del Bel, M.J.; Benoit, D.L.; Carsen, S. Criteria Used to Determine Unrestricted Return to Activity After ACL Reconstruction in Pediatric and Adolescent Patients: A Systematic Review. Orthop. J. Sports Med. 2023, 11, 23259671231154540. [Google Scholar] [CrossRef]
- van Melick, N.; van Cingel, R.E.H.; Brooijmans, F.; Neeter, C.; van Tienen, T.; Hullegie, W.; Nijhuis-van der Sanden, M.W.G. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br. J. Sports Med. 2016, 50, 1506–1515. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Wang, L.; Dong, S.; Ding, Y.; Zuo, H.; Jia, S.; Wang, G.; Chen, C.; Zheng, C. Abnormal Lower Limb Biomechanics During a Bilateral Vertical Jump Despite the Symmetry in Single-Leg Vertical Hop Height in Athletes after ACL Reconstruction. Orthop. J. Sports Med. 2024, 12, 23259671241230989. [Google Scholar] [CrossRef]
- Benjaminse, A.; Holden, S.; Myer, G.D. Acl rupture is a single leg injury but a double leg problem: Too much focus on ‘symmetry’ alone and that’s not enough! Br. J. Sports Med. 2018, 53, 993–995. [Google Scholar] [CrossRef]
- Wellsandt, E.; Failla, M.J.; Snyder-Mackler, L. Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury. J. Orthop. Sports Phys. Ther. 2017, 47, 334–338. [Google Scholar] [CrossRef]
- Fischer, F.; Blank, C.; Dünnwald, T.; Gföller, P.; Herbst, E.; Hoser, C.; Fink, C. Isokinetic Extension Strength Is Associated With Single-Leg Vertical Jump Height. Orthop. J. Sports Med. 2017, 5, 2325967117736766. [Google Scholar] [CrossRef]
- Kotsifaki, A.; Korakakis, V.; Graham-Smith, P.; Sideris, V.; Whiteley, R. Vertical and Horizontal Hop Performance: Contributions of the Hip, Knee, and Ankle. Sports Health 2021, 13, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Wren, T.A.L.; O’callahan, B.; Katzel, M.J.; Zaslow, T.L.; Edison, B.R.; VandenBerg, C.D.; Conrad-Forrest, A.; Mueske, N.M. Movement variability in pre-teen and teenage athletes performing sports related tasks. Gait Posture 2020, 80, 228–233. [Google Scholar] [CrossRef]
- Kotsifaki, A.; Van Rossom, S.; Whiteley, R.; Korakakis, V.; Bahr, R.; Sideris, V.; Smith, P.G.; Jonkers, I. Symmetry in Triple Hop Distance Hides Asymmetries in Knee Function After ACL Reconstruction in Athletes at Return to Sports. Am. J. Sports Med. 2021, 50, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Hughes, G.; Musco, P.; Caine, S.; Howe, L. Lower Limb Asymmetry After Anterior Cruciate Ligament Reconstruction in Adolescent Athletes: A Systematic Review and Meta-Analysis. J. Athl. Train. 2020, 55, 811–825. [Google Scholar] [CrossRef] [PubMed]
- Leppänen, M.; Pasanen, K.; Kujala, U.M.; Vasankari, T.; Kannus, P.; Äyrämö, S.; Krosshaug, T.; Bahr, R.; Avela, J.; Perttunen, J.; et al. Stiff Landings Are Associated With Increased ACL Injury Risk in Young Female Basketball and Floorball Players. Am. J. Sports Med. 2016, 45, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Zarro, M.J.; Stitzlein, M.G.; Lee, J.S.; Rowland, R.W.; Gray, V.L.; Taylor, J.B.; Meredith, S.J.; Packer, J.D.; Nelson, C.M. Single-Leg Vertical Hop Test Detects Greater Limb Asymmetries Than Horizontal Hop Tests After Anterior Cruciate Ligament Reconstruction in NCAA Division 1 Collegiate Athletes. Int. J. Sports Phys. Ther. 2021, 16, 1405–1414. [Google Scholar] [CrossRef]
- Taylor, J.B.; Westbrook, A.E.; Head, P.L.; Glover, K.M.; Paquette, M.R.; Ford, K.R. The single-leg vertical hop provides unique asymmetry information in individuals after anterior cruciate ligament reconstruction. Clin. Biomech. 2020, 80, 105107. [Google Scholar] [CrossRef] [PubMed]
- Pratt, K.A.; Sigward, S.M. Knee Loading Deficits During Dynamic Tasks in Individuals Following Anterior Cruciate Ligament Reconstruction. J. Orthop. Sports Phys. Ther. 2017, 47, 411–419. [Google Scholar] [CrossRef] [PubMed]
- Sigward, S.M.; Chan, M.-S.M.; Lin, P.E.; Almansouri, S.Y.; Pratt, K.A. Compensatory Strategies That Reduce Knee Extensor Demand During a Bilateral Squat Change From 3 to 5 Months Following Anterior Cruciate Ligament Reconstruction. J. Orthop. Sports Phys. Ther. 2018, 48, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Larwa, J.; Stoy, C.; Chafetz, R.S.; Boniello, M.; Franklin, C. Stiff Landings, Core Stability, and Dynamic Knee Valgus: A Systematic Review on Documented Anterior Cruciate Ligament Ruptures in Male and Female Athletes. Int. J. Environ. Res. Public Health 2021, 18, 3826. [Google Scholar] [CrossRef] [PubMed]
- Abrams, G.D.; Harris, J.D.; Gupta, A.K.; McCormick, F.M.; Bush-Joseph, C.A.; Verma, N.N.; Cole, B.J.; Bach, B.R. Functional Performance Testing After Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2014, 2, 2325967113518305. [Google Scholar] [CrossRef] [PubMed]
| Takeoff | SLHH | SLVH | ||||
|---|---|---|---|---|---|---|
| Contralateral | ACLR | p | Contralateral | ACLR | p | |
| Hop distance or height (leg lengths) | 1.41 (0.1) | 1.28 (0.1) | 0.005 | 0.30 (0.02) | 0.26 (0.02) | 0.01 |
| Kinematics | ||||||
| Max ankle dorsiflexion [deg] | 29.9 (1.3) | 26.7 (1.3) | 0.01 | 24.7 (1.4) | 20.6 (1.4) | 0.001 |
| Max knee flexion [deg] | 60.2 (2.4) | 51.2 (2.4) | <0.001 | 63.3 (2.1) | 54.8 (2.1) | <0.001 |
| Max hip flexion [deg] | 61.2 (2.7) | 56.2 (2.7) | 0.02 | 61.0 (2.6) | 58.3 (2.6) | 0.18 |
| Moments | ||||||
| Max ankle dorsiflexion moment [N·m/kg] | 3.1 (0.3) | 3.0 (0.3) | 0.41 | 2.0 (0.1) | 2.0 (0.1) | 0.93 |
| Max knee flexion moment [N·m/kg] | 2.0 (0.2) | 1.2 (0.2) | 0.001 | 2.1 (0.2) | 1.5 (0.2) | <0.001 |
| Max hip flexion moment [N·m/kg] | 2.8 (0.4) | 2.8 (0.4) | 0.73 | 2.0 (0.2) | 2.1 (0.2) | 0.20 |
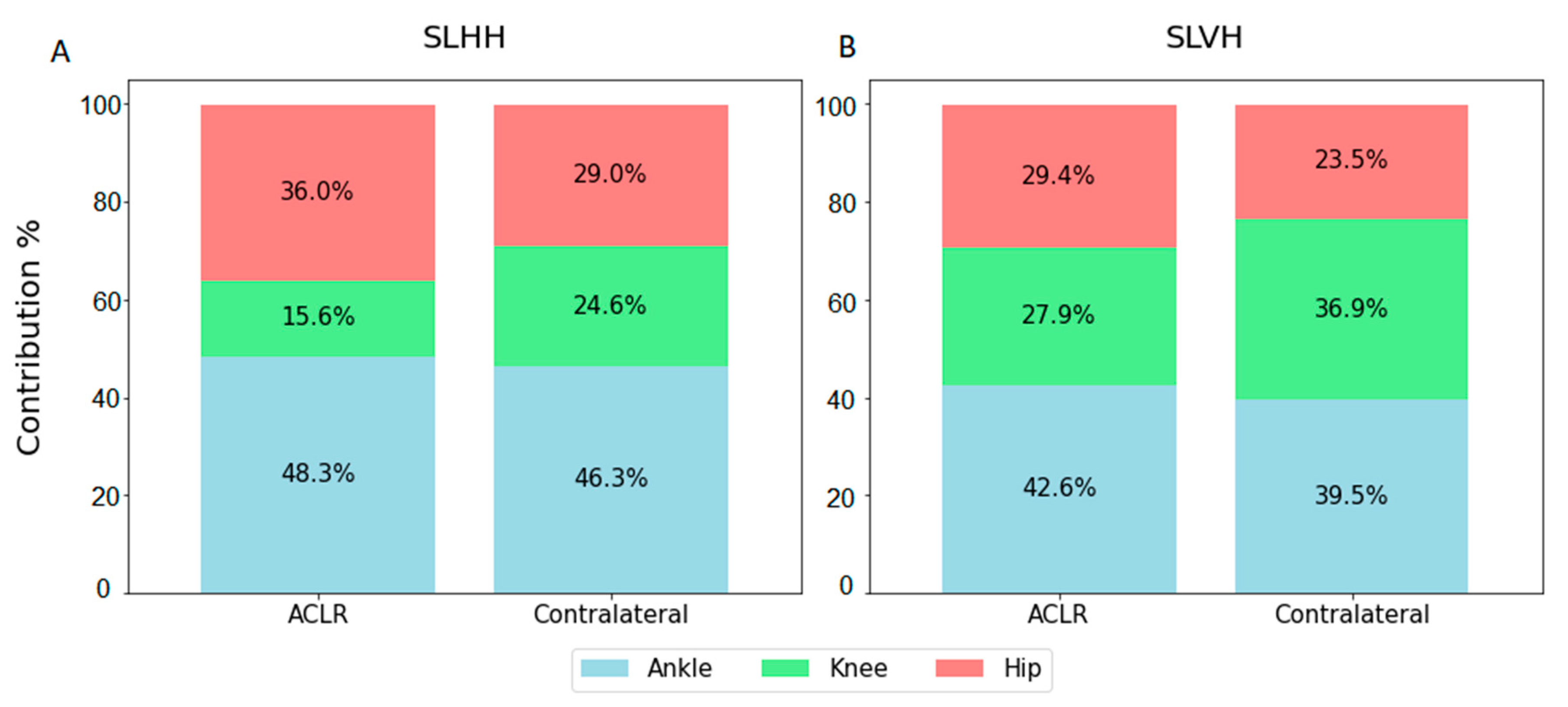
| Power | ||||||
| Total generation [W/kg] | 3.2 (0.2) | 2.5 (0.2) | 0.001 | 3.0 (0.2) | 2.5 (0.2) | 0.002 |
| % ankle | 46.3 (1.8) | 48.3 (1.8) | 0.15 | 39.5 (2.7) | 42.6 (2.7) | 0.04 |
| % knee | 24.6 (1.7) | 15.6 (1.7) | 0.001 | 36.9 (1.9) | 27.9 (1.9) | 0.001 |
| % hip | 29.0 (2.2) | 36.0 (2.2) | 0.005 | 23.5 (2.5) | 29.4 (2.5) | 0.02 |
| SLHH | LSI < 90% | LSI ≥ 90% | ||||
|---|---|---|---|---|---|---|
| Contralateral | ACLR | p | Contralateral | ACLR | p | |
| Hop Distance (leg lengths) | 1.5 (0.1) | 1.2 (0.1) | <0.001 | 1.3 (0.1) | 1.3 (0.1) | 0.89 |
| TAKEOFF | ||||||
| Max ankle dorsiflexion [deg] | 30.8 (1.8) | 25.8 (1.8) | 0.001 | 28.9 (1.9) | 27.6 (1.9) | 0.41 |
| Max knee flexion [deg] | 62.0 (3.3) | 50.8 (3.3) | <0.001 | 58.2 (3.5) | 51.6 (3.5) | 0.03 |
| Max hip flexion [deg] | 64.8 (3.7) | 59.2 (3.7) | 0.04 | 57.1 (3.9) | 52.9 (3.9) | 0.16 |
| Max ankle dorsiflexion moment [N·m/kg] | 3.1 (0.5) | 3.0 (0.5) | 0.09 | 3.0 (0.5) | 3.1 (0.5) | 0.62 |
| Max knee flexion moment [N·m/kg] | 2.1 (0.3) | 1.1 (0.3) | 0.001 | 2.0 (0.3) | 1.3 (0.3) | 0.03 |
| Max hip flexion moment [N·m/kg] | 3.0 (0.6) | 3.1 (0.6) | 0.84 | 2.5 (0.7) | 2.5 (0.7) | 0.79 |
| Total power generation [W/kg] | 3.4 (0.3) | 2.5 (0.3) | <0.001 | 2.9 (0.4) | 2.5 (0.4) | 0.09 |
| Power generation, % ankle | 44.2 (2.5) | 46.7 (2.5) | 0.18 | 48.7 (2.7) | 50.2 (2.7) | 0.46 |
| Power generation, % knee | 24.5 (2.3) | 13.0 (2.3) | <0.001 | 24.7 (2.4) | 18.5 (2.4) | 0.047 |
| Power generation, % hip | 31.3 (2.8) | 40.3 (2.8) | 0.003 | 26.5 (3.0) | 31.3 (3.0) | 0.14 |
| LANDING | ||||||
| Max ankle dorsiflexion [deg] | 14.5 (2.5) | 10.9 (2.5) | 0.04 | 19.1 (2.6) | 13.9 (2.6) | 0.006 |
| Max knee flexion [deg] | 68.8 (3.7) | 55.8 (3.7) | <0.001 | 73.2 (3.9) | 63.9 (3.9) | 0.001 |
| Max hip flexion [deg] | 76.5 (4.2) | 71.7 (4.2) | 0.13 | 70.9 (4.4) | 68.1 (4.4) | 0.41 |
| Max ankle dorsiflexion moment [N·m/kg] | 1.0 (0.1) | 1.1 (0.1) | 0.28 | 0.9 (0.9) | 1.1 (0.9) | 0.06 |
| Max knee flexion moment [N·m/kg] | 2.6 (0.2) | 1.8 (0.2) | <0.001 | 2.7 (0.2) | 2.1 (0.2) | <0.001 |
| Max hip flexion moment [N·m/kg] | 3.4 (0.4) | 3.0 (0.4) | 0.05 | 2.5 (0.4) | 2.6 (0.4) | 0.63 |
| Total power absorption [W/kg] | 2.8 (0.3) | 1.8 (0.3) | <0.001 | 2.8 (0.3) | 2.3 (0.3) | 0.007 |
| Power absorption, % ankle | 12.0 (1.6) | 20.1 (1.6) | <0.001 | 12.5 (1.7) | 17.4 (1.7) | 0.007 |
| Power absorption, % knee | 57.8 (3.2) | 43.8 (3.2) | <0.001 | 64.9 (3.3) | 51.3 (3.3) | <0.001 |
| Power absorption, % hip | 30.1 (3.0) | 36.1 (3.0) | 0.03 | 22.5 (3.2) | 31.4 (3.2) | 0.002 |
| SLVH | LSI < 90% | LSI ≥ 90% | ||||
|---|---|---|---|---|---|---|
| Contralateral | ACLR | p | Contralateral | ACLR | p | |
| Hop Height (leg lengths) | 0.25 (0.03) | 0.17 (0.03) | <0.001 | 0.34 (0.02) | 0.34 (0.02) | 0.47 |
| TAKEOFF | ||||||
| Max ankle dorsiflexion [deg] | 23.3 (2.1) | 19.4 (2.1) | 0.01 | 25.8 (2.0) | 21.7 (2.0) | 0.006 |
| Max knee flexion [deg] | 61.3 (3.1) | 52.1 (3.1) | 0.001 | 65.1 (2.9) | 57.2 (2.9) | 0.004 |
| Max hip flexion [deg] | 61.5 (3.9) | 61.5 (3.7) | 1.00 | 60.5 (3.7) | 55.5 (3.7) | 0.047 |
| Max ankle dorsiflexion moment [N·m/kg] | 2.0 (0.2) | 1.9 (0.2) | 0.20 | 2.0 (0.2) | 2.1 (0.2) | 0.18 |
| Max knee flexion moment [N·m/kg] | 2.0 (0.2) | 1.3 (0.2) | <0.001 | 2.2 (0.2) | 1.8 (0.2) | 0.002 |
| Max hip flexion moment [N·m/kg] | 1.9 (0.3) | 2.1 (0.3) | 0.049 | 2.1 (0.3) | 2.1 (0.3) | 0.98 |
| Total power generation [W/kg] | 2.7 (0.3) | 2.2 (0.3) | 0.03 | 3.3 (0.3) | 2.8 (0.3) | 0.006 |
| Power generation, % ankle | 42.1 (4.0) | 44.5 (4.0) | 0.25 | 37.2 (3.8) | 40.9 (3.8) | 0.06 |
| Power generation, % knee | 35.5 (2.4) | 21.5 (2.4) | <0.001 | 38.2 (2.2) | 33.7 (2.2) | 0.13 |
| Power generation, % hip | 22.4 (3.5) | 33.9 (3.5) | <0.001 | 24.6 (3.3) | 25.4 (3.3) | 0.77 |
| LANDING | ||||||
| Max ankle dorsiflexion [deg] | 17.5 (1.6) | 11.7 (1.6) | <0.001 | 24.3 (1.5) | 19.2 (1.5) | <0.001 |
| Max knee flexion [deg] | 45.7 (4.3) | 32.7 (4.3) | <0.001 | 60.0 (4.1) | 52.2 (4.1) | <0.001 |
| Max hip flexion [deg] | 42.9 (5.5) | 44.0 (5.5) | 0.75 | 53.2 (5.2) | 51.1 (5.2) | 0.51 |
| Max ankle dorsiflexion moment [N·m/kg] | 1.9 (0.2) | 1.8 (0.2) | 0.41 | 2.2 (0.1) | 2.3 (0.1) | 0.39 |
| Max knee flexion moment [N·m/kg] | 1.9 (0.2) | 0.9 (0.2) | <0.001 | 2.5 (0.2) | 2.0 (0.2) | 0.001 |
| Max hip flexion moment [N·m/kg] | 1.3 (0.2) | 1.2 (0.2) | 0.79 | 1.6 (0.2) | 1.5 (0.2) | 0.45 |
| Total power absorption [W/kg] | 1.7 (0.3) | 1.2 (0.3) | <0.001 | 3.0 (0.3) | 2.4 (0.3) | <0.001 |
| Power absorption, % ankle | 46.4 (5.8) | 58.8 (5.8) | 0.01 | 42.1 (5.5) | 49.7 (5.5) | 0.10 |
| Power absorption, % knee | 37.9 (3.3) | 19.1 (3.3) | <0.001 | 42.2 (3.2) | 33.6 (3.2) | 0.02 |
| Power absorption, % hip | 15.7 (4.4) | 22.1 (4.4) | 0.10 | 15.7 (4.2) | 16.6 (4.2) | 0.79 |
| Landing | SLHH | SLVH | ||||
|---|---|---|---|---|---|---|
| Contralateral | ACLR | p | Contralateral | ACLR | p | |
| Kinematics | ||||||
| Max ankle dorsiflexion (deg) | 16.7 (1.8) | 12.3 (1.8) | 0.003 | 21.1 (1.4) | 15.7 (1.4) | <0.001 |
| Max knee flexion (deg) | 70.9 (2.7) | 59.6 (2.7) | <0.001 | 53.2 (3.5) | 42.9 (3.5) | <0.001 |
| Max hip flexion (deg) | 73.9 (3.0) | 70.0 (3.0) | 0.11 | 48.4 (3.8) | 47.8 (3.8) | 0.79 |
| Moments | ||||||
| Max ankle dorsiflexion moment (N·m/kg) | 4.5 (3.7) | 4.9 (3.7) | 0.16 | 9.6 (6.7) | 7.9 (6.7) | 0.34 |
| Max knee flexion moment (N·m/kg) | 10.8 (6.8) | 7.1 (6.8) | 0.23 | 9.6 (6.1) | 6.0 (6.1) | 0.23 |
| Max hip flexion moment (N·m/kg) | 9.9 (7.4) | 10.7 (7.4) | 0.44 | 7.5 (6.3) | 7.9 (6.3) | 0.47 |
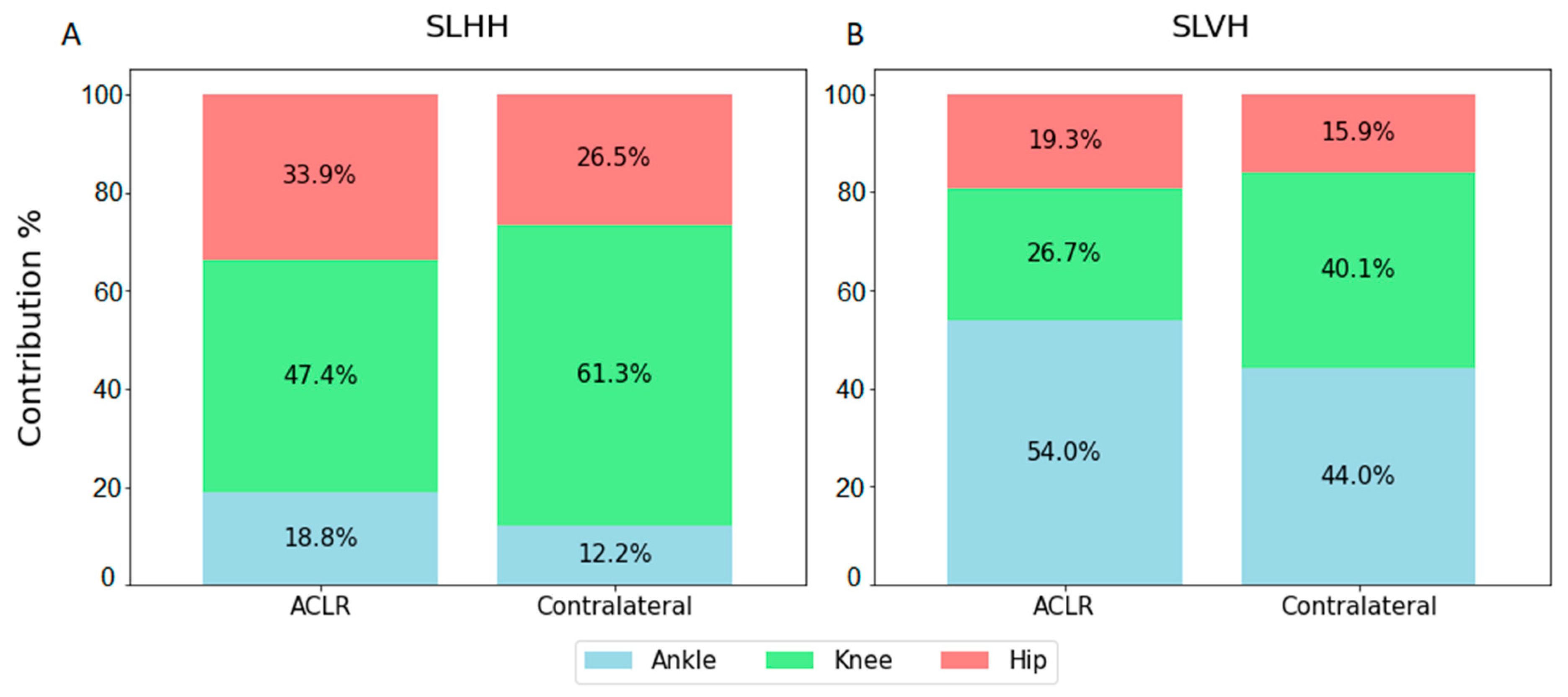
| Power | ||||||
| Total absorption (W/kg) | 11.8 (8.7) | 10.4 (8.7) | 0.04 | 10.4 (7.7) | 9.1 (7.7) | 0.09 |
| % ankle | 12.2 (1.2) | 18.8 (1.2) | <0.001 | 44.0 (4.0) | 53.9 (4.0) | 0.008 |
| % knee | 61.3 (2.4) | 47.4 (2.4) | <0.001 | 40.1 (2.6) | 26.7 (2.6) | <0.001 |
| % hip | 26.5 (2.3) | 33.9 (2.3) | 0.001 | 15.9 (3.0) | 19.3 (3.0) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciccodicola, E.M.; Hanson, A.M.; Roberts, S.E.; Katzel, M.J.; Wren, T.A.L. Biomechanics and Performance of Single-Leg Vertical and Horizontal Hop in Adolescents Post-Anterior Cruciate Ligament Reconstruction. Biomechanics 2025, 5, 5. https://doi.org/10.3390/biomechanics5010005
Ciccodicola EM, Hanson AM, Roberts SE, Katzel MJ, Wren TAL. Biomechanics and Performance of Single-Leg Vertical and Horizontal Hop in Adolescents Post-Anterior Cruciate Ligament Reconstruction. Biomechanics. 2025; 5(1):5. https://doi.org/10.3390/biomechanics5010005
Chicago/Turabian StyleCiccodicola, Eva M., Alison M. Hanson, Shawn E. Roberts, Mia J. Katzel, and Tishya A. L. Wren. 2025. "Biomechanics and Performance of Single-Leg Vertical and Horizontal Hop in Adolescents Post-Anterior Cruciate Ligament Reconstruction" Biomechanics 5, no. 1: 5. https://doi.org/10.3390/biomechanics5010005
APA StyleCiccodicola, E. M., Hanson, A. M., Roberts, S. E., Katzel, M. J., & Wren, T. A. L. (2025). Biomechanics and Performance of Single-Leg Vertical and Horizontal Hop in Adolescents Post-Anterior Cruciate Ligament Reconstruction. Biomechanics, 5(1), 5. https://doi.org/10.3390/biomechanics5010005







