A Survival Analysis Based on Forensic Investigation of Motorcycle Road Traffic Accidents in the Athens Metropolitan Area During 2021–2023
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Status Report on Road Safety 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Whyte, T.; Gibson, T.; Anderson, R.; Eager, D.; Milthorpe, B. Mechanisms of Head and Neck Injuries Sustained by Helmeted Motorcyclists in Fatal Real-World Crashes: Analysis of 47 In-Depth Cases. J. Neurotrauma 2016, 33, 1802–1807. [Google Scholar] [CrossRef]
- Kuo, S.C.H.; Kuo, P.J.; Rau, C.S.; Chen, Y.C.; Hsieh, H.Y.; Hsieh, C.H. The protective effect of helmet use in motorcycle and bicycle accidents: A propensity score-matched study based on a trauma registry system. BMC Public Health 2017, 17, 639. [Google Scholar] [CrossRef]
- Boughton, O.; Jones, G.G.; Lavy, C.B.; Grimes, C.E. Young, male, road traffic victims: A systematic review of the published trauma registry literature from low and middle income countries. SICOT J. 2015, 1, 10. [Google Scholar] [CrossRef] [PubMed]
- Ganem, G.; Fernandes, R.C.P. Motorcycle accidents: Characteristics of victims admitted to public hospitals and circumstances. Rev. Bras. Med. Trab. 2020, 18, 51–58. [Google Scholar] [CrossRef] [PubMed]
- Giovannini, E.; Santelli, S.; Pelletti, G.; Bonasoni, M.P.; Lacche, E.; Pelotti, S.; Fais, P. Motorcycle injuries: A systematic review for forensic evaluation. Int. J. Leg. Med. 2024, 138, 1907–1924. [Google Scholar] [CrossRef] [PubMed]
- Kiwango, G.; Katopola, D.; Francis, F.; Moller, J.; Hasselberg, M. A systematic review of risk factors associated with road traffic crashes and injuries among commercial motorcycle drivers. Int. J. Inj. Contr. Saf. Promot. 2024, 31, 332–345. [Google Scholar] [CrossRef]
- Barzegar, A.; Ghadipasha, M.; Forouzesh, M.; Valiyari, S.; Khademi, A. Epidemiologic study of traffic crash mortality among motorcycle users in Iran (2011–2017). Chin. J. Traumatol. 2020, 23, 219–223. [Google Scholar] [CrossRef]
- Bakovic, M.; Mazuranic, A.; Petrovecki, V.; Mayer, D. Fatal motorcycle crashes in wide urban area of Zagreb, Croatia-A 10-year review. Traffic Inj. Prev. 2019, 20, 655–660. [Google Scholar] [CrossRef]
- Rappole, C.; Canham-Chervak, M.; Taylor, B.; Jones, B.H. Factors associated with motorcycle traffic crash fatalities among active duty U.S. Army personnel. Traffic Inj. Prev. 2019, 20, 174–181. [Google Scholar] [CrossRef]
- Souza, C.D.F.; Paiva, J.P.S.; Leal, T.C.; Silva, L.F.D.; Machado, M.F.; Araujo, M.D.P. Mortality in motorcycle accidents in Alagoas (2001–2015): Temporal and spatial modeling before and after the “lei seca”. Rev. Assoc. Med. Bras. 2019, 65, 1482–1488. [Google Scholar] [CrossRef]
- Roehler, D.R.; Ear, C.; Parker, E.M.; Sem, P.; Ballesteros, M.F. Fatal motorcycle crashes: A growing public health problem in Cambodia. Int. J. Inj. Contr. Saf. Promot. 2015, 22, 165–171. [Google Scholar] [CrossRef]
- Emiogun, E.F.; Sanni, D.A.; Soyemi, S.S.; Faduyile, F.A.; Obafunwa, J.O. Trends in motorcycle accident mortality in Lagos: Consequences of government policy changes. Med. Sci. Law 2022, 62, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Ghadipasha, M.; Vaghefi, S.S.; Kazemi Esfeh, S.; Teimoori, M.; Ouhadi, A.R.; Mirhosseini, S.M. An annual analysis of clinical diagnosis versus autopsy findings in fatal motor vehicle accident in legal medicine organization of Kerman province, Iran. J. Forensic Leg. Med. 2015, 34, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi-Bazargani, H.; Samadirad, B.; Hosseinpour-Feizi, H. Epidemiology of Traffic Fatalities among Motorcycle Users in East Azerbaijan, Iran. Biomed Res. Int. 2018, 2018, 6971904. [Google Scholar] [CrossRef] [PubMed]
- Kukde, H.G.; Kumar, N.B.; Sabale, M.R.; Sawardekar, S.G.; Dere, R.C. Study of Motorcycle Fatalities in Mumbai: A Two Year Retrospective Analysis. J. Forensic Med. Sci. Law 2019, 28, 22–26. [Google Scholar]
- Naildo Cardoso Leitão, F.; Furlan, C.; Luiz Figueiredo, J.; Ricardo Perez-Riera, A. Traffic accident mortality of motorcyclists, pedestrians and hospital costs in the city of São Paulo. J. Human Growth Dev. 2023, 33, 365–375. [Google Scholar] [CrossRef]
- Department for Transport. Reported Road Casualties Great Britain: Motorcyclist Factsheet 2022; Department for Transport: London, UK, 2023. [Google Scholar]
- Medeiros, A.L.; Nadanovsky, P. Car and motorcycle deaths: An evolutionary perspective. Cienc. Saude Coletiva 2016, 21, 3691–3702. [Google Scholar] [CrossRef]
- Benghuzzi, H.; Powe, C.; Watts, D.; Barrett, T.; Tucci, M. Motorcycle Helmet Use and Fatalities in the Southeast Region of the USA. Biomed Sci. Instrum. 2021, 57, 145–152. [Google Scholar] [CrossRef]
- Faduyile, F.; Emiogun, F.; Soyemi, S.; Oyewole, O.; Okeke, U.; Williams, O. Pattern of Injuries in Fatal Motorcycle Accidents Seen in Lagos State University Teaching Hospital: An Autopsy-Based Study. Open Access Maced. J. Med. Sci. 2017, 5, 112–116. [Google Scholar] [CrossRef]
- Hosseinpour, M.; Mohammadian-Hafshejani, A.; Esmaeilpour Aghdam, M.; Mohammadian, M.; Maleki, F. Trend and Seasonal Patterns of Injuries and Mortality Due to Motorcyclists Traffic Accidents; A Hospital-Based Study. Bull. Emerg. Trauma 2017, 5, 47–52. [Google Scholar]
- Jama, H.H.; Grzebieta, R.H.; Friswell, R.; McIntosh, A.S. Characteristics of fatal motorcycle crashes into roadside safety barriers in Australia and New Zealand. Accid. Anal. Prev. 2011, 43, 652–660. [Google Scholar] [CrossRef]
- Chung, Y.S.; Wong, J.T. Beyond general behavioral theories: Structural discrepancy in young motorcyclist’s risky driving behavior and its policy implications. Accid. Anal. Prev. 2012, 49, 165–176. [Google Scholar] [CrossRef] [PubMed]
- Genowska, A.; Jamiolkowski, J.; Szafraniec, K.; Fryc, J.; Pajak, A. Health Care Resources and 24,910 Deaths Due to Traffic Accidents: An Ecological Mortality Study in Poland. Int. J. Environ. Res. Public Health 2021, 18, 5561. [Google Scholar] [CrossRef] [PubMed]
- Granieri, S.S.; Reitano, E.E.; Bindi, F.F.; Renzi, F.F.; Sammartano, F.F.; Cimbanassi, S.S.; Gupta, S.S.; Chiara, O.O. Motorcycle-related trauma:effects of age and site of injuries on mortality. A single-center, retrospective study. World J. Emerg. Surg. 2020, 15, 18. [Google Scholar] [CrossRef]
- Champahom, T.; Se, C.; Jomnonkwao, S.; Boonyoo, T.; Leelamanothum, A.; Ratanavaraha, V. Temporal Instability of Motorcycle Crash Fatalities on Local Roadways: A Random Parameters Approach with Heterogeneity in Means and Variances. Int. J. Environ. Res. Public Health 2023, 20, 3845. [Google Scholar] [CrossRef]
- Chang, F.; Li, M.; Xu, P.; Zhou, H.; Haque, M.M.; Huang, H. Injury Severity of Motorcycle Riders Involved in Traffic Crashes in Hunan, China: A Mixed Ordered Logit Approach. Int. J. Environ. Res. Public Health 2016, 13, 714. [Google Scholar] [CrossRef]
- Takeda, A.; Koh, M.; Nakanishi, T.; Hitosugi, M. Differences in severity of injuries between motorcyclist and bicyclist fatalities in single vehicle collisions. J. Forensic Leg. Med. 2020, 70, 101917. [Google Scholar] [CrossRef]
- Matsuyama, T.; Kitamura, T.; Katayama, Y.; Hirose, T.; Kiguchi, T.; Sado, J.; Kiyohara, K.; Izawa, J.; Okada, N.; Takebe, K.; et al. Motor vehicle accident mortality by elderly drivers in the super-aging era: A nationwide hospital-based registry in Japan. Medicine 2018, 97, e12350. [Google Scholar] [CrossRef]
- Jou, R.C.; Yeh, T.H.; Chen, R.S. Risk factors in motorcyclist fatalities in Taiwan. Traffic Inj. Prev. 2012, 13, 155–162. [Google Scholar] [CrossRef]
- Puac-Polanco, V.; Keyes, K.M.; Li, G. Mortality from motorcycle crashes: The baby-boomer cohort effect. Inj. Epidemiol. 2016, 3, 19. [Google Scholar] [CrossRef]
- Islam, M. The effect of motorcyclists’ age on injury severities in single-motorcycle crashes with unobserved heterogeneity. J. Safety Res. 2021, 77, 125–138. [Google Scholar] [CrossRef]
- Ahmed, N.; Kuo, Y.H.; Sharma, J.; Kaul, S. Elevated blood alcohol impacts hospital mortality following motorcycle injury: A National Trauma Data Bank analysis. Injury 2020, 51, 91–96. [Google Scholar] [CrossRef]
- Sarmiento, J.M.; Gogineni, A.; Bernstein, J.N.; Lee, C.; Lineen, E.B.; Pust, G.D.; Byers, P.M. Alcohol/Illicit Substance Use in Fatal Motorcycle Crashes. J. Surg. Res. 2020, 256, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Lu, N.; Butler, C.C.; Gogineni, A.; Sarmiento, J.M.; Lineen, E.B.; Yeh, D.D.; Babu, M.; Byers, P.M. Redefining Preventable Death-Potentially Survivable Motorcycle Scene Fatalities as a New Frontier. J. Surg. Res. 2020, 256, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Mohd Saman, S.A.; Jothee, S.; Nor, F.M.; Shafie, M.S. The Pattern of Injuries Among Motorcyclists in Fatal Road Traffic Accidents: An Autopsy-Based Study. Am. J. Forensic Med. Pathol. 2021, 42, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yao, H.; Hu, G.; Cui, M.; Gu, Y.; Xiang, H. Basic characteristics of road traffic deaths in China. Iran. J. Public Health 2013, 42, 7–15. [Google Scholar]
- Ramli, R.; Oxley, J.; Noor, F.M.; Abdullah, N.K.; Mahmood, M.S.; Tajuddin, A.K.; McClure, R. Fatal injuries among motorcyclists in Klang Valley, Malaysia. J. Forensic Leg. Med. 2014, 26, 39–45. [Google Scholar] [CrossRef]
- Christophersen, A.S.; Gjerde, H. Prevalence of alcohol and drugs among motorcycle riders killed in road crashes in Norway during 2001–2010. Accid. Anal. Prev. 2015, 80, 236–242. [Google Scholar] [CrossRef]
- Lusetti, A.; Dagoli, S.; Banchini, A.; Gentile, M.; Lezzi, P.; Cecchi, R. Over 30-year retrospective analyses of moped-motorcycle fatal road accidents in the northern area of the Italian region of Emilia Romagna and review of the literature: Aiming for further preventive measures in the future. Leg. Med. 2022, 59, 102139. [Google Scholar] [CrossRef]
- Canzi, G.; De Ponti, E.; Filippi, A.; Bozzetti, A.; Sozzi, D.; Novelli, G. The burden of facial trauma on mortality in patients with multiple injuries: A single-center analysis of 1862 motorcycle accidents. J. Craniomaxillofac. Surg. 2022, 50, 146–149. [Google Scholar] [CrossRef]
- Tchin, D.; Atsi, W.; Tchaa, T.H.; Essossinam, K.; Edem, J.Y.; Amegbor, K.K.; Gado, N.K. Epidemiological data and forensic aspects of road traffic fatalities in Lome, Togo. Med. Sante Trop. 2016, 26, 332–333. [Google Scholar] [CrossRef]
- Takeda, A.; Hitosugi, M.; Furukawa, S. Autopsy Cases of Motorcyclists Dying of Trauma or Disease. Am. J. Forensic Med. Pathol. 2017, 38, 222–225. [Google Scholar] [CrossRef]
- Hollis, S.; Lecky, F.; Yates, D.W.; Woodford, M. The effect of pre-existing medical conditions and age on mortality after injury. J. Trauma Acute Care Surg. 2006, 61, 1255–1260. [Google Scholar] [CrossRef]
- Charlton, J.; Koppel, S.; O’Hare, M.; Andrea, D.; Smith, G.; Khodr, B.; Langford, J.; Odell, M.; Fildes, B. Influence of chronic illness on crash involvement of motor vehicle drivers (Report No. 213). Natl. Acad. Sci. Eng. Med. 2004, 213, 436. [Google Scholar]
- Cuthbertson, J.; Drummond, G. Prehospital Care Post-Road-Crash: A Systematic Review of the Literature. Prehosp. Disaster Med. 2025, 40, 94–100. [Google Scholar] [CrossRef]
| Variable | Category | Frequency | Percent | Median (IQR) |
|---|---|---|---|---|
| General Demographics | ||||
| Sex | Male | 89 | 94.68% | |
| Female | 5 | 5.32% | ||
| Age | 40.5 (27–53) | |||
| Nationality | Greek | 80 | 85.11% | |
| Other | 14 | 14.89% | ||
| Time and Distance | ||||
| Time to Arrive | <60 min | 36 | 54.55% | |
| >60 min | 30 | 45.45% | ||
| Distance to Hospital | 10.4 (5.25–16.65) | |||
| Social History Data (Obtained Through Interviews of the Relatives of the Deceased) | ||||
| Alcohol | Yes | 15 | 21.13% | |
| No | 56 | 78.87% | ||
| Smoking | Yes | 62 | 77.50% | |
| No or stopped | 18 | 22.50% | ||
| Substance | Yes | 19 | 23.46% | |
| No | 62 | 76.54% | ||
| Pre-Existing Medical Conditions (Obtained Through Interview of the Relatives of the Deceased) | ||||
| Cardiovascular Disease | No | 78 | 82.98% | |
| Yes | 16 | 17.02% | ||
| Metabolic Disease | No | 92 | 97.87% | |
| Yes | 2 | 2.13% | ||
| Decreased Mobility | No | 91 | 96.81% | |
| Yes | 3 | 3.19% | ||
| Psychiatric Condition | No | 89 | 96.74% | |
| Yes | 3 | 3.26% | ||
| Injuries Sustained, as Ascertained by the Post-Mortem Examination | ||||
| Head Injury | No | 25 | 26.60% | |
| Yes | 69 | 73.40% | ||
| Neck Injury | No | 73 | 77.66% | |
| Yes | 21 | 22.34% | ||
| Chest Injury | No | 21 | 22.34% | |
| Yes | 73 | 77.66% | ||
| Abdominal Injury | No | 40 | 42.55% | |
| Yes | 54 | 57.45% | ||
| Upper Limb Injury | No | 65 | 69.15% | |
| Yes | 29 | 30.85% | ||
| Lower Limb Injury | No | 65 | 69.15% | |
| Yes | 29 | 30.85% | ||
| Multiple Injuries | No | 31 | 32.98% | |
| Yes | 63 | 67.02% | ||
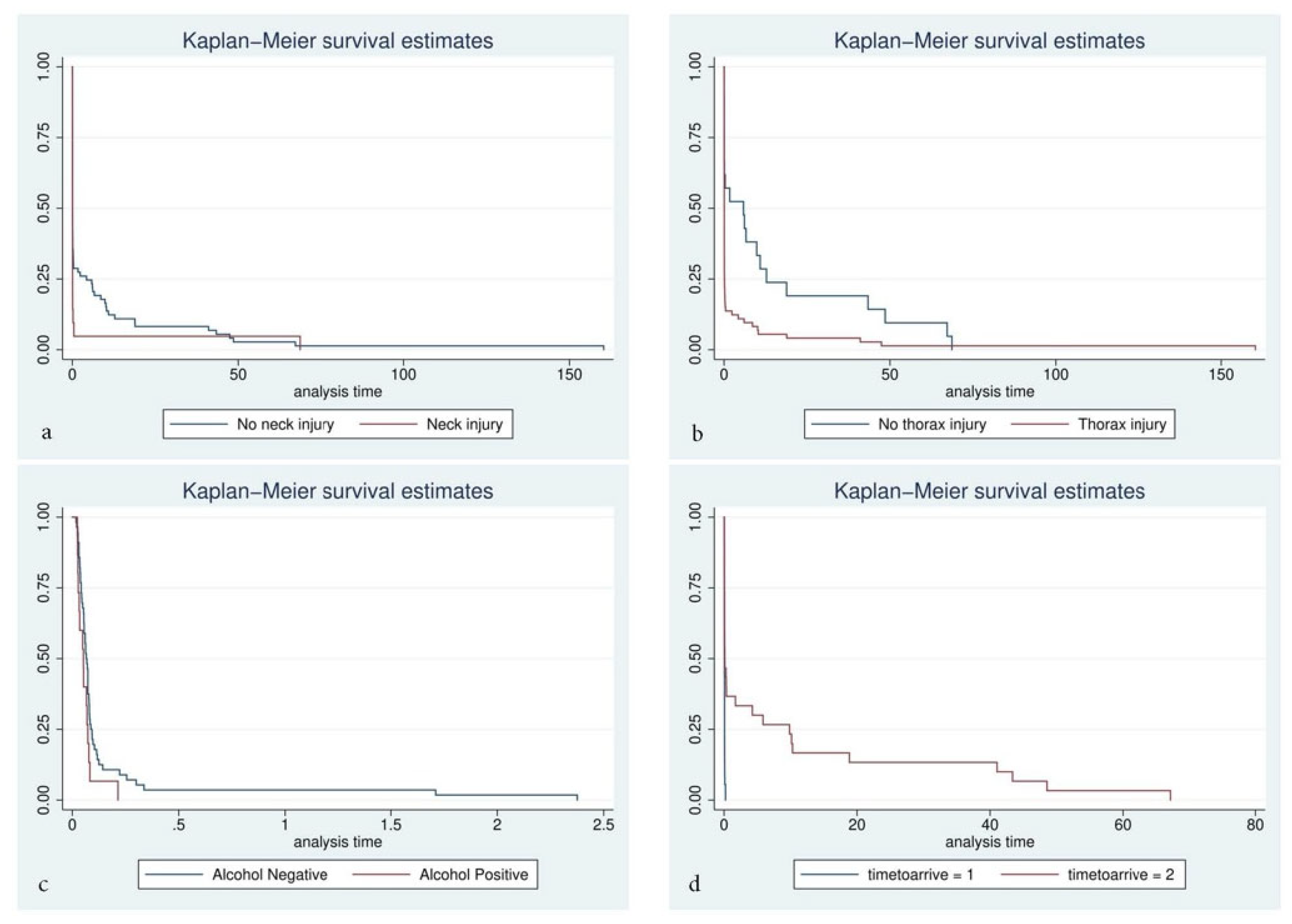
| Variable | Group | Median Survival Time (Days) | Hazard Ratio | 95% CI | p-Value |
|---|---|---|---|---|---|
| General Demographics | |||||
| Sex | Male (Ref) | 0.07 | 0.44 | 0.16–1.23 | 0.118 |
| Female | 5.9 | ||||
| Age | ≤40 years (median) (ref) | 0.07 | 0.84 | 0.56–1.26 | 0.396 |
| >40 years | 0.081 | ||||
| Nationality | Greek | 0.073 | 1.43 | 0.80–2.55 | 0.23 |
| Other | 0.066 | ||||
| Time and Distance | |||||
| Time to Arrive | ≤60 min (golden hour) (ref) | 0.05 | 0.22 | 0.12–0.41 | <0.001 |
| >60 min | 0.115 | ||||
| Distance to Hospital | ≤10 km (median) (ref) | 0.081 | 1.34 | 0.877–2.06 | 0.173 |
| >10 km | 0.073 | ||||
| Social History Data (Obtained Through Interview of the Relatives of the Deceased) | |||||
| Alcohol | Yes | 0.05 | 1.74 | 1.12–3.11 | 0.049 |
| No (ref) | 0.07 | ||||
| Smoking | Yes (ref) | 0.068 | 0.7 | 0.41–1.21 | 0.204 |
| No (never or stopped) | 0.097 | ||||
| Substance | Yes | 0.073 | 1.04 | 0.62–1.74 | 0.893 |
| No (ref) | 0.073 | ||||
| Pre-Existing Medical Conditions (Obtained Through Interview of the Relatives of the Deceased) | |||||
| Cardiovascular | Yes | 0.083 | 0.94 | 0.54–1.61 | 0.808 |
| No (ref) | 0.073 | ||||
| Metabolic | Yes | 0.035 | 1.99 | 0.49–8.19 | 0.338 |
| No (ref) | 0.073 | ||||
| Decreased Mobility | Yes | 0.073 | 0.97 | 0.31–3.09 | 0.962 |
| No (ref) | 0.073 | ||||
| Psychiatric Condition | Yes | 0.093 | 0.65 | 0.20–2.08 | 0.473 |
| No (ref) | 0.073 | ||||
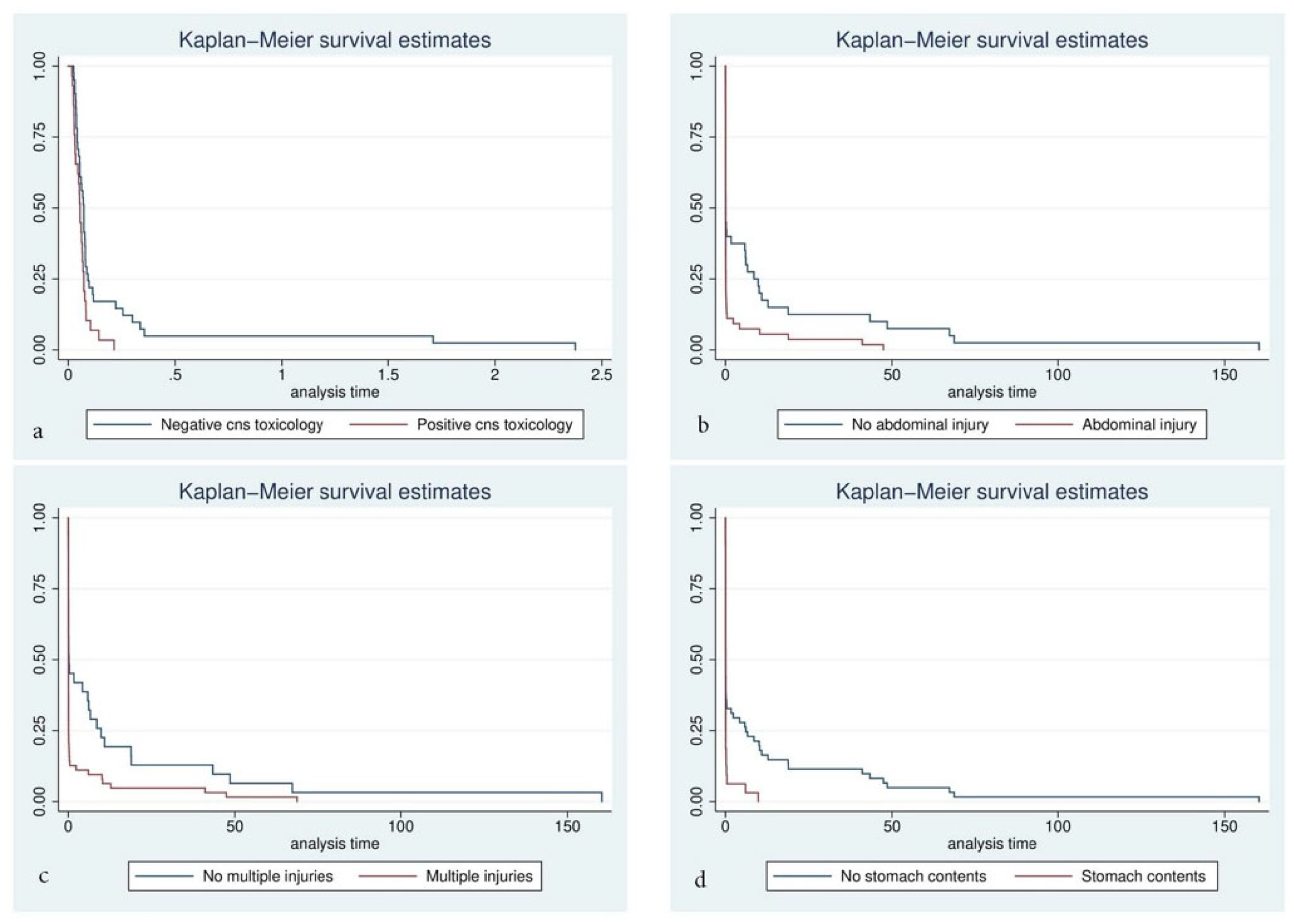
| Injuries Sustained, as Ascertained by the Post-Mortem Examination | |||||
| Head Trauma | Yes | 0.07 | 0.94 | 0.59–1.5 | 0.782 |
| No (ref) | 0.08 | ||||
| Neck Trauma | Yes | 0.066 | 1.62 | 1.04–2.67 | 0.047 |
| No (ref) | 0.081 | ||||
| Thorax Trauma | Yes | 0.07 | 2.15 | 1.3–3.56 | 0.003 |
| No (ref) | 5.85 | ||||
| Abdominal Trauma | Yes | 0.068 | 1.79 | 1.16–2.77 | 0.009 |
| No (ref) | 0.079 | ||||
| Upper Limb Trauma | Yes | 0.073 | 1.09 | 0.69–1.69 | 0.707 |
| No (ref) | 0.073 | ||||
| Lower Limb Trauma | Yes | 0.062 | 1.26 | 0.81–1.96 | 0.312 |
| No (ref) | 0.078 | ||||
| Multiple Injuries | Yes | 0.066 | 1.94 | 1.24–3.02 | 0.004 |
| No (ref) | 0.2 | ||||
| Variable | Adjusted Hazard Ratio | 95% Conf. Interval | p-Value |
|---|---|---|---|
| Time to Arrive | 0.54 | 0.28–1.03 | 0.06 |
| Multiple Injuries | 1.93 | 0.97–3.82 | 0.06 |
| Positive Toxicological Examination for Psychoactive Substances | 2.12 | 1.16–3.88 | 0.015 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tousia, A.; Kouzos, D.; Katsos, K.; Ketsekioulafis, I.; Papoutsis, I.; Ntona, A.; Georgiadis, N.; Sergentanis, T.N.; Spiliopoulou, C.A.; Sakelliadis, E.I. A Survival Analysis Based on Forensic Investigation of Motorcycle Road Traffic Accidents in the Athens Metropolitan Area During 2021–2023. Forensic Sci. 2025, 5, 68. https://doi.org/10.3390/forensicsci5040068
Tousia A, Kouzos D, Katsos K, Ketsekioulafis I, Papoutsis I, Ntona A, Georgiadis N, Sergentanis TN, Spiliopoulou CA, Sakelliadis EI. A Survival Analysis Based on Forensic Investigation of Motorcycle Road Traffic Accidents in the Athens Metropolitan Area During 2021–2023. Forensic Sciences. 2025; 5(4):68. https://doi.org/10.3390/forensicsci5040068
Chicago/Turabian StyleTousia, Athina, Dimitris Kouzos, Konstantinos Katsos, Ioannis Ketsekioulafis, Ioannis Papoutsis, Artemisia Ntona, Nikolaos Georgiadis, Theodoros N. Sergentanis, Chara A. Spiliopoulou, and Emmanouil I. Sakelliadis. 2025. "A Survival Analysis Based on Forensic Investigation of Motorcycle Road Traffic Accidents in the Athens Metropolitan Area During 2021–2023" Forensic Sciences 5, no. 4: 68. https://doi.org/10.3390/forensicsci5040068
APA StyleTousia, A., Kouzos, D., Katsos, K., Ketsekioulafis, I., Papoutsis, I., Ntona, A., Georgiadis, N., Sergentanis, T. N., Spiliopoulou, C. A., & Sakelliadis, E. I. (2025). A Survival Analysis Based on Forensic Investigation of Motorcycle Road Traffic Accidents in the Athens Metropolitan Area During 2021–2023. Forensic Sciences, 5(4), 68. https://doi.org/10.3390/forensicsci5040068








