Biomacromolecules as Immunomodulators: Utilizing Nature’s Tools for Immune Regulation
Abstract
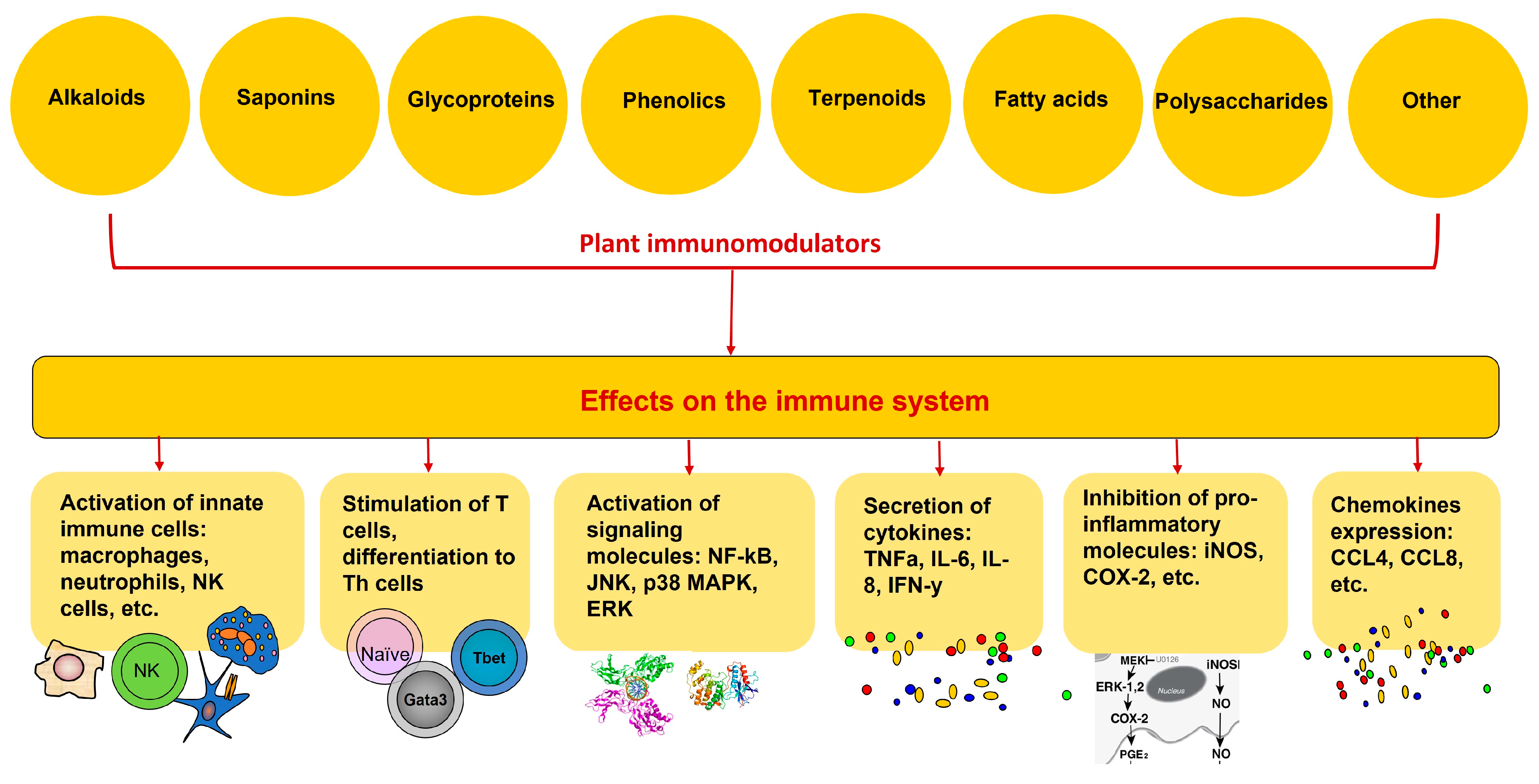
:1. Introduction
2. Immunity, Immune System, and Immunomodulators
3. Selected Medicinal Plants with Immunomodulatory Activity
4. Selected Plant Chemicals with Immunomodulatory Activity in Clinical Trials
4.1. Resveratrol
4.2. Curcumin
4.3. Quercetin
4.4. Capsaicin
4.5. Epigallocatechin-3-gallate
4.6. Andrographolide
4.7. Genistein
4.8. Colchicin
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Puri, A.; Saxena, R.; Saxena, R.P.; Saxena, K.C.; Srivastava, V.; Tandon, J.S. Immunostimulant activity of Nyctanthes arbor-tristis, L.J. Ethnopharmacol. 1994, 42, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Li, Y. The unexpected side effects and safety of therapeutic monoclonal antibodies. Drugs Today 2014, 50, 33–50. [Google Scholar] [CrossRef] [PubMed]
- Golan, D.E. Principles of Pharmacology. In The Pathophysiologic Basic of Drug Therapy, 2nd ed.; Lippincott Williams & Wilkins: Pennsylvania, PA, USA, 2008; pp. 795–809. [Google Scholar]
- Hansel, T.T.; Kropshofer, H.; Singer, T.; Mitchell, J.A.; George, A.J. The safety and side effects of monoclonal antibodies. Nat. Rev. Drug Discov. 2010, 9, 325–338. [Google Scholar] [CrossRef]
- Bartelds, G.M.; Krieckaert, C.L.; Nurmohamed, M.T.; Van Schouwenburg, P.A.; Lems, W.F.; Twisk, J.W.; Dijkmans, B.A.; Aarden, L.; Wolbink, G.J. Development of antidrug antibodies against adalimumab and association with disease activity and treatment failure during long-term follow-up. JAMA 2011, 305, 1460–1468. [Google Scholar] [CrossRef] [PubMed]
- Auffenberg, C.; Rosenthal, L.J.; Dresner, N. Levamisole: A common cocaine adulterant with life-threatening side effects. Psychosomatics 2013, 54, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Oberlies, N.H.; Kroll, D.J. Camptothecin taxol: Historic achievements in natural products research. J. Nat. Prod. 2004, 67, 129–135. [Google Scholar] [CrossRef]
- Rakotoarivelo, N.H.; Rakotoarivony, F.; Ramarosandratana, A.V.; Jeannoda, V.H.; Kuhlman, A.R.; Randrianasolo, A.; Bussmann, R.W. Medicinal plants used to treat the most frequent diseases encountered in Ambalabe rural community, Eastern Madagascar. J. Ethnobiol. Ethnomed. 2015, 11, 68. [Google Scholar] [CrossRef]
- Mintah, S.; Asafo-Agyei, T.; Archer, M.; Atta-Adjei, P.; Boamah, D.; Kumadoh, D.; Appiah, A.; Ocloo, A.; Duah Boakye, Y.; Agyare, C. Medicinal Plants for Treatment of Prevalent Diseases. In Pharmacognosy-Medicinal Plants; Perveen, S., Al-Taweel, A., Eds.; IntechOpen: London, UK, 2019; Chapter 9. [Google Scholar] [CrossRef]
- Aschale, Y.; Wubetu, M.; Abebaw, A.; Yirga, T.; Minwuyelet, A.; Toru, M. A Systematic Review on Traditional Medicinal Plants Used for the Treatment of Viral and Fungal Infections in Ethiopia. J. Exp. Pharmacol. 2021, 13, 807–815. [Google Scholar] [CrossRef]
- Jantan, I.; Ahmad, W.; Bukhari, S.N. Plant-derived immunomodulators: An insight on their preclinical evaluation and clinical trials. Front. Plant Sci. 2015, 6, 655, Erratum in Front. Plant Sci. 2018, 9, 1178. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shukla, S.; Bajpai, V.K.; Kim, M. Plants as potential sources of natural immunomodulators. Rev. Env. Sci. Biotechnol. 2014, 13, 17–33. [Google Scholar] [CrossRef]
- Di Sotto, A.; Vitalone, A.; Di Giacomo, S. Plant-Derived Nutraceuticals and Immune System Modulation: An Evidence-Based Overview. Vaccines 2020, 8, 468. [Google Scholar] [CrossRef]
- Mohamed, S.I.A.; Jantan, I.; Haque, M.A. Naturally occurring immunomodulators with antitumor activity: An insight on their mechanisms of action. Int. Immunopharmacol. 2017, 50, 291–304. [Google Scholar] [CrossRef]
- Nair, A.; Chattopadhyay, D.; Saha, B. Chapter 17—Plant-derived immunomodulators. In New Lokk to Phytomedicine, Advancements in Herbal. Products as Novel Drugs Leads; Elsevier Inc.: Amsterdam, The Netherlands, 2019; pp. 435–499. [Google Scholar] [CrossRef]
- Pathak, S.; Fialho, J.; Nandi, D. Plant-based Immunomodulators and Their Potential Therapeutic Actions. J. Explor. Res. Pharmacol. 2022, 7, 243–256. [Google Scholar] [CrossRef]
- Kumar, S.; Arya, V.; Kaur, R.; Ali Bhat, Z.; Gupta, V.K.; Kumar, V. A review of immunomodulators in the Indian traditional health care system. J. Microbiol. Immunol. Infect. 2012, 45, 165–184. [Google Scholar] [CrossRef]
- Acharya, P.; Mohanty, S.; Mohanty, M. Immuno Protective Role of Medicinal Herbs as Phytotherapeutic Drugs in Ayurveda—A Prospective Approach for Defending COVID19. J. Nat. Ayurvedic Med. 2022, 6, 000342. [Google Scholar] [CrossRef]
- Huang, S.-C.; Kao, Y.-H.; Shih, S.-F.; Tsai, M.-C.; Lin, C.-S.; Chen, L.W.; Chuang, Y.-P.; Tsui, P.-F.; Ho, L.-J.; Lai, J.-H.; et al. Epigallocatechin-3-gallate exhibits immunomodulatory effects in human primary T cells. Biochem. Biophys. Res. Commun. 2021, 550, 70–76. [Google Scholar] [CrossRef]
- Alhazmi, H.A.; Najmi, A.; Javed, S.A.; Sultana, S.; Al Bratty, B.; Makeen, H.A.; Meraya, A.M.; Ahsan, W.; Mohan, S.; Taha, M.M.E.; et al. Medicinal Plants and Isolated Molecules Demonstrating Immunomodulation Activity as Potential Alternative Therapies for Viral Diseases Including COVID-19. Front. Immunol. 2021, 12, 637553. [Google Scholar] [CrossRef]
- Singh, N.; Tailang, M.; Mehta, C.S. A review on herbal plants as immunomodulators. Int. J. Pharm. Sci. Res. 2016, 7, 3602–3610. [Google Scholar]
- Tharakan, A.; Shukla, H.; Benny, I.R.; Tharakan, M.; George, L.; Koshy, S. Immunomodulatory effect of Withania somnifera (Ashwagandha) Extract-A Randomized, Double-Blind, Placebo Controlled Trial with an Open Label Extension on Healthy Participants. J. Clin. Med. 2021, 10, 3644. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dar, N.J.; Hamid, A.; Ahmad, M. Pharmacologic overview of Withania somnifera, the Indian Ginseng. Cell Mol. Life Sci. 2015, 72, 4445–4460. [Google Scholar] [CrossRef] [PubMed]
- Lopresti, A.; Smith, S. Ashwagandha (Withania somnifera) for the treatment and enhancement of mental and physical conditions: A systematic review of human trials. J. Herb. Med. 2021, 21, 00434. [Google Scholar] [CrossRef]
- Della Porta, M.; Maier, J.A.; Cazzola, R. Effects of Withania somnifera on Cortisol Levels in Stressed Human Subjects: A Systematic Review. Nutrients 2023, 15, 5015. [Google Scholar] [CrossRef]
- Akhgarjand, C.; Asoudeh, F.; Bagheri, A.; Kalantar, Z.; Vahabi, Z.; Shab-Bidar, S.; Rezvani, H.; Djafarian, K. Does Ashwagandha supplementation have a beneficial effect on the management of anxiety and stress? A systematic review and meta-analysis of randomized controlled trials. Phytother. Res. 2022, 36, 4115–4124. [Google Scholar] [CrossRef]
- Fatima, K.; Malik, J.; Muskan, F.; Raza, G.; Waseem, A.; Shahid, H.; Jaffery, S.F.; Khan, U.; Zaheer, M.K.; Shaikh, Y.; et al. Safety and efficacy of Withania somnifera for anxiety and insomnia: Systematic review and meta-analysis. Human. Psychopharmacol. Clin. Exp. 2024, e2911. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, D.A.; Moreno, Y.; Gho, C.; Petro, J.L.; Odriozola-Martínez, A.; Kreider, R.B. Effects of Ashwagandha (Withania somnifera) on Physical Performance: Systematic Review and Bayesian Meta-Analysis. J. Funct. Morphol. Kinesiol. 2021, 6, 20. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Didio, F.P.; Duarte, A.R.; Stefani, G.P. Effects of the Withania somnifera supplementation on sports performance: A systematic review and meta-analysis. Nor. Afr. J. Food Nutr. Res. 2022, 6, 1–8. [Google Scholar] [CrossRef]
- Riaz, M.; Khalid, R.; Afzal, M.; Anjum, F.; Fatima, H.; Zia, S.; Rasool, G.; Egbuna, C.; Mtewa, A.G.; Uche, C.Z.; et al. Phytobioactive compounds as therapeutic agents for human diseases: A review. Food Sci. Nutr. 2023, 11, 2500–2529. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gupta, P.K.; Chakraborty, P.; Kumar, S.; Singh, P.K.; Rajan, M.G.R.; Sainis, K.B.; Kulkarni, S. G1-4A, a Polysaccharide from Tinospora cordifolia Inhibits the Survival of Mycobacterium tuberculosis by Modulating Host Immune Responses in TLR4 Dependent Manner. PLoS ONE 2016, 11, e0154725. [Google Scholar] [CrossRef]
- Wang, R.; Deng, X.; Gao, Q.; Wu, X.; Han, L.; Gao, X.; Zhao, S.; Chen, W.; Zhou, R.; Li, Z.; et al. Sophora alopecuroides L.: An ethnopharmacological, phytochemical, and pharmacological review. J. Ethnopharmacol. 2020, 248, 112172. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Wang, R.; Zhao, S.; Chen, D.; Hao, F.; Wang, B.; Zhang, J.; Ma, Y.; Chen, X.; Gao, X.; et al. Extraction, Separation, Antitumor Effect, and Mechanism of Alkaloids in Sophora alopecuroides: A Review. Separations 2022, 9, 380. [Google Scholar] [CrossRef]
- Zhang, L.-H.; Huang, Y.; Wang, L.-W.; Xiao, P.-G. Several Compounds from Chinese Traditional and Herbal Medicine as Immunomodulators. Phytother. Res. 1995, 9, 315–322. [Google Scholar] [CrossRef]
- Dinesh, P.; Rasool, M. Herbal Formulations and Their Bioactive Components as Dietary Supplements for Treating Rheumatoid Arthritis. In Bioactive Food as Dietary Interventions for Arthritis and Related Inflammatory Diseases, 2nd ed.; Watson, R.R., Preedy, V.R., Eds.; Academic Press: Cambridge, MA, USA, 2019; Chapter 22; pp. 385–399. ISBN 9780128138205. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, L.; Zhang, X.; Wu, D.; Chen, L.; Hu, C.; Wen, C.; Zhou, J. Tripterygium wilfordii glycosides ameliorates collagen-induced arthritis and aberrant lipid metabolism in rats. Front. Pharmacol. 2022, 13, 938849. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Han, M.; Li, Y.T.; Wang, Z.; Liu, J.P. Efficacy and safety of Tripterygium wilfordii polyglycosides for diabetic kidney disease: An overview of systematic reviews and meta-analyses. Syst. Rev. 2022, 11, 226. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coon, J.T.; Ernst, E. Panax ginseng. Drug Saf. 2002, 25, 323–344. [Google Scholar] [CrossRef]
- Shin, J.-Y.; Song, J.-Y.; Yun, Y.-S.; Yang, H.-O.; Rhee, D.-K.; Pyo, S. Immunostimulating Effects of Acidic Polysaccharides Extract of Panax Ginseng On Macrophage Function. Immunopharmacol. Immunotoxicol. 2002, 24, 469–482. [Google Scholar] [CrossRef]
- Pham, H.N.T.; Vuong, Q.V.; Bowyer, M.C.; Scarlett, C.J. Phytochemicals Derived from Catharanthus roseus and Their Health Benefits. Technologies 2020, 8, 80. [Google Scholar] [CrossRef]
- Mahomoodally, M.F. Traditional medicines in Africa: An appraisal of ten potent african medicinal plants. Evid. Based Complement. Altern. Med. 2013, 2013, 617459. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tawinwung, S.; Junsaeng, D.; Utthiya, S.; Khemawoot, P. Immunomodulatory effect of standardized C. asiatica extract on a promotion of regulatory T Cells Rats. BMC Complement. Med. Ther. 2021, 21, 220. [Google Scholar] [CrossRef]
- Batiha, G.E.-S.; Alqahtani, A.; Ojo, O.A.; Shaheen, H.M.; Wasef, L.; Elzeiny, M.; Ismail, M.; Shalaby, M.; Murata, T.; Zaragoza-Bastida, A.; et al. Biological Properties, Bioactive Constituents, and Pharmacokinetics of Some Capsicum spp. and Capsaicinoids. Int. J. Mol. Sci. 2020, 21, 5179. [Google Scholar] [CrossRef]
- Arado, G.M.; Amatto, P.P.G.; Marins, M.; Rizzi, E.S.; França, S.C.; Coppede, J.D.S.; Carmona, F.; Pereira, A.M.S. Anti-inflammatory and/or immunomodulatory activities of Uncaria tomentosa (cat’s claw) extracts: A systematic review and meta-analysis of in vivo studies. Front. Pharmacol. 2024, 15, 1378408. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Manayi, A.; Vazirian, M.; Saeidnia, S. Echinacea purpurea: Pharmacology, phytochemistry and analysis methods. Pharmacogn. Rev. 2015, 9, 63–72. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- David, S.; Cunningham, R. Echinacea for the prevention and treatment of upper respiratory tract infections: A systematic review and meta-analysis. Complement. Ther. Med. 2019, 44, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Gancitano, G.; Mucci, N.; Stange, R.; Ogal, M.; Vimalanathan, S.; Sreya, M.; Booker, A.; Hadj-Cherif, B.; Albrich, W.C.; Woelkart-Ardjomand, K.; et al. Echinacea Reduces Antibiotics by Preventing Respiratory Infections: A Meta-Analysis (ERA-PRIMA). Antibiotics 2024, 13, 364. [Google Scholar] [CrossRef] [PubMed]
- Pelvan, E.; Karaoğlu, Ö.; Fırat, E.Ö.; Kalyon, K.B.; Ros, E.; Alasalvar, C. Immunomodulatory effects of selected medicinal herbs and their essential oils: A comprehensive review. J. Funct. Foods 2022, 94, 105108. [Google Scholar] [CrossRef]
- Cosentino, M.; Bombelli, R.; Conti, A.; Maria, C.; Azzetti, A.; Bergamaschi, A.; Franca, M.; Lecchini, S. Antioxidant properties in vitro immunomodulatory effects of peppermint (Mentha x piperita l) essential oils in human leukocytes. J. Pharm. Sci. Res. 2009, 1, 33–43. Available online: https://www.sciencedirect.com/science/article/pii/S1756464622001785 (accessed on 21 August 2024).
- Ogaly, H.A.; Eltablawy, N.A.; Abd-Elsalam, R.M. Antifibrogenic Influence of Mentha piperita L. Essential Oil against CCl4-Induced Liver Fibrosis in Rats. Oxid. Med. Cell Longev. 2018, 2018, 4039753. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kong, C.K.; Low, L.E.; Siew, W.S.; Yap, W.-H.; Khaw, K.-Y.; Ming LCh Mocan, A.; Goh, B.-H.; Goh, P.H. Biological Activities of Snowdrop (Galanthus spp., Family Amaryllidaceae). Front. Pharmacol. 2021, 11, 552453. [Google Scholar] [CrossRef]
- Matić, S.; Stanić, S.; Mihailović, M.; Bogojević, D. Cotinus coggygria Scop.: An overview of its chemical constituents, pharmacological and toxicological potential. Saudi J. Biol. Sci. 2016, 23, 452–461. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Antal, D.; Ardelean, F.; Jijie, R.; Pinzaru, I.; Soica, C.; Dehelean, C. Integrating Ethnobotany, Phytochemistry, and Pharmacology of Cotinus coggygria and Toxicodendron vernicifluum: What Predictions can be Made for the European Smoketree? Front. Pharmacol. 2021, 12, 662852. [Google Scholar] [CrossRef]
- Moutia, M.; Habti, N.; Badou, A. In Vitro and In Vivo Immunomodulator Activities of Allium sativum L. Evid. Based Complement. Altern. Med. 2018, 2018, 4984659. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Uritu, C.M.; Mihai, C.T.; Stanciu, G.D.; Dodi, G.; Alexa-Stratulat, T.; Luca, A.; Leon-Constantin, M.M.; Stefanescu, R.; Bild, V.; Melnic, S.; et al. Medicinal Plants of the Family Lamiaceae in Pain Therapy: A Review. Pain. Res. Manag. 2018, 2018, 7801543. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Park, Y.-G.; Cho, J.-H.; Choi, J.; Ju, E.-M.; Adam, G.O.; Hwang, D.-I.; Lee, J.-H.; An, S.-Y.; Choi, H.-K.; Park, C.-B.; et al. Immunomodulatory effects of Curcuma longa L. and Carthamus tinctorius L. on RAW 264.7 macrophages and cyclophosphamide-induced immunosuppression C57BL/6 mouse models. J. Funct. Foods 2022, 91, 105000. [Google Scholar] [CrossRef]
- Różański, G.; Tabisz, H.; Zalewska, M.; Niemiro, W.; Kujawski, S.; Newton, J.; Zalewski, P.; Słomko, J. Meta-Analysis of Exploring the Effect of Curcumin Supplementation with or without Other Advice on Biochemical and Anthropometric Parameters in Patients with Metabolic-Associated Fatty Liver Disease (MAFLD). Int. J. Env. Res. Public Health 2023, 20, 4266. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barbalho, S.M.; de Sousa Gonzaga, H.F.; de Souza, G.A.; de Alvares Goulart, R.; de Sousa Gonzaga, M.L.; de Alvarez Rezende, B. Dermatological effects of Curcuma species: A systematic review. Clin. Exp. Dermatol. 2021, 46, 825–833. [Google Scholar] [CrossRef] [PubMed]
- Sunil, M.A.; Sunitha, V.S.; Radhakrishnan, E.K.; Jyothis, M. Immunomodulatory activities of Acacia catechu, a traditional thirst quencher of South India. J. Ayurveda Integr. Med. 2019, 10, 185–191. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sharififar, F.; Pournournohammadi, S.; Arabnejad, M. Immunomodulatory activity of aqueous extract of Achiella wilhelmsii C. Koch in mice. Indian J. Exp. Biol. 2009, 47, 668–671. [Google Scholar]
- Saeidnia, S.; Gohari, A.; Mokhber-Dezfuli, N.; Kiuchi, F. A review on phytochemistry and medicinal properties of the genus Achillea. Daru 2011, 19, 173–186. [Google Scholar] [PubMed] [PubMed Central]
- Rajanna, M.; Bharathi, B.; Shivakumar, B.R.; Deepak, M.; Prashanth, D.S.; Prabakaran, D.; Vijayabhaskar, T.; Arun, B. Immunomodulatory effects of Andrographis paniculata extract in healthy adults—An open-label study. J. Ayurveda Integr. Med. 2021, 12, 529–534. [Google Scholar] [CrossRef]
- Intharuksa, A.; Arunotayanun, W.; Yooin, W.; Sirisa-ard, P. A Comprehensive Review of Andrographis paniculata (Burm. f.) Nees and Its Constituents as Potential Lead Compounds for COVID-19 Drug Discovery. Molecules 2022, 27, 4479. [Google Scholar] [CrossRef]
- Bushmeleva, K.; Vyshtakalyuk, A.; Terenzhev, D.; Belov, T.; Parfenov, A.; Sharonova, N.; Nikitin, E.; Zobov, V. Radical Scavenging Actions and Immunomodulatory Activity of Aronia melanocarpa Propylene Glycol Extracts. Plants 2021, 10, 2458. [Google Scholar] [CrossRef]
- Ho, G.T.; Bräunlich, M.; Austarheim, I.; Wangensteen, H.; Malterud, K.E.; Slimestad, R.; Barsett, H. Immunomodulating activity of Aronia melanocarpa polyphenols. Int. J. Mol. Sci. 2014, 15, 11626–11636. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lewu, F.B.; Grierson, D.S.; Afolayan, A.J. The leaves of Pelargonium sidoides may substitute for its roots in the treatment of bacterial infections. Biol. Conserv. 2006, 128, 582–584. [Google Scholar] [CrossRef]
- Çiğdem, Y.; Şeker, K.G.; Bahadır, A.Ö.; Küpeli, A.E.; Hakan, B.T.; Eduardo, S.-S.; Michael, A.; Samira, S. Immunomodulatory and anti-inflammatory therapeutic potential of gingerols and their nanoformulations. Front. Pharmacol. 2022, 13, 902551. [Google Scholar] [CrossRef]
- Suciyati, S.W.; Adnyana, I.K. Red ginger (Zingiber officinale Roscoe var rubrum): A review. Pharmacologyonline 2017, 2, 60–65. [Google Scholar]
- Zakharchenko, N.S.; Belous, A.S.; Biryukova, Y.K.; Medvedeva, O.A.; Belyakova, A.V.; Masgutova, G.A.; Trubnikova, E.V.; Buryanov, Y.I.; Lebedeva, A.A. Immunomodulating and Revascularizing Activity of Kalanchoe pinnata Synergize with Fungicide Activity of Biogenic Peptide Cecropin P1. J. Immunol. Res. 2017, 2017, 3940743. [Google Scholar] [CrossRef]
- Coutinho, M.A.; Muzitano, M.F.; Cruz, E.A.; Bergonzi, M.C.; Kaiser, C.R.; Tinoco, L.W.; Bilia, A.R.; Vincieric, F.F.; Rossi-Bergmann, B.; Costa, S.S. Flowers from Kalanchoe pinnata are a rich source of T cell-suppressive flavonoids. Nat. Prod. Commun. 2012, 7, 175–178. [Google Scholar] [CrossRef] [PubMed]
- Anil, S.M.; Peeri, H.; Koltai, H. Medical Cannabis Activity Against Inflammation: Active Compounds and Modes of Action. Front. Pharmacol. 2022, 13, 908198. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Chamorro, I.; Santos-Sánchez, G.; Bollati, C.; Bartolomei, M.; Li, J.; Arnoldi, A.; Lammi, C. Hempseed (Cannabis sativa) Peptides WVSPLAGRT and IGFLIIWV Exert Anti-inflammatory Activity in the LPS-Stimulated Human Hepatic Cell Line. J. Agric. Food Chem. 2022, 70, 577–583. [Google Scholar] [CrossRef]
- Magcwebeba, T.; Swart, P.; Swanevelder, S.; Joubert, E.; Gelderblom, W. Anti-Inflammatory Effects of Aspalathus linearis and Cyclopia spp. Extracts in a UVB/Keratinocyte (HaCaT) Model Utilising Interleukin-1α Accumulation as Biomarker. Molecules 2016, 21, 1323. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Roza, O.; Lai, W.-C.; Zupkó, I.; Hohmann, J.; Jedlinszki, N.; Chang, F.-R.; Csupor, D.; Eloff, J.N. Bioactivity-guided isolation of phytoestrogenic compounds from Cyclopia genistoides by the pER8: GUS reporter system. S. Afr. J. Bot. 2017, 110, 201–207. [Google Scholar] [CrossRef]
- Noor-E-Tabassum Das, R.; Lami, M.S.; Chakraborty, A.J.; Mitra, S.; Tallei, T.E.; Idroes, R.; Mohamed, A.A.; Hossain, M.J.; Dhama, K.; Mostafa-Hedeab, G.; et al. Ginkgo biloba: A Treasure of Functional Phytochemicals with Multimedicinal Applications. Evid. Based Complement. Altern. Med. 2022, 2022, 8288818. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Oskoueian, E.; Abdullah, N.; Ahmad, S.; Saad, W.Z.; Omar, A.R.; Ho, Y.W. Bioactive compounds and biological activities of Jatropha curcas L. kernel meal extract. Int. J. Mol. Sci. 2011, 12, 5955–5970. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ramadan, M.F. Bioactive Phytochemicals from Jatropha (Jatropha curcas L.) Oil Processing Byproducts. In Bioactive Phytochemicals from Vegetable Oil and Oilseed Processing By-Products; Reference Series in Phytochemistry; Ramadan Hassanien, M.F., Ed.; Springer: Cham, Switzerland, 2022. [Google Scholar] [CrossRef]
- An, E.-K.; Hwang, J.; Kim, S.-J.; Park, H.-B.; Zhang, W.; Ryu, J.-H.; You, S.; Jin, J.-O. Comparison of the immune activation capacities of fucoidan and laminarin extracted from Laminaria japonica. Int. J. Biol. Macromol. 2022, 208, 230–242. [Google Scholar] [CrossRef] [PubMed]
- Yadav, N.; Shakya, P.; Kumar, A.; Gautam, R.D.; Chauhan, R.; Kumar, D.; Kumar, A.; Singh, S.; Singh, S. Investigation on pollination approaches, reproductive biology and essential oil variation during floral development in German chamomile (Matricaria chamomilla L.). Sci Rep. 2022, 12, 15285. [Google Scholar] [CrossRef]
- Singh, O.; Khanam, Z.; Misra, N.; Srivastava, M.K. Chamomile (Matricaria chamomilla L.): An overview. Pharmacogn. Rev. 2011, 5, 82–95. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Janeczek, M.; Moy, L.; Lake, E.P.; Swan, J. Review of the Efficacy and Safety of Topical Mahonia aquifolium for the Treatment of Psoriasis and Atopic Dermatitis. J. Clin. Aesthet. Dermatol. 2018, 11, 42–47. [Google Scholar] [PubMed] [PubMed Central]
- Andreicuț, A.D.; Fischer-Fodor, E.; Pârvu, A.E.; Ţigu, A.B.; Cenariu, M.; Pârvu, M.; Cătoi, F.A.; Irimie, A. Antitumoral and Immunomodulatory Effect of Mahonia aquifolium Extracts. Oxid. Med. Cell Longev. 2019, 2019, 6439021. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bharani, S.E.R.; Asad, M.; Dhamanigi, S.S.; Chandrakala, G.K. Immunomodulatory activity of methanolic extract of Morus alba linn. (mulberry) leaves. Pak. J. Pharm. Sci. 2010, 23, 63–68. [Google Scholar]
- Grajek, K.; Wawro, A.; Kokocha, D. Bioactivity of Morus alba L. Extracts—An Overview. Int. J. Pharm. Sci. Res. 2015, 6, 3110–3122. [Google Scholar]
- Raudone, L.; Vilkickyte, G.; Pitkauskaite, L.; Raudonis, R.; Vainoriene, R.; Motiekaityte, V. Antioxidant Activities of Vaccinium vitis-idaea L. Leaves within Cultivars and Their Phenolic Compounds. Molecules 2019, 24, 844. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sánchez, M.; Ureña-Vacas, I.; González-Burgos, E.; Kumar, P.D.; Gómez-Serranillos, M.P. The Genus Cetraria s. str.—A Review of Its Botany, Phytochemistry, Traditional Uses and Pharmacology. Molecules 2022, 27, 4990. [Google Scholar] [CrossRef] [PubMed]
- Dobros, N.; Zawada, K.; Paradowska, K. Phytochemical Profile and Antioxidant Activity of Lavandula angustifolia and Lavandula x intermedia Cultivars Extracted with Different Methods. Antioxidants 2022, 11, 711. [Google Scholar] [CrossRef] [PubMed]
- Takaoka, M. Of the phenolic substrate of hellebore (Veratrum grandiflorum Loes. fil.). J. Fac. Sci. Hokkaido Imp. Univ. 1940, 3, 1–16. [Google Scholar]
- Rauf, A.; Imran, M.; Har, S.; Ahmad, B.; Peters, D.G.; Mubarak, M.S. A comprehensive review of the health perspectives of resveratrol. Food Funct. 2017, 8, 4284–4305. [Google Scholar] [CrossRef]
- Alvarez, M.V.; Moreira, M.R.; Ponce, A. Antiquorum sensing and antimicrobial activity of natural agents with potential use in food. J. Food Saf. 2012, 32, 379–387. [Google Scholar] [CrossRef]
- Makwana, S.M. Study of Antibacterial Property of Plant Based Phenolic Compounds and Food Contact Materials Coated with Functionalized Nanoparticles. Master’s Thesis, Southern Illinois University, Carbondale, IL, USA, 2013. [Google Scholar]
- Abuamero, K.K.; Kondkar, A.A.; Chalam, K.V. Resveratrol and ophthalmic diseases. Nutrients 2016, 8, 200. [Google Scholar] [CrossRef]
- Oliveira, A.R.; Domingues, F.C.; Ferreira, S. The influence of resveratrol adaptation on resistance to antibiotics, benzalkonium chloride, heat and acid stresses of Staphylococcus aureus and Listeria monocytogenes. Food Control 2017, 73 Pt B, 1420–1425. [Google Scholar] [CrossRef]
- Seukep, J.A.; Sandjo, L.P.; Ngadjui, B.T.; Kuete, V. Antibacterial and antibiotic-resistance modifying activity of the extracts and compounds from Nauclea pobeguinii against gram-negative multi-drug resistant phenotypes. BMC Complement. Altern. Med. 2016, 16, 193. [Google Scholar] [CrossRef]
- Szkudelska, K.; Szkudelski, T. Resveratrol, obesity and diabetes. Eur. J. Pharmacol. 2010, 635, 1–8. [Google Scholar] [CrossRef]
- Vanamala, J.; Reddivari, L.; Radhakrishnan, S.; Tarver, C. Resveratrol suppresses IGF-1 induced human colon cancer cell proliferation and elevates apoptosis via suppression of IGF-1R/Wnt and activation of p53 signaling pathways. BMC Cancer 2010, 10, 238. [Google Scholar] [CrossRef]
- Anya, A.; Malka, B.S.; Kramer, M.Y.; Schwartz, N.S.; Holz, M.K. The combination of rapamycin and resveratrol blocks autophagy and induces apoptosis in breast cancer cells. J. Cell. Biochem. 2015, 116, 450–457. [Google Scholar]
- Meza-Torres, C.; Hernández-Camacho, J.D.; Cortés-Rodríguez, A.B.; Fang, L.; Thanh, T.B.; Rodríguez-Bies, E.; Navas, P.; López-Lluch, G. Resveratrol regulates the expression of genes involved in CoQ synthesis in liver in mice fed with high fat diet. Antioxidants 2020, 9, 431. [Google Scholar] [CrossRef] [PubMed]
- Rotondo, S.; Rajtar, G.; Manarini, S.; Celardo, A.; Rotillo, D.; Gaetano, G.; Evangelista, V.; Cerletti, C. Effect of trans-resveratrol, a natural polyphenolic compound, on human polymorphonuclear leukocyte function. Br. J. Pharmacol. 2010, 123, 1691–1699. [Google Scholar] [CrossRef]
- Gao, X.; Xu, Y.X.; Janakiraman, N.; Chapman, R.A.; Gautam, S.C. Immunomodulatory activity of resveratrol: Suppression of lymphocyte proliferation, development of cell-mediated cytotoxicity, and cytokine production. Biochem. Pharmacol. 2001, 62, 1299–1308. [Google Scholar] [CrossRef] [PubMed]
- Holmes-McNary, M.; Baldwin, A.S. Chemopreventive properties of trans-resveratrol are associated with inhibition of activation of the IkappaB kinase. Cancer Res. 2000, 60, 3477–3483. [Google Scholar]
- Manna, S.K.; Mukhopadhyay, A.; Aggarwal, B.B. Resveratrol suppresses TNF-induced activation of nuclear transcription factors NF-kappa B, activator protein-1, and apoptosis: Potential role of reactive oxygen intermediates and lipid peroxidation. J. Immunol. 2000, 164, 6509–6519. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.M.; Oliveira, M.I.; Sette, L.; Almeida, C.R.; Oliveira, M.J.; Barbosa, M.A.; Santos, S.G. Resveratrol as a natural anti-tumor necrosis factor-α molecule: Implications to dendritic cells and their crosstalk with mesenchymal stromal cells. PLoS ONE 2014, 9, e91406. [Google Scholar] [CrossRef]
- Donnelly, L.E.; Newton, R.; Kennedy, G.E.; Fenwick, P.S.; Leung, R.H.; Ito, K.; Russell, R.E.K.; Barnes, P.J. Anti-inflammatory effects of resveratrol in lung epithelial cells: Molecular mechanisms. Am. J. Physiol. Lung Cell Mol. Physiol. 2004, 287, L774–L783. [Google Scholar] [CrossRef]
- Eo, S.H.; Kim, S.J. Resveratrol-mediated inhibition of cyclooxygenase-2 in melanocytes suppresses melanogenesis through extracellular signal-regulated kinase 1/2 and phosphoinositide 3-kinase/Akt signalling. Eur. J. Pharmacol. 2019, 860, 172586. [Google Scholar] [CrossRef]
- Kowalski, J.; Samojedny, A.; Paul, M.; Pietsz, G.; Wilczok, T. Effect of apigenin, kaempferol and resveratrol on the expression of interleukin-1beta and tumor necrosis factor-alpha genes in J774.2 macrophages. Pharmacol. Rep. 2005, 57, 390–394. [Google Scholar]
- Ma, C.; Wang, Y.; Shen, A.; Cai, W. Resveratrol upregulates SOCS1 production by lipopolysaccharide-stimulated RAW264.7 macrophages by inhibiting miR-155. Int. J. Mol. Med. 2017, 39, 231–237. [Google Scholar] [CrossRef]
- Wung, B.S.; Hsu, M.C.; Wu, C.C.; Hsieh, C.W. Resveratrol suppresses IL-6-induced ICAM-1 gene expression in endothelial cells: Effects on the inhibition of STAT3 phosphorylation. Life Sci. 2005, 78, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.X.; Li, C.X.; Kakar, M.U.; Khan, M.S.; Wu, P.F.; Amir, R.M.; Dai, D.F.; Naveed, M.; Li, Q.Y.; Saeed, M.; et al. Resveratrol (RV): A pharmacological review and call for further research. Biomed. Pharmacother. 2021, 143, 112164. [Google Scholar] [CrossRef] [PubMed]
- Tomé-Carneiro, J.; Larrosa, M.; González-Sarrías, A.; Tomás-Barberán, F.A.; García-Conesa, M.T.; Espín, J.C. Resveratrol and clinical trials: The crossroad from in vitro studies to human evidence. Curr. Pharm. Des. 2013, 19, 6064–6093. [Google Scholar] [CrossRef] [PubMed]
- Jang, M.; Cai, L.; Udeani, G.O.; Slowing, K.V.; Thomas, C.F.; Beecher, C.W.; Fong, H.H.S.; Farnsworth, N.R.; Kinghorn, A.D.; Mehta, R.G.; et al. Cancer chemopreventive activity of resveratrol a natural product derived from grapes. Science 1997, 275, 218–220. [Google Scholar] [CrossRef]
- Zhang, F.; Shi, J.S.; Zhou, H.; Wilson, B.; Zhang, F.; Shi, J.S.; Zhou, H.; Wilson, B.; Hong, J.S.; Gao, H.M.; et al. Resveratrol protects dopamine neurons against lipopolysaccharide-induced neurotoxicity through its anti-inflammatory actions. Mol. Pharmacol. 2010, 78, 466–477. [Google Scholar] [CrossRef]
- Xia, N.; Daiber, A.; Habermeier, A.; Closs, E.I.; Thum, T.; Spanier, G.; Lu, Q.; Oelze, M.; Torzewski, M.; Lackner, K.J.; et al. Resveratrol reverses endothelial nitric-oxide synthase uncoupling in apolipoprotein E knockout mice. J. Pharmacol. Exp. Ther. 2010, 335, 149–154. [Google Scholar] [CrossRef]
- Ungvari, Z.; Labinskyy, N.; Mukhopadhyay, P.; Pinto, J.T.; Bagi, Z.; Ballabh, P.; Zhang, C.; Pacher, P.; Csiszar, A. Resveratrol attenuates mitochondrial oxidative stress in coronary arterial endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2009, 297, H1876–H1881. [Google Scholar] [CrossRef]
- Kaga, S.; Zhan, L.; Matsumoto, M.; Maulik, N. Resveratrol enhances neovascularization in the infarcted rat myocardium through the induction of thioredoxin-1 heme oxygenase-1 and vascular endothelial growth factor. J. Mol. Cell Cardiol. 2005, 39, 813–822. [Google Scholar] [CrossRef]
- Ziegler, C.C.; Rainwater, L.; Whelan, J.; McEntee, M.F. Dietary resveratrol does not affect intestinal tumorigenesis in Apc (Min/+) mice. J. Nutr. 2004, 134, 5–10. [Google Scholar] [CrossRef]
- Zunino, S.J.; Storms, D.H.; Newman, J.W.; Pedersen, T.L.; Keen, C.L.; Ducore, J.M. Resveratrol given intraperitoneally does not inhibit the growth of high-risk t (4.1) acute lymphoblastic leukemia cells in a NOD/SCID mouse model. Int. J. Oncol. 2012, 40, 1277–1284. [Google Scholar] [PubMed]
- Stakleff, K.S.; Sloan, T.; Blanco, D.; Marcanthony, S.; Booth, T.D.; Bishayee, A. Resveratrol exerts differential effects in vitro and in vivo against ovarian cancer cells. Asian Pac. J. Cancer Prev. 2012, 13, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.P.; Huang, S.S.; Deng, J.Y.; Chang, C.C.; Day, Y.J.; Hung, L.M. Insulin and resveratrol act synergistically preventing cardiac dysfunction in diabetes, but the advantage of resveratrol in diabetics with acute heart attack is antagonized by insulin. Free Radic. Biol. Med. 2010, 49, 1710–1721. [Google Scholar] [CrossRef] [PubMed]
- Azorín-Ortuño, M.; Yañéz-Gascón, M.J.; Pallarés, F.J.; Rivera, J.; González-Sarrías, A.; Larrosa, M.; Vallejo, F.; García-Conesa, M.T.; Tomás-Barberán, F.; Espín, J.C. A dietary resveratrol-rich grape extract prevents the developing of atherosclerotic lesions in the aorta of pigs fed an atherogenic diet. J. Agric. Food Chem. 2012, 60, 5609–5620. [Google Scholar] [CrossRef]
- Akar, F.; Uludağ, O.; Aydın, A.; Aytekin, Y.A.; Elbeg, S.; Tuzcu, M.; Sahin, K. High-fructose corn syrup causes vascular dysfunction associated with metabolic disturbance in rats protective effect of resveratrol. Food Chem. Toxicol. 2012, 50, 2135–2141. [Google Scholar] [CrossRef]
- Kumar, A.; Naidu, P.S.; Seghal, N.; Padi, S.S. Neuroprotective effects of resveratrol against intracerebroventricular colchicine-induced cognitive impairment and oxidative stress in rats. Pharmacology 2007, 79, 17–26. [Google Scholar] [CrossRef]
- Mudo, G.; Mäkelä, J.; Liberto, V.D.; Tselykh, T.V.; Olivieri, M.; Piepponen, P.; Eriksson, O.; Mälkiä, A.; Bonomo, A.; Kairisalo, M.; et al. Transgenic expression and activation of PGC-1α protect dopaminergic neurons in the MPTP mouse model of Parkinson’s disease. Cell Mol. Life Sci. 2012, 7, 1153–1165. [Google Scholar] [CrossRef]
- Singh, A.P.; Singh, R.; Verma, S.S.; Rai, V.; Kaschula, C.H.; Maiti, P.; Gupta, S.C. Health benefits of resveratrol: Evidence from clinical studies. Med. Res. Rev. 2019, 39, 1851–1891. [Google Scholar] [CrossRef]
- Schraufstatter, E.; Bernt, H. Antibacterial action of curcumin and related compounds. Nature 1949, 164, 456. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Sung, B. Pharmacological basis for the role of curcumin in chronic diseases: An age-old spice with modern targets. Trends Pharmacol. Sci. 2009, 30, 85–94. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Yuan, W.; Li, S.; Gupta, S.C. Curcumin-free turmeric exhibits anti-inflammatory and anticancer activities: Identification of novel components of turmeric. Mol. Nutr. Food Res. 2013, 57, 1529–1542. [Google Scholar] [CrossRef] [PubMed]
- Girisa, S.; Kumar, A.; Rana, V.; Parama, D.; Daimary, U.D.; Warnakulasuriya, S.; Kunnumakkara, A.B. From simple mouth cavities to complex oral mucosal disorders-curcuminoids as a promising therapeutic approach. ACS Pharmacol. Transl. Sci. 2021, 4, 647–665. [Google Scholar] [CrossRef]
- Shabnam, B.; Harsha, C.; Thakur, K.K.; Khatoon, E.; Kunnumakkara, A.B. Curcumin: A potential molecule for the prevention and treatment of inflammatory diseases. In The Chemistry and Bioactive Components of Turmeric; The Royal Society of Chemistry: London, UK, 2021; Chapter 7; pp. 150–171. [Google Scholar]
- Sivani, B.M.; Azzeh, M.; Patnaik, R.; Pantea Stoian, A.; Rizzo, A.M.; Banerjee, Y. Reconnoitering the Therapeutic Role of Curcumin in Disease Prevention and Treatment: Lessons Learned and Future Directions. Metabolites 2022, 12, 639. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Zhuang, Z.; Lu, Y.; Tao, T.; Zhou, Y.; Liu, G.; Wang, H.; Zhang, D.; Wu, L.; Dai, H. Curcumin mitigates neuro-inflammation by modulating microglia polarization through inhibiting TLR4 axis signaling pathway following experimental subarachnoid hemorrhage. Front. Neurosci. 2019, 13, 1223. [Google Scholar] [CrossRef] [PubMed]
- Dhandapani, K.M.; Mahesh, V.B.; Brann, D.W. Curcumin suppresses growth and chemoresistance of human glioblastoma cells via AP-1 and NFkappaB transcription factors. J. Neurochem. 2007, 102, 522–538. [Google Scholar] [CrossRef]
- Zhang, J.; Zheng, Y.; Luo, Y.; Du, Y.; Zhang, X.; Fu, J. Curcumin inhibits LPS-induced neuroinflammation by promoting microglial M2 polarization via TREM2/TLR4/NF-B pathways in BV2 cells. Mol. Immunol. 2019, 116, 29–37. [Google Scholar] [CrossRef]
- Wang, Q.; Ye, C.; Sun, S.; Li, R.; Shi, X.; Wang, S.; Zeng, X.; Kuang, N.; Liu, Y.; Shi, Q. Curcumin attenuates collagen-induced rat arthritis via anti-inflammatory and apoptotic effects. Int. Immunopharmacol. 2019, 72, 292–300. [Google Scholar] [CrossRef]
- Murakami, Y.; Kawata, A.; Fujisawa, S. Expression of cyclooxygenase-2, nitric oxide synthase 2 and heme oxygenase-1 mRNA induced by bis-eugenol in RAW264. 7 cells and their antioxidant activity determined using the induction period method. In Vivo 2017, 31, 819–831. [Google Scholar]
- Bhaumik, S.; Jyothi, M.D.; Khar, A. Differential modulation of nitric oxide production by curcumin in host macrophages and NK cells. FEBS Lett. 2000, 483, 78–82. [Google Scholar] [CrossRef]
- Surh, Y.J.; Chun, K.S.; Cha, H.H.; Han, S.S.; Keum, Y.S.; Park, K.K.; Lee, S.S. Molecular mechanisms underlying chemopreventive activities of anti-inflammatory phytochemicals: Down-regulation of COX-2 and iNOS through suppression of NF-κB activation. Mutat. Res. 2001, 481, 243–268. [Google Scholar] [CrossRef]
- Sadeghi, A.; Rostamirad, A.; Seyyedebrahimi, S.; Meshkani, R. Curcumin ameliorates palmitate-induced inflammation in skeletal muscle cells by regulating JNK/NF-kB pathway and ROS production. Inflammopharmacology 2018, 26, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Garufi, A.; Giorno, E.; Gilardini Montani, M.S.; Pistritto, G.; Crispini, A.; Cirone, M.; D’Orazi, G. p62/SQSTM1/Keap1/NRF2 axis reduces cancer cells death-sensitivity in response to Zn (II)–curcumin complex. Biomolecules 2021, 11, 348. [Google Scholar] [CrossRef] [PubMed]
- Mou, Y.; Wen, S.; Li, Y.X.; Gao, X.X.; Zhang, X.; Jiang, Z.Y. Recent progress in Keap1-Nrf2 protein-protein interaction inhibitors. Eur. J. Med. Chem. 2020, 202, 112532. [Google Scholar] [CrossRef] [PubMed]
- Yan, D.; He, B.; Guo, J.; Li, S.; Wang, J. Involvement of TLR4 in the protective effect of intra-articular administration of curcumin on rat experimental osteoarthritis. Acta Cir. Bras. 2019, 34, e201900604. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Liu, W.; Zhang, H.; Li, H.; Liu, J.; Zhang, F.; Jiang, T.; Jiang, S. Curcumin Prevents Osteoarthritis by Inhibiting the Activation of Inflammasome NLRP3. J. Interf. Cytokine Res. 2017, 37, 449–455. [Google Scholar] [CrossRef]
- Zhang, Z.; Leong, D.J.; Xu, L.; He, Z.; Wang, A.; Navati, M.; Kim, S.J.; Hirsh, D.M.; Hardin, J.A.; Cobelli, N.J.; et al. Curcumin slows osteoarthritis progression and relieves osteoarthritis-associated pain symptoms in a post-traumatic osteoarthritis mouse model. Arthritis Res. Ther. 2016, 18, 128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Csaki, C.; Mobasheri, A.; Shakibaei, M. Synergistic chondroprotective effects of curcumin and resveratrol in human articular chondrocytes: Inhibition of IL-1β-induced NF-κB-mediated inflammation and apoptosis. Arthritis Res. Ther. 2009, 11, R165. [Google Scholar] [CrossRef]
- Yabas, M.; Orhan, C.; Er, B.; Tuzcu, M.; Durmus, A.S.; Ozercan, I.H.; Sahin, N.; Bhanuse, P.; Morde, A.A.; Padigaru, M.; et al. A Next Generation Formulation of Curcumin Ameliorates Experimentally Induced Osteoarthritis in Rats via Regulation of Inflammatory Mediators. Front. Immunol. 2021, 12, 609629. [Google Scholar] [CrossRef]
- Paultre, K.; Cade, W.; Hernandez, D.; Reynolds, J.; Greif, D.; Best, T.M. Therapeutic effects of turmeric or curcumin extract on pain and function for individuals with knee osteoarthritis: A systematic review. BMJ Open Sport. Exerc. Med. 2021, 7, e000935. [Google Scholar] [CrossRef]
- Panda, S.K.; Nirvanashetty, S.; Parachur, V.A.; Mohanty, N.; Swain, T. A Randomized, Double Blind, Placebo Controlled, Parallel-Group Study to Evaluate the Safety and Efficacy of Curene® versus Placebo in Reducing Symptoms of Knee OA. Biomed. Res. Int. 2018, 2018, 5291945. [Google Scholar] [CrossRef]
- Nakagawa, Y.; Mukai, S.; Yamada, S.; Matsuoka, M.; Tarumi, E.; Hashimoto, T.; Tamura, C.; Imaizumi, A.; Nishihira, J.; Nakamura, T. Short-term effects of highly-bioavailable curcumin for treating knee osteoarthritis: A randomized, double-blind, placebo-controlled prospective study. J. Orthop. Sci. 2014, 19, 933–939. [Google Scholar] [CrossRef] [PubMed]
- Shep, D.; Khanwelkar, C.; Gade, P.; Karad, S. Efficacy and safety of combination of curcuminoid complex and diclofenac versus diclofenac in knee osteoarthritis: A randomized trial. Medicine 2020, 99, e19723. [Google Scholar] [CrossRef] [PubMed]
- Lev-Ari, S.; Strier, L.; Kazanov, D.; Elkayam, O.; Lichtenberg, D.; Caspi, D.; Arber, N. Curcumin synergistically potentiates the growth-inhibitory and pro-apoptotic effects of celecoxib in osteoarthritis synovial adherent cells. Rheumatology 2006, 45, 171–177. [Google Scholar] [CrossRef]
- Henrotin, Y.; Gharbi, M.; Dierckxsens, Y.; Priem, F.; Marty, M.; Seidel, L.; Albert, A.; Heuse, E.; Bonnet, V.; Castermans, C. Decrease of a specific biomarker of collagen degradation in osteoarthritis, Coll2-1, by treatment with highly bioavailable curcumin during an exploratory clinical trial. BMC Complement. Altern. Med. 2014, 14, 159. [Google Scholar] [CrossRef] [PubMed]
- Middleton, E.; Kandaswami, C.; Theoharides, T.C. The effects of plant flavonoids on mammalian cells: Implications for inflammation, heart disease, and cancer. Pharmacol. Rev. 2000, 52, 673–751. [Google Scholar] [PubMed]
- Ito, T.; Warnken, S.P.; May, W.S. Protein synthesis inhibition by flavonoids: Roles of eukaryotic initiation factor 2alpha kinases. Biochem. Biophys. Res. Commun. 1999, 265, 589–594. [Google Scholar] [CrossRef]
- Ruiz, P.A.; Braune, A.; Hölzlwimmer, G.; Quintanilla-Fend, L.; Haller, D. Quercetin inhibits TNF-induced NF-kappaB transcription factor recruitment to proinflammatory gene promoters in murine intestinal epithelial cells. J. Nutr. 2007, 137, 1208–1215. [Google Scholar] [CrossRef]
- Boots, A.W.; Haenen, G.R.; Bast, A. Health effects of quercetin: From antioxidant to nutraceutical. Eur. J. Pharmacol. 2008, 585, 325–337. [Google Scholar] [CrossRef]
- Min, Z.; Yangchun, L.; Yuquan, W.; Changying, Z. Quercetin inhibition of myocardial fibrosis through regulating MAPK signaling pathway via ROS. Pak. J. Pharm. Sci. 2019, 32 (Suppl. S3), 1355–1359. [Google Scholar]
- Hämäläinen, M.; Nieminen, R.; Vuorela, P.; Heinonen, M.; Moilanen, E. Anti-inflammatory effects of flavonoids: Genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-kappaB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-kappaB activation along with their inhibitory effect on iNOS expression and NO production in activated macrophages. Mediators Inflamm. 2007, 2007, 45673. [Google Scholar]
- Kobuchi, H.; Roy, S.; Sen, C.K.; Nguyen, H.G.; Packer, L. Quercetin inhibits inducible ICAM-1 expression in human endothelial cells through the JNK pathway. Am. J. Physiol. 1999, 277, C403–C411. [Google Scholar] [CrossRef] [PubMed]
- Ying, B.; Yang, T.; Song, X.; Hu, X.; Fan, H.; Lu, X.; Chen, L.; Cheng, D.; Wang, T.; Liu, D.; et al. Quercetin inhibits IL-1 beta-induced ICAM-1 expression in pulmonary epithelial cell line A549 through the MAPK pathways. Mol. Biol. Rep. 2009, 36, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Morikawa, K.; Nonaka, M.; Narahara, M.; Torii, I.; Kawaguchi, K.; Yoshikawa, T.; Kumazawa, Y.; Morikawa, S. Inhibitory effect of quercetin on carrageenan-induced inflammation in rats. Life Sci. 2003, 74, 709–721. [Google Scholar] [CrossRef] [PubMed]
- Rogerio, A.P.; Dora, C.L.; Andrade, E.L.; Chaves, J.S.; Silva, L.F.; Lemos-Senna, E.; Calixto, J.B. Anti-inflammatory effect of quercetin-loaded microemulsion in the airways allergic inflammatory model in mice. Pharmacol. Res. 2010, 61, 288–297. [Google Scholar] [CrossRef]
- Bungsu, I.; Kifli, N.; Ahmad, S.R.; Ghani, H.; Cunningham, A.C. Herbal Plants: The Role of AhR in Mediating Immunomodulation. Front. Immunol. 2021, 12, 697663. [Google Scholar] [CrossRef]
- Yu, W.; Zhu, Y.; Li, H.; He, Y. Injectable Quercetin-Loaded Hydrogel with Cartilage-Protection and Immunomodulatory Properties for Articular Cartilage Repair. ACS Appl. Bio Mater. 2020, 3, 761–771. [Google Scholar] [CrossRef]
- Hu, Y.; Gui, Z.; Zhou, Y.; Xia, L.; Lin, K.; Xu, Y. Quercetin alleviates rat osteoarthritis by inhibiting inflammation and apoptosis of chondrocytes, modulating synovial macrophages polarization to M2 macrophages. Free Radic. Biol. Med. 2019, 145, 146–160. [Google Scholar] [CrossRef]
- Karimi, A.; Naeini, F.; Asghari Azar, V.; Hasanzadeh, M.; Ostadrahimi, A.; Niazkar, H.R.; Mobasseri, M.; Tutunchi, H. A comprehensive systematic review of the therapeutic effects and mechanisms of action of quercetin in sepsis. Phytomedicine 2021, 86, 153567. [Google Scholar] [CrossRef]
- Rifaai, R.A.; El-Tahawy, N.F.; Ali, S.E. Effect of quercetin on the endocrine pancreas of the experimentally induced diabetes in male albino rats: A histological and immunohistochemical study. J. Diabetes Metab. 2012, 3, 3. [Google Scholar] [CrossRef]
- Eitah, H.E.; Maklad, Y.A.; Abdelkader, N.F.; El Din, A.A.G.; Badawi, M.A.; Kenawy, S.A. Modulating impacts of quercetin/sitagliptin combination on streptozotocin-induced diabetes mellitus in rats. Toxicol. Appl. Pharmacol. 2019, 365, 30–40. [Google Scholar] [CrossRef]
- Yi, H.; Peng, H.; Wu, X.; Xu, X.; Kuang, T.; Zhang, J.; Du, L.; Fan, G. The Therapeutic Effects and Mechanisms of Quercetin on Metabolic Diseases: Pharmacological Data and Clinical Evidence. Oxid. Med. Cell Longev. 2021, 2021, 6678662. [Google Scholar] [CrossRef]
- Bonezzi, C.; Costantini, A.; Cruccu, G.; Fornasari, D.M.; Guardamagna, V.; Palmieri, V.; Polati, E.; Zini, P.; Dickenson, A.H. Capsaicin 8% dermal patch in clinical practice: An expert opinion. Expert. Opin. Pharmacother. 2020, 21, 1377–1387. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Zheng, J. Understand spiciness: Mechanism of TRPV1 channel activation by capsaicin. Protein Cell 2017, 8, 169–177. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J.; Brock, C.; Olesen, A.E.; Andresen, T.; Nilsson, M.; Dickenson, A.H. Unravelling the mystery of capsaicin: A tool to understand and treat pain. Pharmacol. Rev. 2012, 64, 939–971. [Google Scholar] [CrossRef] [PubMed]
- Haanpää, M.; Treede, R.D. Capsaicin for neuropathic pain: Linking traditional medicine and molecular biology. Eur. Neurol. 2012, 68, 264–275. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Salvador, L.; Andrés-Borderia, A.; Ferrer-Montiel, A.; Planells-Cases, R. Agonist- and Ca2+-dependent desensitization of TRPV1 channel targets the receptor to lysosomes for degradation. J. Biol. Chem. 2012, 287, 19462–19471. [Google Scholar] [CrossRef]
- Kim, C.S.; Kawada, T.; Kim, B.S.; Han, I.S.; Choe, S.Y.; Kurata, T.; Yu, R. Capsaicin exhibits anti-inflammatory property by inhibiting IkB-a degradation in LPS-stimulated peritoneal macrophages. Cell Signal 2003, 15, 299–306. [Google Scholar] [CrossRef]
- Li, T.; Wang, G.; Hui, V.C.C.; Saad, D.; de Sousa Valente, J.; La Montanara, P.; Nagy, I. TRPV1 feed-forward sensitisation depends on COX2 upregulation in primary sensory neurons. Sci. Rep. 2021, 11, 3514. [Google Scholar] [CrossRef]
- Fischer, B.S.; Qin, D.; Kim, K.; McDonald, T.V. Capsaicin inhibits Jurkat T-cell activation by blocking calcium entry current I(CRAC). J. Pharmacol. Exp. Ther. 2001, 299, 238–246. [Google Scholar]
- Zhang, J.; Nagasaki, M.; Tanaka, Y.; Morikawa, S. Capsaicin inhibits growth of adult T-cell leukemia cells. Leuk. Res. 2003, 27, 275–283. [Google Scholar] [CrossRef]
- Nevius, E.; Srivastava, P.K.; Basu, S. Oral ingestion of Capsaicin, the pungent component of chili pepper, enhances a discreet population of macrophages and confers protection from autoimmune diabetes. Mucosal. Immunol. 2012, 5, 76–86. [Google Scholar] [CrossRef]
- Viveros-Paredes, J.M.; Puebla-Pérez, A.M.; Gutiérrez-Coronado, O.; Macías-Lamas, A.M.; Hernández-Flores, G.; Ortiz-Lazareno, P.C.; Bravo-Cuéllar, A.; Villaseñor-García, M.M. Capsaicin attenuates immunosuppression induced by chronic stress in BALB/C mice. Int. Immunopharmacol. 2021, 93, 107341. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.N.; Shankar, S.; Srivastava, R.K. Green tea catechin, epigallocatechin-3-gallate (EGCG): Mechanisms, perspectives and clinical applications. Biochem. Pharmacol. 2011, 82, 1807–1821. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Landis-Piwowar, K.; Chan, T.H.; Dou, Q.P. Green tea polyphenols as proteasome inhibitors: Implication in chemoprevention. Curr. Cancer Drug Targets 2011, 11, 296–306. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Tang, J.; Du, Y.; Ding, J.; Liu, J.Y. The green tea polyphenol EGCG potentiates the antiproliferative activity of sunitinib in human cancer cells. Tumour Biol. 2016, 37, 8555–8566. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.H.; Hsieh, C.H.; Tsai, S.Y.; Wang, C.Y.; Wang, C.C. Anticancer effects of epigallocatechin-3-gallate nanoemulsion on lung cancer cells through the activation of AMP-activated protein kinase signaling pathway. Sci. Rep. 2020, 10, 5163. [Google Scholar] [CrossRef]
- Muraoka, K.; Shimizu, K.; Sun, X.; Tani, T.; Izumi, R.; Miwa, K.; Yamamoto, K. Flavonoids exert diverse inhibitory effects on the activation of NF-kappaB. Transplant Proc. 2002, 34, 1335–1340. [Google Scholar] [CrossRef]
- Joo, S.Y.; Song, Y.A.; Park, Y.L.; Myung, E.; Chung, C.Y.; Park, K.J.; Cho, S.B.; Lee, W.S.; Kim, H.S.; Rew, J.S.; et al. Epigallocatechin-3-gallate Inhibits LPS-Induced NF-κB and MAPK Signaling Pathways in Bone Marrow-Derived Macrophages. Gut Liver 2012, 6, 188–196. [Google Scholar] [CrossRef]
- Chung, J.Y.; Park, J.O.; Phyu, H.; Dong, Z.; Yang, C.S. Mechanisms of inhibition of the Ras-MAP kinase signaling pathway in 30.7b Ras 12 cells by tea polyphenols (-)-epigallocatechin-3-gallate and theaflavin-3,3′-digallate. FASEB J. 2001, 15, 2022–2024. [Google Scholar] [CrossRef]
- Shih, L.J.; Lin, Y.R.; Lin, C.K.; Liu, H.S.; Kao, Y.H. Green tea (-)-epigallocatechin gallate induced growth inhibition of human placental choriocarcinoma cells. Placenta 2016, 41, 1–9. [Google Scholar] [CrossRef]
- Hara, Y.; Fujino, M.; Adachi, K.; Li, X.K. The reduction of hypoxia-induced and reoxygenation-induced apoptosis in rat islets by epigallocatechin gallate. Transpl. Proc. 2006, 38, 2722–2725. [Google Scholar] [CrossRef]
- Yu, H.N.; Ma, X.L.; Yang, J.G.; Shi, C.C.; Shen, S.R.; He, G.Q. Comparison of effects of epigallocatechin-3-gallate on hypoxia injury to human umbilical vein, RF/6A, and ECV304 cells induced by Na2S2O4. Endothelium 2007, 14, 227–231. [Google Scholar] [CrossRef]
- Gu, J.J.; Qiao, K.S.; Sun, P.; Chen, P.; Li, Q. Study of EGCG induced apoptosis in lung cancer cells by inhibiting PI3K/Akt signaling pathway. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 4557–4563. [Google Scholar] [PubMed]
- Aktas, O.; Prozorovski, T.; Smorodchenko, A.; Savaskan, N.E.; Lauster, R.; Kloetzel, P.M.; Infante-Duarte, C.; Brocke, S.; Zipp, F. Green tea epigallocatechin-3-gallate mediates T cellular NF-kappa B inhibition and exerts neuroprotection in autoimmune encephalomyelitis. J. Immunol. 2004, 173, 5794–5800. [Google Scholar] [CrossRef]
- Wang, J.; Ren, Z.; Xu, Y.; Xiao, S.; Meydani, S.N.; Wu, D. Epigallocatechin-3-gallate ameliorates experimental autoimmune encephalomyelitis by altering balance among CD4+ T-cell subsets. Am. J. Pathol. 2012, 180, 221–234. [Google Scholar] [CrossRef] [PubMed]
- Byun, J.K.; Yoon, B.Y.; Jhun, J.Y.; Oh, H.J.; Kim, E.K.; Min, J.K.; Cho, M.L. Epigallocatechin-3-gallate ameliorates both obesity and autoinflammatory arthritis aggravated by obesity by altering the balance among CD4+ T-cell subsets. Immunol. Lett. 2014, 157, 51–59. [Google Scholar] [CrossRef]
- Wong, C.P.; Nguyen, L.P.; Noh, S.K.; Bray, T.M.; Bruno, R.S.; Ho, E. Induction of regulatory T cells by green tea polyphenol EGCG. Immunol. Lett. 2011, 139, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Sadava, D.; Whitlock, E.; Kane, S.E. The green tea polyphenol, epigallocatechin-3-gallate inhibits telomerase and induces apoptosis in drug-resistant lung cancer cells. Biochem. Biophys. Res. Commun. 2007, 360, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Bandele, O.J.; Osheroff, N. (-)-Epigallocatechin gallate, a major constituent of green tea, poisons human type II topoisomerases. Chem. Res. Toxicol. 2008, 21, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Shim, J.Y.; Zhu, B.T. Mechanisms for the inhibition of DNA methyltransferases by tea catechins and bioflavonoids. Mol. Pharmacol. 2005, 68, 1018–1030. [Google Scholar] [CrossRef]
- Cai, Y.; Kurita-Ochiai, T.; Hashizume, T.; Yamamoto, M. Green tea epigallocatechin-3-gallate attenuates Porphyromonas gingivalis-induced atherosclerosis. Pathog. Dis. 2013, 67, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Huang, A.C.; Cheng, H.Y.; Lin, T.S.; Chen, W.H.; Lin, J.H.; Lin, J.J.; Lu, C.C.; Chiang, J.H.; Hsu, S.C.; Wu, P.; et al. Epigallocatechin gallate (EGCG), influences a murine WEHI-3 leukemia model in vivo through enhancing phagocytosis of macrophages and populations of T- and B-cells. In Vivo 2013, 27, 627–634. [Google Scholar]
- Farooqi, A.A.; Attar, R.; Sabitaliyevich, U.Y.; Alaaeddine, N.; de Sousa, D.P.; Xu, B.; Cho, W.C. The Prowess of Andrographolide as a Natural Weapon in the War against Cancer. Cancers 2020, 12, 2159. [Google Scholar] [CrossRef]
- Maiti, K.; Gantait, A.; Mukherjee, K.; Saha, B.; Mukherjee, P.K. Therapeutic potentials of Andrographolide from Andrographis paniculata: A review. J. Nat. Remed. 2006, 6, 1–13. [Google Scholar]
- Qin, L.H.; Kong, L.; Shi, G.J.; Wang, Z.T.; Ge, B.X. Andrographolide inhibits the production of TNF-alpha and interleukin-12 in lipopolysaccharide-stimulated macrophages: Role of mitogen-activated protein kinases. Biol. Pharm. Bull. 2006, 29, 220–224. [Google Scholar] [CrossRef] [PubMed]
- Rajagopal, S.; Kumar, R.A.; Deevi, D.S.; Satyanarayana, C.; Rajagopalan, R. Andrographolide a potential cancer therapeutic agent isolated from Andrographis paniculate. J. Exp. Ther. Oncol. 2003, 3, 147–158. [Google Scholar] [CrossRef]
- Chiou, W.F.; Chen, C.F.; Lin, J.J. Mechanisms of suppression of inducible nitric oxide synthase (iNOS) expression in RAW 264.7 cells by andrographolide. Br. J. Pharmacol. 2000, 129, 1553–1560. [Google Scholar] [CrossRef]
- Lee, K.C.; Chang, H.H.; Chung, Y.H.; Lee, T.Y. Andrographolide acts as an anti-inflammatory agent in LPS-stimulated RAW2647 macrophages by inhibiting STAT3-mediated suppression of the NF-κB pathway. J. Ethnopharmacol. 2011, 135, 678–684. [Google Scholar] [CrossRef]
- Islam, M.T. Andrographolide, a New Hope in the Prevention and Treatment of Metabolic Syndrome. Front. Pharmacol. 2017, 8, 571. [Google Scholar] [CrossRef]
- Corbett, J.A.; Kwon, G.; Marino, M.H.; Rodi, C.P.; Sullivan, P.M.; Turk, J.; McDaniel, M.L. Tyrosine kinase inhibitors prevent cytokine-induced expression of iNOS and COX-2 by human islets. Am. J. Physiol. 1996, 270, C1581–C1587. [Google Scholar] [CrossRef]
- Mccabe, M.J.; Orrenius, S., Jr. Genistein induces apoptosis in immature human thymocytes by inhibiting, topoisomerase-II. Biochem. Biophys. Res. Commun. 1993, 194, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Si, H.; Liu, D. Phytochemical genistein in the regulation of vascular function: New insights. Curr. Med. Chem. 2007, 14, 2581–2589. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.W.; Lee, W.H. Protective effects of genistein on proinflammatory pathways in human brain microvascular endothelial cells. J. Nutr. Biochem. 2008, 19, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhang, Q.; Jin, S.; He, D.; Zhao, S.; Liu, S. Genistein modulate immune responses in collagen-induced rheumatoid arthritis model. Maturitas 2008, 59, 405–412. [Google Scholar] [CrossRef]
- Wang, X.; Chen, S.; Ma, G.; Ye, M.; Lu, G. Genistein protects dopaminergic neurons by inhibiting microglial activation. Neuroreport 2005, 16, 267–270. [Google Scholar] [CrossRef]
- Yalniz, M.; Bahcecioglu, I.H.; Kuzu, N.; Poyrazoglu, O.K.; Bulmus, O.; Celebi, S.; Ustundag, B.; Ozercan, I.H.; Sahin, K. Preventive role of genistein in an experimental non-alcoholic steatohepatitis model. J. Gastroenterol. Hepatol. 2007, 22, 2009–2014. [Google Scholar] [CrossRef]
- Seibel, J.; Molzberger, A.F.; Hertrampf, T.; Laudenbach-Leschowski, U.; Diel, P. Oral treatment with genistein reduces the expression of molecular biochemical markers of inflammation in a rat model of chronic TNBS-induced colitis. Eur. J. Nutr. 2009, 48, 213–220. [Google Scholar] [CrossRef]
- Bhattacharyya, B.; Panda, D.; Gupta, S.; Banerjee, M. Anti-mitotic activity of colchicine and the structural basis for its interaction with tubulin. Med. Res. Rev. 2008, 28, 155–183. [Google Scholar] [CrossRef]
- Stanton, R.A.; Gernert, K.M.; Nettles, J.H.; Aneja, R. Drugs that target dynamic microtubules: A new molecular perspective. Med. Res. Rev. 2011, 31, 443–481. [Google Scholar] [CrossRef]
- Imazio, M.; Bobbio, M.; Cecchi, E.; Demarie, D.; Demichelis, B.; Pomari, F.; Moratti, M.; Gaschino, G.; Giammaria, M.; Ghisio, A.; et al. Colchicine in addition to conventional therapy for acute pericarditis: Results of the COlchicine for acute PEricarditis (COPE) trial. Circulation 2005, 112, 2012–2016. [Google Scholar] [CrossRef]
- Imazio, M.; Brucato, A.; Cemin, R.; Ferrua, S.; Belli, R.; Maestroni, S.; Trinchero, R.; Spodick, D.H.; Adler, Y.; CORP (COlchicine for Recurrent Pericarditis) Investigators. Colchicine for recurrent pericarditis (CORP): A randomized trial. Ann. Intern. Med. 2011, 155, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Imazio, M.; Brucato, A.; Cemin, R.; Ferrua, S.; Maggiolini, S.; Beqaraj, F.; Demarie, D.; Forno, D.; Ferro, S.; Maestroni, S.; et al. A randomized trial of colchicine for acute pericarditis. N. Engl. J. Med. 2013, 369, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Deftereos, S.; Giannopoulos, G.; Kossyvakis, C.; Efremidis, M.; Panagopoulou, V.; Kaoukis, A.; Raisakis, K.; Bouras, G.; Angelidis, C.; Theodorakis, A.; et al. Colchicine for prevention of early atrial fibrillation recurrence after pulmonary vein isolation: A randomized controlled study. J. Am. Coll. Cardiol. 2012, 60, 1790–1796. [Google Scholar] [CrossRef] [PubMed]
- Perico, N.; Ostermann, D.; Bontempeill, M.; Morigi, M.; Amuchastegui, C.S.; Zoja, C.; Akalin, E.; Sayegh, M.H.; Remuzzi, G. Colchicine interferes with L-selectin and leukocyte function-associated antigen-1 expression on human T lymphocytes and inhibits T cell activation. J. Am. Soc. Nephrol. 1996, 7, 594–601. [Google Scholar] [CrossRef]
- Titus, R.G. Colchicine is a potent adjuvant for eliciting T cell responses. J. Immunol. 1991, 146, 4115–4119. [Google Scholar] [CrossRef]
- Weng, J.H.; Koch, P.D.; Luan, H.H.; Tu, H.C.; Shimada, K.; Ngan, I.; Ventura, R.; Jiang, R.; Mitchison, T.J. Colchicine acts selectively in the liver to induce hepatokines that inhibit myeloid cell activation. Nat. Metab. 2021, 3, 513–522. [Google Scholar] [CrossRef]
- Li, C.; Yang, C.W.; Ahn, H.J.; Kim, W.Y.; Park, C.W.; Park, J.H.; Lee, M.J.; Yang, J.H.; Kim, Y.S.; Bang, B.K. Colchicine decreases apoptotic cell death in chronic cyclosporine nephrotoxicity. J. Lab. Clin. Med. 2002, 139, 364–371. [Google Scholar] [CrossRef]
- Bozkurt, D.; Bicak, S.; Sipahi, S.; Taskin, H.; Hur, E.; Ertilav, M.; Sen, S.; Duman, S. The effects of colchicine on the progression and regression of encapsulating peritoneal sclerosis. Perit. Dial. Int. 2008, 28 (Suppl. S5), S53–S57. [Google Scholar] [CrossRef]
- Lee, F.Y.; Lu, H.I.; Zhen, Y.Y.; Leu, S.; Chen, Y.L.; Tsai, T.H.; Chung, S.Y.; Chua, S.; Sheu, J.J.; Hsu, S.Y.; et al. Benefit of combined therapy with nicorandil and colchicine in preventing monocrotaline-induced rat pulmonary arterial hypertension. Eur. J. Pharm. Sci. 2013, 50, 372–384. [Google Scholar] [CrossRef]
- Nuki, G. Colchicine: Its mechanism of action and efficacy in crystal-induced inflammation. Curr. Rheumatol. Rep. 2008, 10, 218–227. [Google Scholar] [CrossRef]
- Lin, W.C.; Lin, J.Y. Berberine down-regulates the Th1/Th2 cytokine gene expression ratio in mouse primary splenocytes in the absence or presence of lipopolysaccharide in a preventive manner. Int. Immunopharmacol. 2011, 11, 1984–1990. [Google Scholar] [CrossRef] [PubMed]
- Son, D.J.; Akiba, S.; Hong, J.T.; Yun, Y.P.; Hwang, S.Y.; Park, Y.H.; Lee, S.E. Piperine inhibits the activities of platelet cytosolic phospholipase A2 and thromboxane A2 synthase without affecting cyclooxygenase-1 activity: Different mechanisms of action are involved in the inhibition of platelet aggregation and macrophage inflammatory response. Nutrients 2014, 6, 3336–3352. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.; Nozawa, H.; Daikonnya, A.; Kondo, K.; Kitanaka, S. Inhibitors of nitric oxide production from hops (Humulus lupulus L.). Biol. Pharm. Bull. 2003, 26, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B.; Liu, Z.Y.; Li, Y.Y.; Luo, Y.; Liu, M.L.; Dong, H.Y.; Wang, Y.X.; Liu, Y.; Zhao, P.T.; Jin, F.G.; et al. Antiinflammatory effects of matrine in LPS-induced acute lung injury in mice. Eur. J. Pharm. Sci. 2011, 44, 573–579. [Google Scholar] [CrossRef]
- Chen, C.Y.; Peng, W.H.; Tsai, K.D.; Hsu, S.L. Luteolin suppresses inflammation-associated gene expression by blocking NF-κB and AP-1 activation pathways in mouse alveolar macrophages. Life Sci. 2007, 81, 1602–1614. [Google Scholar] [CrossRef]
- Kang, H.-K.; Ecklund, D.; Liu, M.; Datta, S.K. Apigenin, a non-mutagenic dietary flavonoid, suppresses lupus by inhibiting autoantigen presentation for expansion of autoreactive Th1 and Th17 cells. Arthritis Res. Ther. 2009, 11, R59. [Google Scholar] [CrossRef]
- Kang, S.R.; Park, K.I.; Park, H.S.; Lee, D.H.; Kim, J.A.; Nagappan, A.; Kim, E.H.; Lee, W.S.; Shin, S.C.; Park, M.K.; et al. Anti-inflammatory effect of flavonoids isolated from Korea Citrus aurantium L. on lipopolysaccharide-induced mouse macrophage RAW 264.7 cells by blocking of nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) signalling pathways. Food Chem. 2011, 129, 1721–1728. [Google Scholar] [CrossRef]
- Chandrashekar, N.; Selvamani, A.; Subramanian, R.; Pandi, A.; Thiruvengadam, D. Baicalein inhibits pulmonary carcinogenesis-associated inflammation and interferes with COX-2, MMP-2 and MMP-9 expressions in-vivo. Toxicol. Appl. Pharmacol. 2012, 261, 10–21. [Google Scholar] [CrossRef]
- Lee, W.; Ku, S.-K.; Bae, J.-S. Anti-inflammatory effects of Baicalin, Baicalein, and Wogonin in vitro and in vivo. Inflammation 2015, 38, 110–125. [Google Scholar] [CrossRef]
- Yoo, H.; Ku, S.-K.; Baek, Y.-D.; Bae, J.-S. Anti-inflammatory effects of rutin on HMGB1-induced inflammatory responses in vitro and in vivo. Inflam. Res. 2014, 63, 197–206. [Google Scholar] [CrossRef]
- Liu, X.; Mei, Z.; Qian, J.; Zeng, Y.; Wang, M. Puerarin partly counteracts the inflammatory response after cerebral ischemia/reperfusion via activating the cholinergic anti-inflammatory pathway. Neural Regen. Res. 2013, 8, 3203. [Google Scholar] [CrossRef] [PubMed]
- Vaillancourt, F.; Silva, P.; Shi, Q.; Fahmi, H.; Fernandes, J.C.; Benderdour, M. Elucidation of molecular mechanisms underlying the protective effects of thymoquinone against rheumatoid arthritis. J. Cell. Biochem. 2011, 112, 107–117. [Google Scholar] [CrossRef]
- Youn, J.; Lee, J.S.; Na, H.K.; Kundu, J.K.; Surh, Y.J. Resveratrol and piceatannol inhibit iNOS expression and NF-κB activation in dextran sulfate sodium-induced mouse colitis. Nutr. Cancer 2009, 61, 847–854. [Google Scholar] [CrossRef]
- Andújar, I.; Recio, M.C.; Bacelli, T.; Giner, R.M.; Rios, J.L. Shikonin reduces oedema induced by phorbol ester by interfering with IκBα degradation thus inhibiting translocation of NF-κB to the nucleus. Br. J. Pharmacol. 2010, 160, 376–388. [Google Scholar] [CrossRef] [PubMed]
- Brinker, A.M.; Ma, J.; Lipsky, P.E.; Raskin, I. Medicinal chemistry and pharmacology of genus Tripterygium (Celastraceae). Phytochemistry 2007, 68, 732–766. [Google Scholar] [CrossRef] [PubMed]
- Kannaiyan, R.; Shanmugam, M.K.; Sethi, G. Molecular targets of celastrol derived from Thunder of God Vine: Potential role in the treatment of inflammatory disorders and cancer. Cancer Lett. 2011, 303, 9–20. [Google Scholar] [CrossRef]
- Wu, C.J.; Wang, Y.H.; Lin, C.J.; Chen, H.H.; Chen, Y.J. Tetrandrine down-regulates ERK/NF-κB signaling and inhibits activation of mesangial cells. Toxicol. Vitr. 2011, 25, 1834–1840. [Google Scholar] [CrossRef]
- Kim, S.Y.; Moon, K.A.; Jo, H.Y.; Jeong, S.; Seon, S.H.; Jung, E.; Cho, Y.S.; Chun, E.; Lee, K.Y. Anti-inflammatory effects of apocynin, an inhibitor of NADPH oxidase, in airway inflammation. Immunol. Cell Biol. 2012, 90, 441–448. [Google Scholar] [CrossRef]
- Ammon, H.P. Boswellic acids in chronic inflammatory diseases. Planta Med. 2006, 72, 1100–1116. [Google Scholar] [CrossRef]
- Khanna, K.; Kohli, S.K.; Kaur, R.; Bhardwaj, A.; Bhardwaj, V.; Ohri, P.; Sharma, A.; Ahmad, A.; Bhardwaj, R.; Ahmad, P. Herbal immune-boosters: Substantial warriors of pandemic COVID-19 battle. Phytomedicine 2021, 85, 153361. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Botanical Name/Family | Source Countries | Part Used | Bioactive-Chemical Constituent | Biological Activity | Reference |
|---|---|---|---|---|---|
| Acacia catechu/Fabaceae | India, East Africa | leaves, bark | flavonoids (quercetin, catechin, epicatechin) | antioxidant, immunomodulatory, hypoglycemic | [17,41,59] |
| Achillea millefolium/Compositae | Northern Hemisphere | whole plant | Flavonoids, alkaloids, polyacetylenes, coumarins, triterpenes, lactones | anti-inflammatory, antispasmodic, antipyretic, diuretic | [60,61] |
| Andrographis paniculata/Acanthaceae | India, Sri Lanka | whole plant, leaves, stems, roots | diterpenoids (andrographolide), lactones, flavonoids, polysaccharides | immunomodulatory, hepatoprotective, antispasmodic, anticancer, anti-inflammatory, antiviral, antiproliferative, antiplatelet | [62,63] |
| Aronia melanocarpa/Rosaceae | North America | fruits, bark, leaves | flavonoids (procyanidins anthocyanins), catechins, phenolic acids, ascorbic acid | immunomodulatory, anti-inflammatory, antioxidant, gastroprotective, hepatoprotective, antiproliferative, cardiovascular-protective, antioxidants | [20,64,65] |
| Pelargonium sidoides/ Geraniaceae | South Africa | roots, shoot, leaves | coumarins, phenols | immunomodulatory, antibacterial | [41,66] |
| Zingiber officinale/Zingiberaceae (ginger) | Asia | roots, leaves | phenolic acid (eugenol, gingerols, shogaols, paradols) lactons, terpenes | immunostimulation, antimicrobial, antioxidant, analgesic, anti-inflammatory, anticancer, antihypertensive | [67,68] |
| Kalanchoe pinnata/Crassulaceae | Madagascar | leaves, flowers | flavonoid glycosides (quercitrin), bufadienolides, lectins, polyphenols | immunosuppressive, antifungal, antimicrobial, antiviral, wound healing (antiscar), anti-inflammatory | [69,70] |
| Camellia sinensis/Theaceae (green tea) | China, India, Nepal | leaves | catechins (epigallocatechin-3-gallate, epigallocatechin, epicatechin), triterpenoids, saponins | immunomodulatory, antioxidant, antiviral, anticancer, antifungal activities. | [20] |
| Cannabis sativa/Cannabaceae | Central Asia, widely cultivated around the world | leaves, seeds, inflorescence | cannabinoid (cannabidiol, cannabigerol, Δ9-tetrahydrocannabinol), terpenes, flavonoids | anti-inflammatory, immunosuppressive, neuroprotective, antioxidant | [71,72] |
| Capsicum species/Solanaceae | Central and South America | fruits | provitamin A, vitamins (E, C) carotenoids, phenolic compounds (capsaicinoids, luteolin, quercetin) | antioxidant, antimicrobial, antiseptic, anticancer, counterirritant, antioxidant, immunomodulator | [43] |
| Cyclopia genistoides/Fabaceae (Honeybush) | South Africa | flowers, leaves, stems | phenols, flavones, flavanones isoflavones, xanthones (mangiferin), coumestans, catechins (epigallocatechin-3-gallate), benzaldehyde derivates, phytoestrogens | immunomodulatory, anti-inflammatory, antioxidant, antiproliferative, anticancer, cytoprotective | [73,74] |
| Euphorbia hirta/Euphorbiaceae | India, Australia | herb, leaves, roots | flavanoid glycoside, phenolic acids, alkaloids | anticancer, antioxidant, antibacterial, antifungal, antimalarial, anti-inflammatory, antiasthmatic | [17,64] |
| Ginkgo biloba/Ginkgoaceae | China | leaves, seeds | flavonoids, terpenoids, alkylphenols, anthocyanidins, lignans, polyprenols polysaccharides, 4′-o-methylpyridoxine | immunomodulatory, antioxidant, anti-inflammatory, anticancer, antidiabetic, antilipidemic, antimicrobial, anti-lipid peroxidation, antiplatelet, hepatoprotective, neuroprotective | [75] |
| Jatropha curcas/Euphorbiaceae | Mexico, Central America, Brazil | leaves, roots, stems | phenolics, flavonoids, sterols, saponins, phorbol esters, cyclic peptides, lignans, alkaloids, coumarins, terpenes | anti-inflammatory, antimicrobial, antioxidant | [76,77] |
| Lycium barbarum/Solanaceae (Goji berry) | China, Asia, Europe | fruits, leaves, roots | polysaccharides, scopoletin, carotenoids, flavonoids, vitamins | antioxidant, antiviral, anticancer, anti-inflammatory, cardioprotective | [20,78] |
| Matricaria chamomilla/Asteraceae | Southeast Europe | flowers | terpenoids (α-bisabolol, chamazulene), flavonoids sesquiterpenes, coumarins, polyacetylenes | immunomodulatory, antioxidant, anti-inflammatory, antiseptic, antispasmodic | [79,80] |
| Mahonia aquifolium/Berberidacea | Eastern Asia, North and Central America | leaves, bark | alkaloids, phenolics, flavonoids, quinones, vitamins, coumarins | anti-inflammatory, antifungal, antimicrobial, antiproliferative, hepatoprotective, analgesic, antioxidant | [81,82] |
| Morus alba/Moraceae | Central and Eastern Asia, Caucasus, widely cultivated around the world | fruits, leaves, bark | flavonoids, anthocyanins, saponins, alkaloids, tannins, phenolic acids, anthocyanins, ascorbic acid, β-carotene | anticancer, antimicrobial, antidiabetic, immunomodulatory, cardioprotective, hepatoprotective, hypocholesterolemic, | [17,83,84] |
| Vaccinium vitis-idaea/Ericaceae | Baltic countries (Europe), Russia, Canada | leaves, fruits | phenolic, arbutin, flavonol glycosides, proanthocyanidins | antioxidant | [85] |
| Cetraria islandica/Parmeliaceae | Europe, North America | seeds, fruits, roots, leaves, stems, | dibenzofuranos, depsidones, fatty acids (lichesterinic acid, protolichesterinic acids), depsides, terpenes | immunomodulatory, antioxidant, cytotoxic, genotoxic, antigenotoxic, antimicrobial, anticancer, antidiabetic, anti-inflammatory | [86] |
| Lavandula angustifolia/Lamiaceae | Europe | stems, flowers | terpenes, polyphenols (rosmarinic acid, caffeic acid, lavandufurandiol, lavandunat), coumarins, flavonoids (apigenin, luteolin glycosides, catechin) | immunomodulatory, antioxidant, anti-inflammatory, analgesic, antibacterial | [87] |
| Chemical Compounds/Molecules | Mechanism | Clinical Trials (Number) | Reference |
|---|---|---|---|
| Berberine | Regulate T cell cytokines TNF-α, IL-2, and IL-4 production | 84 | [228] |
| Piperine | Reduce IL-1β, IL-6, and TNF-α; regulate expression of COX-2, NOS-2, and NF-κB | 28 | [229] |
| Xanthohumol | Inhibit NO production | 10 | [230] |
| Matrine | Reduced reactive oxygen species inflammatory mediators and myeloperoxidase and maleic dialdehyde activity | 2 | [231] |
| Daidzein | Decreases TNF-α, IL-1β, MCP-1, NO, and iNOS | 24 | [157] |
| Luteolin | Reduce secretion of INF-γ, IL-6, COX-2, and ICAM-1 Block heat shock protein 90 activity | 18 | [232] |
| Apigenin | Downregulate expression of IL-1α, TNF-α, IL-8, COX-2, and iNOS Decreased response of Th1 and Th17 cells | 12 | [233] |
| Nobiletin | Inhibit COX-2 and iNOS expression by blocking NF-κB and MAPK signaling | 1 | [234] |
| Baicalein | Inhibit expression of iNOS, COX-2, TNF-α, IL-1β, PGE2, and TNF-α by regulating NF-κB and ER-dependent pathway | 1 | [235,236] |
| Kaempferol | Reduce iNOS and COX-2 by suppressing STAT-1, NF-kappa B, and AP-1 Decrease expression of ICAM-1, VCAM-1, and MCP-1 | 5 | [157] |
| Rutin | Suppress production of TNF-α and IL-6 Activation of NF-κB and leukocyte migration | 34 | [237] |
| Puerarin | Inhibit NF-κB and activation of STAT3 | 8 | [238] |
| Thymoquinone | Inhibit IL-1β, TNF-α, MMP-13, COX-2, and PGE2, MAPK p38, ERK1/2, and NF-kBp65 | 8 | [239] |
| Piceatannol | Inhibit iNOS expression and NF-kB, ERK, and STAT3 | 1 | [240] |
| Shikonin | Inhibit NF-κB activity and Th1 cytokines expression and induce Th2 cytokines | 2 | [241] |
| Oleanolic acid | Reduce the level of IL-1α, IL-6, and TNF-α and adenosine deaminase activity | 4 | [242] |
| Triptolide | Inhibits lymphocyte activation, IL-2, iNOS, TNF-α, COX-2, IFN-γ, NF-kB, NFAT, and STAT3 | 25 | [243] |
| Celastrol | Inhibit IL-2, iNOS, TNF-α, COX-2, adhesion molecules and topoisomerase II | 2 | [244] |
| Tetrandrine | Regulates ERK/NF-κB signaling and inhibits activation of mesangial cells | 2 | [245] |
| Apocynin | Inhibit NADPH oxidase and suppress pro-inflammatory cytokines, and CD4+ and CD8+ T cell production | 8 | [246] |
| 11-keto-β-boswellic acid | Decrease IL-1, IL-2, IL-4, IL-6, and IFN-γ | 1 | [247] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miteva, D.; Kitanova, M.; Velikova, T. Biomacromolecules as Immunomodulators: Utilizing Nature’s Tools for Immune Regulation. Macromol 2024, 4, 610-633. https://doi.org/10.3390/macromol4030037
Miteva D, Kitanova M, Velikova T. Biomacromolecules as Immunomodulators: Utilizing Nature’s Tools for Immune Regulation. Macromol. 2024; 4(3):610-633. https://doi.org/10.3390/macromol4030037
Chicago/Turabian StyleMiteva, Dimitrina, Meglena Kitanova, and Tsvetelina Velikova. 2024. "Biomacromolecules as Immunomodulators: Utilizing Nature’s Tools for Immune Regulation" Macromol 4, no. 3: 610-633. https://doi.org/10.3390/macromol4030037
APA StyleMiteva, D., Kitanova, M., & Velikova, T. (2024). Biomacromolecules as Immunomodulators: Utilizing Nature’s Tools for Immune Regulation. Macromol, 4(3), 610-633. https://doi.org/10.3390/macromol4030037








