Introduction to Surgical Navigation in Oral Surgery: A Case-Series
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
- Geometric accuracy is an index of image recording precision and indicates the technical quality of the image. Marmulla et al. [22] and Eggers et al. [23] analyzed the geometric accuracy of cone beam CT compared to Spiral CT. These studies showed that the geometric accuracy of cone beam CT was lower than Spiral CT, in the range of fractions of millimeters; moreover, it was unequally distributed over the region of interest. However, cone beam CT appeared to be adequate for the purpose of oral surgery.
- The type of navigation systems influences the accuracy of computer-assisted surgery:
- ○
- Electromagnetic systems superimpose a magnetic field over the surgical site. The position of a tracking probe is determined by analyzing the effect of its ferromagnetic parts on the magnetic field. They have a fast intra-operative registration, but there are interferences with metal instruments [24].
- ○
- Optical systems measure the time that it takes a transducer-emitted tone to reach the microphone-bearing frame. They have a higher technical precision without interference with the metal instruments commonly present in the operating room. However, they must be positioned in a linear way with the patient in order to interact with the surgical field [25,26].
- Target registration error is an index of accuracy of the navigation system. It is defined as the discrepancy, in millimeters, between the real and virtual anatomical points and the fiducial markers [27,28]. The factors that can most influence the target registration error are the type and position of fiducial markers [29]:
- ○
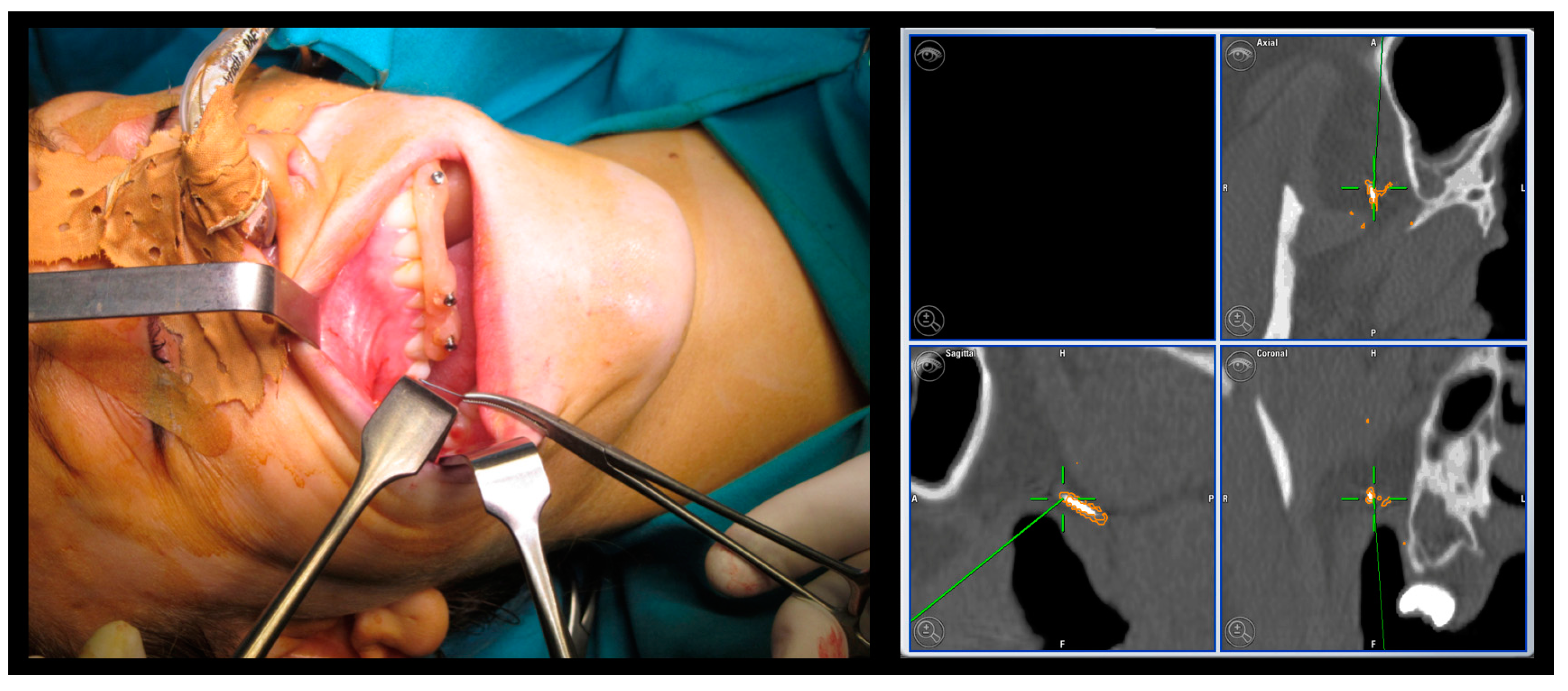
- Invasive fiducial markers: they are normally made up of self-tapping titanium screws inserted into bone through a cutaneous or mucosal access. They are extremely precise, small in size, and do not undergo modifications from the image acquisition phase to the operative time. Due to their characteristics, they can be applied in large numbers. The disadvantages are linked to the invasiveness of their positioning.
- ○
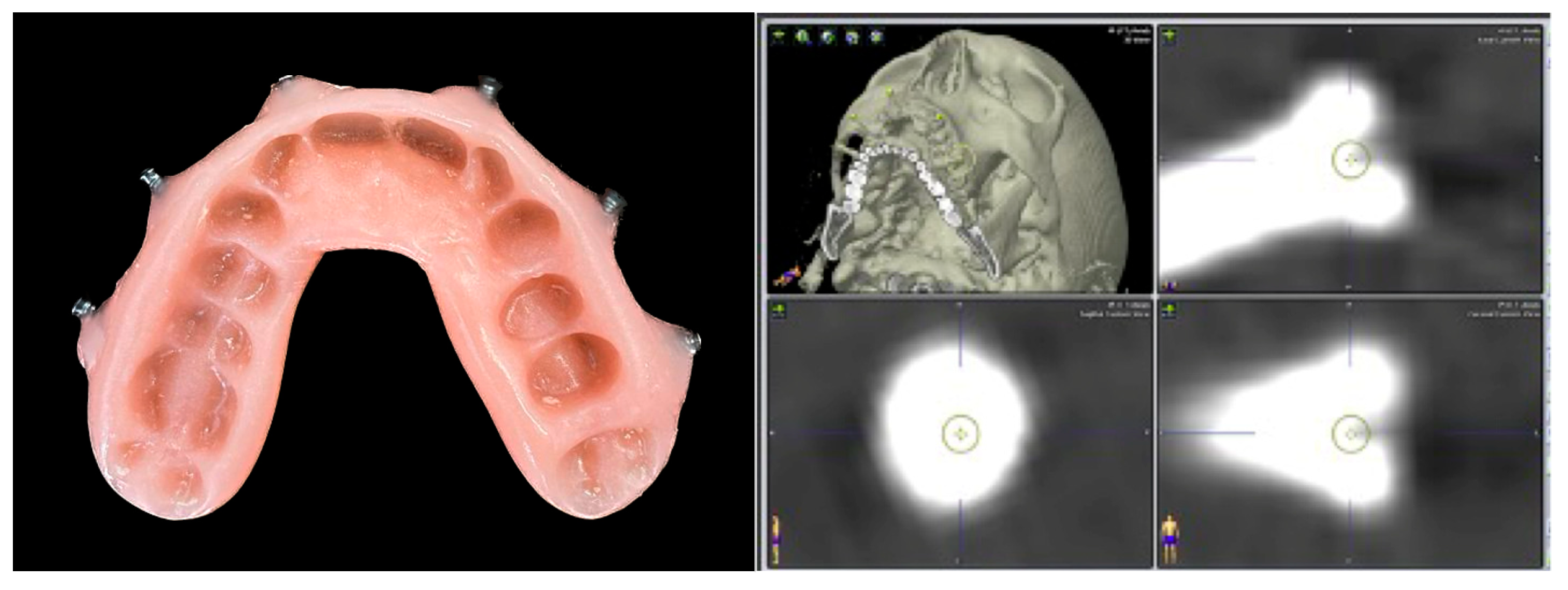
- Non-invasive fiducial markers: specific occlusal dental splints in which radiopaque landmarks are placed in such a way that they can be worn during the CT scan acquisition and used as non-invasive fiducial markers. It is an easy technique, but it requires the additional time to fabricate the splint. It cannot be used in edentulous patients, and its accuracy tends to be reduced above the plane passing through the orbital floor. The splint can be safely removed after registration and re-used during surgery and if the recording has to be repeated to verify the post-operative accuracy.
- ○
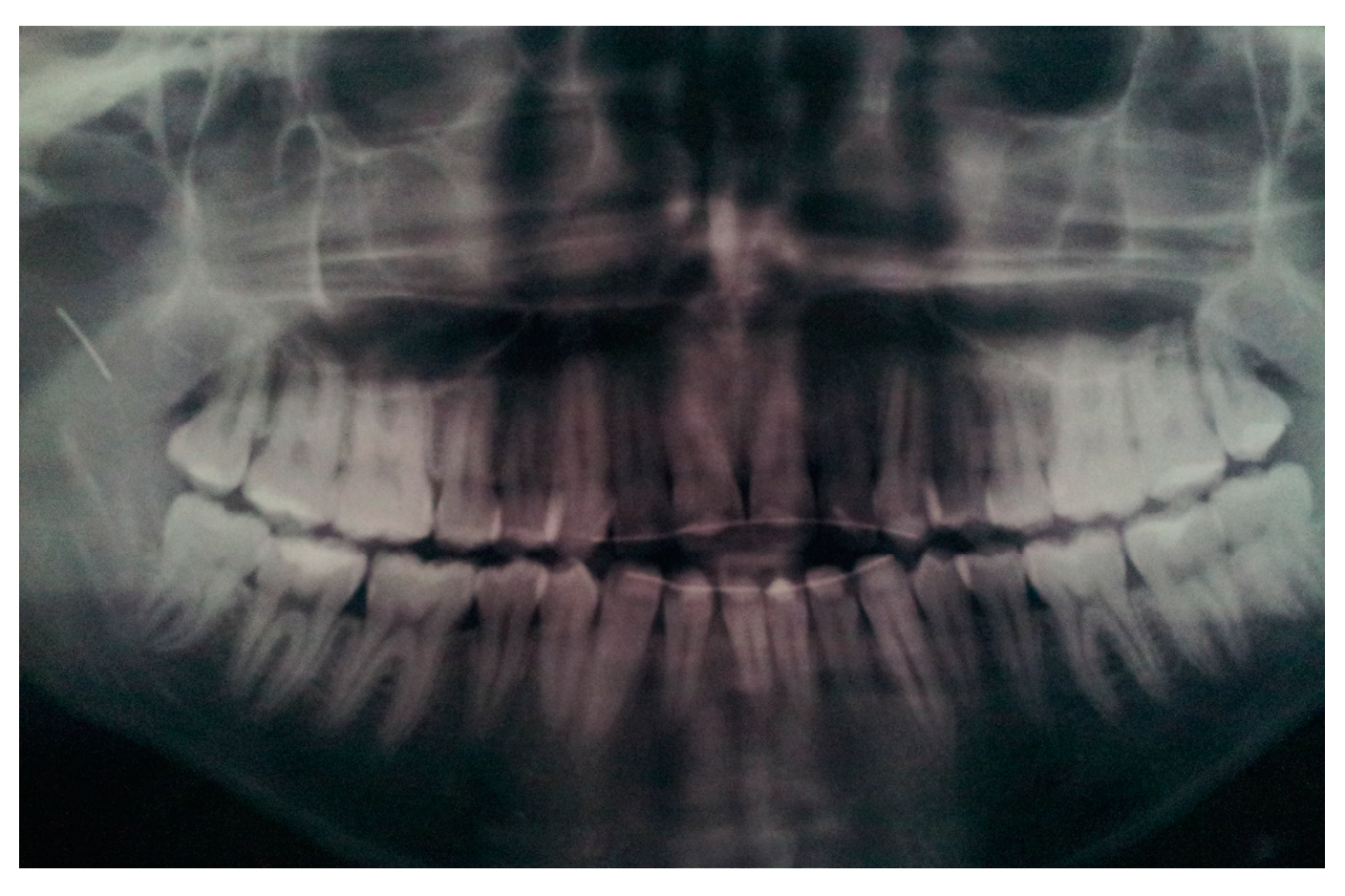
- Dental landmarks: they can be used as an alternative to the occlusal splint. This method requires the presence of at least 4 to 5 non-periodontopathic dental elements in the upper dental arch on which dental brackets could be placed.
- ○
- Surface scanner: it allows one to scan the surface of soft tissues, recording an average of 100–200 surface points. The advantage of this method is to allow a rapid acquisition of a large number of reference points in order to obtain an accurate superimposition with the virtual images, without the need of a CT scan with landmarks.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Horsley, V.; Clarke, R.H. The structure and function of the cerebellum esamine by a new method. Brain 1908, 31, 45–124. [Google Scholar] [CrossRef]
- Spiegel, E.A.; Wycis, H.T.; Marks, M.; Lee, A.J. Stereotaxic Apparatus for Operations on the Human Brain. Science 1947, 106, 349–350. [Google Scholar] [CrossRef] [PubMed]
- Collyer, J. Stereotactic navigation in oral and maxillofacial surgery. Br. J. Oral Maxillofac. Surg. 2010, 48, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Leksell, L.; Jernberg, B. Stereotaxis and tomography a technical note. Acta Neurochir. 1980, 52, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, E.; Watanabe, T.; Manaka, S.; Mayanagi, Y.; Takakura, K. Three-dimensional digitizer (neuronavigator): New equipment for computed tomography-guided stereotaxic surgery. Surg. Neurol. 1987, 27, 543–547. [Google Scholar] [CrossRef]
- No, G.; Tonellini, G.; Mazzoleni, F.; Sozzi, D.; Bozzetti, A. Surgical Navigation Recording Systems in Orbitozygomatic Traumatology. J. Craniofac. Surg. 2012, 23, 890–892. [Google Scholar] [CrossRef]
- Novelli, G.; Tonellini, G.; Mazzoleni, F.; Bozzetti, A.; Sozzi, D. Virtual surgery simulation in orbital wall reconstruction: Integration of surgical navigation and stereolithographic models. J. Cranio-Maxillofacial Surg. 2014, 42, 2025–2034. [Google Scholar] [CrossRef]
- Dubron, K.; Van Camp, P.; Jacobs, R.; Politis, C.; Shaheen, E. Accuracy of virtual planning and intraoperative navigation in zygomaticomaxillary complex fractures: A systematic review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, e841–e848. [Google Scholar] [CrossRef]
- Azarmehr, I.; Stokbro, K.; Bell, R.B.; Thygesen, T. Surgical Navigation: A Systematic Review of Indications, Treatments, and Outcomes in Oral and Maxillofacial Surgery. J. Oral Maxillofac. Surg. 2017, 75, 1987–2005. [Google Scholar] [CrossRef]
- Sozzi, D.; Filippi, A.; Canzi, G.; De Ponti, E.; Bozzetti, A.; Novelli, G. Surgical Navigation in Mandibular Reconstruction: Accuracy Evaluation of an Innovative Protocol. J. Clin. Med. 2022, 11, 2060. [Google Scholar] [CrossRef]
- Dean, A.; Heredero-Jung, S.; Solivera, J.; Sanjuan, A.; Alamillos-Granados, F.J. Computer-assisted and navigated piezoelectric surgery: A new technology to improve precision and surgical safety in craniomaxillofacial surgery. Laryngoscope Investig. Otolaryngol. 2022, 7, 684–691. [Google Scholar] [CrossRef]
- Minervini, G.; Russo, D.; Herford, A.S.; Gorassini, F.; Meto, A.; D’Amico, C.; Cervino, G.; Cicciù, M.; Fiorillo, L. Teledentistry in the Management of Patients with Dental and Temporomandibular Disorders. BioMed Res. Int. 2022, 2022, 7091153. [Google Scholar] [CrossRef] [PubMed]
- Reddy, L.K.V.; Madithati, P.; Narapureddy, B.R.; Ravula, S.R.; Vaddamanu, S.K.; Alhamoudi, F.H.; Minervini, G.; Chaturvedi, S. Perception about Health Applications (Apps) in Smartphones towards Telemedicine during COVID-19: A Cross-Sectional Study. J. Pers. Med. 2022, 12, 1920. [Google Scholar] [CrossRef]
- Landaeta-Quinones, C.G.; Hernandez, N.; Zarroug, N.K. Computer-Assisted Surgery: Applications in Dentistry and Oral and Maxillofacial Surgery. Dent. Clin. N. Am. 2018, 62, 403–420. [Google Scholar] [CrossRef]
- Pellegrino, G.; Ferri, A.; Del Fabbro, M.; Prati, C.; Gandolfi, M.; Marchetti, C. Dynamic Navigation in Implant Dentistry: A Systematic Review and Meta-analysis. Int. J. Oral Maxillofac. Implant. 2021, 36, e121–e140. [Google Scholar] [CrossRef] [PubMed]
- Gargallo-Albiol, J.; Barootchi, S.; Salomó-Coll, O.; Wang, H.-L. Advantages and disadvantages of implant navigation surgery. A systematic review. Ann. Anat. 2019, 225, 1–10. [Google Scholar] [CrossRef]
- Retana, A.; Emery, R.W.; Keir, V. Removal of Impacted Supernumerary Teeth Using a Dynamic Surgical Navigation System: A Case Report. J. Oral Maxillofac. Surg. 2019, 77, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Li, Q.B.; Li, Z.; Cheng, G. Needle Removal in the Deep Maxillofacial Region Assisted by Computerized Navigation Technique and Digital Guiding Plate. J. Craniofac. Surg. 2023; Epub ahead of print. [Google Scholar] [CrossRef]
- Lan, L.; He, Y.; An, J.; Zhang, Y. Application of Computer-Aided Navigation Technology in the Extraction of Foreign Body from the Face. J. Craniofac. Surg. 2020, 31, e166–e169. [Google Scholar] [CrossRef] [PubMed]
- Strong, E.B.; Rafii, A.; Holhweg-Majert, B.; Fuller, S.C.; Metzger, M.C. Comparison of 3 Optical Navigation Systems for Computer-Aided Maxillofacial Surgery. Arch. Otolaryngol. Neck Surg. 2008, 134, 1080–1084. [Google Scholar] [CrossRef] [PubMed]
- Schramm, A.; Suarez-Cunqueiro, M.M.; Rücker, M.; Kokemueller, H.; Bormann, K.-H.; Metzger, M.C.; Gellrich, N.-C. Computer-assisted therapy in orbital and mid-facial reconstructions. Int. J. Med Robot. Comput. Assist. Surg. 2009, 5, 111–124. [Google Scholar] [CrossRef]
- Marmulla, R.; Wörtche, R.; Mühling, J.; Hassfeld, S. Geometric accuracy of the NewTom 9000 Cone Beam CT. Dentomaxillofac. Radiol. 2005, 34, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Eggers, G.; Klein, J.; Welzel, T.; Mühling, J. Geometric accuracy of digital volume tomography and conventional computed tomography. Br. J. Oral Maxillofac. Surg. 2008, 46, 639–644. [Google Scholar] [CrossRef]
- Fried, M.P.; Kleefield, J.; Gopal, H.; Reardon, E.; Ho, B.T.; Kuhn, F.A. Image-Guided Endoscopic Surgery: Results of Accuracy and Performance in a Multicenter Clinical Study Using an Electromagnetic Tracking System. Laryngoscope 1997, 107, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Heilbrun, M.P.; McDonald, P.; Wiker, C.; Koehler, S.; Peters, W. Stereotactic Localization and Guidance Using a Machine Vision Technique. Ster. Funct. Neurosurg. 1992, 58, 94–98. [Google Scholar] [CrossRef]
- Schramm, A.; Gellrich, N.C.; Schmelzeisen, R. Navigational Surgery of the Facial Skeleton; Springer: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Widmann, G.; Stoffner, R.; Bale, R. Errors and error management in image-guided craniomaxillofacial surgery. Oral Surg Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 701–715. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, J.; West, J. The distribution of target registration error in rigid-body point-based registration. IEEE Trans. Med Imaging 2001, 20, 917–927. [Google Scholar] [CrossRef]
- Metzger, M.C.; Rafii, A.; Holhweg-Majert, B.; Pham, A.M.; Strong, B. Comparison of 4 Registration Strategies for Computer-Aided Maxillofacial Surgery. Otolaryngol. Neck Surg. 2007, 137, 93–99. [Google Scholar] [CrossRef]
- Shah, A.; Gill, D.S.; Tredwin, C.; Naini, F.B. Diagnosis and Management of Supernumerary Teeth. Dent. Updat. 2008, 35, 510–520. [Google Scholar] [CrossRef]



| Case | Target 1 | Target 2 | Target 3 | Target 4 |
|---|---|---|---|---|
| Case 1 Foreign body | 1.00 mm | |||
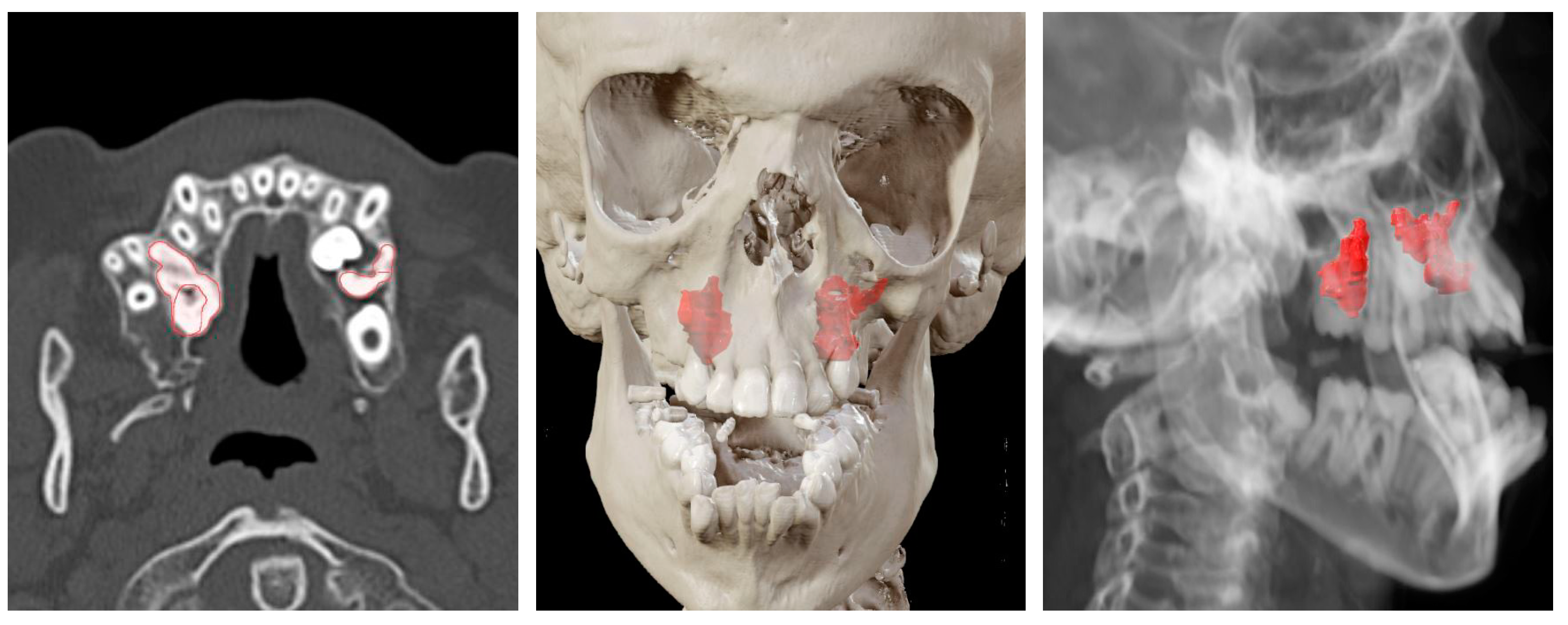
| Case 2 Impacted teeth in Pfeiffer Syndrome | 0.5 mm | 0.3 mm | 0.6 mm | |
| Case 3 Impacted teeth in Apert Syndrome | 0.3 mm | 0.5 mm | 0.4 mm | 0.5 mm |
| Case 4 Impacted teeth | 0.3 mm | 0.2 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Novelli, G.; Moretti, M.; Meazzini, M.C.; Cassé, C.M.A.; Mazzoleni, F.; Sozzi, D. Introduction to Surgical Navigation in Oral Surgery: A Case-Series. Oral 2023, 3, 146-154. https://doi.org/10.3390/oral3020013
Novelli G, Moretti M, Meazzini MC, Cassé CMA, Mazzoleni F, Sozzi D. Introduction to Surgical Navigation in Oral Surgery: A Case-Series. Oral. 2023; 3(2):146-154. https://doi.org/10.3390/oral3020013
Chicago/Turabian StyleNovelli, Giorgio, Mattia Moretti, Maria Costanza Meazzini, Cristina Maria Angela Cassé, Fabio Mazzoleni, and Davide Sozzi. 2023. "Introduction to Surgical Navigation in Oral Surgery: A Case-Series" Oral 3, no. 2: 146-154. https://doi.org/10.3390/oral3020013
APA StyleNovelli, G., Moretti, M., Meazzini, M. C., Cassé, C. M. A., Mazzoleni, F., & Sozzi, D. (2023). Introduction to Surgical Navigation in Oral Surgery: A Case-Series. Oral, 3(2), 146-154. https://doi.org/10.3390/oral3020013







