Rare Complications of Fatal Caffeine Intoxication
Abstract
1. Introduction
2. Case Report
2.1. Case History
2.2. Autopsy Findings
2.2.1. External Examination
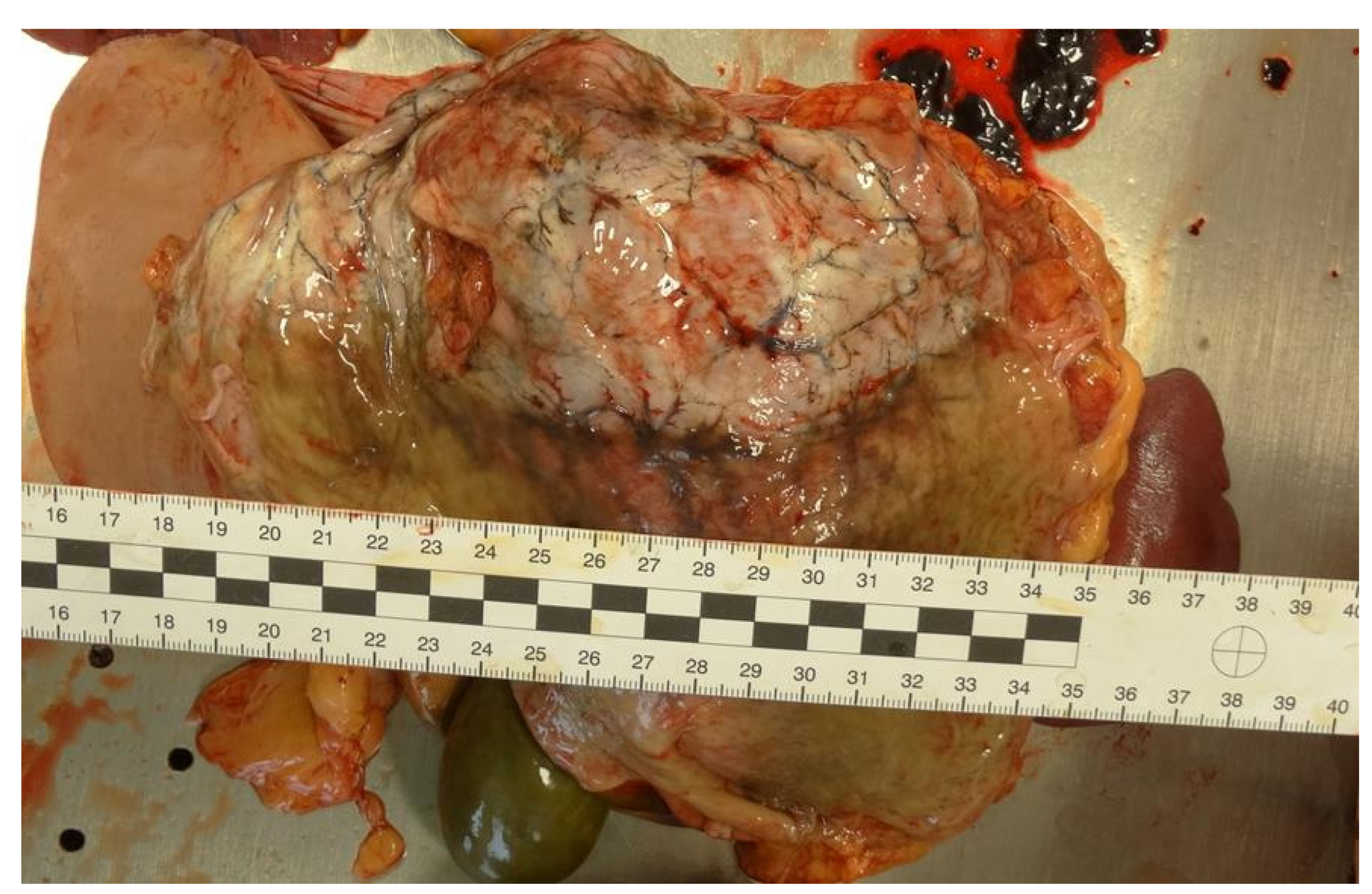
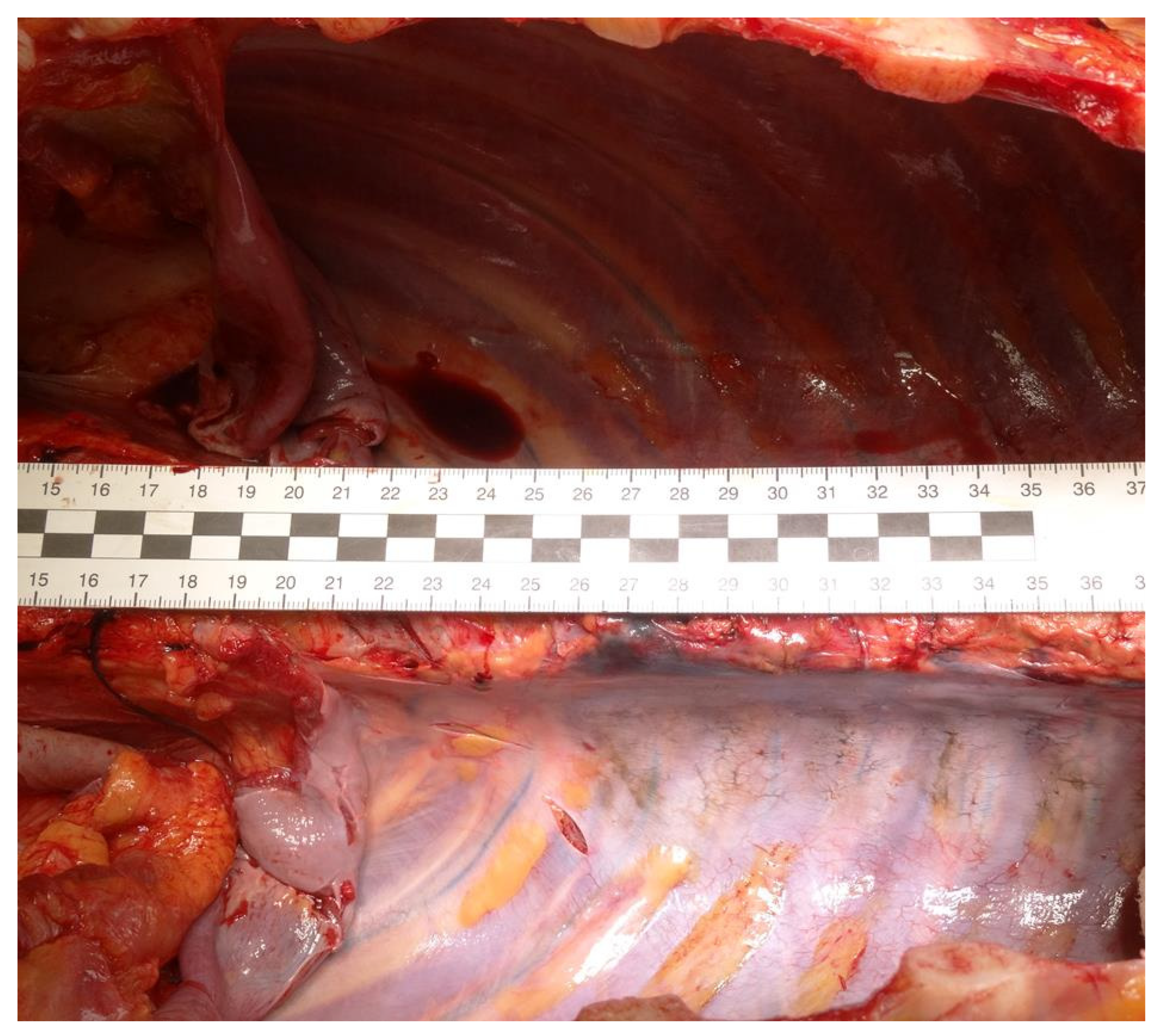
2.2.2. Internal Examination
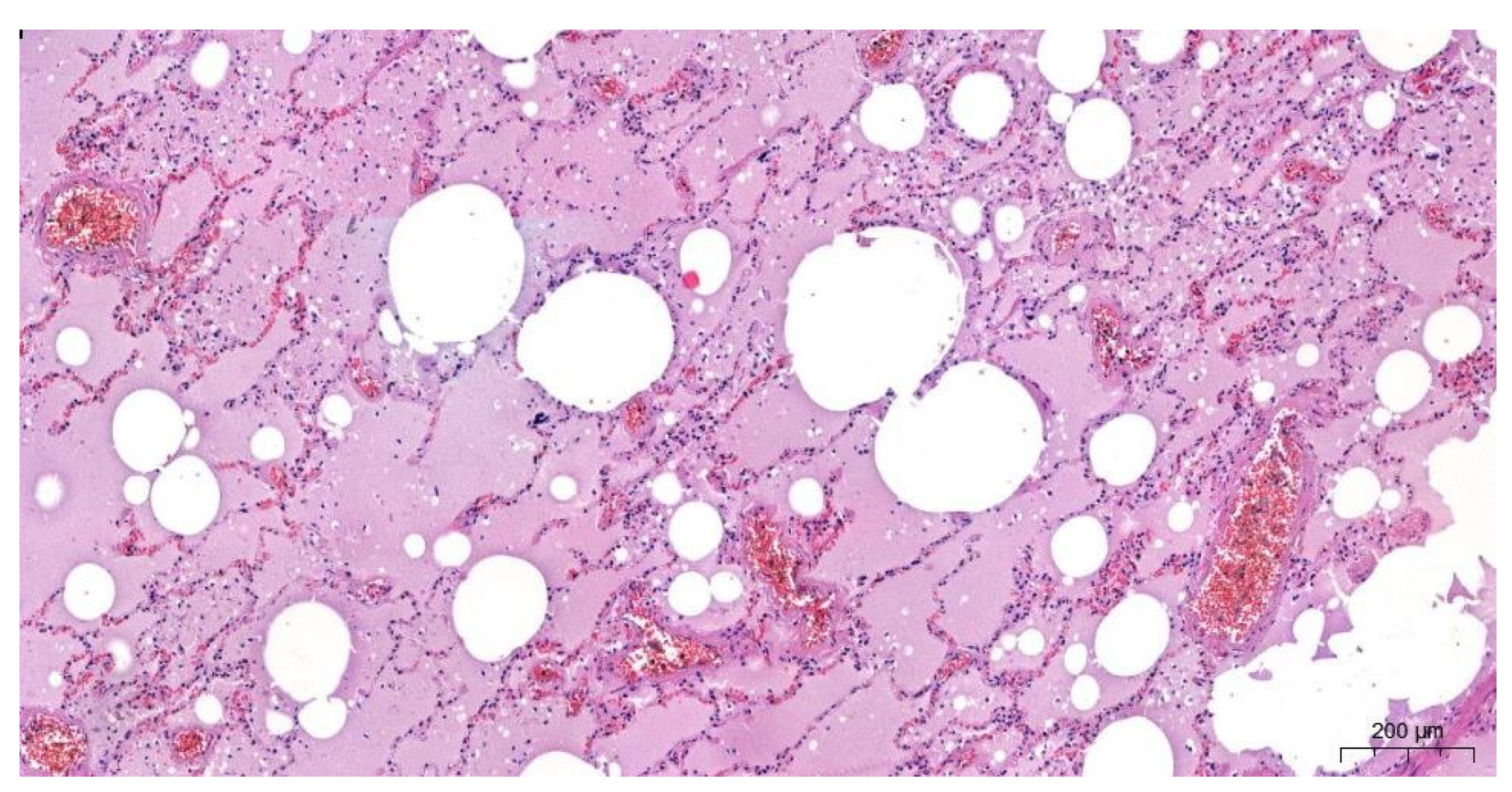
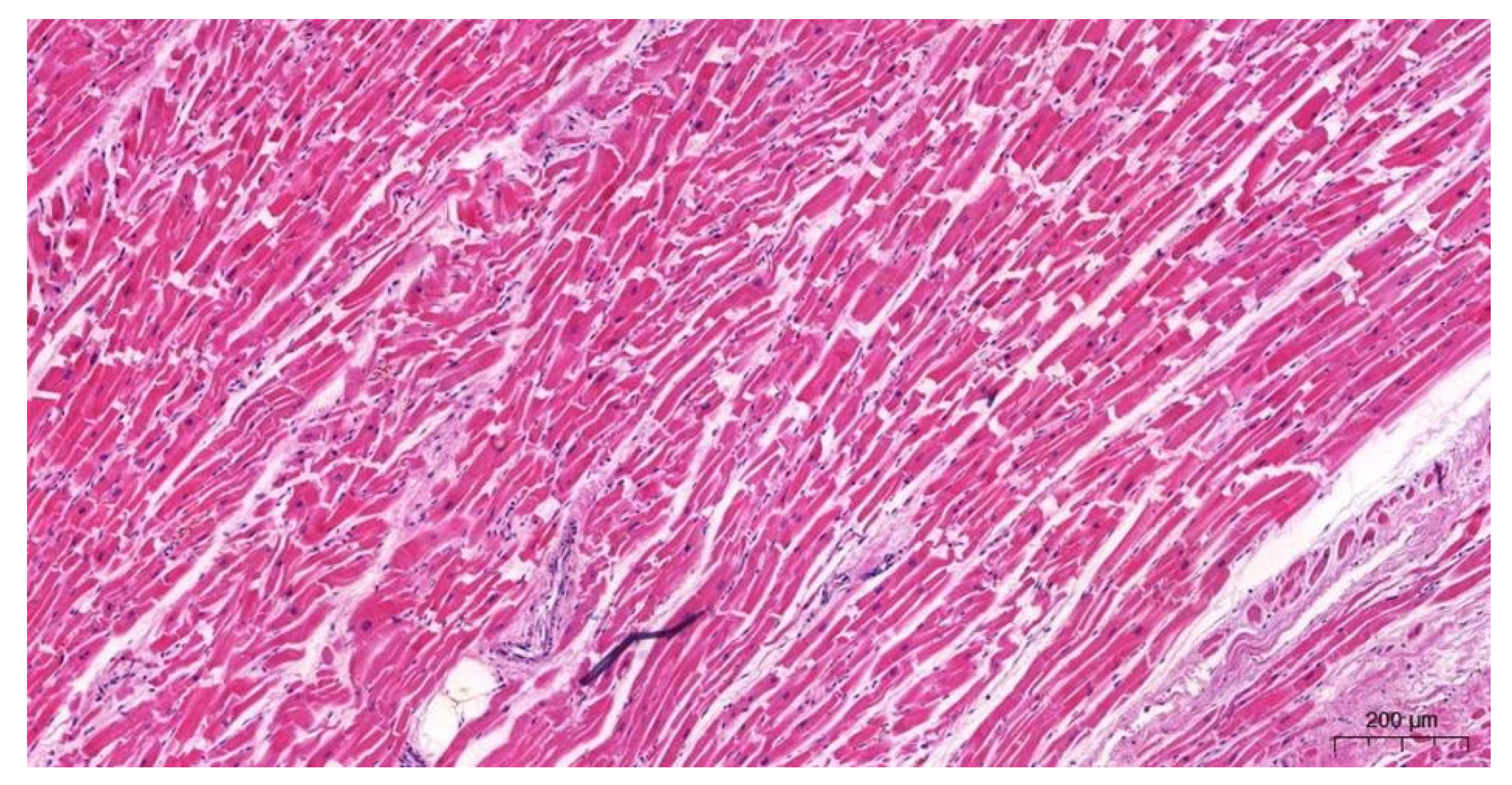
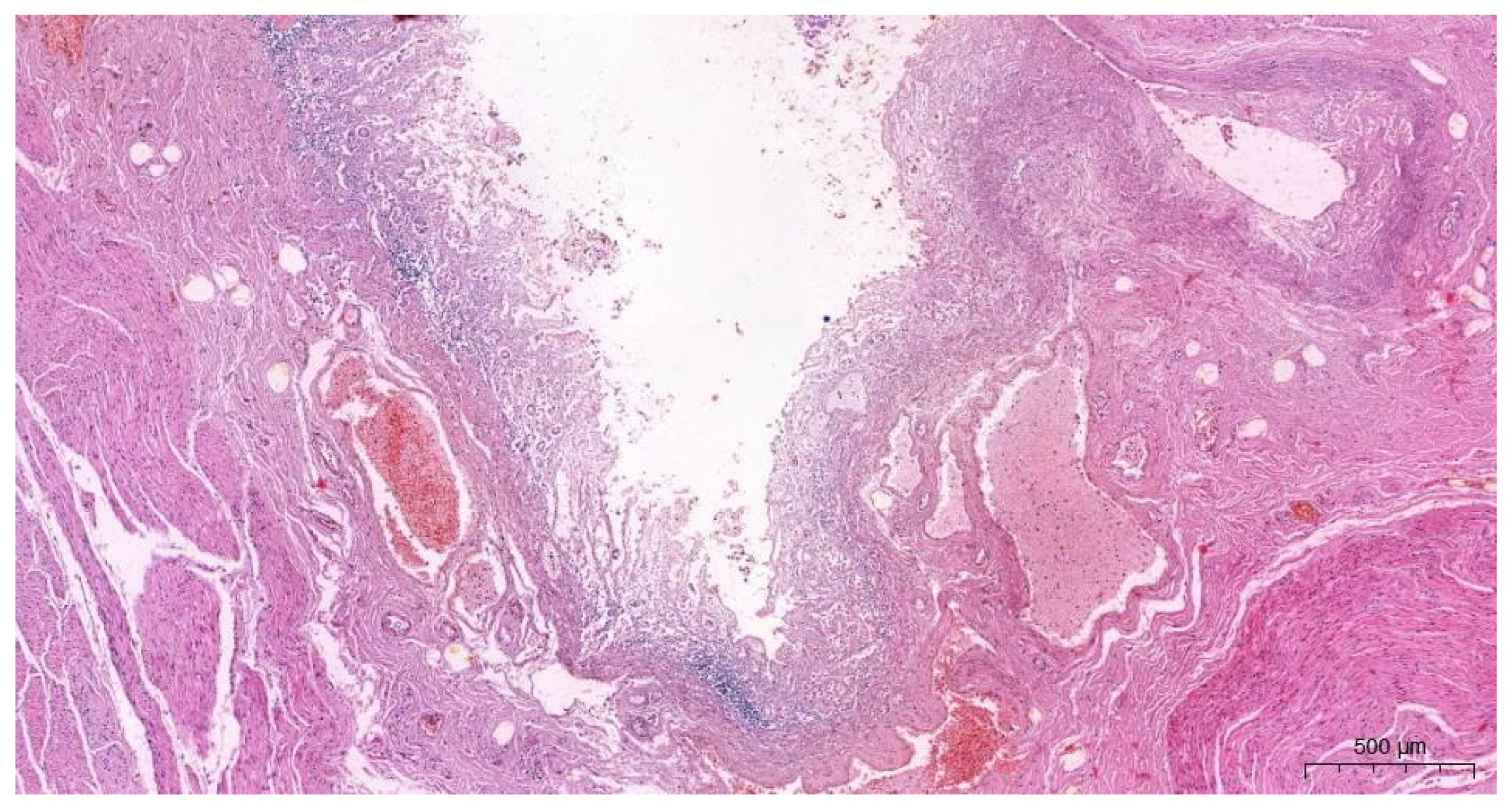
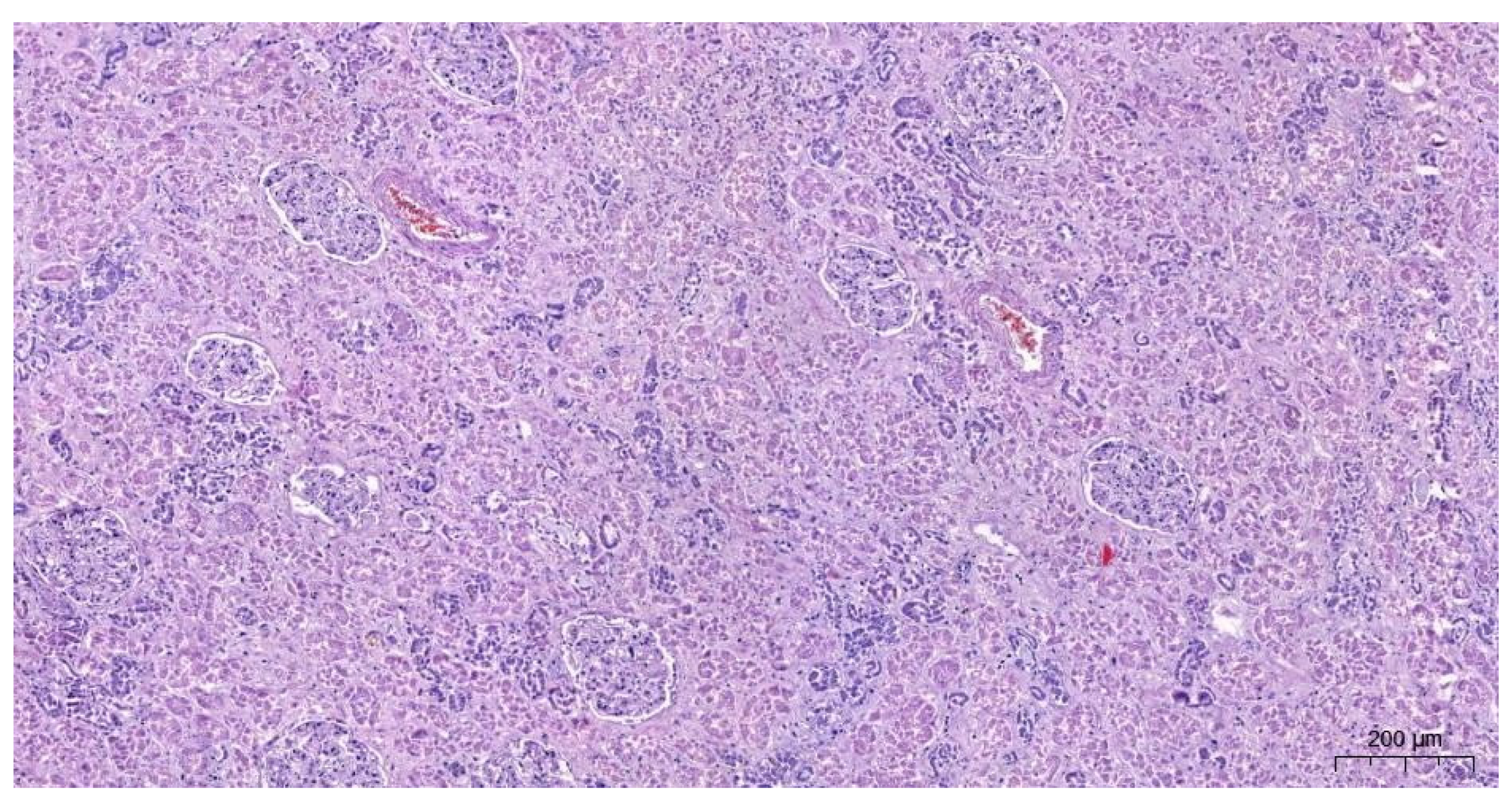
2.2.3. The Microscopic Examinations
2.2.4. Results of Toxicological Analyzes
3. Discussion
4. Conclusions
5. Impact Statement
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tournas, V.H. Microbial contamination of select dietary supplements. J. Food Saf. 2009, 29, 430–442. [Google Scholar] [CrossRef]
- Benedict, K.; Chiller, T.M.; Mody, R.K. Invasive Fungal Infections Acquired from Contaminated Food or Nutritional Supplements: A Review of the Literature. Foodborne Pathog. Dis. 2016, 13, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Genuis, S.J.; Schwalfenberg, G.; Siy, A.K.J.; Rodushkin, I. Toxic Element Contamination of Natural Health Products and Pharmaceutical Preparations. PLoS ONE 2012, 7, e49676. [Google Scholar] [CrossRef]
- Saper, R.B.; Phillips, R.S.; Sehgal, A.; Khouri, N.; Davis, R.B.; Paquin, J.; Thuppil, V.; Kales, S.N. Lead, Mercury, and Arsenic in US- and Indian-Manufactured Ayurvedic Medicines Sold via the Internet. JAMA 2008, 300, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Tucker, J.; Fischer, T.; Upjohn, L.; Mazzera, D.; Kumar, M. Unapproved Pharmaceutical Ingredients Included in Dietary Supplements Associated With US Food and Drug Administration Warnings. JAMA Netw. Open 2018, 1, e183337. [Google Scholar] [CrossRef]
- Holmgren, P.; Lotta Nordén-Pettersson, L.; Johan Ahlner, J. Caffeine fatalities—Four case reports. Forensic Sci. Int. 2004, 139, 71–73. [Google Scholar] [CrossRef] [PubMed]
- Magdalan, J.; Zawadzki, M.; Skowronek, R.; Czuba, M.; Porębska, B.; Sozański, T.; Szpot, P. Nonfatal and fatal intoxications with pure caffeine—Report of three different cases. Forensic Sci. Med. Pathol. 2017, 13, 355–358. [Google Scholar] [CrossRef]
- Cornelis, M.C.; El-Sohemy, A. Coffee, caffeine, and coronary heart disease. Curr. Opin. Lipidol. 2007, 18, 13–19. [Google Scholar] [CrossRef]
- Ullrich, S.; de Vries, Y.; Kühn, S.; Repantis, D.; Dresler, M.; Ohla, K. Feeling smart: Effects of caffeine and glucose on cognition, mood and self-judgment. Physiol. Behav. 2015, 151, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Arnaud, M.J. Pharmacokinetics and metabolism of natural methylxanthines in animal and man, in Methylxanthines. Handb. Exp. Pharmacol. 2011, 200, 33–91. [Google Scholar]
- Grosso, L.M.; Bracken, M.B. Caffeine metabolism, genetics and perinatal outcomes: A review of exposure assessment considerations during pregnancy. Ann. Epidemiol. 2005, 15, 460–466. [Google Scholar] [CrossRef]
- Yamamoto, T.; Yoshizawa, K.; Kubo, S.; Emoto, Y.; Hara, K.; Waters, B.; Umehara, T.; Murase, T.; Ikematsu, K. Autopsy report for a caffeine intoxication case and review of the current literature. J. Toxicol. Pathol. 2015, 28, 33–36. [Google Scholar] [CrossRef]
- Banerjee, P.; Ali, Z.; Levine, B.; Fowler, D.R. Fatal caffeine intoxication: A series of eight cases from 1999 to 2009. J. Forensic Sci 2014, 59, 865–868. [Google Scholar] [CrossRef]
- Musgrave, I.F.; Farrington, R.L.; Hoban, C.; Byard, R.W. Caffeine toxicity in forensic practice: Possible effects and under-appreciated sources. Forensic Sci. Med. Pathol. 2016, 12, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Andrade, A.; Sousa, C.; Pedro, M.; Fernandes, M. Dangerous mistake: An accidental caffeine overdose. Case Rep. 2018, 2018. [Google Scholar] [CrossRef] [PubMed]
- James, J.E. Critical review of dietary caffeine and blood pressure: A relationship that should be taken more seriously. Psychosom. Med. 2004, 66, 63–71. [Google Scholar] [CrossRef]
- Caffeine in Food and Dietary Supplements: Examining Safety: Workshop Summary. Washington (DC): National Academies Press (US). 2014. Available online: https://www.ncbi.nlm.nih.gov/books/NBK202230/ (accessed on 27 December 2021).
- Szpak, A.; Allen, D. A case of acute suicidality following excessive caffeine intake. J. Psychopharmacol. 2012, 26, 1502–1510. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.W.; Holmgren, A. Concentration distributions of the drugs most frequently identified in post-mortem femoral blood representing all causes of death. Med. Sci. Law 2009, 49, 257–273. [Google Scholar] [CrossRef]
- Jones, A.W. Review of Caffeine-Related Fatalities along with Postmortem Blood Concentrations in 51 Poisoning Deaths. J. Anal. Toxicol. 2017, 41, 167–172. [Google Scholar] [CrossRef]
- Schulz, M.; Schmoldt, A. Therapeutic and toxic blood concentrations of more than 800 drugs and other xenobiotics. Pharmazie 2003, 58, 447–474. [Google Scholar]
- Bonsignore, A.; Sblano, S.; Pozzi, F.; Ventura, F.; Dell’Erba, A.; Palmiere, C. A case of suicide by ingestion of caffeine. Forensic Sci. Med. Pathol. 2014, 10, 448–451. [Google Scholar] [CrossRef][Green Version]
- Thelander, G.; Jonsson, A.K.; Personne, M.; Forsberg, G.S.; Lundqvist, K.M.; Ahlner, J. Caffeine fatalities—do sales restrictions prevent intentional intoxications? Clin. Toxicol. 2010, 48, 354–358. [Google Scholar] [CrossRef]
- Pelchovitz, D.J.; Goldberger, J.J. Caffeine and cardiac arrhythmias: A review of the evidence. Am. J. Med. 2011, 124, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, M.K.F.; Gavioli, E.C.; Rosa, L.S.; Soares-Rachetti, V.D.P.; Lobão-Soares, B. Craving espresso: The dialetics in classifying caffeine as an abuse drug. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2018, 391, 1301–1318. [Google Scholar] [CrossRef] [PubMed]
- Jabbar, S.B.; Hanly, M.G. Fatal caffeine overdose: A case report and review of literature. Am. J. Forensic Med. Pathol. 2013, 34, 321–324. [Google Scholar] [CrossRef]
- Poussel, M.; Kimmoun, A.; Levy, B.; Gambier, N.; Dudek, F.; Puskarczyk, E.; Poussel, J.-F.; Chenuel, B. Fatal cardiac arrhythmia following voluntary caffeine overdose in an amateur body-builder athlete. Int. J. Cardiol. 2013, 166, e41–e42. [Google Scholar] [CrossRef] [PubMed]
- Fredholm, B.B.; Bättig, K.; Holmén, J.; Nehlig, A.; Zvartau, E.E. Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol. Rev. 1999, 51, 83–133. [Google Scholar] [PubMed]
- Kidd, M.; Hauso, O.; Drozdov, I.; Gustafsson, B.I.; Modlin, I.M. Delineation of the chemomechanosensory regulation of gastrin secretion using pure rodent G cells. Gastroenterology 2009, 137, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.; Hell, J.; Liszt, K.I.; Dresel, M.; Pignitter, M.; Hofmann, T.; Somoza, V. Identification of beer bitter acids regulating mechanisms of gastric acid secretion. J. Agric. Food Chem. 2012, 60, 1405–1412. [Google Scholar] [CrossRef]
- Schubert, M.L. Gastric secretion. Curr. Opin. Gastroenterol. 2004, 20, 519–525. [Google Scholar] [CrossRef]
- Lieu, M.T.; Layoun, M.E.; Dai, D.; Hoo, G.W.S.; Betancourt, J. Tension hydropneumothorax as the initial presentation of Boerhaave syndrome. Respir. Med. Case Rep. 2018, 25, 100–103. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szeremeta, M.; Sackiewicz, A.; Drobuliak, P.; Reszeć-Giełażyn, J.; Niemcunowicz-Janica, A. Rare Complications of Fatal Caffeine Intoxication. Forensic Sci. 2022, 2, 144-154. https://doi.org/10.3390/forensicsci2010011
Szeremeta M, Sackiewicz A, Drobuliak P, Reszeć-Giełażyn J, Niemcunowicz-Janica A. Rare Complications of Fatal Caffeine Intoxication. Forensic Sciences. 2022; 2(1):144-154. https://doi.org/10.3390/forensicsci2010011
Chicago/Turabian StyleSzeremeta, Michał, Adam Sackiewicz, Petra Drobuliak, Joanna Reszeć-Giełażyn, and Anna Niemcunowicz-Janica. 2022. "Rare Complications of Fatal Caffeine Intoxication" Forensic Sciences 2, no. 1: 144-154. https://doi.org/10.3390/forensicsci2010011
APA StyleSzeremeta, M., Sackiewicz, A., Drobuliak, P., Reszeć-Giełażyn, J., & Niemcunowicz-Janica, A. (2022). Rare Complications of Fatal Caffeine Intoxication. Forensic Sciences, 2(1), 144-154. https://doi.org/10.3390/forensicsci2010011






