1. Introduction
Multiple myeloma (MM) is a disease characterised by the proliferation of neoplastic plasma cells that produce abnormal immunological proteins (The M-protein/paraprotein, or serum free light chains). Infiltration of the bone marrow by these cells impedes normal haematopoiesis leading to anaemia and other cytopenias. Additionally, damage to other organs, including the renal and skeletal system, can result in further complications e.g., hypercalcaemia. The combination of these effects can lead to impairments in physical, psychological and social domains of QOL.
In the UK, approximately 5820 new cases of MM are diagnosed each year. This number has increased by about a third since the early 1990s [
1]. Treatment is antimyeloma chemotherapy and immunotherapy targeted at the abnormal plasma cell population within the bone marrow. Effective responses are monitored by a corresponding reduction in the plasma concentration of the paraprotein/serum free light chains. The treatment of MM has dramatically changed over the last few decades as significant advances in the understanding of the pathogenesis of the condition have led to the development of novel therapeutic agents with a high efficacy. This has resulted in both improved progression-free and overall survival rates for patients with MM. With increasing numbers of such patients living longer, additional factors such as ageing and the development of other co-morbidities impact the patients’ global sense of well-being. The challenge now is how to ensure quality of life keeps pace with improved survival. Supportive and holistic care is vital to this end. The 2011 British Society of Haematology guidelines on supportive care in MM are the most comprehensive guideline with this aspect of management produced to date [
2]. These guidelines stress the importance of effective supportive care, from initial diagnosis to end of life. The Holistic needs assessment (HNA) was developed as a tool to comprehensively assess physical, emotional, mental, spiritual and social concerns to help formulate an individual care plan for each patient. The UK NHS NICE Guidance for Supportive and Palliative Care recommends that all cancer patients should have a HNA at key points in their disease trajectory [
3]. The problem is how to practically integrate these measures into everyday practice where demands on the clinician’s time continue to escalate and MM clinics are becoming increasingly busy.
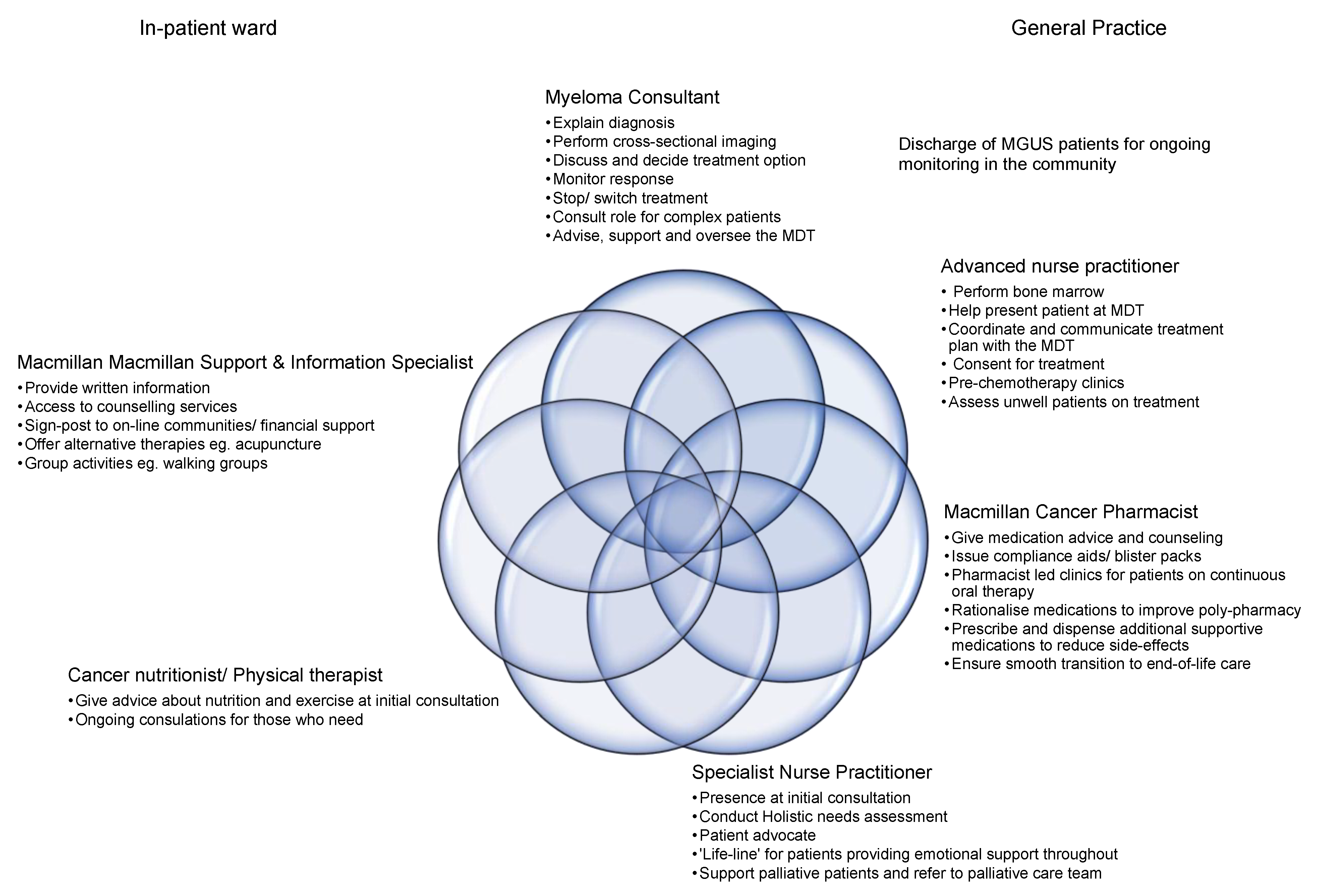
This review focuses on the holistic needs of a patient with MM by describing how each individual within the multidisciplinary team (MDT) has a role to play in supporting the patient through their diagnosis, treatment, and beyond. The aim of this paper is to assist and encourage centres to develop systems and pathways to allow time for the physical, emotional and spiritual needs of the patient to be identified and addressed, thus enabling patients with MM to live better lives.
2. The Myeloma Specialist
There are, essentially, two pathways whereby patients with MM reach the specialist clinic; these being the general practitioner or via referral from a speciality within secondary care establishments (
Figure 1). In both cases, results from analysis of protein electrophoresis or serum-free light chains may likely be available, and the role of the MM specialist is to explain the significance of the findings and the next steps that are required. The latter are likely to include further blood tests, cross-sectional imaging and potentially a bone marrow biopsy (
Figure 1). The decision to proceed to a bone marrow biopsy is often guided by the level of the paraprotein/light chain load and the presence of end-organ damage, but additional factors such as age, frailty, other comorbidities, and also the patients’ wishes, may come into play. The involvement of the patients’ family is often of crucial importance at this stage. The role of the MM specialist nurse practitioner (SNP) is also central at this point. For patients with a low level paraprotein, and without evidence of end-organ damage, no active intervention is likely to be required. The diagnosis is explained to the patient by the MM specialist who may then be discharged back to the general practitioner for ongoing monitoring in primary care (
Figure 1). For those patients who are confirmed to have a diagnosis of MM, the next steps are to explain that myeloma remains a treatable, but incurable, condition that has a remitting and relapsing nature. This is often omitted at the initial consultation yet is key in helping manage the patient’s expectations about their condition and the trajectory of the disease.
At diagnosis, the MM clinician should score patients using the Revised International Staging Score (R-ISS), which uses β2 microglobulin, albumin, lactate dehydrogenase and the presence of cytogenetic abnormalities (17p13 deletion, t(4;14) and t(14;16)) to define three prognostic groups [
4]. Next generation sequencing techniques are revealing the complex genomic landscape of MM, with an increasing number of genetic mutations now identified, as being associated with a poor prognosis; for example,
CCND1,
ATM and
TP53 [
5].
The challenge is how to use this cytogenetic and genetic information to tailor therapy. The poor risk associated with t(4;14) is partly overcome by treatment with bortezomib-based therapy and t(11:14) [
6]. The degree of MCL1-M expression may also help define who may benefit from bortezomib treatment [
7] Tailored therapy will hopefully improve clinical outcomes and reduce the costs and potential toxicities associated with ineffective treatment.
Treatment options should be outlined to the patient and their family. An increasing number of assessment tools have been developed to help with the complex evaluation of whether patients are transplant eligible or not, and also to weigh up the impact of the co-morbidities [
8] The HNA should be completed at this stage, and not only reviewed by the SNP, but fed back to the clinician to help guide treatment goals. Once the patient is established on treatment, close follow-up is crucial to assess for treatment tolerability and toxicity; the cancer pharmacist and advanced nurse practitioner (ANP) are key in this process.
Response to treatment should be assessed after each cycle and treatment adjustments undertaken if necessary. On rare occasions there is a need to discontinue treatment and consider alternative options. Given the gradual move away from fixed duration treatment to continuous therapy, increasing numbers of patients remain on active therapy for long periods of time. If one considers this together with the increasing number of MM patients presenting to the clinic, and the improved survival times, with patients living to fourth and fifth relapses and beyond, the demand on the MM clinician is growing considerably. Extra resources used to manage the expanding follow-up of stable patients include clinics undertaken by the ANP, SNP and myeloma cancer pharmacist. The MM clinician’s role is therefore gradually evolving from one of a “hands on”, lifelong relationship with many individual patients, to a more consultative function supporting these additional clinics. The consultant continues to see and assess new or complex patients in addition to acting in an advisory capacity to his/or her other myeloma team members.
3. The Specialist Nurse Practitioner
The relationship between MM patients and the SNP is a life-long relationship that often develops into a close association and fosters a great deal of trust between the two parties. Consequently, patients often confide to a greater degree in the SNP than the myeloma specialist, or indeed members of their own family. The role is therefore a privileged position, which must be respected in the myeloma service, and care must be taken to ensure that a SNP is engaged at all key stages in the patient’s journey: diagnosis, relapses, and end-of life. MM is an unpredictable disease, owing to a constant cycle of remission and relapse, which can result in significant emotional and physical uncertainty for the patient. SNPs are constant figures through this uncertainty. They are a life-line for patients, able to address concerns, angst and worry by providing telephone advice and support through difficult stages of their condition. The HNA is a recommended requirement for newly diagnosed MM patients, ref. [
3] which should be considered at the commencement and conclusion of each treatment to identify individual patient needs and concerns. Through the HNA, the SNP has an in-depth understanding of the patients’ wishes and concerns. They are the patient’s advocate during clinic consultations and MDT discussions and act to ensure that all decisions consider the individual needs of the patient rather than focus solely on disease management. The future role of the SNP is constantly evolving. The huge demands on the MM specialist have led to the development of nurse-led clinics, particularly for asymptomatic patients not requiring treatment and for follow-up support and survivorship assessments. This is a positive move and will hopefully ensure patients have better access to individualised and high-quality care. The development of the ANP role has helped ensure that the SNP can still be there in a supportive capacity for the patient, providing emotional support by conveying trust, confidence, hope and emotional warmth; a role which is crucial to allow the holistic needs of the MM patient to be met.
4. The Advanced Nurse Practitioner
The ANP, or advanced clinical practitioner, is a relatively new role which links the medical and nursing components of the healthcare professional [
9]. The ANP combines the position of the SNP, as patient advocate, with the clinician who prescribes and is able to formulate patient management plans. The SNP and ANP roles differ in that of knowledge, leadership, and responsibility [
10]
Table 1 outlines the specific differences with reference to the MM patient. ANPs are integral members of the MDT and their contribution is becoming increasingly valued within the MM setting due to the increasing demands on both the SNP and MM clinician.
ANP-led clinics have been established where bone marrow biopsies are undertaken, and have been beneficial both for the MM clinician (who is free to undertake other clinical duties) and the patients (who are given more time pre and post procedure). This is particularly important given that many of the patients with MM are often of an advanced age, frail and have other comorbidities and that demand additional time and care during the procedure.
The advanced training and knowledge of the ANP enables them to assess and consent MM patients for systemic anticancer therapy (SACT). The additional time the ANP can spend with the patient helps consolidate understanding. Pre-SACT nurse-led clinics were developed to help reduce the risk of errors occurring within a SACT setting and to ensure the patient’s needs are addressed promptly. In these clinics, the ANP carefully assesses tolerability to treatment, which allows potential toxicities to be identified and addressed early. Such intervention can also lead to improved compliance [
11].
Utilising their extensive clinical knowledge, the ANP is also ideally placed to help coordinate a teaching programme for the chemotherapy nurses. This is particularly important for MM, given the increasingly complexity of novel regimens now available. The ANP has become a major asset to MM services. The combination of their nursing and clinical skills allows a holistic approach [
12], permitting the MM patient to be treated as a ‘whole’.
5. The Specialist Cancer Pharmacist
The role of the specialist cancer pharmacist is, in many cases, an underutilised resource, particularly in the management of MM patients where there has been a significant increase in the number and complexity of emerging treatment regimens in recent years. The specialty is exceptionally placed to support both other healthcare professionals and MM patients themselves.
Current systemic anticancer treatments (SACT) for MM vary from simple single agent regimes to duplet and triplet treatments, with the drugs being given by various routes of administration. The majority of protocols contain supportive care drugs that can, on occasion, constitute as many as eight additional medications. This can often be overwhelming for patients when added to their pre-existing prescribed medications. The specialist pharmacy team can help by providing expert medication counselling and options for patient support. The latter can include resources such as compliance charts or blister-packs that can significantly improve patient compliance with multi-medication treatment regimens.
Specialist cancer pharmacists can advise about medication side effects, and by working closely alongside the ANP in their nurse-led pre-chemotherapy clinics can identify problems that allow earlier intervention (e.g., antiemetic therapy). This enables patients to be maintained on optimal SACT dosing and avoid treatment interruptions. The cancer pharmacists’ specialist knowledge of medication also means that they are well placed to support the ANP when reviewing patient treatment directed at problems such as pain relief, peripheral neuropathy and other common side effects associated with anti-MM treatment and the disease itself.
Similar to the nurse practitioners, the role of specialist cancer pharmacists continues to evolve. Specialist pharmacists are well placed to conduct oral SACT clinics for MM patients, particularly those established on long-term treatments incorporating immunomodulatory drugs. This allows the ANP to focus on patients receiving subcutaneous and intravenous treatments. Their role could also include review of other medications and suggest discontinuation of unnecessary drugs, thereby reducing poly-pharmacy and the inherent risks it generates.
In order to undertake many of the tasks outlined above the specialist pharmacist is ideally based on the day case chemotherapy unit, thereby allowing ease of access for both the clinicians and patients. They are independent prescribers, able to prescribe and supply medication at the time SACT treatment is being administered. This ‘one-stop-shop’ allows a medication review as well as facilitating dispensing and supply of medication from a satellite pharmacy based on the unit, facilitating reduced visits to, and waiting time in, the pharmacy, further improving the patient experience.
Specialist Macmillan pharmacists are another group of healthcare workers that can be engaged at any stage of a patient’s treatment, including an important role in providing input in end-of-life care.
6. The MacMillan/Psychological and Alternative Support
The Macmillan Support and Information Specialist assists the newly diagnosed MM patients by helping them understand and process the impact and shock of a new diagnosis. Although nonclinical, the team understands the condition and is able to reassure patients that whilst MM is incurable, long term intervention and support can be offered. This can provide an immense sense of relief to those affected and their families. The Macmillian team helps establish the patients’ own ‘personal network’ of support, but also offers psychological support and alternative therapies.
Complementary therapies are also offered in the form of reflexology, Indian head massage and light touch body massage which are useful to help with pain, improve fatigue and sleep patterns, and enhance a sense of general wellbeing. The therapies, above all else, aim to promote relaxation for the patient during clinical treatment interventions.
The team offers activities to prevent the myeloma from ‘taking over’. Physical activity is encouraged through gentle walking groups. This greatly helps support the patient with MM, where anaemia, pain and treatment-related fatigue can often be over-whelming.
Professional person-centred counselling is available in a nonclinical, safe space for up to a six-month period, for either the patient or carer. This intervention alone can alleviate significant emotional suffering, ease fears and concerns, and helps patients manage the roller coaster of MM treatment.
For patients who decline counselling, online communities can help lessen fear and worry. Patients can share their stories which provides a sense of connection, recognising they are not alone can be empowering for some patients. The Macmillan team can also signpost patients to practical, financial and benefit helplines which can all play their part in this holistic approach to patient care.
7. Conclusions
An increasing number of MM patients are diagnosed each year, and highly efficacious anti-MM agents are now available to treat these patients. Patients are living longer, often to fifth line therapy and beyond. There has also been a trend away from fixed-duration treatment to continuous therapy. The result is an increasingly stretched and time poor MM clinician. This abstract focuses a spotlight on the crucial roles of each individual member in the MDT, and how an effective MM service needs to recruit the diverse expertise of each to ensure that MM patients are assessed thoroughly, and holistically, during their diagnosis, treatment and beyond.
Our vision of the future is a MM clinic where patients rotate from the MM specialist, who explains the diagnosis and treatment overview, to the ANP for a bone marrow biopsy, further explanation of the treatment plan and obtaining consent. The patient will then have the opportunity to spend more time with the SNP reviewing the HNA. If required, the patient will have the opportunity to meet a dietician and physiotherapist before being introduced to the Macmillan support and information team to learn how additional counselling and alternative therapy can be accessed. The specialist cancer pharmacist will introduce themselves at diagnosis and meet with the patient on the chemotherapy unit on day one of treatment to explain the regimen and supportive medications. Follow-up consultations will similarly involve the MM clinician, if required, but will be focused on close-follow up ANP and cancer pharmacist to assess for treatment toxicities, with SNP and Macmillan team support to ensure patients are emotionally coping with treatment.
The diagnosis and treatment of MM was historically the sole remit of the MM specialist, but this model needs to be reformed to match current day demands, both in terms of the number and complexity of the modern-day MM patient. A shake-up of our rigid clinician-approach to care is required, and the expertise of the ANP, SNP, cancer pharmacist and Macmillan cancer specialist are all crucial to a future clinic-model focusing on providing high-quality, holistic, patient-centred care.