Photobiomodulation after Surgical Extraction of the Lower Third Molars: A Narrative Review
Abstract
1. Introduction
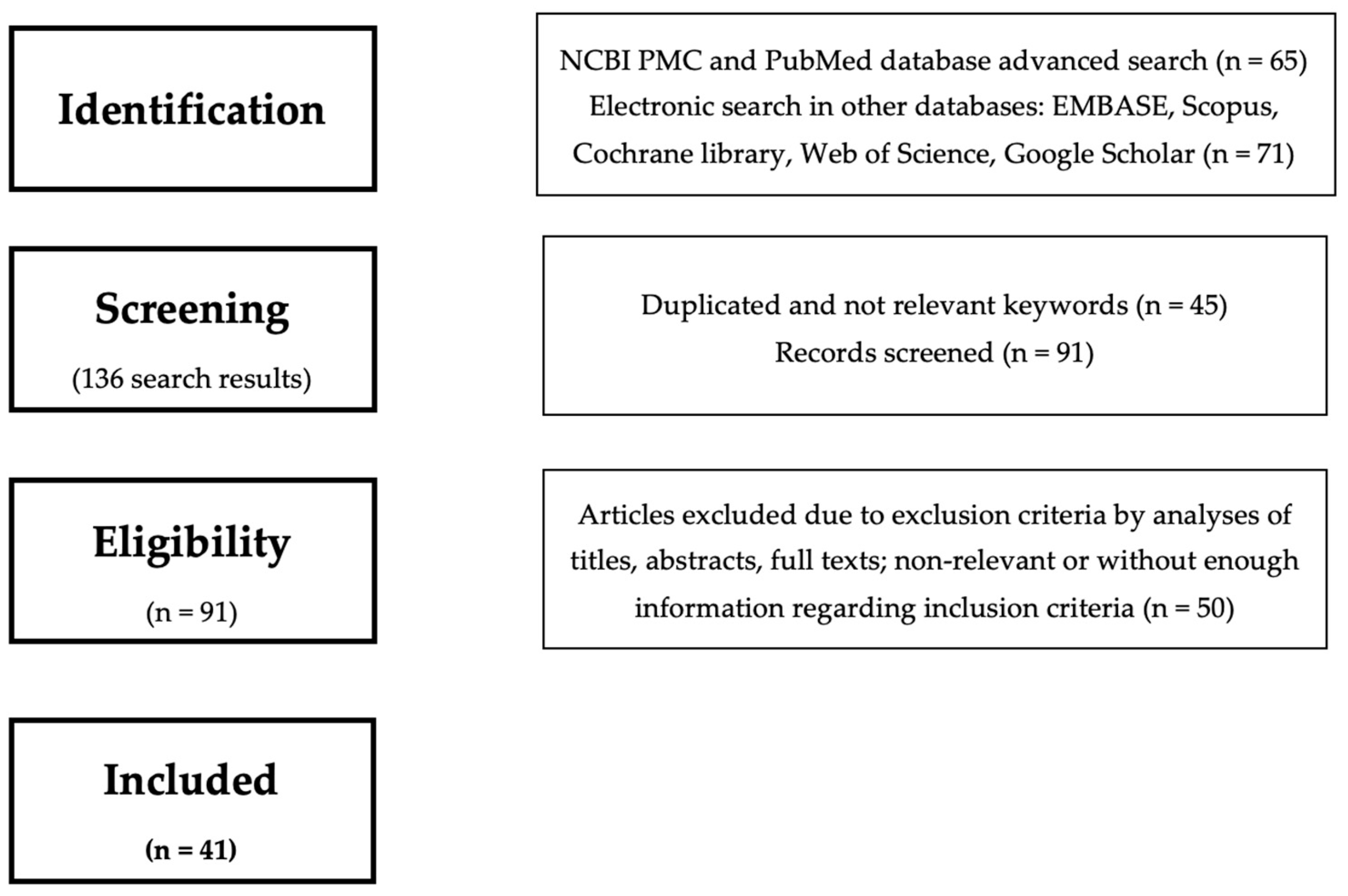
2. Methods
3. Results
3.1. Description of the Studies
3.2. Efficacy of PBM
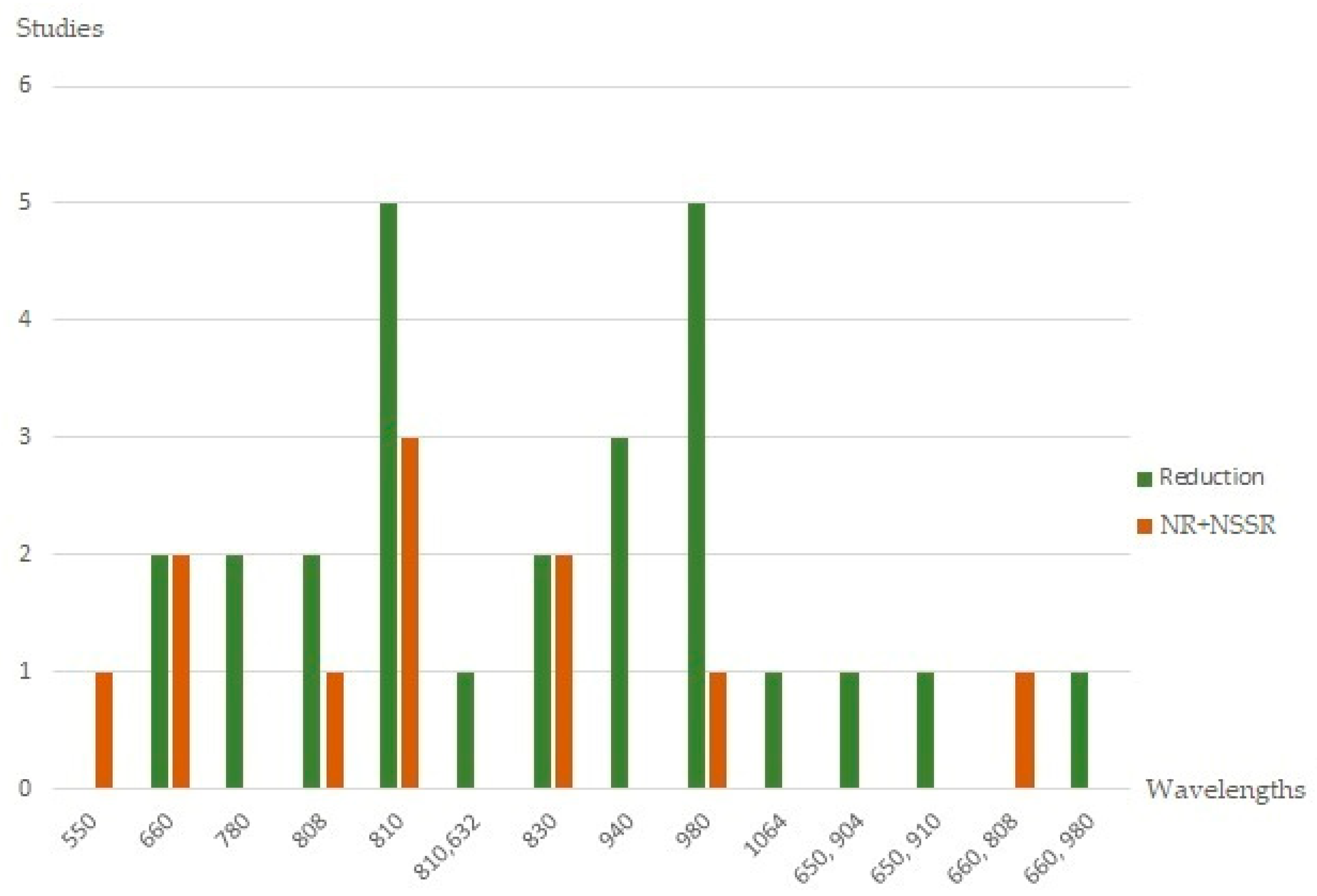
3.2.1. Pain
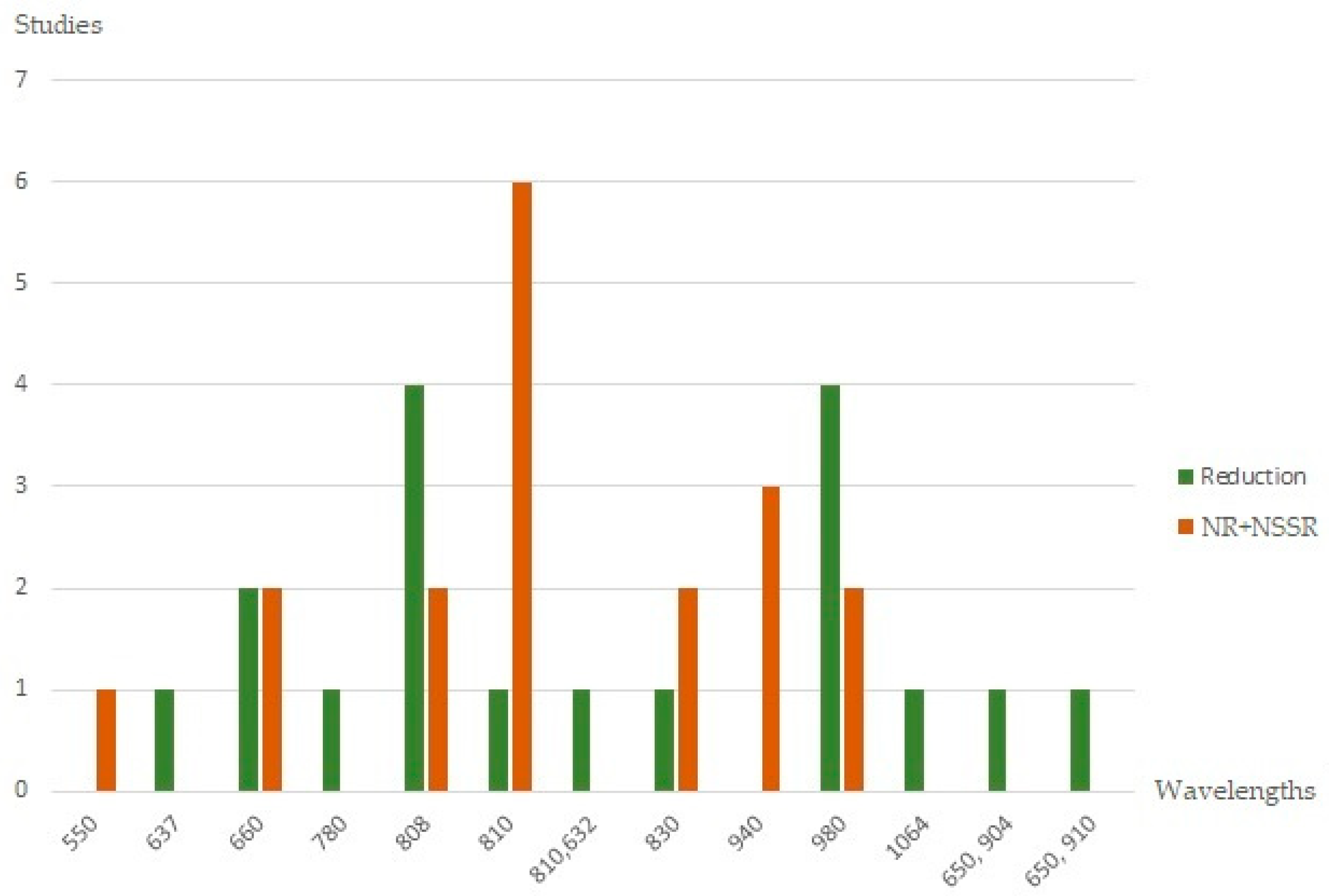
3.2.2. Facial Swelling
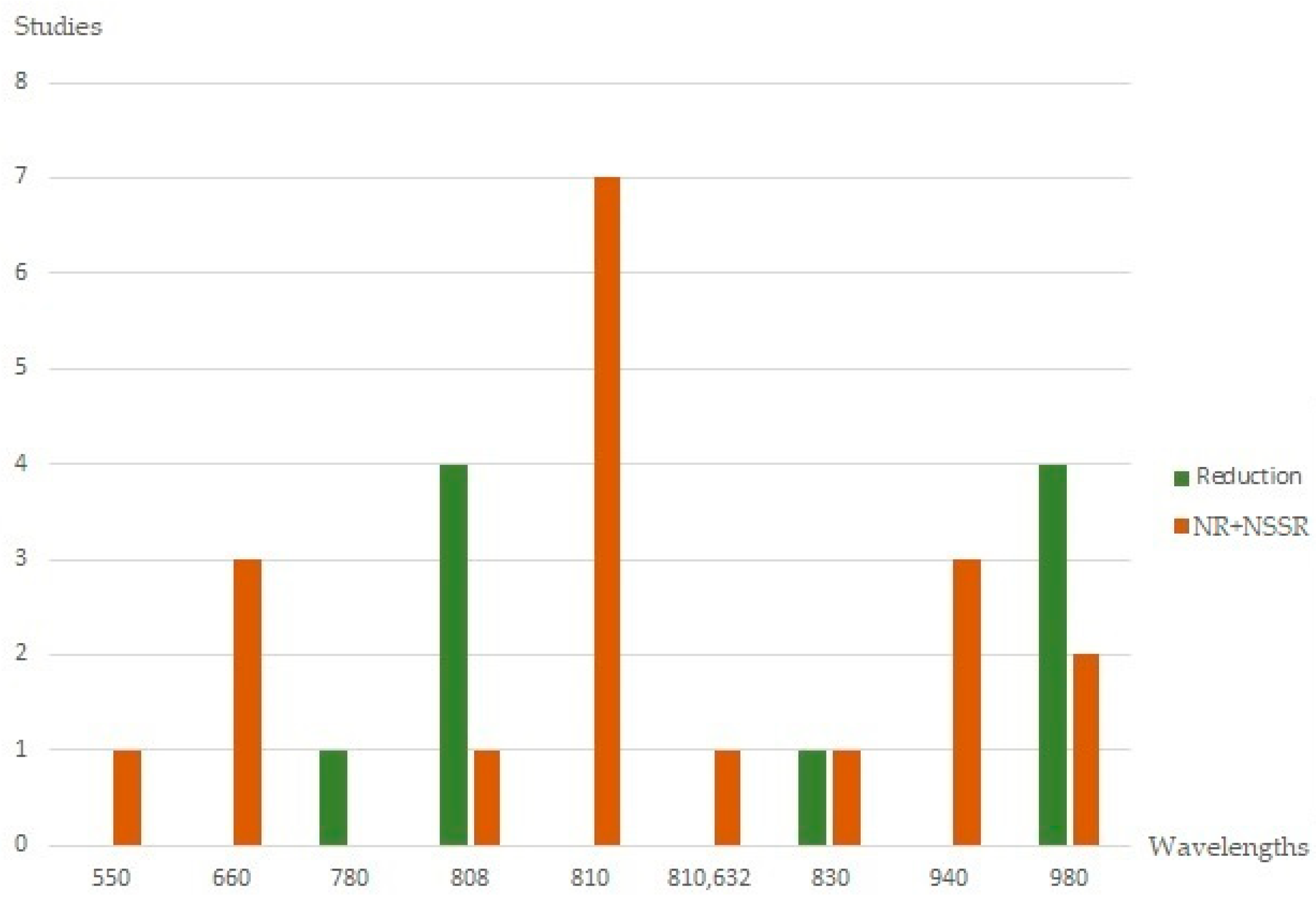
3.2.3. Trismus
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chiapasco, M.; De Cicco, L.; Marrone, G. Side effects and complications associated with third molar surgery. Oral Surg. Oral. Med. Oral Pathol. 1993, 76, 412–420. [Google Scholar] [CrossRef]
- Srivastava, N.; Shetty, A.; Goswami, R.D.; Apparaju, V.; Bagga, V.; Kale, S. Incidence of distal caries in mandibular second molars due to impacted third molars: Nonintervention strategy of asymptomatic third molars causes harm? A retrospective study. Int. J. Appl. Basic Med. Res. 2017, 7, 15–19. [Google Scholar] [PubMed]
- Singh, V.; Garg, A.; Bhagol, A.; Savarna, S.; Agarwal, S.K. Photobiomodulation Alleviates Postoperative Discomfort After Mandibular Third Molar Surgery. J. Oral Maxillofac Surg. 2019, 77, 2412–2421. [Google Scholar] [CrossRef]
- Oikarinen, K. Postoperative pain after mandibular third-molar surgery. Acta Odontol. Scand. 1991, 49, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Beech, A.N.; Haworth, S.; Knepil, G.J. Measurement of generic compared with disease-specific quality of life after removal of mandibular third molars: A patient-centred evaluation. Br. J. Oral Maxillofac. Surg. 2017, 55, 274–280. [Google Scholar] [CrossRef][Green Version]
- Lago-Méndez, L.; Diniz-Freitas, M.; Senra-Rivera, C.; Gude-Sampedro, F.; Gándara Rey, J.M.; García-García, A. Relationships between surgical difficulty and postoperative pain in lower third molar extractions. J. Oral Maxillofac. Surg. 2007, 65, 979–983. [Google Scholar] [CrossRef]
- He, W.L.; Yu, F.Y.; Li, C.J.; Pan, J.; Zhuang, R.; Duan, P.J. A systematic review and meta-analysis on the efficacy of low-level laser therapy in the management of complication after mandibular third molar surgery. Lasers Med. Sci. 2015, 30, 1779–1788. [Google Scholar] [CrossRef]
- Rullo, R.; Addabbo, F.; Papaccio, G.; D’Aquino, R.; Festa, V.M. Piezoelectric device vs. conventional rotative instruments in impacted third molar surgery: Relationships between surgical difficulty and postoperative pain with histological evaluations. J. Craniomaxillofac. Surg. 2013, 41, e33–e38. [Google Scholar] [CrossRef]
- Lo Giudice, R.; Puleio, F.; Rizzo, D.; Alibrandi, A.; Lo Giudice, G.; Centofanti, A.; Fiorillo, L.; Di Mauro, D.; Nicita, F. Comparative investigation of cutting devices on bone blocks: An SEM morphological analysis. Appl. Sci. 2019, 9, 351. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Elmansi, Y.A.; Al-Sharaee, Y.A.; Alrmali, A.E.; Alkhutari, A.S. Does the piezoelectric surgical technique produce fewer postoperative sequelae after lower third molar surgery than conventional rotary instruments? A systematic review and meta analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 383–391. [Google Scholar] [CrossRef]
- Sortino, F.; Pedullà, E.; Masoli, V. The piezoelectric and rotatory osteotomy technique in impacted third molar surgery: Comparison of postoperative recovery. J. Oral Maxillofac. Surg. 2008, 66, 2444–2448. [Google Scholar] [CrossRef] [PubMed]
- Lodi, G.; Figini, L.; Sardella, A.; Carrassi, A.; Del Fabbro, M.; Furness, S. Antibiotics to prevent complications following tooth extractions. Cochrane Database Syst. Rev. 2012, 14, CD003811. [Google Scholar] [CrossRef] [PubMed]
- do Nascimento-Júnior, E.M.; Dos Santos, G.M.S.; Tavares Mendes, M.L.; Cenci, M.; Correa, M.B.; Pereira-Cenci, T.; Martins-Filho, P.R.S. Cryotherapy in reducing pain, trismus, and facial swelling after third-molar surgery: Systematic review and meta-analysis of randomized clinical trials. J. Am. Dent. Assoc. 2019, 150, 269–277. [Google Scholar] [CrossRef]
- Armond, A.C.V.; Glória, J.C.R.; dos Santos, C.R.R.; Galo, R.; Falci, S.G.M. Acupuncture on anxiety and inflammatory events following surgery of mandibular third molars: A splitmouth, randomized, triple-blind clinical trial. Int. J. Oral Maxillofac. Surg. 2019, 48, 274–281. [Google Scholar] [CrossRef]
- Isolan, C.; Kinalski, M.D.; Leão, O.A.; Post, L.K.; Isolan, T.M.; Dos Santos, M.B. Photobiomodulation therapy reduces postoperative pain after third molar extractions: A randomized clinical trial. Med. Oral Patol Oral Cir. Bucal. 2021, 26, e341–e348. [Google Scholar] [CrossRef]
- Del Vecchio, A.; Tenore, G.; Luzi, M.C.; Palaia, G.; Mohsen, A.; Pergolini, D.; Romeo, U. Laser Photobiomodulation (PBM)-A Possible New Frontier for the Treatment of Oral Cancer: A Review of In Vitro and In Vivo Studies. Healthcare 2021, 29, 134. [Google Scholar] [CrossRef]
- Saracino, S.; Mozzati, M.; Martinasso, G.; Pol, R.; Canuto, R.A.; Muzio, G. Superpulsed laser irradiation increases osteoblast activity via modulation of bone morphogenetic factors. Lasers Surg. Med. 2009, 41, 298–304. [Google Scholar] [CrossRef]
- Suter, V.G.A.; Sjölund, S.; Bornstein, M.M. Effect of laser on pain relief and wound healing of recurrent aphthous stomatitis: A systematic review. Lasers Med. Sci. 2017, 32, 953–963. [Google Scholar] [CrossRef]
- Tenore, G.; Zimbalatti, A.; Rocchetti, F.; Graniero, F.; Gaglioti, D.; Mohsen, A.; Caputo, M.; Lollobrigida, M.; Lamazza, L.; De Biase, A.; et al. Management of Medication-Related Osteonecrosis of the Jaw (MRONJ) Using Leukocyte- and Platelet-Rich Fibrin (L-PRF) and Photobiomodulation: A Retrospective Study. J. Clin. Med. 2020, 9, 3505. [Google Scholar] [CrossRef]
- Basso, F.G.; Oliveira, C.F.; Kurachi, C.; Hebling, J.; Costa, C.A. Biostimulatory effect of low-level laser therapy on keratinocytes in vitro. Lasers Med. Sci. 2013, 28, 367–374. [Google Scholar] [CrossRef]
- Ross, G.; Ross, A. Low level lasers in dentistry. Gen. Dent. 2008, 56, 629–634. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 21, 339:b2535. [Google Scholar]
- Asutay, F.; Ozcan-Kucuk, A.; Alan, H.; Koparal, M. Three dimensional evaluation of the effect of low-level laser therapy on facial swelling after lower third molar surgery: A randomized, placebo controlled study. Niger. J. Clin. Pract. 2018, 21, 1107–1113. [Google Scholar]
- Hamid, M.A. Low-level laser therapy on postoperative pain after mandibular third molar surgery. Ann. Maxillofac. Surg. 2017, 7, 207–216. [Google Scholar] [CrossRef]
- Landucci, A.; Wosny, A.; Uetanabaro, L.; Moro, A.; Araujo, M. Efficacy of a single dose of low-level laser therapy in reducing pain, swelling, and trismus following third molar extraction surgery. Int. J. Oral Maxillofac. Surg. 2016, 45, 392–398. [Google Scholar] [CrossRef]
- Sierra, S.O.; Deana, A.M.; Bussadori, S.K.; da Mota, A.C.; Motta, L.J.; Ferrari, R.A.; Schalch, T.D.; Fernandes, K.P. Effect of lowintensity laser treatment on pain after extraction of impacted mandibular third molars: A randomised, controlled, clinical trial. Br. J. Oral Maxillofac. Surg. 2015, 53, 996–1000. [Google Scholar] [CrossRef]
- Sierra, S.O.; Deana, A.M.; Bussadori, S.K.; da Mota, A.C.; Ferrari, R.A.; do Vale, K.L.; Fernandes, K.P. Choosing between intraoral or extraoral, red or infrared laser irradiation after impacted third molar extraction. Lasers Surg. Med. 2016, 48, 511–518. [Google Scholar] [CrossRef]
- Pol, R.; Ruggiero, T.; Gallesio, G.; Riso, M.; Bergamasco, L.; Mortellaro, C.; Mozzati, M. Efficacy of anti-inflammatory and analgesic of superpulsed low level laser therapy after impacted mandibular third molars extractions. J. Craniofac. Surg. 2016, 27, 685–690. [Google Scholar] [CrossRef]
- Abdel-Alim, H.M.; Abdel-Dayem, H.; Mustafa, Z.A.; Bayoumi, A.; Jan, A.; Jadu, F. A comparative study of the effectiveness of immediate versus delayed photobiomodulation therapy in reducing the severity of postoperative inflammatory complications. Photomed. Laser Surg. 2015, 33, 447–451. [Google Scholar] [CrossRef]
- Fabre, H.S.; Navarro, R.L.; Oltramari-Navarro, P.V.; Oliveira, R.F.; Pires-Oliveira, D.A.; Andraus, R.A.; Fuirini, N.; Fernandes, K.B. Anti-inflammatory and analgesic effects of low-level laser therapy on the postoperative healing process. J. Phys. Sci. 2015, 27, 1645–1648. [Google Scholar] [CrossRef]
- Merigo, E.; Vescovi, P.; Margalit, M.; Ricotti, E.; Stea, S.; Meleti, M.; Manfredi, M.; Fornaini, C. Efficacy of LLLT in swelling and pain control after the extraction of lower impacted third molars. Laser 2015, 24, 39–46. [Google Scholar] [CrossRef]
- Ferrante, M.; Petrini, M.; Trentini, P.; Perfetti, G.; Spoto, G. Effect of low-level laser therapy after extraction of impacted lower third molars. Lasers Med. Sci. 2013, 28, 845–849. [Google Scholar] [CrossRef]
- Koparal, M.; Ozcan Kucuk, A.; Alan, H.; Asutay, F.; Avci, M. Effects of low-level laser therapy following surgical extraction of the lower third molar with objective measurement of swelling using a three-dimensional system. Exp. Med. 2018, 15, 3820–3826. [Google Scholar] [CrossRef]
- Raiesian, S.; Khani, M.; Khiabani, K.; Hemmati, E.; Pouretezad, M. Assessment of low-level laser therapy effects after extraction of impacted lower third molar surgery. J. Laser Med. Sci. 2017, 8, 42–45. [Google Scholar] [CrossRef]
- Petrini, M.; Ferrante, M.; Trentini, P.; Perfetti, G.; Spoto, G. Effect of pre-operatory low-level laser therapy on pain, swelling, and trismus associated with third-molar surgery. Med. Oral Patol. Oral Circ. Bucal 2017, 22, e467–e472. [Google Scholar] [CrossRef]
- Kahraman, S.A.; Cetiner, S.; Strauss, R.A. The effects of transcutaneous and intraoral low-level laser therapy after extraction of lower third molars: A randomized single blind, placebo controlled dual-center study. Photomed. Laser Surg. 2017, 35, 401–407. [Google Scholar] [CrossRef]
- Alan, H.; Yolcu, Ü.; Koparal, M.; Özgür, C.; Öztürk, S.A.; Malkoç, S. Evaluation of the effects of the low-level laser therapy on swelling, pain, and trismus after removal of impacted lower third molar. Head Face Med. 2016, 12, 12–25. [Google Scholar] [CrossRef]
- Eroglu, C.N.; Keskin Tunc, S. Effectiveness of single session of low-level laser therapy with a 940 nm wavelength diode laser on pain, swelling, and trismus after impacted third molar surgery. Photomed. Laser Surg. 2016, 34, 406–410. [Google Scholar] [CrossRef]
- Eshghpour, M.; Ahrari, F.; Takallu, M. Is low-level laser therapy effective in the management of pain and swelling after mandibular third molar surgery? J. Oral Maxillofac. Surg. 2016, 74, 1321–1322. [Google Scholar] [CrossRef]
- Kazancioglu, H.O.; Ezirganli, S.; Demirtas, N. Comparison of the influence of ozone and laser therapies on pain, swelling, and trismus following impacted third-molar surgery. Lasers Med. Sci. 2014, 29, 1313–1319. [Google Scholar] [CrossRef]
- Tuk, J.G.C.; van Wijk, A.J.; Mertens, I.C.; Keles, Z.; Lindeboom, J.A.H.; Milstein, D.M.J. Analgesic effects of preinjection lowlevel laser/light therapy (LLLT) before third molar surgery: A double-blind randomized controlled trial. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 124, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Farhadi, F.; Eslami, H.; Majidi, A.; Fakhrzadeh, V.; Ghanizadeh, M.; KhademNeghad, S. Evaluation of adjunctive effect of low-level laser Therapy on pain, swelling and trismus after surgical removal of impacted lower third molar: A double blind randomized clinical trial. Laser 2017, 26, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Pedreira, A.A.; Wanderley, F.G.; Sa, M.F.; Viena, C.S.; Perez, A.; Hoshi, R.; Leite, M.P.; Reis, S.R.; Medrado, A.P. Thermographic and clinical evaluation of 808-nm laser photobiomodulation effects after third molar extraction. Minerva Stomatol. 2016, 65, 213–222. [Google Scholar] [PubMed]
- Lopez-Ramırez, M.; Vılchez-Perez, M.A.; Gargallo-Albiol, J.; Arnabat-Domı´nguez, J.; Gay-Escoda, C. Efficacy of low-level laser therapy in the management of pain, facial swelling, and postoperative trismus after a lower third molar extraction. A preliminary study. Lasers Med. Sci. 2012, 27, 559–566. [Google Scholar] [CrossRef]
- Amarillas-Escobar, E.D.; Toranzo-Fernández, J.M.; Martínez-Rider, R.; Noyola-Frías, M.A.; Hidalgo-Hurtado, J.A.; Serna, V.M.; Gordillo-Moscoso, A.; Pozos-Guillén, A.J. Use of therapeutic laser after surgical removal of impacted lower third molars. J. Oral Maxillofac. Surg. 2010, 68, 319–324. [Google Scholar] [CrossRef]
- Roynesdal, A.; Bjornland, T.; Barkvoll, P.; Haanaes, H. The effect of soft-laser application on postoperative pain and swelling: A double-blind, crossover study. Int. J. Oral Maxillofac. Surg. 1993, 22, 242–245. [Google Scholar] [CrossRef]
- Fernando, S.; Hill, C.; Walker, R. A randomised double blind comparative study of low level laser therapy following surgical extraction of lower third molar teeth. Br. J. Oral Maxillofac. Surg. 1993, 31, 170–172. [Google Scholar] [CrossRef]
- Markovic, A.; Todorovic, L. Effectiveness of dexamethasone and low-power laser in minimizing oedema after third molar surgery: A clinical trial. Int. J. Oral Maxillofac. Surg. 2007, 36, 226–229. [Google Scholar] [CrossRef]
- Aras, M.H.; Güngörmüş, M. The effect of low-level laser therapy on trismus and facial swelling following surgical extraction of a lower third molar. Photomed. Laser Surg. 2009, 27, 21–24. [Google Scholar] [CrossRef]
- Aras, M.H.; Güngörmüş, M. Placebo-controlled randomized clinical trial of the effect two different low-level laser therapies (LLLT)—intraoral and extraoral—on trismus and facial swelling following surgical extraction of the lower third molar. Lasers Med. Sci. 2010, 25, 641–645. [Google Scholar] [CrossRef]
- Feslihan, E.; Eroglu, C.N. Can Photobiomodulation Therapy Be an Alternative to Methylprednisolone in Reducing Pain, Swelling, and Trismus After Removal of Impacted Third Molars? Photobiomodulation Photomed. Laser Surg. 2019, 37, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Santos, P.L.; Marotto, A.P.; Zatta da Silva, T.; Bottura, M.P.; Valencise, M.; Marques, D.O.; Queiroz, T.P. Is Low-Level Laser Therapy Effective for Pain Control After the Surgical Removal of Unerupted Third Molars? A Randomized Trial. J. Oral Maxillofac. Surg. 2020, 78, 184–189. [Google Scholar] [CrossRef] [PubMed]
- Lakshmi, K.P.; Ali Baig, S.; Walia, S.; Priyadharshini, V.; Vigneswaran, T.; Mazgaonkar, F.S.; Tiwari, R.V.C. Evaluation of effect of low level laser therapy post third molar surgery: An original research. Turk. J. Physiother. Rehabil. 2016, 32, 15240–15243. [Google Scholar]
- El Saeed, A.M.; Al-Fakharany, A.H. Effect of single dose low-level laser therapy on some sequalae after impacted lower third molar surgery. Al-Azhar J. Dent. Sci. 2020, 23, 41–47. [Google Scholar]
- Nejat, A.H.; Eshghpour, M.; Danaeifar, N.; Abrishami, M.; Vahdatinia, F.; Fekrazad, R. Effect of Photobiomodulation on the Incidence of Alveolar Osteitis and Postoperative Pain following Mandibular Third Molar Surgery: A Double-Blind Randomized Clinical Trial. Photochem. Photobiol. 2021, 97, 1129–1135. [Google Scholar] [CrossRef] [PubMed]
- Girgis, M.; Elsharrawy, E.; Hassan, M. Effect of single session of low-level laser therapy on pain, swelling, and trismus after surgical extraction of impacted lower third molar: A clinical study. Dent. Sci. Updates 2021, 2, 55–60. [Google Scholar] [CrossRef]
- Bianchi de Moraes, M.; Gomes de Oliveira, R.; Raldi, F.V.; Nascimento, R.D.; Santamaria, M.P.; Loureiro Sato, F.R. Does the Low-Intensity Laser Protocol Affect Tissue Healing After Third Molar Removal? Am. Assoc. Oral Maxillofac. Surg. 2020, 78, 1920.e1–1920.e9. [Google Scholar] [CrossRef]
- Gulia, S.K.; Kumar, a.; Singh, M.; Thakker, R.; Goya, P.; Tiwari, H.; Tiwari, R.V.C. Effectiveness of Low-Level Lasers Subsequent to Third Molar Surgery: An Original Research. Ann. Rom. Soc. Cell Biol. 2021, 25, 2048–2053. [Google Scholar]
- Scarano, A.; Lorusso, F.; Postiglione, F.; Mastrangelo, F.; Petrini, M. Photobiomodulation Enhances the Healing of Postextraction Alveolar Sockets: A Randomized Clinical Trial with Histomorphometric Analysis and Immunohistochemistry. J. Oral Maxillofac. Surg. 2021, 79, 57.e1–57.e12. [Google Scholar] [CrossRef]
- Momeni, E.; Barati, H.; Arbabi, M.R.; Jalali, B.; Moosavi, M.S. Low-level laser therapy using laser diode 940 nm in the mandibular impacted third molar surgery: Double-blind randomized clinical trial. BMC Oral Health 2021, 77. [Google Scholar] [CrossRef]
- Hadad, H.; Santos, A.; de Jesus, L.K.; Poli, P.P.; Mariano, R.C.; Theodoro, L.H.; Maiorana, C.; Souza, F.Á. Photobiomodulation Therapy Improves Postoperative Pain and Edema in Third Molar Surgeries: A Randomized, Comparative, Double-Blind, and Prospective Clinical Trial. J. Oral Maxillofac. Surg. 2021, 80, 37.e1–37.e12. [Google Scholar] [CrossRef] [PubMed]
- Fraga, R.S.; Antunes, L.; Fialho, W.; Valente, M.I.; Gomes, C.C.; Fontes, K.; Antunes, L.S. Do Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy Minimize Postoperative Pain and Edema After Molar Extraction? Am. Assoc. Oral Maxillofac. Surg. 2020, 78, 2155.e1–2155.e10. [Google Scholar] [CrossRef] [PubMed]
- Mohajerani, H.; Tabeie, F.; Alirezaei, A.; Keyvani, G.; Bemanali, M. Does Combined Low-Level Laser and Light-Emitting Diode Light Irradiation Reduce Pain, Swelling, and Trismus After Surgical Extraction of Mandibular Third Molars? A Randomized Double-Blinded Crossover Study. Am. Assoc. Oral Maxillofac. Surg. 2021, 79, 1621–1628. [Google Scholar] [CrossRef] [PubMed]
| Authors and Year of Publication | Laser Properties | Outcomes | Sample Size | |||
|---|---|---|---|---|---|---|
| (nm) | (mW) | (J/cm2) | ||||
| [23] | Asutay et al. (2018) | 810 | 300 | 4 | pain, trismus, swelling | 45 |
| [24] | Hamid et al. (2017) | 810 | 100 | 32, 86 | pain | 30 |
| [25] | Landucci et al. (2016) | 780 | 10 | 7, 5 | pain, trismus, swelling | 22 |
| [26] | Sierra et al. (2015) | 660, 808 | 100 | 106 | pain | 60 |
| [27] | Sierra et al. (2016) | 660, 808 | 100 | 106 | pain | 60 |
| [28] | Pol et al. (2016) | 650, 904 | 8–500, 70 | no reported | pain, swelling | 25 |
| [29] | Abdel-Alim et al. (2015) | 830 | 4 | no reported | pain, trismus, swelling | 80 |
| [30] | Fabre et al. (2015) | 660 | 35 | 5 | pain, trismus, swelling | 10 |
| [31] | Merigo et al. (2015) | 650, 910 | no reported | 480, 31 | pain, swelling | 59 |
| [32] | Ferrante et al. (2013) | 980 | 300 | no reported | pain, trismus, swelling | 30 |
| [33] | Koparal et al. (2018) | 810 | 300 | 4 | pain, trismus, swelling | 45 |
| [34] | Raisesian et al. (2017) | 980 | 300 | 18 | pain, trismus, swelling | 44 |
| [35] | Petrini et al. (2017) | 980 | 300 | no reported | pain, trismus, swelling | 45 |
| [36] | Kahraman et al. (2017) | 830 | 100 | 3 | pain | 53 |
| [37] | Alan et al. (2016) | 810 | 300 | 4 | pain, trismus, swelling | 15 |
| [38] | Eroglu et al. (2016) | 940 | no reported | 4 | pain, trismus, swelling | 35 |
| [39] | Eshghpour et al. (2016) | 660 | 200 | 85, 7 | pain, swelling | 40 |
| [40] | Kazancioglu et al. (2014) | 808 | 100 | 4 | pain, trismus, swelling | 60 |
| [41] | Tuk et al. (2017) | 660 | 198 | 67,5 | pain | 163 |
| [42] | Farhadi et al. (2017) | 550 | 100 | 5 | pain, trismus, swelling | 48 |
| [43] | Pedreira et al. (2016) | 808 | no reported | 2 | pain, trismus, swelling | 24 |
| [44] | Lopez Ramirez et al. (2012) | 810 | 500 | 5 | pain, trismus, swelling | 20 |
| [45] | Amarillas et al. (2010) | 810 | 100 | 4 | pain, trismus, swelling | 30 |
| [46] | Roynesdal et al. (1993) | 830 | 40 | no reported | pain, trismus, swelling | 25 |
| [47] | Fernando et al. (1993) | 830 | 30 | no reported | pain, swelling | 52 |
| [48] | Markovic et al. (2007) | 637 | 50 | 4 | swelling | 120 |
| [49] | Aras et al. (2009) | 808 | 100 | 4 | swelling, trismus | 32 |
| [50] | Aras et al. (2010) | 808 | 100 | 4 | swelling, trismus | 48 |
| [51] | Feslihan et al. (2019) | 810 | 300 | 6 | pain, trismus, swelling | 30 |
| [52] | Santos et al. (2020) | 780 | 70 | 52, 5 | pain | 32 |
| [53] | Lakshmi et al. (2021) | 980 | 300 | no reported | pain, trismus, swelling | 100 |
| [54] | El Saeed et al. (2020) | 980 | 500 | 4 | pain, trismus, swelling | 20 |
| [55] | Nejat et al. (2021) | 660, 980 | 200 | 1.5, 6 | pain | 80 |
| [56] | Kamal et al. (2021) | 980 | 100 | no reported | pain, trismus, swelling | 24 |
| [57] | Bianchi de Moraes et al. (2020) | 660 | 30 | 10, 30 | pain, trismus, swelling | 57 |
| [58] | Kumar Gulia et al. (2021) | 940 | 500 | 10 | pain, trismus, swelling | 32 |
| [59] | Scarano et al. (2021) | 1064 | 1000 | no reported | pain, swelling | 20 |
| [60] | Momeni et al. (2021) | 940 | 500 | 10 | pain, trismus, swelling | 25 |
| [61] | Hadad et al. (2021) | 810 | 100 | 212 | pain, trismus, swelling | 13 |
| [62] | Fraga et al. (2020) | 808 | 100 | 133 | pain, swelling | 40 |
| [63] | Mohajerani et al. (2020) | 810, 632 | 500 | 5, 2 | pain, trismus, swelling | 40 |
| Method of Evaluation | Comparison | Results | |||
|---|---|---|---|---|---|
| Pain | Swelling | Trismus | |||
| [23] | VAS, MO, 3dMD FP | vs. placebo | Reduction | Not statistically significant | Not statistically significant |
| [24] | VAS | vs. placebo | Reduction | ||
| [25] | VAS, NRS | vs. placebo | Not statistically significant | Reduction | Reduction |
| [26] | VAS, FDM, MO | vs. placebo | Reduction | ||
| [27] | FDM, MO | 808 nm vs. 660 nm | 808 Reduction | 808 Reduction | |
| [28] | VAS, FDM | vs. placebo | Reduction | Reduction | |
| [29] | MO, Bello’s FSA | vs. delayed PBM | Reduction | Reduction | Reduction |
| [30] | VAS, FDM, MO | vs. placebo | Reduction | Reduction | Reduction |
| [31] | VAS, FDM | vs. placebo | Reduction | Reduction | |
| [32] | VAS, FDM, MO | vs. placebo | Reduction | Reduction | Reduction |
| [33] | VAS, MO, 3dMD FP | vs. placebo | Reduction | Not statistically significant | Not statistically significant |
| [34] | VAS, FDM, MO | vs. drug therapy | Reduction | Not statistically significant | Not statistically significant |
| [35] | VAS, FDM, MO | vs. drug therapy | Reduction | Reduction | Not statistically significant |
| [36] | VAS | intraoral vs. extraoral | Reduction | ||
| [37] | VAS, MO, 3dMD FP | vs. placebo | Reduction | Not statistically significant | Not statistically significant |
| [38] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [39] | VAS, ECE | vs. placebo | Reduction | Reduction | |
| [40] | VAS, FDM, MO | vs. ozone therapy | Reduction | Reduction | Reduction |
| [41] | HR, SR, Questionnaire | vs. placebo | Not statistically significant | ||
| [42] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [43] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [44] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [45] | VAS, FDM, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [46] | VAS, FS, MO | vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [47] | VAS, Swelling scale | vs. placebo | Not statisticallysignificant | Not statisticallysignificant | |
| [48] | FDM | vs. placebo | Reduction | ||
| [49] | Amin Laskin FS, MO | vs. placebo | Reduction | Reduction | |
| [50] | Amin Laskin FS, MO | intraoral vs. extraoral | Reduction | Reduction | |
| [51] | VAS, FDM, MO | vs. methylprednisolone | Not statisticallysignificant | Not statisticallysignificant | Not statisticallysignificant |
| [52] | VAS | vs. split mouth | Reduction | ||
| [53] | VAS, FS, MO | vs. placebo | Not statisticallysignificant | Reduction | Reduction |
| [54] | VAS, FS, MO | vs. placebo | Reduction | Reduction | Reduction |
| [55] | VAS | vs. placebo | Reduction | ||
| [56] | VAS, FS, MO | vs placebo | Reduction | Reduction | Reduction |
| [57] | VAS, MO, 3dMD FP | 10 J/cm2 vs. 30 J/cm2 vs. placebo | Not statistically significant | Not statistically significant | Not statistically significant |
| [58] | VAS, FS, MO | vs. placebo | Reduction | Not statistically significant | Not statistically significant |
| [59] | VAS, FS | vs. placebo | Reduction | Reduction | |
| [60] | VAS, FS, MO | vs. placebo | Reduction | Not statistically significant | Not statistically significant |
| [61] | VAS, FS, MO | vs. placebo | Reduction | Reduction | Not statistically significant |
| [62] | VAS, FS | LLLT + aPDT vs. placebo | Reduction | Not statistically significant | |
| [63] | VAS, FS, MO | vs. split mouth | Reduction | Reduction | Not statistically significant |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pergolini, D.; Del Vecchio, A.; Palaia, G.; Rocchetti, F.; Cefalà, R.; De Angelis, R.; Tenore, G.; Romeo, U. Photobiomodulation after Surgical Extraction of the Lower Third Molars: A Narrative Review. Oral 2022, 2, 18-28. https://doi.org/10.3390/oral2010004
Pergolini D, Del Vecchio A, Palaia G, Rocchetti F, Cefalà R, De Angelis R, Tenore G, Romeo U. Photobiomodulation after Surgical Extraction of the Lower Third Molars: A Narrative Review. Oral. 2022; 2(1):18-28. https://doi.org/10.3390/oral2010004
Chicago/Turabian StylePergolini, Daniele, Alessandro Del Vecchio, Gaspare Palaia, Federica Rocchetti, Raffaele Cefalà, Riccardo De Angelis, Gianluca Tenore, and Umberto Romeo. 2022. "Photobiomodulation after Surgical Extraction of the Lower Third Molars: A Narrative Review" Oral 2, no. 1: 18-28. https://doi.org/10.3390/oral2010004
APA StylePergolini, D., Del Vecchio, A., Palaia, G., Rocchetti, F., Cefalà, R., De Angelis, R., Tenore, G., & Romeo, U. (2022). Photobiomodulation after Surgical Extraction of the Lower Third Molars: A Narrative Review. Oral, 2(1), 18-28. https://doi.org/10.3390/oral2010004












