Abstract
Cone beam computed tomography (CBCT) is an emerging radiographic imaging modality. The diagnostic benefit must exceed the individual detriment that its generally higher radiation exposure may cause. Since limited studies exist on the use and impact of CBCT in paediatric dentistry, a service evaluation was carried out to explore the reasons for CBCT referral and to identify its impact on the treatment plan and/or management in a paediatric dentistry department. Clinical records for all paediatric patients who underwent a CBCT were reviewed, to identify the reason for referral and its influence on diagnosis or management, by comparing the provisional treatment plan with the definitive treatment plan, post-CBCT. A total of 130 paediatric patients underwent CBCT in a 12-month period, of which 52 satisfied the inclusion criteria. CBCTs were most commonly requested for the localisation of unerupted/impacted teeth 14/52 (27%), assessment of supernumerary teeth 12/52 (23%), and to investigate root resorption 9/52 (17%). All CBCTs provided additional information that assisted treatment planning, diagnosis, or management and, most significantly, 16/52 (31%) of treatment plans were changed based on CBCT findings. All CBCTs requested in this study were justified and confirmed or influenced the management of paediatric patients, ultimately reducing the risk of complications and further treatment.
1. Introduction
Since the discovery of x-rays in 1895 by Wilhelm Conrad Roentgen, radiography is considered the most frequent special investigatory tool in daily dental practice [1]. However, two-dimensional imaging modalities suffer from the same inherent limitations, whether they are used individually or in combination. These include, but are not limited to, image magnification, image distortion, and the superimposition of anatomical structures over the region of interest [2]. The introduction of cone beam computed tomography (CBCT) in 1998 represented a true paradigm shift. CBCT provides accurate, sub-millimetre resolution images, providing three-dimensional visualisation of the oral and maxillofacial region.
CBCT imaging is performed using a cone-shaped x-ray beam linked to a flat panel detector that performs a single rotation around the patient, producing a series of two-dimensional “frames” or “projections.” The scan time is generally less than 20 seconds. The two-dimensional frames are reconstructed into a three-dimensional dataset, from which slices in the axial, coronal and sagittal planes are produced. The smallest field of view compatible with the information required should always be selected to reduce the radiation dose to the patient [3].
Criteria for conventional dental radiography is well established but it is only recently these have included the use of CBCT [4]. The growth of CBCT has moved faster than the procurement of the research evidence required to develop high-grade referral criteria for CBCT in the various fields of dentistry [3]. The European Commission has created evidence-based guidelines on the appropriate use and justification of CBCT in dentistry [5]. As CBCT examinations provide an effective radiation dose generally higher than periapical, occlusal, and panoramic radiography, it is essential that all exposures are fully justified and that once justified are optimised [6,7,8,9]. All radiation doses should be kept as low as reasonably achievable (ALARA) and the diagnostic benefit must exceed the individual detriment that the radiation exposure may cause. This is particular true in paediatric patients, who are much more susceptible to stochastic biological effects of radiation (ICRP) [10]. Justification of CBCT investigations is not only an ethical requirement but also a legal requirement, as outlined in the Ionising Radiation Medical Exposure Regulations (IRMER) 2017 [11].
CBCT is becoming a popular diagnostic investigation in various fields of dentistry. In a literature review, Alamri et al. compiled a list of 129 articles related to the applications of CBCT in dentistry. The majority of CBCT use was observed in oral and maxillofacial surgery (26.3%), followed by endodontics (25.6%), implantology (16.3%), orthodontics (11.6%), general dentistry (9.3%), temporomandibular joint disorder (5.4%), periodontology (4.65%), and forensic dentistry (0.8%) [12].
CBCT certainly has its function in paediatric dentistry, and its use has been reported by various authors. Often the studies discuss the uses of CBCT in orthodontic adolescents, rather than providing a comprehensive overview of its uses in children and young people [13,14,15]. Hidalgo-Rivas et al., 2014, surveyed the use of CBCT in paediatric patients across three dental hospitals in the UK [16]. The indications of use of CBCT in paediatric dentistry were reported, however there was limited investigation on the impact of the CBCT imaging on treatment planning and dental management of paediatric patients. Mizban et al., 2019, audited the compliance of CBCT use with the European guidelines (SEDENTEXCT) and evaluated the influence of CBCT on treatment planning, in a department of paediatric dentistry in London [17].
Therefore, the aim of this service evaluation was to explore the reasons for referral for CBCT in a paediatric dentistry department and to identify its impact on the treatment plan and/or management of paediatric patients.
2. Methods
The work formed part of a service evaluation in the paediatric dentistry department at the University Dental Hospital (UDH), Cardiff, and was registered with the University Health Board Clinical Audit Database. The Health Research Authority Decision Tool confirmed that National Health Service UK (NHS) ethical approval was not required [18].
The data were collected retrospectively over a 12-month period, and all relevant data were recorded on a data collection MS Excel Spreadsheet.
The inclusion criteria taken into consideration for case selection required the age of the patient at the time of CBCT examination to be 16 years or younger and for the UDH paediatric dental team or the multidisciplinary team managing the child’s dental problems to have requested the CBCT. The case was excluded from selection, if the CBCT was undertaken but did not yield a diagnostic image, or the CBCT scans were requested from external professionals or neighbouring health boards, since no judgement on management could be made.
Details of all patients that undergo CBCT at UDH are recorded in a daybook. This daybook was accessed to retrieve details of paediatric patients that underwent CBCT. For all cases, the clinical records were requested, and the clinical notes and radiographic reports were reviewed to identify the justification for referral for CBCT and to compare the provisional treatment plan, prior to the CBCT referral with the definitive treatment plan, following the CBCT examination. If no provisional treatment plan was documented due to insufficient information from investigations utilising the conventional radiographic techniques, then the treatment plan was recorded as confirmed.
The total number of patients seen in the paediatric department, over the time period, was obtained from the patient management system (PMS) that was developed by the Cardiff and Vale University Health Board. All CBCTs were performed on the Instrumentarium Orthopantomograph OP300 Maxio (Instrumentarium Dental, Tuusula, Finland).
3. Results
During the data collection period, 130 CBCT scans were requested and carried out on patients aged between 7 and 16 years. All of the CBCT scans were of diagnostic quality and were reported by a single dental and maxillofacial radiologist. Moreover, 52 of the cases were internal referrals from UDH and 78 were external referrals from local practitioners and neighbouring health boards. These external referrals were subsequently excluded from the analysis. In this same period, 6733 paediatric patients were seen in University Dental Hospital, Cardiff (UDH.) This equates to 0.92% of the paediatric patients having undergone a CBCT scan.
The majority of scans (38/52, 73%) were carried out using a 5 cm × 5 cm volume scan. Only two other protocols were used. The distribution of scan protocols is presented in Table 1.

Table 1.
Table showing the scan protocols used for the 52 patients included in the service evaluation.
Table 2 illustrates the range of clinical cases that required a CBCT. The most frequent principal diagnosis was unerupted, ectopic, or impacted teeth, and this accounted for 44% (23/52) of all CBCT referrals. This was followed by supernumeraries (23%, 12/52) and cases involving bony pathosis (11%, 6/52).

Table 2.
Table showing the principal clinical diagnosis of the cases in which a cone beam computed tomography (CBCT) was requested.
The CBCTs reviewed covered a wide range of clinical indications as shown in Table 3. Examinations were most commonly requested for the localisation of unerupted, ectopic, or impacted teeth 14/52 (27%), followed by localisation and assessment of supernumerary teeth 12/52 (23%), and to investigate root resorption 9/52 (17%). The remaining 33% of cases were requested to assess bony pathology, surgical planning, to gather more information on the pulpal or dental anatomy and to determine the presence of a root fracture. However, it must be noted that in the majority of cases, multiple reasons were documented justifying the need for a CBCT examination. Details of these are presented in Table 4.

Table 3.
Table showing the principal reason for requesting a CBCT in the paediatric patient.

Table 4.
Table showing the principal and additional reasons for requesting a CBCT in the paediatric patient.
The results show that in 31% (16/52) of the cases, the assessment of tooth restorability, treatment plan and/or management were changed following CBCT examination. These changes are described in Table 5. In the remaining 69% (36/52) of the cases, the provisional treatment plans were confirmed in light of the new information provided by CBCT, increasing the clinician’s confidence in diagnosis and/or management. CBCT provided guiding information for the surgical approach, which included localisation of teeth; confirmation whether the teeth had a poor prognosis diagnosis and were suitable for extraction; identification and localisation of supernumerary teeth or odontomes and visualisation of anatomical structures.

Table 5.
Table showing how the treatment plans were changed following the CBCT examination.
4. Discussion
The International Commission on Radiological Protection (ICRP) states that for paediatric patients the use of dental CBCT is a concern, as radiation risk is age-dependent and paediatric patients are much more susceptible to stochastic biological effects. The multiplication factor for radiation risk in patients younger than 10 years is ×3, and for patients between 10 and 16 years, it is ×2. This relative attributable lifetime risk is based upon an average population relative risk of 1 at age 30 [10].
For this reason, appropriate justification for each CBCT examination in the paediatric patient is crucial for patient risk reduction. The referral criteria used in the dental hospital for paediatric patients are “Cone beam CT for dental and maxillofacial radiology (evidence-based guidelines)” published by the European Commission [5] and “Selection Criteria for Dental Radiography” published by the Faculty of General Dental Practice [4].
The results of this service evaluation are in consensus with a comparable service evaluation conducted by Mizban et al., 2019, in a department of paediatric dentistry in London [17]. Both have demonstrated that the CBCT was invaluable in enabling the clinicians to confirm the provisional treatment plans, aiding in surgical planning and procedure in a proportion of cases. Its value was further evidenced by effecting change in treatment plan and hence management of approximately a third (31%, 16/52) of paediatric patients in this study and 44% (22/50) in the study conducted by Mizban et al. (Table 5) [17].
Analysis of the data reveals that the most common principal clinical diagnosis in cases where a CBCT was requested in our cohort of patients was unerupted, ectopic, impacted teeth or supernumerary cases (Table 2). While the most common reason for referral for a CBCT scan was to aid in localisation of unerupted/impacted teeth or supernumerary teeth, assess the presence and extent of root resorption, and assist the clinicians in surgical treatment planning. This is in agreement with a recent retrospective UK study that showed that the most common reasons for requesting CBCT were to assess localisation of the developing dentition (46%) [19].
The majority of CBCT referrals requesting localisation of unerupted, ectopic or impacted teeth were allied with an impacted, ectopic maxillary canine. Precise localisation is needed in determining the feasibility of as well as guiding access for the surgical approach and direction for the application of orthodontic forces. Assessment of tooth location, using conventional radiological modalities, relies upon the use of parallax movement between images taken with different perspectives. Information gathered by CBCT imaging on the bucco–palatal position, inclination of the long axis of the tooth, quantity of overlying bone, presence and condition of adjacent root resorption, and the stage of dental development, enables more accurate localisation of impacted teeth [20].
These cases were often associated with a high suspicion of resorption of the adjacent roots. This is apparent, as root resorption was the most common additional reason for requesting a CBCT for the localisation of unerupted, ectopic teeth (Table 4). CBCT scans in our review proved invaluable in diagnosing cases of root resorption as CBCT aided to identify the location and extent of resorption of roots more effectively than the conventional radiographs that were taken previously. This was particularly relevant on the buccal and palatal surfaces of the teeth that are not easily identified on conventional radiographs. This increased the clinicians’ confidence in confirming the diagnosis in all cases.
Figure 1 represents an impacted canine case that was referred for CBCT to assess localisation and the extent of root resorption after the panoramic radiographic revealed root resorption of the upper right central incisor. The provisional treatment plan, which suggested the surgical exposure of the upper right canine for orthodontic alignment into the upper right central incisor position, was altered following the acquisition of additional information from the CBCT. The CBCT revealed the exact inclination of the long axis of the canine, the extent and location of the root resorption of the upper right central incisor and of the upper right lateral incisor. Due to the unfavourable oblique position of the upper right canine, the treatment plan was revised for its surgical removal. The upper right central incisor was deemed poor prognosis due to the significant resorption visualised in the apical root third with pulpal involvement and was to be closely monitored alongside the upper right lateral incisor.
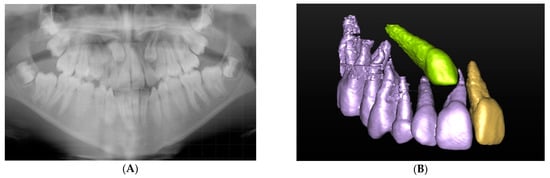
Figure 1.
(A) Panoramic radiograph showing bilateral ectopic and impacted canines. (B) Three-dimensional (3D) segmented reconstruction showing the position of the upper right ectopic canine localisation and associated resorption of the upper right central incisor (©DentsplySirona-Simplant® Pro).
Failure to diagnose and manage this ectopic upper canine and resorption of adjacent teeth efficiently, could have resulted in more complex treatment becoming necessary and be costly in time for both the patient and clinician. The Royal College of Surgeons suggest that it may also lead to litigation claims [21]. Although, not always of clinical significance, one study using CBCT imaging detected root resorption in 66.7% of permanent lateral incisors adjacent to ectopic maxillary canines [22]. In a clinical study, Alqerban et al., 2011, compared observers’ detection of root resorption in relation to impacted canine teeth. A higher detection rate of “slight” resorption and a lower detection rate of “no resorption” was reported when the observer used CBCT compared with panoramic radiographs [23]. An in-vitro study, which compared the accuracy of diagnosis of simulated resorption cavities, concluded that, overall, CBCT scans exhibited greater sensitivity and specificity. However, it must be noted that panoramic radiography and not intraoral radiographs were used for comparison and the study did not have a reference standard [24].
The importance of CBCT in pre surgical assessment has been discussed in the European Commission document for evidence-based guidelines for CBCT. The European Commission document states, “CBCT may be indicated for pre-surgical assessment of an unerupted tooth in selected cases where conventional radiographs fail to provide the information required” [5]. Similarly, UK guidance suggests that CBCT has a role in the assessment of impacted teeth with possible resorption of the adjacent teeth where lower dose conventional radiography has failed to provide the necessary information [4,25]. Other indications include the assessment of dilacerated teeth, surgical planning of the removal of unerupted teeth, and supernumeraries, and in the assessment of cleft palate [25].
The CBCT scan reports proved invaluable in assisting the clinicians confirm and guide the surgical treatment plan and thus justified the radiation dose, as demonstrated in Figure 2. The panoramic and upper standard occlusal radiography aided in the detection of a mixed complex-compound odontome in the left anterior maxilla, but provided insufficient information for management and treatment planning. The capacity of CBCT to provide three-dimensional multiplanar reconstruction of the region of interest allows visualisation of the anatomical structures possible from all viewpoints. This aided in the surgical excision of the odontome to minimise any damage to adjacent teeth and structures.
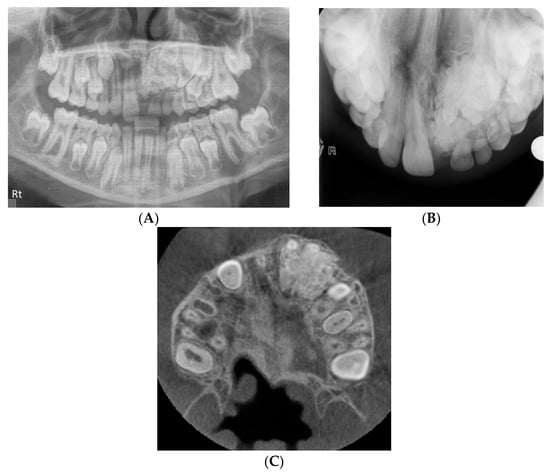
Figure 2.
(A) Panoramic radiograph showing a mixed complex-compound odontome in the left anterior maxilla. (B) Upper standard occlusal view of the mixed complex-compound odontome. (C) CBCT axial view demonstrating the full extent of the odontome and its relationship to the teeth.
Gürler et al., acknowledge that although “initial diagnosis [of supernumerary teeth] can be made using conventional techniques, further evaluation by CBCT is recommended” [26]. An evaluation of 626 supernumerary teeth by Liu et al., 2007, found a statistically significant increase in accuracy in localisation when using three-dimensional parameters compared with two-dimensional [27]. CBCT provides accurate linear measurement of the distances from the anatomical landmarks, which facilitates less invasive surgical planning [26].
Indeed, there were multiple cases where a greater number of unerupted supernumeraries was detected following CBCT assessment and, therefore, helped avoid treatment errors. Figure 3 illustrates a case where four additional supernumerary teeth could be located on the CBCT that were not detected on the panoramic view and would have been missed. Superimposition of the anatomical structures on conventional scans could affect the management of the case as a whole and possibly result in a repeat general anaesthetic for the patient in the future.
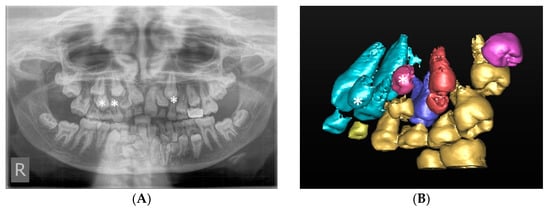
Figure 3.
(A) Panoramic radiograph demonstrating multiple supernumerary teeth in the maxilla and mandible. There are three clearly visible supernumerary teeth in the maxilla (marked with asterisks. (B) Three-dimensional (3D) segmented reconstruction of the right maxilla viewed from the palatal aspect showing two further maxillary supernumerary teeth marked with an asterisk, one palatal to the upper right central incisor and the other palatal to the upper right canine (©DentsplySirona-Simplant® Pro).
Out of the 12 cases referred for assessment of supernumerary teeth, the clinician was querying the presence of a supernumerary in two cases. In both of these cases, the CBCT confirmed no supernumerary teeth in the anterior maxilla and revealed that the periapical condition of all of the anterior teeth to be normal. Thus, unnecessary and invasive dental and surgical interventions were avoided.
The presence of supernumerary teeth can pose a challenge to the clinician’s ability to distinguish the supernumerary from the true tooth, as illustrated in Figure 4. This case was referred for CBCT to differentiate the true lateral incisor tooth and the supplemental tooth. The supplemental lateral incisor was identified as the palatally positioned tooth, following a CBCT assessment of the more rudimentary tooth morphology. Precise morphological measurements and accurate localisation of teeth from CBCT images allow the clinician to make an informed decision on which tooth to extract and the optimal surgical approach to reduce the risk of damage to the true tooth.
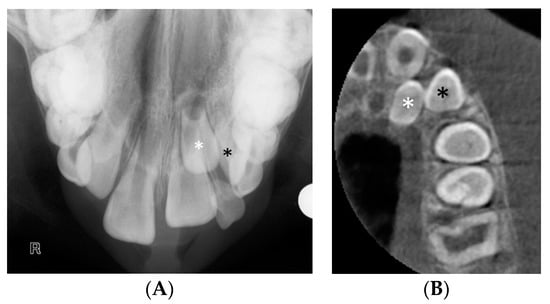
Figure 4.
(A) The upper standard occlusal shows a supplemental tooth in the maxillary left lateral incisor area. It is difficult to discern from the conventional views which of the two teeth, marked with a white and a black asterisk would be morphologically optimal to serve as the lateral incisor. (B) CBCT axial view of the left maxilla. An analysis of the dimensions of the teeth revealed that the tooth marked with the white asterisk was smaller compared to the adjacent unerupted tooth and the contralateral lateral incisor, and as such, more likely to represent the supplemental lateral incisor.
A number of case reports and non-systematic reviews have highlighted the value of CBCT for identification of periapical pathology or lesions in selected cases [28,29]. The cases referred for CBCT at UDH, Cardiff, were indicated for periapical assessment, when there was a lack of consensus between the findings from conventional radiographs and the clinical signs and symptoms.
There is limited literature documenting the benefit of CBCT on the detection of root fractures. In vitro studies document an overall increased accuracy of detecting vertical root fractures using CBCT [29,30]. However, the presence of root fillings in teeth may reduce specificity by artefact [30].
The smallest CBCT volume compatible with the clinical scenario should always be selected. In our service, the vast majority of scans were undertaken using a 5 cm x 5 cm scan. This is the smallest volume possible on this particular CBCT unit. The advantage of using a smaller volume is the lower radiation dose to the patient and potentially, a better contrast in the CBCT image as a result of reduced scatter [5]. Choosing the smallest volume size possible is one of the best ways of optimising the radiation dose. Other ways include selecting optimal exposure factors and by reducing the arc of rotation. In all cases, a “standard resolution” scan with automatic exposure control was chosen, which ensured optimal exposure factors were employed. The OP300 Maxio (Instrumentarium Dental, Tuusula, Finland) uses a 195° rotation rather than a 360° rotation, which further reduces dose to the patient by reducing the number of “frames” or “projections” obtained.
There is a lack of agreed guidelines for using CBCT in paediatric dentistry. Because of the limited diagnostic value of conventional radiographs for complex cases, CBCT has many indications. In the light of the detailed information obtained from CBCT scans and additional incidental findings, treatment plans and management of the paediatric patients were confirmed or revised for all cases. However, this may not always correlate with better outcomes for paediatric patients.
The authors acknowledge that one of the limitations of this service review is the sample size, with only 52 cases included. Furthermore, since the review period was 12 months, patients who received a previous CBCT were not included. This cohort of patients is important to audit. Further research is necessary to understand the use and impact of CBCT on children by dentists in all settings, since this study excluded CBCT referrals made by external practitioners. In contrast to the findings in this study, a questionnaire conducted by the European Academy of Paediatric Dentistry (EAPD) and the Turkish Society of Paediatric Dentistry (TSPD) reported that “pathology of the jaws” was the most common indication paediatric dentists requested a CBCT investigation. They further reported that 36% of paediatric dentists had no knowledge of CBCT [31].
5. Conclusions
CBCT has many indications in complex paediatric cases where conventional radiographs provide limited diagnostic value. Appropriate case selection and judicious use of CBCT can significantly alter the diagnoses and management and influence tooth restorability in commonly encountered clinical cases in paediatric dental departments. Clinicians should continue to exercise caution by requesting this investigation in selective cases in order to minimise the risk for their paediatric patient. This includes ensuring all CBCT examinations are justified, optimised, and that the service is evaluated regularly.
Author Contributions
Conceptualization, S.K.B.; methodology, formal analysis, data curation, writing—original draft preparation, C.H.; writing—review and editing and supervision, S.K.B. and N.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This service review was registered and approved by the Paediatric Dentistry and Orthodontics Quality and Safety Group, reference number 6824, Cardiff and Vale University Health Board on 20 November 2019.
Informed Consent Statement
Informed consent was not required, as this was a service review and the data was collected anonymously.
Data Availability Statement
Records of paediatric patients undergoing CBCT in University Dental Hospital, Cardiff, is accessible from the radiology daybook.
Acknowledgments
The authors would like to thank all of the radiographers, audit administration staff, and consultants in the Paediatric Dentistry Department, UDH, Cardiff, for their cooperation during the conduct of the service evaluation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Panchbhai, S.A. Wilhelm Conrad röntgen and the discovery of X-rays: Revisited after centennial. J. Indian Acad. Oral Med. Radiol. 2015, 27, 90–95. [Google Scholar] [CrossRef]
- Saati, S.; Kaveh, F.; Yarmohammadi, S. Comparison of Cone Beam Computed Tomography and Multi Slice Computed Tomography Image Quality of Human Dried Mandible using 10 Anatomical Landmarks. J. Clin. Diagn. Res. 2017, 11, ZC13–ZC16. [Google Scholar] [CrossRef]
- Horner, K.; O’Malley, L.; Taylor, K.; Glenny, A.-M. Guidelines for clinical use of CBCT: A review. Dentomaxillofac. Radiol. 2015, 44, 20140225. [Google Scholar] [CrossRef]
- Horner, K.; Eaton, K.A. Selection Criteria for Dental Radiography, 3rd ed.; Faculty of General Dental Practice: London, UK, 2018. [Google Scholar]
- European Commission. Radiation Protection No 172: Cone Beam CT for Dental and Maxillofacial Radiology; Evidence Based Guidelines: A Report Prepared by the Sedentex CT Project, 2011 (v2.0); European Commission: Brussels, Belgium, 2012. [Google Scholar]
- Koong, B. Cone beam imaging: Is this the ultimate imaging modality? Clin. Oral Implant. Res. 2010, 21, 1201–1208. [Google Scholar] [CrossRef]
- Katheria, B.C.; Kau, C.H.; Tate, R.; Chen, J.-W.; English, J.; Bouquot, J. Effectiveness of impacted and supernumerary tooth diagnosis from traditional radiography versus cone beam computed tomography. Pediatr. Dent. 2010, 32, 304–309. [Google Scholar] [PubMed]
- Davies, J.; Johnson, B.; Drage, N. Effective doses from cone beam CT investigation of the jaws. Dentomaxillofac. Radiol. 2012, 41, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Pauwels, R.; Beinsberger, J.; Collaert, B.; Theodorakou, C.; Rogers, J.; Walker, A.; Cockmartin, L.; Bosmans, H.; Jacobs, R.; Bogaerts, R.; et al. Effective dose range for dental cone beam computed tomography scanners. Eur. J. Radiol. 2012, 81, 267–271. [Google Scholar] [CrossRef] [PubMed]
- Rehani, M.M.; Gupta, R.; Bartling, S.H.; Sharp, G.; Pauwels, R.; Berris, T.; Boone, J. ICRP Publication 129: Radiological Protection in Cone Beam Computed Tomography (CBCT). Ann. ICRP 2015, 44, 7–127. [Google Scholar] [CrossRef] [PubMed]
- The Ionising Radiation (Medical Exposure) Regulations (IRMER) No 1322; Department of Health: London, UK, 2017. Available online: https://www.legislation.gov.uk/uksi/2017/1322/made (accessed on 20 November 2019).
- Alamri, H.M.; Sadrameli, M.; Alshalhoob, M.A.; Sadrameli, M.; AlShehri, M.A. Applications of CBCT in dental practice: A review of the literature. Gen. Dent. 2012, 60, 390–400. [Google Scholar]
- Dobbyn, L.M.; Morrison, J.F.; Brocklebank, L.M.; Chung, L.L.-K. A survey of the first 6 years of experience with cone beam CT scanning in a teaching hospital orthodontic department. J. Orthod. 2013, 40, 14–21. [Google Scholar] [CrossRef]
- Kapila, S.; Conley, R.S.; Harrell, W.E. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofac. Radiol. 2011, 40, 24–34. [Google Scholar] [CrossRef]
- Nervina, J.M. Cone beam computed tomography use in orthodontics. Aust. Dent. J. 2012, 57, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo-Rivas, J.A.; Theodorakou, C.; Carmichael, F.; Murray, B.; Payne, M.; Horner, K. Use of cone beam CT in children and young people in three United Kingdom dental hospitals. Int. J. Paediatr. Dent. 2013, 24, 336–348. [Google Scholar] [CrossRef] [PubMed]
- Mizban, L.; El-Belihy, M.; Vaidyanathan, M.; Brown, J. An audit and service evaluation of the use of cone beam computed tomography (CBCT) in a paediatric dentistry department. Dentomaxillofac. Radiol. 2019, 48, 20180393. [Google Scholar] [CrossRef] [PubMed]
- NHS Health Research Authority. Do I Need Research Ethics Committee Approval? 2018. Available online: https://www.hra-decisiontools.org.uk/ethics/ (accessed on 20 November 2019).
- Gallichan, N.; Dixon, C.; Doughty, F.; Jorgenson, K.; Albadri, S. Cone Beam CT: How is it used in Paediatric Dentistry? Int. J. Paediatr. Dent. 2019, 29, 4–74. [Google Scholar]
- Weiss, R., II; Read-Fuller, A. Cone Beam Computed Tomography in Oral and Maxillofacial Surgery: An Evidence-Based Review. Dent. J. 2019, 7, 52. [Google Scholar] [CrossRef]
- Husain, J.; Burden, D.; McSherry, P.; Royal College of Surgeons (RCS). Management of the Palatally Ectopic Maxillary Canine. 2016. Available online: https://www.rcseng.ac.uk/-/media/files/rcs/fds/publications/canine-guideline-2016.pdf (accessed on 25 April 2020).
- Walker, L.; Enciso, R.; Mah, J. Three-dimensional localisation of maxillary canines with cone beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 418–423. [Google Scholar] [CrossRef]
- Alqerban, A.; Jacobs, R.; Fieuws, S.; Willems, G. Comparison of two cone beam computed tomographic systems versus panoramic imaging for localization of impacted maxillary canines and detection of root resorption. Eur. J. Orthod. 2011, 33, 93–102. [Google Scholar] [CrossRef]
- Alqerban, A.; Jacobs, R.; Souza, P.C.; Willems, G. In-vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 764.e1–764.e11. [Google Scholar] [CrossRef]
- Isaacson, K.G.; Thom, A.R.; Atack, N.E.; Horner, K.; Whaites, E. Guidelines for the Use of Radiographs in Clinical Orthodontics, 4th ed.; British Orthodontic Society: London, UK, 2015. [Google Scholar]
- Gürler, G.; Delilbasi, C.; Delilbasi, E. Investigation of Impacted Supernumerary Teeth: A Cone Beam Computed Tomograph (CBCT) Study. J. Istanb. Univ. Fac. Dent. 2017, 51, 18–24. [Google Scholar] [CrossRef]
- Liu, D.-G.; Zhang, W.-L.; Zhang, Z.-Y.; Wu, Y.-T.; Ma, X.-C. Three-dimensional evaluations of supernumerary teeth using cone-beam computed tomography for 487 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 103, 403–411. [Google Scholar] [CrossRef]
- Nakata, K.; Naitoh, M.; Izumi, M.; Inamoto, K.; Ariji, E.; Nakamura, H. Effectiveness of Dental Computed Tomography in Diagnostic Imaging of Periradicular Lesion of Each Root of a Multirooted Tooth: A Case Report. J. Endod. 2006, 32, 583–587. [Google Scholar] [CrossRef] [PubMed]
- Cotton, T.P.; Geisler, T.M.; Holden, D.T.; Schwartz, S.A.; Schindler, W.G. Endodontic Applications of Cone-Beam Volumetric Tomography. J. Endod. 2007, 33, 1121–1132. [Google Scholar] [CrossRef]
- Hassan, B.; Metska, M.E.; Ozok, A.R.; Van Der Stelt, P.; Wesselink, P.R. Comparison of Five Cone Beam Computed Tomography Systems for the Detection of Vertical Root Fractures. J. Endod. 2010, 36, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Giray, F.E.; Peker, S.; Yalcinkaya, S.E.; Kargul, B.; Aps, J. Attitudes and knowledge of paediatric dentists’ on digital radiography and cone beam computed tomography. J. Pak. Med. Assoc. 2019, 69, 205–210. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).