Commonalities between ENT Specialists and Oral Medicine Experts: Old HPV Diseases and New Oral HPV-Cancer along the Borders
Abstract
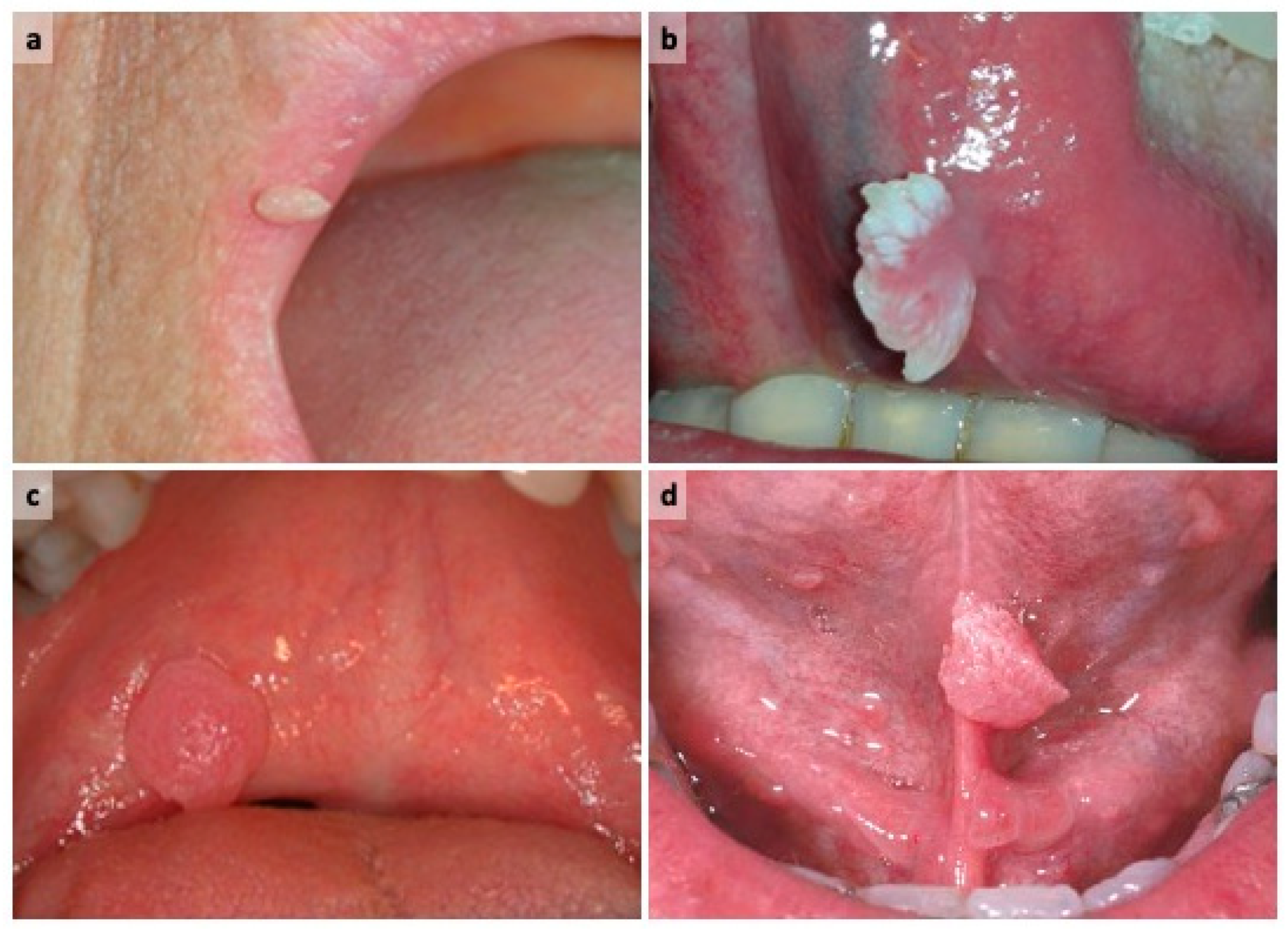
What does HPV oral oncology have in common with warts, papillomas and condylomata of the oral cavity and the oropharynx?
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Termine, N.; Campisi, G. Oral infection by Human papillomavirus: From warts to oral cancer. Focus on epidemiology, clinics, prevention and therapy. Dent. Cadmos 2015, 83, 307–321. [Google Scholar] [CrossRef]
- Campisi, G.; Panzarella, V. Human Papillomavirus Infection: A Risk Factor for Oral and Oropharyngeal Cancers. In Textbook of Oral Cancer Prevention, Diagnosis and Management; Warn, S., Greenspan, J.S., Eds.; Springer: Cham, Switzerland, 2020; pp. 31–45. [Google Scholar] [CrossRef]
- Hariri, S.; Unger, E.R.; Sternberg, M.; Dunne, E.F.; Swan, D.; Patel, S.; Markowitz, L.E. Prevalence of genital human papillomavirus among females in the United States, the National Health and Nutrition Examination Survey, 2003–2006. J. Infect. Dis. 2011, 204, 566–573. [Google Scholar] [CrossRef] [PubMed]
- De Vuyst, H.; Clifford, G.; Li, N.; Franceschi, S. HPV infection in Europe. Eur. J. Cancer 2009, 45, 2632–2639. [Google Scholar] [CrossRef] [PubMed]
- Gillison, M.L.; Broutian, T.; Pickard, R.K.L.; Tong, Z.Y.; Xiao, W.; Kahle, L.; Gilliso, M.L. Prevalence of oral HPV infection in the United States, 2009–2010. JAMA J. Am. Med. Assoc. 2012, 307, 693–703. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, G.; Kreimer, A.R.; Viscidi, R.; Pawlita, M.; Fakhry, C.; Koch, W.M.; Westra, W.H.; Gillison, M.L. Case–Control Study of Human Papillomavirus and Oropharyngeal Cancer. N. Engl. J. Med. 2007, 356, 1944–1956. [Google Scholar] [CrossRef] [PubMed]
- Elango, K.J.; Suresh, A.; Erode, E.M.; Subhadradevi, L.; Ravindran, H.K.; Iyer, S.K.; Iyer, S.K.R.; Kuriakose, M.A. Role of human papilloma virus in oral tongue squamous cell carcinoma. Asian Pac. J. Cancer Prev. 2011, 12, 889–896. [Google Scholar] [PubMed]
- Chernock, R.D.; Zhang, Q.; El-Mofty, S.K.; Thorstad, W.L.; Lewis, J.S. Human papillomavirus-related squamous cell carcinoma of the oropharynx: A comparative study in whites and African Americans. Arch. Otolaryngol Head Neck Surg. 2011, 137, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Farasat, S.; Yu, S.S.; Neel, V.A.; Nehal, K.S.; Lardaro, T.; Mihm, M.C.; Byrd, D.R.; Balch, C.M.; Califano, J.A.; Chuang, A.Y.; et al. A new American Joint Committee on Cancer staging system for cutaneous squamous cell carcinoma: Creation and rationale for inclusion of tumor (T) characteristics. J. Am. Acad. Dermatol. 2011, 64, 1051–1059. [Google Scholar] [CrossRef] [PubMed]
- Syrjänen, S.; Lodi, G.; von Bültzingslöwen, I.; Aliko, A.; Arduino, P.; Campisi, G.; Challacombe, S.; Ficarra, G.; Flaitz, C.; Zhou, H.M.; et al. Human papillomaviruses in oral carcinoma and oral potentially malignant disorders: A systematic review. Oral. Dis. 2011, 17, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Pannone, G.; Rodolico, V.; Santoro, A.; Lo Muzio, L.; Franco, R.; Botti, G.; Aquino, G.; Pedicillo, M.C.; Cagiano, S.; Campisi, G.; et al. Evaluation of a combined triple method to detect causative HPV in oral and oropharyngeal squamous cell carcinomas: p16 Immunohistochemistry, Consensus PCR HPV-DNA.; and In Situ Hybridization. Infect. Agent. Cancer 2012, 7, 4. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.; Greenspan, J.S. Textbook of Oral Cancer: Prevention, Diagnosis and Management; Springer: Cham, Switzerland, 2020. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campisi, G.; Mauceri, R.; Tozzo, P.; Panzarella, V. Commonalities between ENT Specialists and Oral Medicine Experts: Old HPV Diseases and New Oral HPV-Cancer along the Borders. Oral 2021, 1, 108-111. https://doi.org/10.3390/oral1020011
Campisi G, Mauceri R, Tozzo P, Panzarella V. Commonalities between ENT Specialists and Oral Medicine Experts: Old HPV Diseases and New Oral HPV-Cancer along the Borders. Oral. 2021; 1(2):108-111. https://doi.org/10.3390/oral1020011
Chicago/Turabian StyleCampisi, Giuseppina, Rodolfo Mauceri, Pietro Tozzo, and Vera Panzarella. 2021. "Commonalities between ENT Specialists and Oral Medicine Experts: Old HPV Diseases and New Oral HPV-Cancer along the Borders" Oral 1, no. 2: 108-111. https://doi.org/10.3390/oral1020011
APA StyleCampisi, G., Mauceri, R., Tozzo, P., & Panzarella, V. (2021). Commonalities between ENT Specialists and Oral Medicine Experts: Old HPV Diseases and New Oral HPV-Cancer along the Borders. Oral, 1(2), 108-111. https://doi.org/10.3390/oral1020011









