Abstract
Light-curing units (LCUs) are often subject to clinician-determined factors such as infection control barriers (ICBs) and different positionings of the light tip that may reduce their radiant exposure. The objective of this study was to investigate the individual and cumulative effects of ICBs and LCU positioning on light output. One LCU was used, in combination with five different ICBs and five different distances and angles. ICBs were also tested when placed correctly to manufacturers’ guidelines, and with creases or seams obstructing the light tip. All variables were tested in isolation and in combination with other variables. Measurements were taken from a laboratory-grade spectrometer, giving values of radiant exposure, irradiance and spectral emission. All ICBs, angles and distances showed significant reductions in light output compared to the control (p < 0.001). With increasing angle and distance, the light output was decreased further, with the greatest reduction of 80.6% from the control seen at 40° and 8 mm with an incorrectly placed ICB. When used with an ICB, an increasing angle also showed a protective relationship on the light output. When ICBs are used or when an increase in distance/angle is unavoidable, clinicians should consider compensating for the loss in radiant exposure by increasing curing times.
1. Introduction
Light-curing units (LCUs) are used daily in almost every dental practice as they are required for resin-based composites, luting cements and adhesives. The output from these curing units is very important as insufficient light or an incorrect light wavelength can mean that materials may not have their intended properties. This can lead to premature failure due to marginal leakage, fracture or increased wear [1,2,3,4,5,6].
The measurement of the quality of light coming from these units was historically carried out with dental radiometers. However, many studies have found that radiometers are inherently inaccurate and can give varying results for the same light-curing unit [7,8,9,10]. This is also due to the fact that radiometers tend to give a single average value, and therefore, light beam inhomogeneity is not taken into consideration. Currently, the literature agrees that light output should be measured by a laboratory-grade spectrometer as it takes into account the wavelength of the light, irradiance at different points in time and radiant exposure [11,12,13,14]. Additionally, information on the light beam profile of the curing lights should be included in order to show any hot and cold spots as well as potential discrepancies in the light quality received by different areas of the composite resin material [11]. Measuring radiant exposure accurately is also clinically relevant as each brand of composite resin needs to reach a certain radiant exposure to adequately cure, and studies have reported that the majority of commercially available composite resins cure at 16 to 20 J/cm2 [15,16,17].
LCUs are used intraorally, and therefore, they are classed as a semi-critical instrument, meaning that they can cause the cross-transmission of infections between patients if not sterilised properly. This is especially relevant with the present coronavirus (COVID-19) situation where people have become more aware of infection control protocols and their importance [18]. Therefore, infection control barriers (ICBs), which are disposable materials, can be used to cover the light tip of curing units. However, various manufacturers produce ICBs with different barrier thicknesses and opacities, and variation in placement by clinicians may have an adverse effect on the light output, as ICBs can partially block the light and increase its dispersion [19,20,21,22,23,24].
Along with ICBs, there are other factors controlled by the clinician that can have an adverse effect on light output. The distance and angulation of the light tip to the surface can also diminish the amount of light reaching the specimen. Past in vitro studies have assessed the effect of distances of LCUs from the spectrometer sensor and reported that an increase in distance caused a decrease in the radiant exposure [21,25,26,27]. The correct positioning of the LCU also takes into account the tilt angle. A previous in vitro study has shown that the deviation of a 20° curing angle from the perpendicular position resulted in as much as a 31% drop in light output [21]. Clinically, the angle is a variable that is heavily dependent on the design of LCUs and the location of the restoration [28,29,30]. Patients with limited mouth opening, deep posterior restorations, and a bulky LCU can pose a greater risk for placing the light tip incorrectly.
The current literature has assessed the individual effect of changes in the distances and angles on the efficiency of LCUs. With the increase in the importance of cross-infection control, using disposable ICBs has become a common practice. While it is acknowledged that there may be some additional impacts of ICBs on the light output, there is still a lack of well-designed in vitro studies using appropriate measurement methods to show the cumulative effects of all these variables. Therefore, the objective of this study was to investigate both the individual and cumulative effects of ICBs, distance and light tip angulation on the quality of light output from a dental LCU.
2. Materials and Methods
The MARC patient simulator (BlueLight Analytics Inc., Halifax, NS, Canada) was used to measure light output. It is a laboratory-grade spectrometer system integrated into a phantom simulation head. It has a sensor positioned 1 mm deep between the maxillary central incisors in a class III simulated restoration. All measurements were output to a dedicated computer with values recorded for irradiance over time, radiant exposure as well as the wavelength of the LCU.
A single LED LCU (SmartLite Pro, Dentsply Sirona, Charlotte, NC, USA) was used. Light beam profile, wavelength and other relevant information was provided by the manufacturer in order to properly assess this LCU—tip diameter: 10 mm; stated irradiance: 1200 mW/cm2; emission spectrum: 450–480 nm (peak at 465 nm); light source: modular LED. The output stability of this LCU was measured prior to and during the investigation to ensure that there was no significant loss of power over the experimental phase. It was fully charged and activated for a 10 s curing time and repeated 20 times without recharging to measure the stability of the output.
Five different ICBs (Pinnacle Cure Sleeve, CMS Dental Sleeve, Aluro Camrex Disposable Sleeve, Dentsply SmartLite Sleeve and cling wrap) were used. Each barrier was first fitted according to the manufacturer’s instructions, and then again fitted incorrectly with seams or creases over the light tip to simulate possible clinical situations (Figure 1).
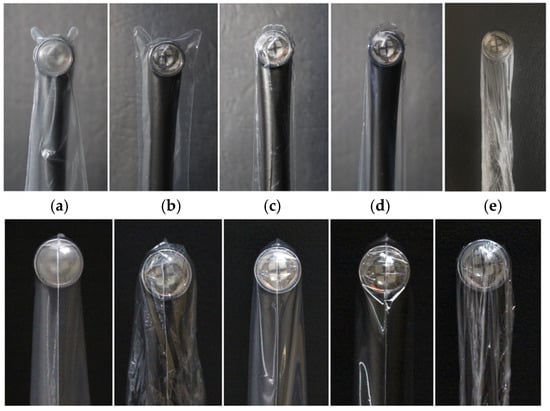
Figure 1.
Examples of five different ICBs placed correctly (above) and incorrectly (below) on SmartLite Pro LCU: (a) Pinnacle Cure Sleeve, (b) CMS Dental Sleeve, (c) Aluro Camrex Disposable Sleeve, (d) Dentsply SmartLite Sleeve and (e) cling wrap.
Light output was measured at distances of 0 (control), 2, 4, 6 and 8 mm from the top surface of the anterior sensor. As the anterior sensor was positioned 1 mm deep, the control represented 1 mm, and there was a 2 mm increase every increment for testing. These distances were chosen as they are readily seen in clinical situations. For example, 0 to 2 mm represents anterior restorations, whereas 4 mm is an average depth of a class I occlusal restoration, and 6 to 8 mm can be seen in a posterior class II cavity. Distances were standardised using a custom-made LCU mount that stabilised the light tip at the specified distance for all repeated tests (Figure 2).
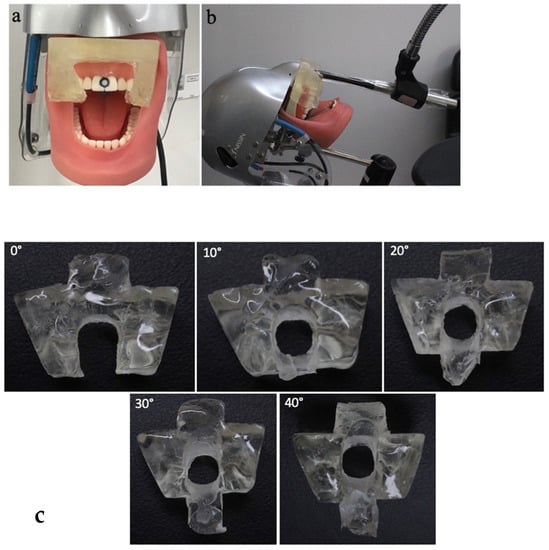
Figure 2.
(a) MARC spectrometer with custom jig mount, (b) adjustable arm holding the SmartLite Pro LCU, guided to the sensor with the custom jig, (c) interchangeable custom-made silicone jigs to fit the larger template (shown in (a)) to standardise all tested angles.
Output was measured at different tilt angles of 0 (control), 10, 20, 30 and 40 degrees from the perpendicular position to the anterior sensor. These were standardised by using clear silicone jigs (Exaclear, GC, Tokyo, Japan) which were custom made to fit the LCU at each angle (Figure 2c).
The control used was light output from the LCU at a distance of 0 mm, a tilt angle of 0° and used without an ICB. Variables were compared against the control, as well as barriers, angles and distances being tested in conjunction with each other, to determine both the individual and cumulative effects of these variables.
Statistical analysis was undertaken with SPSS (version 26, IBM, Armonk, NY, USA). All variables were measured over a curing time of 10 s, and 10 repeats of each test were carried out. A Kruskal–Wallis stepwise step down analysis of the data was carried out for pairwise comparison, with multiple Mann–Whitney U tests to determine significance between groups. The significant level of difference was set at p < 0.05.
3. Results
At baseline, with a fully charged battery, the SmartLite Pro LCU was outputting a mean irradiance of approximately 1290 mW/cm2 and a radiant exposure of 13.1 J/cm2. Throughout testing, the output stability was regularly assessed under the above-mentioned control conditions, and it showed no significant reduction in light output throughout testing.
When ICBs were placed according to manufacturers’ instructions, different ICBs reduced the light output by 0.6 to 1.5 J/cm2 and with a 5 to 11% reduction compared to the control (p < 0.001) (Figure 3). Pinnacle Cure Sleeve was the most opaque barrier tested and showed the largest decrease in the mean radiant exposure of a group that had correctly placed barriers at 0° and 0 mm from the sensor. At this position, the ICB with the least effect on radiant exposure and mean irradiance was cling wrap, followed closely by the Aluro Camrex Sleeve and the SmartLite barrier. However, with an increase in distance to 8 mm, the SmartLite barrier had a much more marked effect on light output and showed the biggest reduction at this distance (Figure 3).
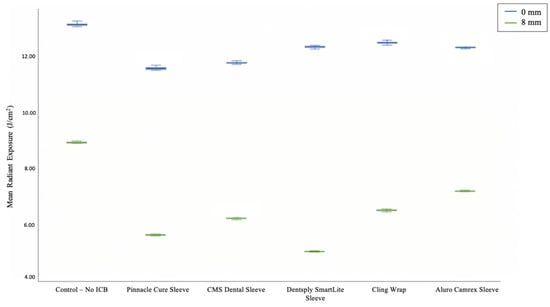
Figure 3.
Box plot comparing ICB mean radiant exposure after 10 s (J/cm2) of correctly placed ICB groups at 0 mm against each other, and against ICB groups at 8 mm.
Placing each barrier incorrectly, there was a further reduction of 3.7% for the SmartLite barrier and 2.8% for cling wrap (p < 0.001). However, there was a slight increase in light output for the Pinnacle Cure Sleeve, CMS Dental Sleeve and Aluro Camrex Sleeve by 2.1%, 4.9% and 1.2%, respectively (p < 0.001) (Table 1).

Table 1.
Radiant exposure (J/cm2) and percentage difference correct vs. incorrect ICB groups.
Distance as an individual variable showed a significant reduction in light output at every tested distance compared to the control (p < 0.001). The initial increase of 2 mm from the control gave a significant reduction in light output with a 12.4% loss of radiant exposure when distance was assessed in isolation (Table 2). However, this increased to 16.5% when looking at 2 mm distances across all test groups over every angle and ICB. The largest total decrease in radiant exposure occurred at 8 mm, which, over all test groups, showed an average of 47.5% reduction in radiant exposure (Table 2).

Table 2.
Radiant exposure after 10 s (J/cm2) at control, and percentage reduction against the control with increasing distances per correctly placed ICB groups.
The effect of increasing angle was seen to be statistically significant at every angle compared to the control (p < 0.001). The biggest decrease in radiant exposure was seen when increasing the angle from 30 to 40°, with radiant exposure dropping by 2.25 J/cm2 (Table 3). An increase of 40° from the control (0°) showed a total energy decrease of almost 40% (p < 0.001) (Table 3). Across all test groups, an increase in the angle always caused a reduction in light output. With increasing angle, across all ICBs, the smallest reduction was a 4.7% drop in radiant exposure at 10°. The effect of angle increase on radiant exposure was not linear and tended to vary between different angulations. The increase in angle from 20 to 30° often showed the smallest decrease in radiant exposure across test groups (Table 3).

Table 3.
Radiant exposure after 10 s (J/cm2) at control, and percentage reduction against the control with increasing angulation per correctly placed ICB groups.
The presence of an ICB decreased the adverse effect of increasing tip angulation on radiant exposure (Table 3). For the 10° angulation group without an ICB, there was an 11.8% reduction in radiant exposure, whereas with an ICB, the reduction in radiant exposure ranged from only 1 to 7.8% (Table 3). This trend was seen for all tip angulations, where the control group without the ICB consistently showed a greater reduction in light output per angle compared to the ICB groups.
Almost the opposite effect was seen when looking at ICBs’ effect on the reduction in light output with increasing distance. With an increase in distance from 0 to 4 mm, there was a trend showing an exacerbated effect of ICB on the reduction in radiant exposure, with the exception of the CMS barrier (Table 2). This trend was more established at 6 mm and 8 mm, with a consistently greater decrease in ICB groups compared to those without an ICB. This trend showed that with increasing distance, ICBs were seen to further exacerbate the effect of distance on light reduction.
Data on the cumulative effect of angle, distance, and infection control barriers were also gathered in this study. Compared to the control, the correctly placed Pinnacle Cure Sleeve at a distance on 4 mm and angulation of 20° showed a cumulative decrease of 5.33 J/cm2 (Table 4). When looking at the impact of these factors individually, the ICB showed a 0.84 J/cm2 decrease, 20° angulation had a 1.21 J/cm2 decrease, and a distance of 4 mm had a 1.57 J/cm2 decrease. The combined effect of these variables in isolation was 3.62 J/cm2, which was less than the cumulative effect when all the variables are seen together. This trend was seen at every angle and distance for the Pinnacle barrier and for cling wrap, in which the cumulative effect of the variables was always greater than the combined individual effects. For all other barriers, there was no consistent trend seen (Table 4).

Table 4.
Effect of individual factors on radiant exposure after 10 s (J/cm2) combined, compared to the cumulative effect of all test variables.
4. Discussion
The hypothesis of this research was that the presence of an ICB in conjunction with the increase in distance and angle from the sensor would have significant individual and cumulative diminutive effects on the quality of light output from the LCU. This hypothesis can be accepted as when compared to the control, there was a statistically significant reduction in light output at every test variable.
LCUs when used with an ICB significantly reduced radiant exposure. This was in agreement with other literature showing similar results with light reduction when using ICBs [19,24]. Variations in light reduction between different barriers may be attributed to different barrier thicknesses, opacities, and materials. The opaquest barrier, Pinnacle Cure Sleeve, showed the greatest reduction in radiant exposure at the control position, whereas cling wrap showed the least. Increased opacity leads to less light penetrating through the barrier, and hence, less light reaching the sensor. Barrier thickness is also a contributing factor, which can also be seen with other clear barriers also showing a significant reduction in light output [31,32,33].
There is a risk that ICBs are not placed according to manufacturers’ instructions, and creases or seams may be placed over the tip. In the current study, the results showed the inadequate placement of the ICB did not always cause a further reduction in light output. In the case of the CMS Dental Sleeve, there was an increase in light output of 4.9% when placed incorrectly compared to correctly. This could possibly have been due to an increased refraction of light. As the SmartLite Pro light tip was convex, this feature might have diverged the light away from the sensor, and a seam of the ICB might have encouraged more light to converge towards the sensor. This result was contradictory to other research which found a consistent further decrease in light output when the barrier was placed incorrectly [24]. As it was not possible to quantify how incorrectly a barrier was placed, the degree to which seams or wrinkles played a role in affecting light output was difficult to measure. However, increasing barrier thickness has been shown to have a diminutive effect; thus, clinicians should be aware of this when placing ICBs [32].
An increase in distance from the resin-based composite material is arguably the most commonly seen factor in light curing [21,26]. As an individual variable, there was a significant reduction in radiant exposure at all investigated distances. Distance across all groups showed a fairly linear reduction, with around a further 10% decrease in radiant exposure with every 2 mm increase, after the initial 16.5% decrease from 0 to 2 mm (Table 2). Similar trends were seen in another study regarding the impact of increasing the distance of LCUs [26]. The diminutive effect of distance on radiant exposure was mostly due to the divergence or spread of the light beam, thus resulting in less light ultimately reaching the sensor [25].
Distances of 8 mm can be frequently encountered in restorative dentistry [34]. Almost a 50% reduction in radiant exposure was found at this distance, and therefore, the curing time needed to increase from 12.4 s to over 20 s to reach 16 J/cm2. This shows the importance of why clinicians must be aware of the adverse effect of increases in LCU distances so that they compensate for this in the curing time.
The results in the current study suggested that the effect of distance on radiant exposure could be further exacerbated by the presence of an ICB. As the increase in the distance reduced light output by the increased divergence of the light beam, ICBs may enhance the spread of the light beam, causing more light to miss the sensor. Along with blocking the light, these influences on the radiant exposure showed a significant loss of light compared to the control. A further decrease with ICBs was in line with results seen in the past literature, with one article reporting an additional 7 to 10% loss of light output with ICBs [21].
Light tip angulation was also investigated and showed significant reductions at all angles. Altering the angle of the light tip is often seen in the clinical situation but is often easily overlooked. When working on posterior teeth, it can be difficult to use the LCU at a perpendicular angle due to reduced mouth opening, bulky LCUs or hard-to-reach restorations. At an angle of 10°, a reduction of 11.8% from the control was observed, which showed a further reduction to almost 40% loss at a 40°. This demonstrates the amount of light that is missing the sensor and consequently the composite resin material when the angle is increased. However, the amount of light missing the sensor is not the only issue when dealing with light tip angulation. Often, the curing surface is not as smooth as the sensor in this investigation was, and thus, shadows can form in the undercuts created by the tip angle [35]. These shadow areas will often be at the margins of the composite restoration, possibly having detrimental effects on the radiant exposure these areas receive. Sometimes, an increase in tip angulation is unavoidable in clinical situations. In these cases, the clinician should recognise the potential shadows and light decrease that may occur and perform additional curing from another position for an adequate time that allows sufficient radiant exposure for all aspects of the composite resin material.
When used in conjunction with ICBs, the changes in the angle showed less reduction between incremental increases in the angle. This was consistent across all ICBs. In some cases, the ICB showed a “protective” effect on the radiant exposure at certain angles compared to the control. This relationship has not been reported in the prior literature. A possible explanation of this may be that the speed of light will decrease when entering the plastic material, and thus can show a change in direction if the incidence angle is not perpendicular. This may refract the light, giving a more converging angle and allowing more light to reach the sensor. One limitation of this study was that only one LCU was investigated, the Dentsply SmartLite Pro, which has a convex light tip. The possible protective effect of ICBs may not be seen with other LCUs with varying light tips and light beam profiles, and further research is needed to see if this observed effect can be generalised.
Distance, angle and ICBs have been shown to cause statistically significant reductions in light output when observed in isolation. However, the cumulative effect of all three test variables together has not been reported in the past literature. This study aimed to investigate whether the combined effect of these variables individually showed a greater or lesser reduction in radiant exposure than the cumulative effect of variables together. This was achieved by assessing the effect of each variable in isolation and comparing it to the effect of all variables seen together. The observed effect for one of the ICBs (Pinnacle Cure Sleeve) showed a consistently greater effect of the cumulative variables compared to the combined individual variables (Table 4). This demonstrates that these factors possibly act to exacerbate one another, giving a greater diminutive effect when seen together. This trend was seen at every angle and distance for the Pinnacle barrier and for cling wrap, in which the cumulative effect of the variables was greater than the combined individual effects. Across all other barriers, there was no consistent trend where the cumulative variables showed a greater effect or vice versa (Table 4). At the greatest investigated angle and distance, combined with the presence of the Pinnacle ICB, radiant exposure decreased by over 70%. Any significant decrease in the light output is clinically relevant as it can result in the inadequate polymerisation of composite resin restorative materials, which will lead to the deterioration of restorative margins and reduced mechanical properties of restorations, requiring patients to have the treatment repeated due to failure [5]. Increases in curing time will be needed to compensate for this loss, and curing for this length of time will the increase chair time for these procedures and also may induce implications for pulpal health [36].
The limitations of this study include the fact that only one LCU was tested, as well as only a handful of the ICBs currently available on the market. However, there is still clinically significant value in this study, as several combinations of commonly encountered variables controlled by clinicians such as distances, angles and the usage of ICBs with LCUs have been assessed. While the standardisation within the testing phase of the current study included a single operator with blue blocker glasses using a stable mechanical arm to hold the LCU and custom jigs to guide the light tip and standardise the angulation, there is a minor risk that some minimal movement of the LCU may have occurred when the button was pressed to begin the curing cycle. A possible recommendation for future studies is the development of remote activation to allow the LCU to be fixated at all times.
Future studies should observe the relationship between cumulative variables of angle, distance and ICBs and their effect on light beam profiles. As cling wrap was shown to have the least effect on light output, research should also be carried out regarding the efficacy of cling wrap as an infection control barrier to investigate whether a single layer of cling wrap is sufficient for cross-infection control.
5. Conclusions
This research is significant, as reduced radiant exposure from these clinician-determined variables has the potential to cause increased the failure of restorations. Within the limitations of this study, it can be concluded that:
- When ICBs are used or when an increase in distance/angle is unavoidable, clinicians should consider compensating for the loss in radiant exposure by increasing curing times.
- The increased opacity and thickness of ICBs reduces radiant exposure to a greater extent. When opting to use ICBs for infection control, a thinner, clear barrier has less effect on light output.
- Manufacturers’ guidelines should be followed in regard to the radiant exposure needed to cure particular resin-based dental materials. LCUs should also be tested regularly with a laboratory-grade spectrometer to ensure adequate radiant exposures are being produced.
This research can be used to inform clinical practice guidelines on the use of LCUs and ICBs to aid clinicians in obtaining adequately polymerised dental materials.
Author Contributions
Conceptualisation, S.M. and J.v.d.Z.; methodology, S.M. and J.v.d.Z.; formal analysis, S.M. and J.v.d.Z.; investigation, J.v.d.Z.; data curation, J.v.d.Z.; writing—original draft preparation, S.M. and J.v.d.Z.; writing—review and editing, S.M., J.v.d.Z. and A.T.-S.; supervision, S.M. and A.T.-S.; project administration, S.M. and A.T.-S.; funding acquisition, S.M. and J.v.d.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the New Zealand Dental Research Foundation, New Zealand and RC Tonkin Summer Studentship, University of Otago, New Zealand.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank 3M (New Zealand) and BlueLight Analytics Inc for the loan of the MARC patient simulator unit and Dentsply Sirona (New Zealand) for the loan of the light-curing unit.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Calheiros, F.C.; Daronch, M.; Rueggeberg, F.A.; Braga, R.R. Degree of conversion and mechanical properties of a BisGMA:TEGDMA composite as a function of the applied radiant exposure. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 84, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Bhamra, G.S.; Fleming, G.J. Influence of halogen irradiance on short- and long-term wear resistance of resin-based composite materials. Dent. Mater. 2009, 25, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Rueggeberg, F.A.; Cole, M.A.; Looney, S.W.; Vickers, A.; Swift, E.J. Comparison of manufacturer-recommended exposure durations with those determined using biaxial flexure strength and scraped composite thickness among a variety of light-curing units. J. Esthet. Restor. Dent. 2009, 21, 43–61. [Google Scholar] [CrossRef] [PubMed]
- Hammouda, I.M. Effect of light-curing method on wear and hardness of composite resin. J. Mech. Behav. Biomed. Mater. 2010, 3, 216–222. [Google Scholar] [CrossRef]
- Jadhav, S.; Hegde, V.; Aher, G.; Fajandar, N. Influence of light curing units on failure of directcomposite restorations. J. Conserv. Dent. 2011, 14, 225–227. [Google Scholar] [CrossRef]
- Souza-Junior, E.; Souza-Régis, M.; Alonso, R.; Freitas, A.; Sinhoreti, M.; Cunha, L. Effect of the curing method and composite volume on marginal and internal adaptation of composite restoratives. Oper. Dent. 2011, 36, 231–238. [Google Scholar] [CrossRef]
- Rueggeberg, F. Precision of hand-held dental radiometers. Quintessence Int. 1993, 24, 391–396. [Google Scholar]
- Price, R.B.; Labrie, D.; Kazmi, S.; Fahey, J.; Felix, C.M. Intra- and inter-brand accuracy of four dental radiometers. Clin. Oral Investig. 2012, 16, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Shimokawa, C.A.K.; Harlow, J.E.; Turbino, M.L.; Price, R.B. Ability of four dental radiometers to measure the light output from nine curing lights. J. Dent. 2016, 54, 48–55. [Google Scholar] [CrossRef]
- Giannini, M.; André, C.B.; Gobbo, V.C.; Rueggeberg, F.A. Accuracy of irradiance and power of light-curing units measured with handheld or laboratory grade radiometers. Braz. Dent. J. 2019, 30, 397–403. [Google Scholar] [CrossRef]
- Price, R.; Ferracane, J.; Shortall, A. Light-curing units: A review of what we need to know. J. Dent. Res. 2015, 94, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Shortall, A.C.; Felix, C.J.; Watts, D.C. Robust spectrometer-based methods for characterizing radiant exitance of dental LED light curing units. Dent. Mater. 2015, 31, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Harlow, J.; Sullivan, B.; Shortall, A.; Labrie, D.; Price, R. Characterizing the output settings of dental curing lights. J. Dent. 2016, 44, 20–26. [Google Scholar] [CrossRef]
- Roulet, J.-F.; Rocha, M.G.; Shen, C.; Khudhair, M.M.; De Oliveira, D.C.R.S. Beam profile characterization of a dental light curing unit using a spectrometer-based method. Stomatol. EDU J. 2018, 5, 84–91. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Asmussen, E. Resin composite properties and energy density of light cure. J. Dent. Res. 2005, 84, 659–662. [Google Scholar] [CrossRef]
- Gritsch, K.; Souvannasot, S.; Schembri, C.; Farge, P.; Grosgogeat, B. Influence of light energy and power density on the microhardness of two nanohybrid composites. Eur. J. Oral Sci. 2008, 116, 77–82. [Google Scholar] [CrossRef]
- Jain, L.; Mehta, D.; Meena, N.; Gupta, R. Influence of light energy density, composite type, composite thickness, and postcuring phase on degree of conversion of bulk-fill composites. Contemp. Clin. Dent. 2018, 9, 147–152. [Google Scholar] [CrossRef]
- Bizzoca, M.E.; Campisi, G.; Lo Muzio, L. COVID-19 pandemic: What changes for dentists and oral medicine experts? A narrative review and novel approaches to infection containment. Int. J. Environ. Res. Public Health 2020, 17, 3793. [Google Scholar] [CrossRef]
- Brokos, I.; Turner, S.; Santini, A. The effect of disposable infection control sleeves on the total energy delivered by dental LCUs. Prim. Dent. J. 2012, 1, 11–16. [Google Scholar] [CrossRef]
- AlShaafi, M.M. Effects of different infection control methods on the intensity output of LED light-curing units. King Saud Univ. J. Dent. Sci. 2013, 4, 27–31. [Google Scholar] [CrossRef]
- Konerding, K.L.; Heyder, M.; Kranz, S.; Guellmar, A.; Voelpel, A.; Watts, D.C.; Jandt, K.D.; Sigusch, B.W. Study of energy transfer by different light curing units into a class III restoration as a function of tilt angle and distance, using a MARC Patient Simulator (PS). Dent. Mater. 2016, 32, 676–686. [Google Scholar] [CrossRef] [PubMed]
- Sword, R.J.; Do, U.N.; Chang, J.H.; Rueggeberg, F. Effect of curing light barriers and light types on radiant exposure and composite conversion. J. Esthet. Restor. Dent. 2016, 28, 29–42. [Google Scholar] [CrossRef] [PubMed]
- Suliman, A.; Abdo, A.; Elmasmari, H.A. Effect of contamination, damage and barriers on the light output of light-curing units. Open Dent. J. 2019, 13, 196–202. [Google Scholar] [CrossRef]
- Soares, C.J.; Braga, S.S.L.; Ribeiro, M.T.H.; Price, R.B. Effect of infection control barriers on the light output from a multi-peak light curing unit. J. Dent. 2020, 103, 103503. [Google Scholar] [CrossRef] [PubMed]
- Price, R.B.; Labrie, D.; Whalen, J.M.; Felix, C.M. Effect of distance on irradiance and beam homogeneity from 4 light-emitting diode curing units. J. Can. Dent. Assoc. 2011, 77, b9. [Google Scholar]
- Beolchi, R.S.; Moura-Netto, C.; Palo, R.M.; Torres, C.R.G.; Pelissier, B. Changes in irradiance and energy density in relation to different curing distances. Braz. Oral Res. 2015, 29, 1–7. [Google Scholar] [CrossRef]
- Al-Zain, A.; Eckert, G.; Platt, J. The influence of distance on radiant exposure and degree of conversion using different light-emitting-diode curing units. Oper. Dent. 2019, 44, E133–E144. [Google Scholar] [CrossRef]
- Price, R.B.T.; McLeod, M.E.; Felix, C.M. Quantifying light energy delivered to a Class I restoration. J. Can. Dent. Assoc. 2010, 76, a23. [Google Scholar]
- Mutluay, M.M.; Rueggeberg, F.A.; Price, R.B. Effect of using proper light-curing techniques on energy delivered to a Class 1 restoration. Quintessence Int. 2014, 45, 549–556. [Google Scholar] [CrossRef]
- Soares, C.; De Bragança, G.F.; Pereira, R.A.D.S.; Rodrigues, M.D.P.; Braga, S.S.L.; Oliveira, L.R.S.; Giannini, M.; Price, R. Irradiance and radiant exposures delivered by LED light-curing units used by a left and right-handed operator. Braz. Dent. J. 2018, 29, 282–289. [Google Scholar] [CrossRef]
- Coutinho, M.; Takayassu, R.N.; Leme, A.A.; Soares, G.P.; Trevizam, N.C. Distance and protective barrier effects on the composite resin degree of conversion. Contemp. Clin. Dent. 2013, 4, 152. [Google Scholar] [CrossRef]
- Chang, H.-S.; Lee, S.-R.; Hong, S.-O.; Ryu, H.-W.; Song, C.-K.; Min, K.-S. Effect of infection control barrier thickness on light curing units. J. Korean Acad. Conserv. Dent. 2010, 35, 368–373. [Google Scholar] [CrossRef]
- Al-Marzok, M.I. The effect of wrapping of light-cure tips on the cure of composite resin. Eur. J. Gen. Dent. 2012, 1, 183–186. [Google Scholar] [CrossRef]
- Price, R.B.T.; Fahey, J.; Felix, C.M. Knoop microhardness mapping used to compare the efficacy of LED, QTH and PAC curing lights. Oper. Dent. 2010, 35, 58–68. [Google Scholar] [CrossRef]
- Price, R.B. Light curing in dentistry. Dent. Clin. N. Am. 2017, 61, 751–778. [Google Scholar] [CrossRef]
- Khaksaran, N.K.; Kashi, T.J.; Rakhshan, V.; Zeynolabedin, Z.S.; Bagheri, H. Kinetics of pulpal temperature rise during light curing of 6 bonding agents from different generations, using light emitting diode and quartz-tungsten-halogen units: An in-vitro simulation. Dent. Res. J. 2015, 12, 173–180. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).