Assessing Balance Loss and Stability Control in Older Adults Exposed to Gait Perturbations under Different Environmental Conditions: A Feasibility Study
Abstract
1. Introduction
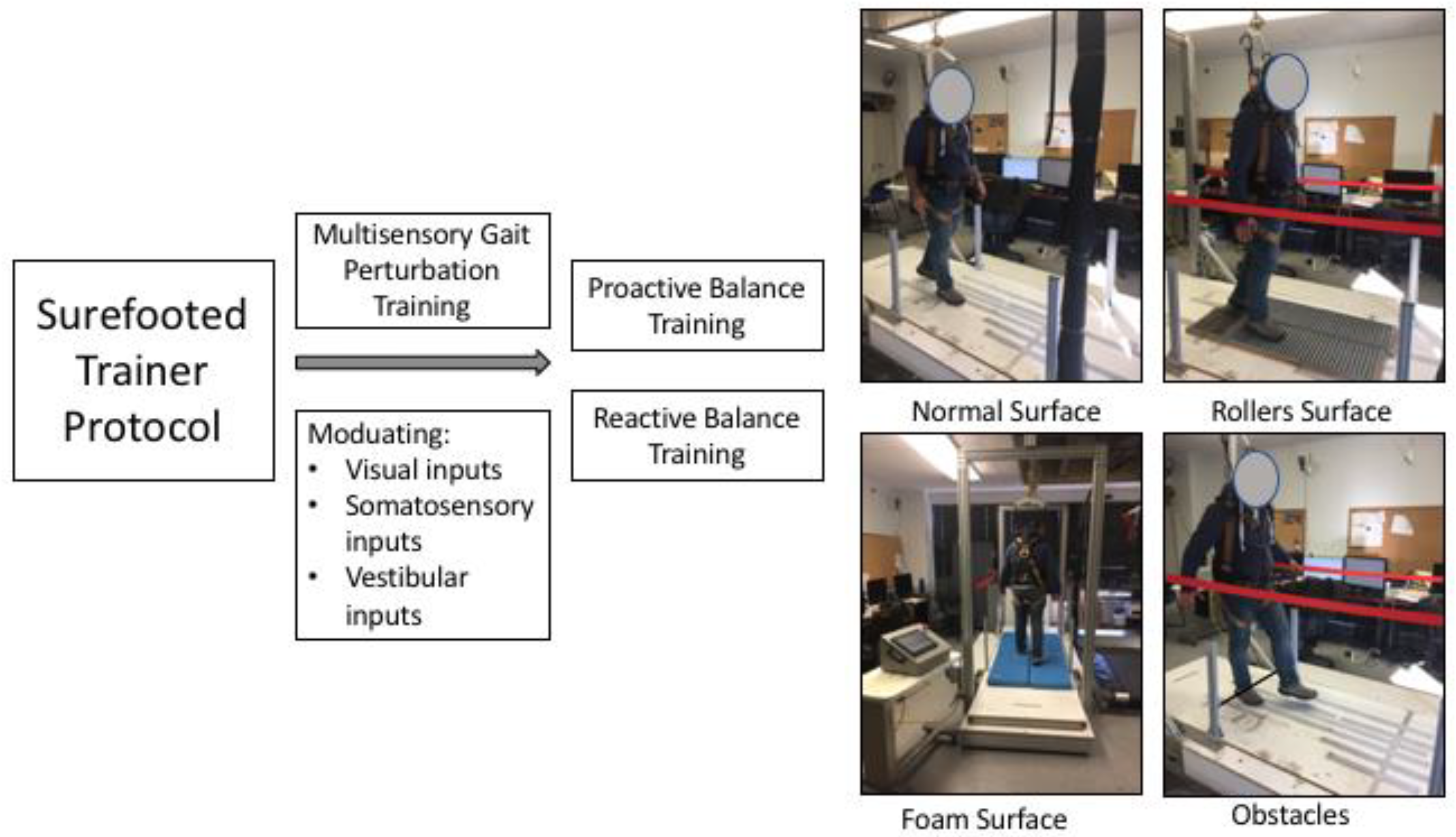
2. Materials and Methods
2.1. Participants
2.2. Computer-Controlled Movable Platform Device
2.3. Experimental Protocol
2.4. Data Collection
2.5. Outcome Measures
2.5.1. Feasibility
2.5.2. Behavioral Results
- Baseline or natural walking trials: trials in which no perturbation was induced;
- Loss of balance;
- No loss of balance.
2.5.3. Validity
Margin of Stability
Trunk Angle
Step Length
2.5.4. Data Synthesis
2.5.5. Statistical Analysis
3. Results
3.1. Feasibility
3.2. Behavioral Outcomes
3.3. Validity
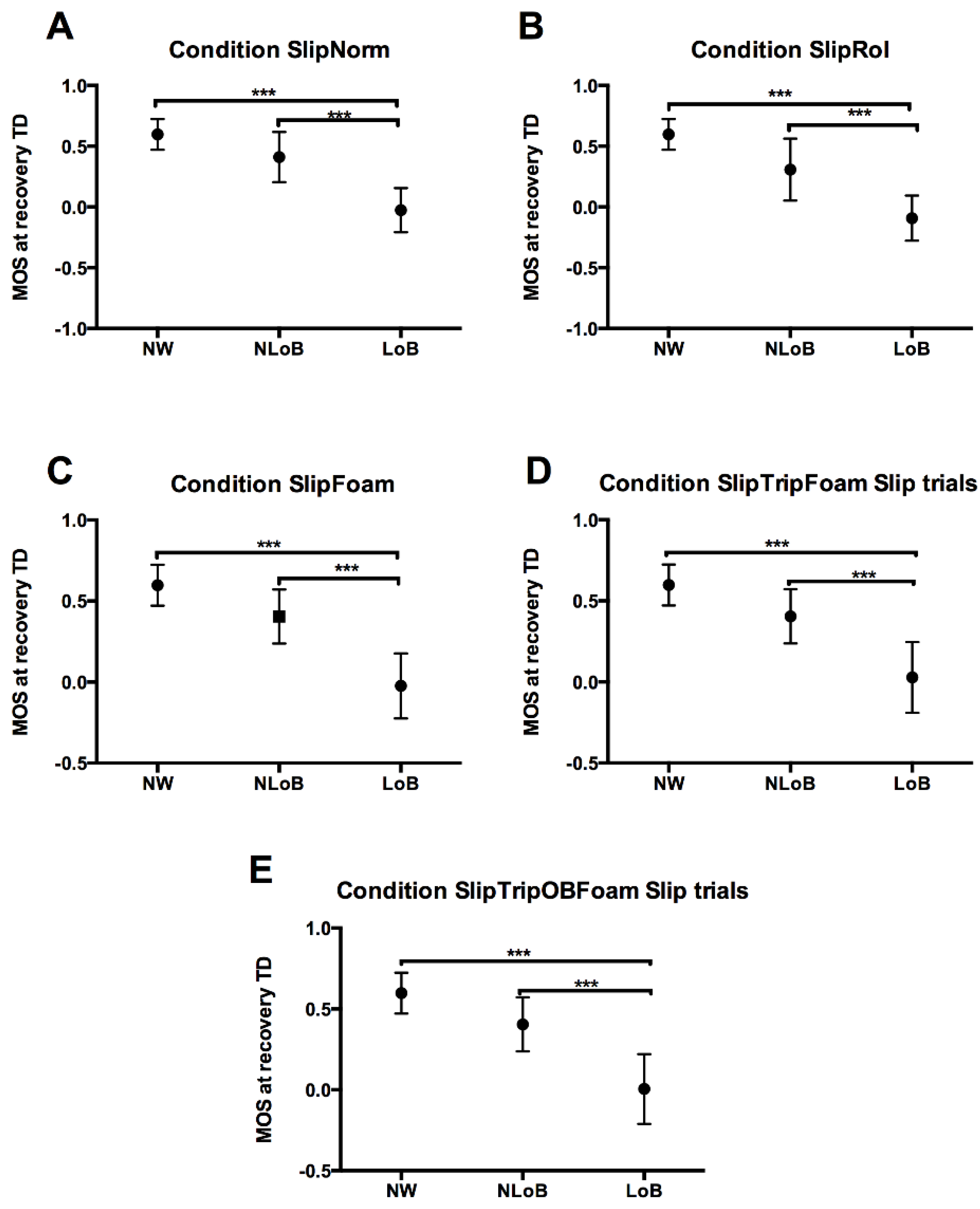
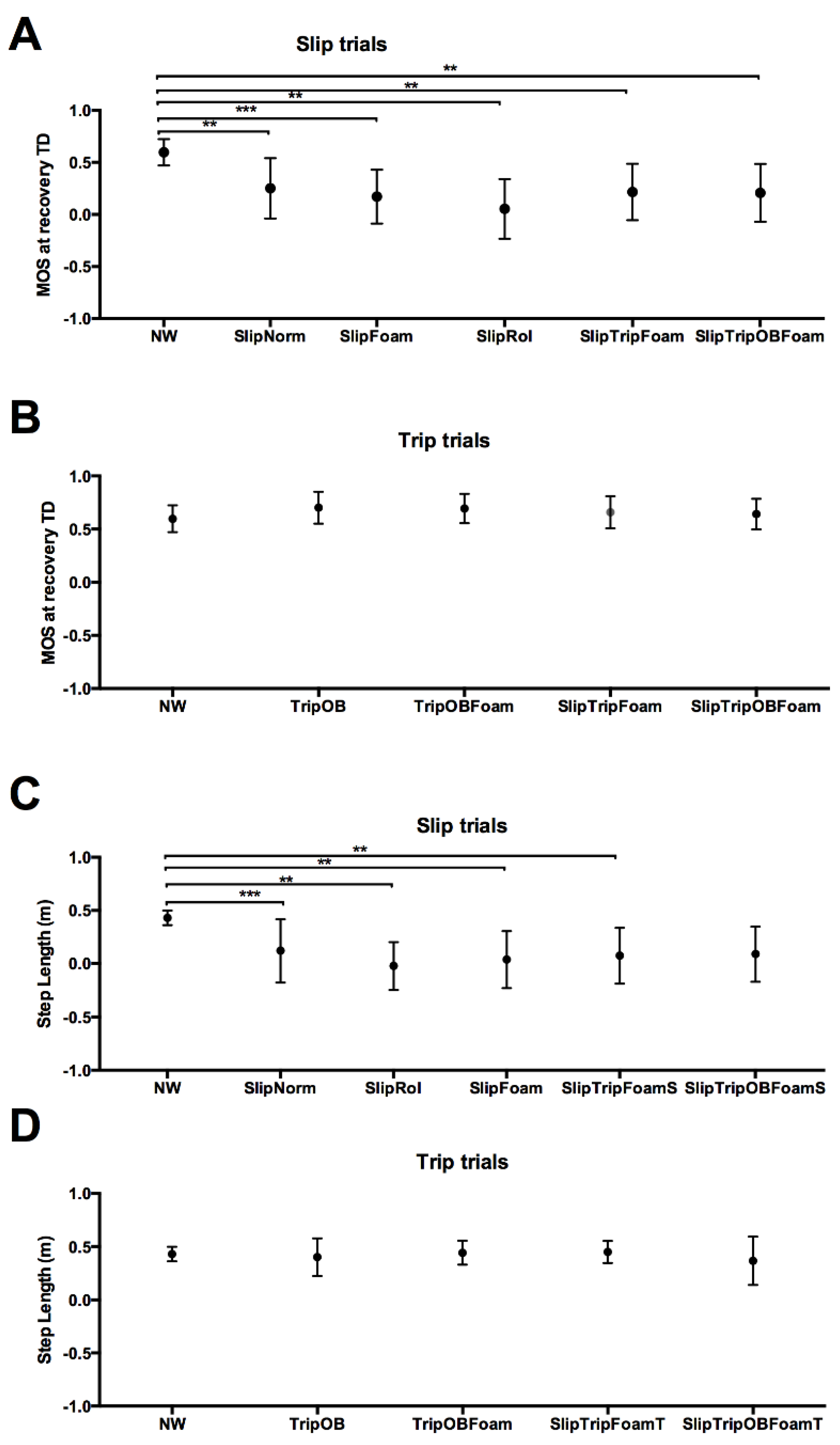
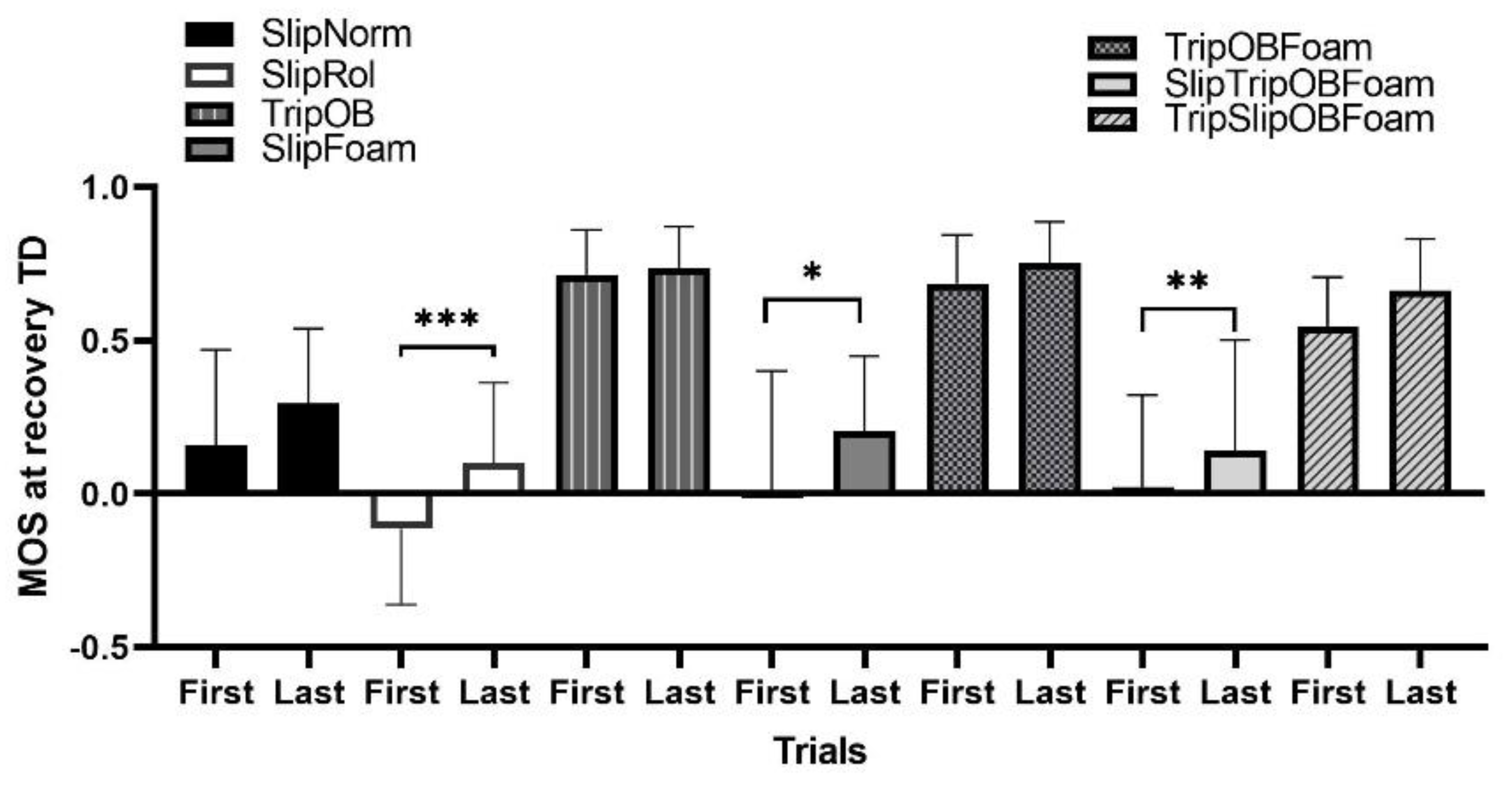
3.3.1. Margin of Stability
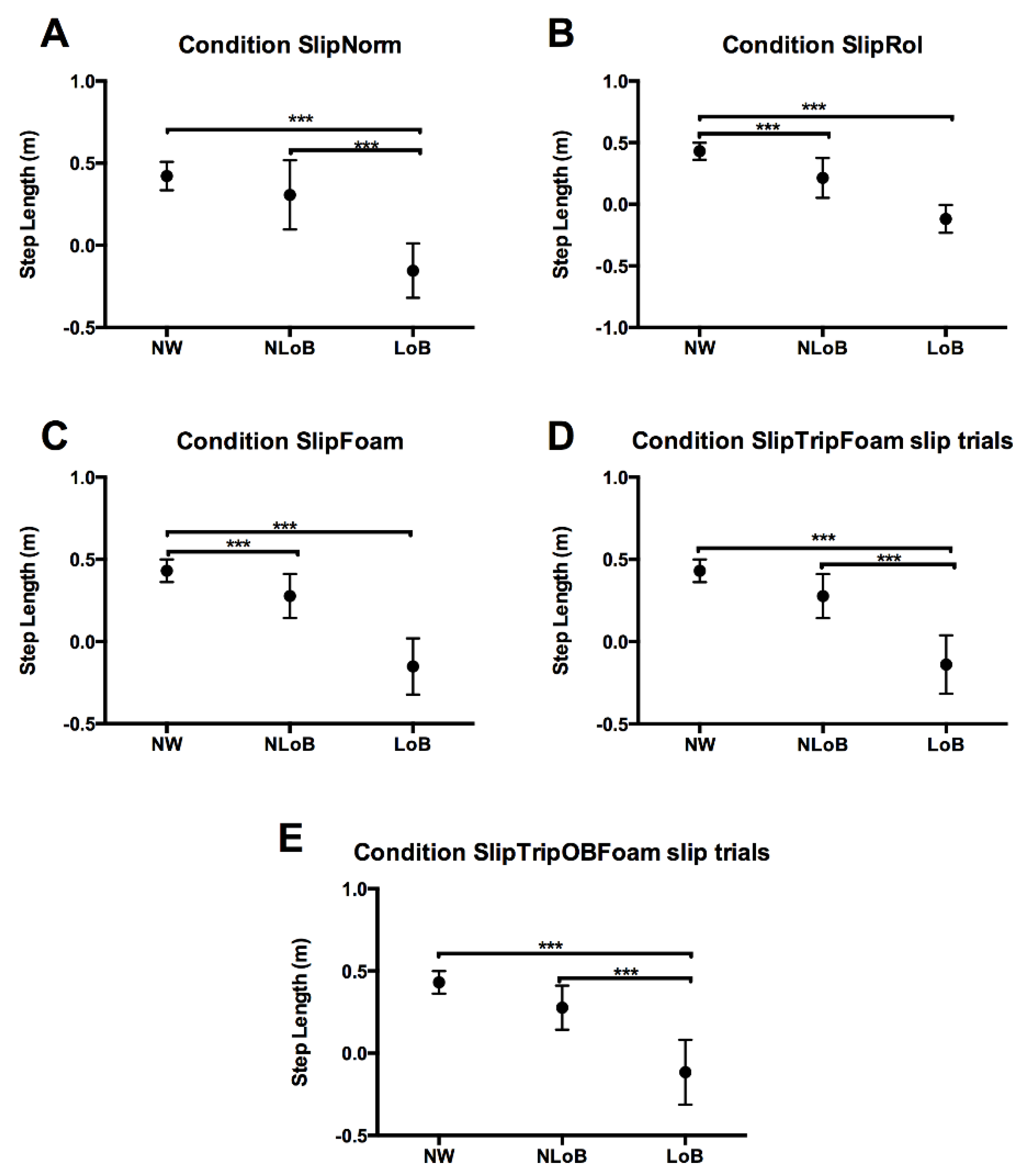
3.3.2. Step Length
3.3.3. Maximum Trunk Angle
4. Discussion
4.1. Feasibility
4.2. Validity
4.3. Perturbation-Based Intervention and Sensory Integration
4.4. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Council on Aging. NCOA Issues Call-to-Action for National Chronic Care Reform Based on Results of Comprehensive Survey of Americans with Chronic Conditions. 2009. Available online: http://multivu.prnewswire.com/mnr/ncoa/37314/ (accessed on 5 December 2015).
- Terroso, M.; Rosa, N.; Torres Marques, A.; Simoes, R. Physical consequences of falls in the elderly: A literature review from 1995 to 2010. Eur. Rev. Aging Phys. Act. 2014, 11, 51–59. [Google Scholar] [CrossRef]
- Cali, C.M.; Kiel, D.P. An epidemiologic study of fall-related fractures among institutionalized older people. J. Am. Geriatr. Soc. 1995, 43, 1336–1340. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E. A fall is a major event in the life of an older person. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M492–M495. [Google Scholar] [CrossRef] [PubMed]
- Berg, W.P.; Alessio, H.M.; Mills, E.M.; Tong, C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 1997, 26, 261–268. [Google Scholar] [CrossRef]
- Kelsey, J.L.; Procter-Gray, E.; Hannan, M.T.; Li, W. Heterogeneity of falls among older adults: Implications for public health prevention. Am. J. Public Health 2012, 102, 2149–2156. [Google Scholar] [CrossRef]
- Li, W.; Keegan, T.H.; Sternfeld, B.; Sidney, S.; Quesenberry, C.P., Jr.; Kelsey, J.L. Outdoor falls among middle-aged and older adults: A neglected public health problem. Am. J. Public Health 2006, 96, 1192–1200. [Google Scholar] [CrossRef]
- Gerards, M.H.G.; McCrum, C.; Mansfield, A.; Meijer, K. Perturbation-based balance training for falls reduction among older adults: Current evidence and implications for clinical practice. Geriatr. Gerontol. Int. 2017, 17, 2294–2303. [Google Scholar] [CrossRef] [PubMed]
- Mansfield, A.; Wong, J.S.; Bryce, J.; Knorr, S.; Patterson, K.K. Does perturbation-based balance training prevent falls? Systematic review and meta-analysis of preliminary randomized controlled trials. Phys. Ther. 2015, 95, 700–709. [Google Scholar] [CrossRef] [PubMed]
- Pai, Y.C.; Wening, J.D.; Runtz, E.F.; Iqbal, K.; Pavol, M.J. Role of feedforward control of movement stability in reducing slip-related balance loss and falls among older adults. J. Neurophysiol. 2003, 90, 755–762. [Google Scholar] [CrossRef]
- Pai, Y.C.; Bhatt, T.; Yang, F.; Wang, E. Perturbation training can reduce community-dwelling older adults’ annual fall risk: A randomized controlled trial. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1586–1594. [Google Scholar] [CrossRef]
- Okubo, Y.; Schoene, D.; Lord, S.R. Step training improves reaction time, gait and balance and reduces falls in older people: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 586–593. [Google Scholar] [CrossRef] [PubMed]
- McCrum, C.; Gerards, M.H.G.; Karamanidis, K.; Zijlstra, W.; Meijer, K. A systematic review of gait perturbation paradigms for improving reactive stepping responses and falls risk among healthy older adults. Eur. Rev. Aging Phys. Act. 2017, 14, 3. [Google Scholar] [CrossRef] [PubMed]
- Bohm, S.; Mademli, L.; Mersmann, F.; Arampatzis, A. Predictive and Reactive Locomotor Adaptability in Healthy Elderly: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 1759–1777. [Google Scholar] [CrossRef]
- Okubo, Y.; Brodie, M.A.; Sturnieks, D.L.; Hicks, C.; Carter, H.; Toson, B.; Lord, S.R. Exposure to trips and slips with increasing unpredictability while walking can improve balance recovery responses with minimum predictive gait alterations. PLoS ONE 2018, 13, e0202913. [Google Scholar] [CrossRef]
- Patla, A.E. Strategies for dynamic stability during adaptive human locomotion. IEEE Eng. Med. Biol. Mag. 2003, 22, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Hof, A.L. The equations of motion for a standing human reveal three mechanisms for balance. J. Biomech. 2007, 40, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Bierbaum, S.; Peper, A.; Karamanidis, K.; Arampatzis, A. Adaptive feedback potential in dynamic stability during disturbed walking in the elderly. J. Biomech. 2011, 44, 1921–1926. [Google Scholar] [CrossRef] [PubMed]
- Marigold, D.S.; Patla, A.E. Strategies for dynamic stability during locomotion on a slippery surface: Effects of prior experience and knowledge. J. Neurophysiol. 2002, 88, 339–353. [Google Scholar] [CrossRef]
- Dusane, S.; Wang, E.; Bhatt, T. Transfer of reactive balance adaptation from stance-slip perturbation to stance-trip perturbation in chronic stroke survivors. Restor. Neurol. Neurosci. 2019, 37, 469–482. [Google Scholar] [CrossRef]
- Patel, P.J.; Bhatt, T. Fall risk during opposing stance perturbations among healthy adults and chronic stroke survivors. Exp. Brain Res. 2018, 236, 619–628. [Google Scholar] [CrossRef]
- Bhatt, T.; Wang, T.Y.; Yang, F.; Pai, Y.C. Adaptation and generalization to opposing perturbations in walking. Neuroscience 2013, 246, 435–450. [Google Scholar] [CrossRef] [PubMed]
- Assländer, L.; Peterka, R.J. Sensory reweighting dynamics in human postural control. J. Neurophysiol. 2014, 111, 1852–1864. [Google Scholar] [CrossRef] [PubMed]
- Jeka, J.J.; Oie, K.S.; Kiemel, T. Asymmetric adaptation with functional advantage in human sensorimotor control. Exp. Brain Res. 2008, 191, 453–463. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Peterka, R.J. Sensorimotor integration in human postural control. J. Neurophysiol. 2002, 88, 1097–1118. [Google Scholar] [CrossRef]
- Peterka, R.J.; Loughlin, P.J. Dynamic regulation of sensorimotor integration in human postural control. J. Neurophysiol. 2004, 91, 410–423. [Google Scholar] [CrossRef]
- Oliveira, A.S.; Schlink, B.R.; Hairston, W.D.; König, P.; Ferris, D.P. Restricted vision increases sensorimotor cortex involvement in human walking. J. Neurophysiol. 2017, 118, 1943–1951. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, N.; Stelmach, G.E.; Breunig, A.; Meeuwsen, H.J. Age differences in visual sensory integration. Exp. Brain Res. 1991, 85, 691–696. [Google Scholar] [CrossRef]
- Woollacott, M.H.; Shumway-Cook, A.; Nashner, L.M. Aging and posture control: Changes in sensory organization and muscular coordination. Int. J. Aging Hum. Dev. 1986, 23, 97–114. [Google Scholar] [CrossRef] [PubMed]
- Allison, L.K.; Kiemel, T.; Jeka, J.J. Sensory-Challenge Balance Exercises Improve Multisensory Reweighting in Fall-Prone Older Adults. J. Neurol. Phys. Ther. 2018, 42, 84–93. [Google Scholar] [CrossRef]
- Enright, P.L.; Sherrill, D.L. Reference equations for the six-minute walk in healthy adults. Am. J. Respir. Crit. Care Med. 1998, 158 Pt 1, 1384–1387. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed]
- Hart, S.G.; Staveland, L.E. Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research. In Human Mental Workload. Advances in PsychologyHancock; Peter, A., Meshkati, N., Eds.; North Holland: Amsterdam, The Netherlands, 1998; Volume 52, pp. 139–183. [Google Scholar]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How we design feasibility studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Reporting Serious Problem to FDA: What Is a Serious Adverse Event? Available online: http://www.fda.gov/safety/medwatch/howtoreport/ucm053087.htm (accessed on 29 January 2013).
- Mourey, F.; Manckoundia, P.; Martin-Arveux, I.; Tavernier-Vidal, B.; Pfitzenmeyer, P. Psychomotor disadaptation syndrome. A new clinical entity in geriatric patients. Geriatrics 2004, 59, 20–24. [Google Scholar]
- Bahari, H.; Vette, A.H.; Hebert, J.S.; Rouhani, H. Predicted threshold against forward and backward loss of balance for perturbed walking. J. Biomech. 2019, 95, 109315. [Google Scholar] [CrossRef] [PubMed]
- Galna, B.; Peters, A.; Murphy, A.T.; Morris, M.E. Obstacle crossing deficits in older adults: A systematic review. Gait Posture 2009, 30, 270–275. [Google Scholar] [CrossRef]
- Hak, L.; Houdijk, H.; Beek, P.J.; van Dieën, J.H. Steps to take to enhance gait stability: The effect of stride frequency, stride length, and walking speed on local dynamic stability and margins of stability. PLoS ONE 2013, 8, e82842. [Google Scholar] [CrossRef]
- Hof, A.L. The ‘extrapolated center of mass’ concept suggests a simple control of balance in walking. Hum. Mov. Sci. 2008, 27, 112–125. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, E.T.; Robinovitch, S.N. Common protective movements govern unexpected falls from standing height. J. Biomech. 1998, 31, 1–9. [Google Scholar] [CrossRef]
- Grabiner, M.D.; Donovan, S.; Bareither, M.L.; Marone, J.R.; Hamstra-Wright, K.; Gatts, S.; Troy, K.L. Trunk kinematics and fall risk of older adults: Translating biomechanical results to the clinic. J. Electromyogr. Kinesiol. 2008, 18, 197–204. [Google Scholar] [CrossRef] [PubMed]
- McCrum, C.; Willems, P.; Karamanidis, K.; Meijer, K. Stability-normalised walking speed: A new approach for human gait perturbation research. J. Biomech. 2019, 87, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Pasma, J.H.; Engelhart, D.; Schouten, A.C.; van der Kooij, H.; Maier, A.B.; Meskers, C.G. Impaired standing balance: The clinical need for closing the loop. Neuroscience 2014, 267, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Burke, T.N.; França, F.J.; Meneses, S.R.; Pereira, R.M.; Marques, A.P. Postural control in elderly women with osteoporosis: Comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clin. Rehabil. 2012, 26, 1021–1031. [Google Scholar] [CrossRef] [PubMed]
- Moreno, C.M.; Woitalla, D.; Arampatzis, A. Recovery performance and factors that classify young fallers and non-fallers in Parkinson’s disease. Hum. Mov. Sci. 2015, 41, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, T.; Wening, J.D.; Pai, Y.C. Adaptive control of gait stability in reducing slip-related backward loss of balance. Exp. Brain Res. 2006, 170, 61–73. [Google Scholar] [CrossRef]


| Demographics Data | Values |
|---|---|
| Age (years) | 66.7 ± 4.4 |
| Weight (Kg) | 79.1 ± 10.05 |
| Height (cm) | 173.67 ± 6 |
| MOCA test | 27.7 ± 1.8 |
| 6 MWT (m) | 431.60 ± 57 |
| TUG (s) | 7.3 ± 2.2 |
| FSS | 4.1 ± 2.4 |
| BBS | 54.2 ± 1 |
| Protocol Condition | Hazards | Type of Perturbation |
|---|---|---|
| Condition1 (SlipNorm) | Regular surface | Slip-like perturbation |
| Condition 2 (SlipRol) | Slippery surface (walking over two 1.2 × 0.30 metallic rollers). | Slip-like perturbation |
| Condition 3 (TripOB) | Regular surface with two elastomeric cables placed at a height of 100 mm as obstacles. | Trip-like perturbation |
| Condition 4 (SlipFoam) | Foam surface | Slip-like perturbations |
| Condition 5 (TripOBFoam) | Foam surface with two elastomeric cables placed at a height of 100 mm as obstacles. | Trip-like perturbations |
| Condition 6 (SlipTripFoam) | Foam surface | Slip and trip-like perturbations |
| Condition 7 (SlipTripOBFoam) | Foam surface with two elastomeric cables placed at a height of 100 mm as obstacles. | Slip and trip-like perturbations |
| Variables | Results |
|---|---|
| Slip-perturbation repetitions | 18 ± 4.7 |
| Trip-perturbation repetitions | 14.4 ± 3.5 |
| NASA-TLX | |
| Mental demand | 3.4 ± 6.7 |
| Physical Demand | 13.4 ± 24.6 |
| Temporal Demand | 5.1 ± 13.6 |
| Performance | 67.4 ± 33.8 |
| Effort | 55.7 ± 16.4 |
| Frustration Level | 4.7 ± 4.8 |
| Global Score | 24.95 |
| Study Conditions | % of Trials That Resulted in LoB or Fall | N of Trials That Resulted in LoB or Fall | N of Perturbation Trials for Each Condition | N of Trials (Total) |
|---|---|---|---|---|
| SlipNorm | 45.8% | 39 (1.95 + 0.2) | 85 (4.25 + 0.3) | 332 (16.6 + 2.4) |
| SlipRol | 73.7% | 59 (2.95 + 0.3) | 80 (4 + 0.2) | 218 (10.9 + 1.1) |
| TripOB | 20.6% | 18 (0.9 + 0.3) | 87 (4.35 + 0.4) | 249 (12.4 + 1.5) |
| SlipFoam | 80% | 64 (3.2 + 0.3) | 80 (4 + 0.2) | 264 (13.2 + 1.5) |
| TripOBFoam | 26.1% | 22 (1.1 + 0.4) | 84 (4.2 + 0.2) | 276 (13.8 + 1.2) |
| SlipTripFoam (sliptrials) | 77.5% | 31 (1.55 + 0.2) | 40 (2 + 0.1) | 109 (5.4 + 0.6) |
| SlipTripOBFoam (trip trials) | 15% | 6 (0.3 + 0.5) | 40 (2 + 0.1) | 100 (5 + 0.6) |
| SlipTripFoam (slip trials) | 75% | 30 (1.5 + 0.3) | 40 (2 + 0.1) | 111 (5.5 + 0.6) |
| SlipTripOBFoam (trip trials) | 35% | 14 (0.7 + 0.5) | 40 (2 + 0.1) | 100 (5 + 0.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Varas-Diaz, G.; Jayakumar, U.; Taras, B.; Wang, S.; Bhatt, T. Assessing Balance Loss and Stability Control in Older Adults Exposed to Gait Perturbations under Different Environmental Conditions: A Feasibility Study. Biomechanics 2022, 2, 374-394. https://doi.org/10.3390/biomechanics2030030
Varas-Diaz G, Jayakumar U, Taras B, Wang S, Bhatt T. Assessing Balance Loss and Stability Control in Older Adults Exposed to Gait Perturbations under Different Environmental Conditions: A Feasibility Study. Biomechanics. 2022; 2(3):374-394. https://doi.org/10.3390/biomechanics2030030
Chicago/Turabian StyleVaras-Diaz, Gonzalo, Udai Jayakumar, Bradford Taras, Shuaijie Wang, and Tanvi Bhatt. 2022. "Assessing Balance Loss and Stability Control in Older Adults Exposed to Gait Perturbations under Different Environmental Conditions: A Feasibility Study" Biomechanics 2, no. 3: 374-394. https://doi.org/10.3390/biomechanics2030030
APA StyleVaras-Diaz, G., Jayakumar, U., Taras, B., Wang, S., & Bhatt, T. (2022). Assessing Balance Loss and Stability Control in Older Adults Exposed to Gait Perturbations under Different Environmental Conditions: A Feasibility Study. Biomechanics, 2(3), 374-394. https://doi.org/10.3390/biomechanics2030030





