Microneedles’ Device: Design, Fabrication, and Applications
Abstract
1. Introduction
2. Types of Microneedles
2.1. Solid Microneedles
2.2. Coated Microneedles
2.3. Dissolving Microneedles
2.4. Hollow Microneedles
2.5. Hydrogel-Forming Microneedles
3. Microneedle Design
3.1. Length
3.2. Needle-to-Needle Spacing
3.3. Tip Diameter and Tip Angle
3.4. Aspect Ratio
3.5. Needle Geometry
4. Microneedle Fabrication Methods
4.1. Microelectromechanical Systems (MEMSs)
4.2. Micromolding
4.3. Laser Cutting
4.4. Laser Ablation
4.5. Drawing-Based Methods
4.6. Atomized Spraying Method
4.7. Injection Molding
4.8. Micro-Mechanical Machining
4.9. Additive Manufacturing
4.9.1. Fused Deposition Modelling (FDM)
4.9.2. Material Jetting (MJ)
4.9.3. Stereolithography (SLA)
4.9.4. Digital Light Processing (DLP)
4.9.5. Continuous Liquid Interface Production (CLIP)
4.9.6. Two-Photon Polymerization (2PP)
5. Microneedle System Applications
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chuong, C.M.; Nickoloff, B.J.; Elias, P.M.; Goldsmith, L.A.; Macher, E.; Maderson, P.A.; Sundberg, J.P.; Tagami, H.; Plonka, P.M.; Thestrup-Pedersen, K.; et al. What is the “true” function of skin? Exp. Dermatol. 2002, 11, 159–160. [Google Scholar] [CrossRef]
- Chien, Y.W.; Liu, J.-C. Transdermal Drug Delivery Systems. J. Biomater. Appl. 1986, 1, 183–206. [Google Scholar] [CrossRef]
- Wong, W.F.; Ang, K.P.; Sethi, G.; Looi, C.Y. Recent Advancement of Medical Patch for Transdermal Drug Delivery. Medicina 2023, 59, 778. [Google Scholar] [CrossRef]
- Lasagna, L.; Greenblatt, D.J. More Than Skin Deep: Transdermal Drug-Delivery Systems. N. Engl. J. Med. 1986, 314, 1638–1639. [Google Scholar] [CrossRef]
- Zhou, Q.; Li, H.; Liao, Z.; Gao, B.; He, B. Bridging the Gap between Invasive and Noninvasive Medical Care: Emerging Microneedle Approaches. Anal. Chem. 2023, 95, 515–534. [Google Scholar] [CrossRef]
- Waghule, T.; Singhvi, G.; Dubey, S.K.; Pandey, M.M.; Gupta, G.; Singh, M.; Dua, K. Microneedles: A smart approach and increasing potential for transdermal drug delivery system. Biomed. Pharmacother. 2019, 109, 1249–1258. [Google Scholar] [CrossRef]
- Pettis, R.J.; Harvey, A.J.; Ham, A.S.; Buckheit, R.W.; Singla, S.K.; Sachdeva, V.; Shin, C.I.; Jeong, S.D.; Rejinold, N.S.; Kim, Y.-C.; et al. Microneedle delivery: Clinical studies and emerging medical applications. Ther. Deliv. 2012, 3, 357–371. [Google Scholar] [CrossRef]
- Al-Japairai, K.A.S.; Mahmood, S.; Almurisi, S.H.; Venugopal, J.R.; Hilles, A.R.; Azmana, M.; Raman, S. Current trends in polymer microneedle for transdermal drug delivery. Int. J. Pharm. 2020, 587, 119673. [Google Scholar] [CrossRef]
- Yan, G.; Warner, K.S.; Zhang, J.; Sharma, S.; Gale, B.K. Evaluation needle length and density of microneedle arrays in the pretreatment of skin for transdermal drug delivery. Int. J. Pharm. 2010, 391, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Xu, D.; Xuan, X.; He, H. Advances of Microneedles in Biomedical Applications. Molecules 2021, 26, 5912. [Google Scholar] [CrossRef] [PubMed]
- Sachan, A.; Sachan, R.J.; Lu, J.; Sun, H.; Jin, Y.J.; Erdmann, D.; Zhang, J.Y.; Narayan, R.J. Injection molding for manufacturing of solid poly(l-lactide-co-glycolide) microneedles. MRS Adv. 2021, 6, 61–65. [Google Scholar] [CrossRef]
- Jin, X.; Zhu, D.D.; Chen, B.Z.; Ashfaq, M.; Guo, X.D. Insulin delivery systems combined with microneedle technology. Adv. Drug Deliv. Rev. 2018, 127, 119–137. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.; Yu, Q.; Liu, Y.; Gai, W.; Ye, L.; Yang, L.; Cui, Y. Closed-Loop Diabetes Minipatch Based on a Biosensor and an Electroosmotic Pump on Hollow Biodegradable Microneedles. ACS Sens. 2022, 7, 1347–1360. [Google Scholar] [CrossRef] [PubMed]
- Han, D.; Morde, R.S.; Mariani, S.; La Mattina, A.A.; Vignali, E.; Yang, C.; Barillaro, G.; Lee, H. 4D Printing of a Bioinspired Microneedle Array with Backward-Facing Barbs for Enhanced Tissue Adhesion. Adv. Funct. Mater. 2020, 30, 1909197. [Google Scholar] [CrossRef]
- Kim, Y.-C.; Park, J.-H.; Prausnitz, M.R. Microneedles for drug and vaccine delivery. Adv. Drug Deliv. Rev. 2012, 64, 1547–1568. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.; Ma, Y.; Lee, Y.-H.; Jung, H. Clinical Evaluation of a Low-pain Long Microneedle for Subcutaneous Insulin Injection. BioChip J. 2018, 12, 309–316. [Google Scholar] [CrossRef]
- Zhang, R.; Miao, Q.; Deng, D.; Wu, J.; Miao, Y.; Li, Y. Research progress of advanced microneedle drug delivery system and its application in biomedicine. Colloids Surf. B Biointerfaces 2023, 226, 113302. [Google Scholar] [CrossRef]
- Parhi, R. Recent advances in 3D printed microneedles and their skin delivery application in the treatment of various diseases. J. Drug Deliv. Sci. Technol. 2023, 84, 104395. [Google Scholar] [CrossRef]
- Yang, G.; Chen, Q.; Wen, D.; Chen, Z.; Wang, J.; Chen, G.; Wang, Z.; Zhang, X.; Zhang, Y.; Hu, Q.; et al. A Therapeutic Microneedle Patch Made from Hair-Derived Keratin for Promoting Hair Regrowth. ACS Nano 2019, 13, 4354–4360. [Google Scholar] [CrossRef] [PubMed]
- Barnum, L.; Samandari, M.; Schmidt, T.A.; Tamayol, A. Microneedle arrays for the treatment of chronic wounds. Expert Opin. Drug Deliv. 2020, 17, 1767–1780. [Google Scholar] [CrossRef]
- Than, A.; Liu, C.; Chang, H.; Duong, P.K.; Cheung, C.M.G.; Xu, C.; Wang, X.; Chen, P. Self-implantable double-layered micro-drug-reservoirs for efficient and controlled ocular drug delivery. Nat. Commun. 2018, 9, 4433. [Google Scholar] [CrossRef] [PubMed]
- Ju, E.; Peng, M.; Xu, Y.; Wang, Y.; Zhou, F.; Wang, H.; Li, M.; Zheng, Y.; Tao, Y. Nanozyme-integrated microneedle patch for enhanced therapy of cutaneous squamous cell carcinoma by breaking the gap between H2O2 self-supplying chemodynamic therapy and photothermal therapy. J. Mater. Chem. B 2023, 11, 6595–6602. [Google Scholar] [CrossRef] [PubMed]
- Shukla, S.; Mamale, K.B.; Arya, R.K.; Kaundal, R.K.; Shukla, R. Therapeutic potential of microneedles based delivery systems for the management of atopic dermatitis. J. Drug Deliv. Sci. Technol. 2023, 84, 104493. [Google Scholar] [CrossRef]
- Cheng, X.; Hu, S.; Cheng, K. Microneedle Patch Delivery of PROTACs for Anti-Cancer Therapy. ACS Nano 2023, 17, 11855–11868. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Chen, J.Y.; Terry, R.N.; Tang, J.; Romanyuk, A.; Schwendeman, S.P.; Prausnitz, M.R. Core-shell microneedle patch for six-month controlled-release contraceptive delivery. J. Control. Release 2022, 347, 489–499. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Park, I.H.; Shin, J.; Choi, J.; Jeon, C.; Jeon, S.; Shin, J.; Jung, H. Sublingual Dissolving Microneedle (SLDMN)-based Vaccine for Inducing Mucosal Immunity Against SARS-CoV-2. Adv. Healthc. Mater. 2023, 12, 2300889. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yang, L.; Zhang, F.; Liu, X.; Xie, Q.; Liu, Q.; Yuan, L.; Zhao, T.; Xie, S.; Xu, Q.; et al. A microneedle-based delivery system for broad-protection seasonal influenza A DNA nanovaccines. Cell Rep. Phys. Sci. 2023, 4, 101430. [Google Scholar] [CrossRef]
- Friedel, M.; Werbovetz, B.; Drexelius, A.; Watkins, Z.; Bali, A.; Plaxco, K.W.; Heikenfeld, J. Continuous molecular monitoring of human dermal interstitial fluid with microneedle-enabled electrochemical aptamer sensors. Lab Chip 2023, 23, 3289–3299. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Cai, X.; Zhang, W.; Zhu, D.; Ruan, Z.; Jin, N. Fabrication of Antibacterial Sponge Microneedles for Sampling Skin Interstitial Fluid. Pharmaceutics 2023, 15, 1730. [Google Scholar] [CrossRef]
- Alimardani, V.; Abolmaali, S.S.; Yousefi, G.; Rahiminezhad, Z.; Abedi, M.; Tamaddon, A.; Ahadian, S. Microneedle Arrays Combined with Nanomedicine Approaches for Transdermal Delivery of Therapeutics. J. Clin. Med. 2021, 10, 181. [Google Scholar] [CrossRef]
- Li, Q.Y.; Zhang, J.N.; Chen, B.Z.; Wang, Q.L.; Guo, X.D. A solid polymer microneedle patch pretreatment enhances the permeation of drug molecules into the skin. RSC Adv. 2017, 7, 15408–15415. [Google Scholar] [CrossRef]
- de Groot, A.M.; Platteel, A.C.M.; Kuijt, N.; van Kooten, P.J.S.; Vos, P.J.; Sijts, A.J.A.M.; van der Maaden, K. Nanoporous Microneedle Arrays Effectively Induce Antibody Responses against Diphtheria and Tetanus Toxoid. Front. Immunol. 2017, 8, 1789. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Roh, M.R.; Park, G.; Kim, Y.J.; Jeon, I.K.; Chang, S.E. Fractionated microneedle radiofrequency for the treatment of periorbital wrinkles. J. Dermatol. 2013, 40, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Abiandu, I.; Ita, K. Transdermal delivery of potassium chloride with solid microneedles. J. Drug Deliv. Sci. Technol. 2019, 53, 101216. [Google Scholar] [CrossRef]
- Bollella, P.; Sharma, S.; Cass, A.E.G.; Antiochia, R. Minimally-invasive Microneedle-based Biosensor Array for Simultaneous Lactate and Glucose Monitoring in Artificial Interstitial Fluid. Electroanalysis 2019, 31, 374–382. [Google Scholar] [CrossRef]
- Senel, M.; Dervisevic, M.; Voelcker, N.H. Gold microneedles fabricated by casting of gold ink used for urea sensing. Mater. Lett. 2019, 243, 50–53. [Google Scholar] [CrossRef]
- Bhadale, R.S.; Londhe, V.Y. Solid microneedle assisted transepidermal delivery of iloperidone loaded film: Characterization and Skin deposition studies. J. Drug Deliv. Sci. Technol. 2023, 79, 104028. [Google Scholar] [CrossRef]
- van der Maaden, K.; Yu, H.; Sliedregt, K.; Zwier, R.; Leboux, R.; Oguri, M.; Kros, A.; Jiskoot, W.; Bouwstra, J.A. Nanolayered chemical modification of silicon surfaces with ionizable surface groups for pH-triggered protein adsorption and release: Application to microneedles. J. Mater. Chem. B 2013, 1, 4466–4477. [Google Scholar] [CrossRef] [PubMed]
- Meyer, B.K.; Kendall, M.A.; Williams, D.M.; Bett, A.J.; Dubey, S.; Gentzel, R.C.; Casimiro, D.; Forster, A.; Corbett, H.; Crichton, M.; et al. Immune response and reactogenicity of an unadjuvanted intradermally delivered human papillomavirus vaccine using a first generation Nanopatch™ in rhesus macaques: An exploratory, pre-clinical feasibility assessment. Vaccine X 2019, 2, 100030. [Google Scholar] [CrossRef]
- Daddona, P.E.; Matriano, J.A.; Mandema, J.; Maa, Y.-F. Parathyroid Hormone (1-34)-Coated Microneedle Patch System: Clinical Pharmacokinetics and Pharmacodynamics for Treatment of Osteoporosis. Pharm. Res. 2010, 28, 159–165. [Google Scholar] [CrossRef]
- Ross, S.; Scoutaris, N.; Lamprou, D.; Mallinson, D.; Douroumis, D. Inkjet printing of insulin microneedles for transdermal delivery. Drug Deliv. Transl. Res. 2015, 5, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Cormier, M.; Johnson, B.; Ameri, M.; Nyam, K.; Libiran, L.; Zhang, D.D.; Daddona, P. Transdermal delivery of desmopressin using a coated microneedle array patch system. J. Control. Release 2004, 97, 503–511. [Google Scholar] [CrossRef] [PubMed]
- Al Sulaiman, D.; Chang, J.Y.H.; Bennett, N.R.; Topouzi, H.; Higgins, C.A.; Irvine, D.J.; Ladame, S. Hydrogel-Coated Microneedle Arrays for Minimally Invasive Sampling and Sensing of Specific Circulating Nucleic Acids from Skin Interstitial Fluid. ACS Nano 2019, 13, 9620–9628. [Google Scholar] [CrossRef] [PubMed]
- Matadh, A.V.; Jakka, D.; Pragathi, S.; Poornima, K.; Shivakumar, H.; Murthy, R.N.; Rangappa, S.; Shivanna, M.; Murthy, S.N. Polymer coated polymeric microneedles for intravitreal delivery of dexamethasone. Exp. Eye Res. 2023, 231, 109467. [Google Scholar] [CrossRef] [PubMed]
- Han, J.H.; Kim, C.R.; Min, C.H.; Kim, M.J.; Kim, S.-N.; Ji, H.B.; Bin Yoon, S.; Lee, C.; Bin Choy, Y. Microneedles coated with composites of phenylboronic acid-containing polymer and carbon nanotubes for glucose measurements in interstitial fluids. Biosens. Bioelectron. 2023, 238, 115571. [Google Scholar] [CrossRef] [PubMed]
- Ramöller, I.K.; Tekko, I.A.; McCarthy, H.O.; Donnelly, R.F. Rapidly dissolving bilayer microneedle arrays—A minimally invasive transdermal drug delivery system for vitamin B12. Int. J. Pharm. 2019, 566, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Lai, K.-Y.; Chiu, Y.-H.; Wu, Y.-W.; Shiau, A.-L.; Chen, M.-C. Implantable microneedles with an immune-boosting function for effective intradermal influenza vaccination. Acta Biomater. 2019, 97, 230–238. [Google Scholar] [CrossRef]
- Dillon, C.; Hughes, H.; O’Reilly, N.J.; Allender, C.J.; Barrow, D.A.; McLoughlin, P. Dissolving microneedle based transdermal delivery of therapeutic peptide analogues. Int. J. Pharm. 2019, 565, 9–19. [Google Scholar] [CrossRef]
- Disphanurat, W.; Sivapornpan, N.; Srisantithum, B.; Leelawattanachai, J. Efficacy of a triamcinolone acetonide-loaded dissolving microneedle patch for the treatment of hypertrophic scars and keloids: A randomized, double-blinded, placebo-controlled split-scar study. Arch. Dermatol. Res. 2023, 315, 989–997. [Google Scholar] [CrossRef]
- Wang, H.; Fu, Y.; Liu, P.; Qu, F.; Du, S.; Li, Y.; Du, H.; Zhang, L.; Tao, J.; Zhu, J. Supramolecular Dissolving Microneedle Patch Loading Hydrophobic Glucocorticoid for Effective Psoriasis Treatment. ACS Appl. Mater. Interfaces 2023, 15, 15162–15171. [Google Scholar] [CrossRef]
- Lin, S.; Quan, G.; Hou, A.; Yang, P.; Peng, T.; Gu, Y.; Qin, W.; Liu, R.; Ma, X.; Pan, X.; et al. Strategy for hypertrophic scar therapy: Improved delivery of triamcinolone acetonide using mechanically robust tip-concentrated dissolving microneedle array. J. Control. Release 2019, 306, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Kim, S.; Jang, M.; Kim, H.; Lee, S.; Kim, Y.; Eom, Y.A.; Kang, G.; Chiang, L.; Baek, J.H.; et al. Two-phase delivery using a horse oil and adenosine-loaded dissolving microneedle patch for skin barrier restoration, moisturization, and wrinkle improvement. J. Cosmet. Dermatol. 2019, 18, 936–943. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.X.; Bozorg, B.D.; Kim, Y.; Wieber, A.; Birk, G.; Lubda, D.; Banga, A.K. Poly (vinyl alcohol) microneedles: Fabrication, characterization, and application for transdermal drug delivery of doxorubicin. Eur. J. Pharm. Biopharm. 2018, 129, 88–103. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Li, Y.; Li, Z.; Xu, N.; Liu, P.; Du, H.; Zhang, Y.; Huang, Y.; Zhu, J.; Ren, G.; et al. Au Nanocage-Strengthened Dissolving Microneedles for Chemo-Photothermal Combined Therapy of Superficial Skin Tumors. ACS Appl. Mater. Interfaces 2018, 10, 9247–9256. [Google Scholar] [CrossRef] [PubMed]
- Huh, I.; Kim, S.; Yang, H.; Jang, M.; Kang, G.; Jung, H. Effects of two droplet-based dissolving microneedle manufacturing methods on the activity of encapsulated epidermal growth factor and ascorbic acid. Eur. J. Pharm. Sci. 2018, 114, 285–292. [Google Scholar] [CrossRef]
- Hamdan, I.M.; Tekko, I.A.; Matchett, K.B.; Arnaut, L.G.; Silva, C.S.; McCarthy, H.O.; Donnelly, R.F. Intradermal Delivery of a Near-Infrared Photosensitizer Using Dissolving Microneedle Arrays. J. Pharm. Sci. 2018, 107, 2439–2450. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, F.; Su, C.; Yu, B.; Liu, D.; Chen, H.-J.; Lin, D.-A.; Yang, C.; Zhou, L.; Wu, Q.; et al. Biodegradable Therapeutic Microneedle Patch for Rapid Antihypertensive Treatment. ACS Appl. Mater. Interfaces 2019, 11, 30575–30584. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Hong, J.; Seo, Y.; Joo, S.; Lim, H.; Lahiji, S.F.; Kim, Y. Self-Assembled Oligopeptoplex-Loaded Dissolving Microneedles for Adipocyte-Targeted Anti-Obesity Gene Therapy. Adv. Mater. 2024, 36, 2309920. [Google Scholar] [CrossRef]
- Wan, W.; Li, Y.; Wang, J.; Jin, Z.; Xin, W.; Kang, L.; Wang, J.; Li, X.; Cao, Y.; Yang, H.; et al. PLGA Nanoparticle-Based Dissolving Microneedle Vaccine of Clostridium perfringens ε Toxin. Toxins 2023, 15, 461. [Google Scholar] [CrossRef]
- Jiang, X.; Chen, P.; Niu, W.; Fang, R.; Chen, H.; An, Y.; Wang, W.; Jiang, C.; Ye, J. Preparation and evaluation of dissolving tofacitinib microneedles for effective management of rheumatoid arthritis. Eur. J. Pharm. Sci. 2023, 188, 106518. [Google Scholar] [CrossRef]
- Xie, J.; Zhu, X.; Wang, M.; Liu, C.; Ling, G.; Zhang, P. Dissolving microneedle-mediated transdermal delivery of flurbiprofen axetil-loaded pH-responsive liposomes for arthritis treatment. Chem. Eng. J. 2024, 482, 148840. [Google Scholar] [CrossRef]
- Abd-El-Azim, H.; Abbas, H.; El Sayed, N.S.; Fayez, A.M.; Zewail, M. Non-invasive management of rheumatoid arthritis using hollow microneedles as a tool for transdermal delivery of teriflunomide loaded solid lipid nanoparticles. Int. J. Pharm. 2023, 644, 123334. [Google Scholar] [CrossRef] [PubMed]
- Kawre, S.; Suryavanshi, P.; Lalchandani, D.S.; Deka, M.K.; Porwal, P.K.; Kaity, S.; Roy, S.; Banerjee, S. Bioinspired labrum-shaped stereolithography (SLA) assisted 3D printed hollow microneedles (HMNs) for effectual delivery of ceftriaxone sodium. Eur. Polym. J. 2024, 204, 112702. [Google Scholar] [CrossRef]
- Golombek, S.; Pilz, M.; Steinle, H.; Kochba, E.; Levin, Y.; Lunter, D.; Schlensak, C.; Wendel, H.P.; Avci-Adali, M. Intradermal Delivery of Synthetic mRNA Using Hollow Microneedles for Efficient and Rapid Production of Exogenous Proteins in Skin. Mol. Ther. Nucleic Acids 2018, 11, 382–392. [Google Scholar] [CrossRef] [PubMed]
- van der Maaden, K.; Heuts, J.; Camps, M.; Pontier, M.; van Scheltinga, A.T.; Jiskoot, W.; Ossendorp, F.; Bouwstra, J. Hollow microneedle-mediated micro-injections of a liposomal HPV E743–63 synthetic long peptide vaccine for efficient induction of cytotoxic and T-helper responses. J. Control. Release 2018, 269, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Iliescu, F.S.; Teo, J.C.M.; Vrtacnik, D.; Taylor, H.; Iliescu, C. Cell therapy using an array of ultrathin hollow microneedles. Microsyst. Technol. 2018, 24, 2905–2912. [Google Scholar] [CrossRef]
- Yin, S.; Yu, Z.; Song, N.; Guo, Z.; Li, W.; Ma, J.; Wang, X.; Liu, J.; Liang, M. A long lifetime and highly sensitive wearable microneedle sensor for the continuous real-time monitoring of glucose in interstitial fluid. Biosens. Bioelectron. 2024, 244, 115822. [Google Scholar] [CrossRef] [PubMed]
- Drăgan, A.-M.; Parrilla, M.; Cambré, S.; Domínguez-Robles, J.; Detamornrat, U.; Donnelly, R.F.; Oprean, R.; Cristea, C.; De Wael, K. Microneedle array-based electrochemical sensor functionalized with SWCNTs for the highly sensitive monitoring of MDMA in interstitial fluid. Microchem. J. 2023, 193, 109257. [Google Scholar] [CrossRef]
- Abbasiasl, T.; Mirlou, F.; Mirzajani, H.; Bathaei, M.J.; Istif, E.; Shomalizadeh, N.; Cebecioğlu, R.E.; Özkahraman, E.E.; Yener, U.C.; Beker, L. A Wearable Touch-Activated Device Integrated with Hollow Microneedles for Continuous Sampling and Sensing of Dermal Interstitial Fluid. Adv. Mater. 2024, 36, e2304704. [Google Scholar] [CrossRef]
- Aziz, A.Y.R.; Hasir, N.A.; Imran, N.B.P.; Hamdan, M.F.; Mahfufah, U.; Wafiah, N.; Arjuna, A.; Utami, R.N.; Permana, A.D. Development of hydrogel-forming microneedles for transdermal delivery of albendazole from liquid reservoir. J. Biomater. Sci. Polym. Ed. 2023, 34, 1101–1120. [Google Scholar] [CrossRef]
- Elim, D.; Fitri, A.M.N.; Mahfud, M.A.S.; Afika, N.; Sultan, N.A.F.; Hijrah; Asri, R.M.; Permana, A.D. Hydrogel forming microneedle-mediated transdermal delivery of sildenafil citrate from polyethylene glycol reservoir: An ex vivo proof of concept study. Colloids Surf. B Biointerfaces 2023, 222, 113018. [Google Scholar] [CrossRef] [PubMed]
- Migdadi, E.M.; Courtenay, A.J.; Tekko, I.A.; McCrudden, M.T.; Kearney, M.-C.; McAlister, E.; McCarthy, H.O.; Donnelly, R.F. Hydrogel-forming microneedles enhance transdermal delivery of metformin hydrochloride. J. Control. Release 2018, 285, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Sivaraman, A.; Banga, A.K. Novel in situ forming hydrogel microneedles for transdermal drug delivery. Drug Deliv. Transl. Res. 2017, 7, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Anjani, Q.K.; Permana, A.D.; Cárcamo-Martínez, Á.; Domínguez-Robles, J.; Tekko, I.A.; Larrañeta, E.; Vora, L.K.; Ramadon, D.; Donnelly, R.F. Versatility of hydrogel-forming microneedles in in vitro transdermal delivery of tuberculosis drugs. Eur. J. Pharm. Biopharm. 2021, 158, 294–312. [Google Scholar] [CrossRef] [PubMed]
- Leanpolchareanchai, J.; Nuchtavorn, N. Response Surface Methodology for Optimization of Hydrogel-Forming Microneedles as Rapid and Efficient Transdermal Microsampling Tools. Gels 2023, 9, 306. [Google Scholar] [CrossRef]
- Mikszta, J.A.; Alarcon, J.B.; Brittingham, J.M.; Sutter, D.E.; Pettis, R.J.; Harvey, N.G. Improved genetic immunization via micromechanical disruption of skin-barrier function and targeted epidermal delivery. Nat. Med. 2002, 8, 415–419. [Google Scholar] [CrossRef] [PubMed]
- Sabri, A.; Ogilvie, J.; McKenna, J.; Segal, J.; Scurr, D.; Marlow, M. Intradermal Delivery of an Immunomodulator for Basal Cell Carcinoma; Expanding the Mechanistic Insight into Solid Microneedle-Enhanced Delivery of Hydrophobic Molecules. Mol. Pharm. 2020, 17, 2925–2937. [Google Scholar] [CrossRef] [PubMed]
- Elahpour, N.; Pahlevanzadeh, F.; Kharaziha, M.; Bakhsheshi-Rad, H.R.; Ramakrishna, S.; Berto, F. 3D printed microneedles for transdermal drug delivery: A brief review of two decades. Int. J. Pharm. 2021, 597, 120301. [Google Scholar] [CrossRef] [PubMed]
- Larrañeta, E.; Lutton, R.E.M.; Woolfson, A.D.; Donnelly, R.F. Microneedle arrays as transdermal and intradermal drug delivery systems: Materials science, manufacture and commercial development. Mater. Sci. Eng. R Rep. 2016, 104, 1–32. [Google Scholar] [CrossRef]
- Donnelly, R.F.; Singh, T.R.R.; Alkilani, A.Z.; McCrudden, M.T.C.; O’Neill, S.; O’Mahony, C.; Armstrong, K.; McLoone, N.; Kole, P.; Woolfson, A.D. Hydrogel-forming microneedle arrays exhibit antimicrobial properties: Potential for enhanced patient safety. Int. J. Pharm. 2013, 451, 76–91. [Google Scholar] [CrossRef]
- Parhi, R. A review of three-dimensional printing for pharmaceutical applications: Quality control, risk assessment and future perspectives. J. Drug Deliv. Sci. Technol. 2021, 64, 102571. [Google Scholar] [CrossRef]
- Gupta, J.; Gill, H.S.; Andrews, S.N.; Prausnitz, M.R. Kinetics of skin resealing after insertion of microneedles in human subjects. J. Control. Release 2011, 154, 148–155. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, B.Z.; Wang, Q.L.; Jin, X.; Guo, X.D. Fabrication of coated polymer microneedles for transdermal drug delivery. J. Control. Release 2017, 265, 14–21. [Google Scholar] [CrossRef]
- Ingrole, R.S.; Gill, H.S. Microneedle Coating Methods: A Review with a Perspective. J. Pharmacol. Exp. Ther. 2019, 370, 555–569. [Google Scholar] [CrossRef]
- Vrdoljak, A.; McGrath, M.G.; Carey, J.B.; Draper, S.J.; Hill, A.V.; O’Mahony, C.; Crean, A.M.; Moore, A.C. Coated microneedle arrays for transcutaneous delivery of live virus vaccines. J. Control. Release 2012, 159, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Chong, R.H.; Gonzalez-Gonzalez, E.; Lara, M.F.; Speaker, T.J.; Contag, C.H.; Kaspar, R.L.; Coulman, S.A.; Hargest, R.; Birchall, J.C. Gene silencing following siRNA delivery to skin via coated steel microneedles: In vitro and in vivo proof-of-concept. J. Control. Release 2013, 166, 211–219. [Google Scholar] [CrossRef]
- Choi, H.-J.; Yoo, D.-G.; Bondy, B.J.; Quan, F.-S.; Compans, R.W.; Kang, S.-M.; Prausnitz, M.R. Stability of influenza vaccine coated onto microneedles. Biomaterials 2012, 33, 3756–3769. [Google Scholar] [CrossRef] [PubMed]
- Pere, C.P.P.; Economidou, S.N.; Lall, G.; Ziraud, C.; Boateng, J.S.; Alexander, B.D.; Lamprou, D.A.; Douroumis, D. 3D printed microneedles for insulin skin delivery. Int. J. Pharm. 2018, 544, 425–432. [Google Scholar] [CrossRef]
- Li, J.; Zeng, M.; Shan, H.; Tong, C. Microneedle Patches as Drug and Vaccine Delivery Platform. Curr. Med. Chem. 2017, 24, 2413–2422. [Google Scholar] [CrossRef] [PubMed]
- Makvandi, P.; Maleki, A.; Shabani, M.; Hutton, A.R.; Kirkby, M.; Jamaledin, R.; Fang, T.; He, J.; Lee, J.; Mazzolai, B.; et al. Bioinspired microneedle patches: Biomimetic designs, fabrication, and biomedical applications. Matter 2022, 5, 390–429. [Google Scholar] [CrossRef]
- Park, J.-H.; Allen, M.G.; Prausnitz, M.R. Polymer Microneedles for Controlled-Release Drug Delivery. Pharm. Res. 2006, 23, 1008–1019. [Google Scholar] [CrossRef]
- McCrudden, M.T.; Alkilani, A.Z.; McCrudden, C.M.; McAlister, E.; McCarthy, H.O.; Woolfson, A.D.; Donnelly, R.F. Design and physicochemical characterisation of novel dissolving polymeric microneedle arrays for transdermal delivery of high dose, low molecular weight drugs. J. Control. Release 2014, 180, 71–80. [Google Scholar] [CrossRef]
- Long, L.; Ji, D.; Hu, C.; Yang, L.; Tang, S.; Wang, Y. Microneedles for in situ tissue regeneration. Mater. Today Bio 2023, 19, 100579. [Google Scholar] [CrossRef]
- Bauleth-Ramos, T.; El-Sayed, N.; Fontana, F.; Lobita, M.; Shahbazi, M.-A.; Santos, H.A. Recent approaches for enhancing the performance of dissolving microneedles in drug delivery applications. Mater. Today 2023, 63, 239–287. [Google Scholar] [CrossRef]
- Lee, K.; Jung, H. Drawing lithography for microneedles: A review of fundamentals and biomedical applications. Biomaterials 2012, 33, 7309–7326. [Google Scholar] [CrossRef]
- Lee, K.; Lee, C.Y.; Jung, H. Dissolving microneedles for transdermal drug administration prepared by stepwise controlled drawing of maltose. Biomaterials 2011, 32, 3134–3140. [Google Scholar] [CrossRef]
- Miyano, T.; Tobinaga, Y.; Kanno, T.; Matsuzaki, Y.; Takeda, H.; Wakui, M.; Hanada, K. Sugar Micro Needles as Transdermic Drug Delivery System. Biomed. Microdevices 2005, 7, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Badkar, A.; Nema, S.; Kolli, C.S.; Banga, A.K. In vitro transdermal delivery of therapeutic antibodies using maltose microneedles. Int. J. Pharm. 2009, 368, 109–115. [Google Scholar] [CrossRef]
- Yang, B.; Dong, Y.; Shen, Y.; Hou, A.; Quan, G.; Pan, X.; Wu, C. Bilayer dissolving microneedle array containing 5-fluorouracil and triamcinolone with biphasic release profile for hypertrophic scar therapy. Bioact. Mater. 2021, 6, 2400–2411. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.Y.; Kwon, H.J.; Ahn, G.R.; Ko, E.J.; Yoo, K.H.; Kim, B.J.; Lee, C.; Kim, D. Hyaluronic acid microneedle patch for the improvement of crow’s feet wrinkles. Dermatol. Ther. 2017, 30, e12546. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Kim, B. Skin permeability of compounds loaded within dissolving microneedles dependent on composition of sodium hyaluronate and carboxymethyl cellulose. Korean J. Chem. Eng. 2017, 34, 133–138. [Google Scholar] [CrossRef]
- Zvezdin, V.; Kasatkina, T.; Kasatkin, I.; Gavrilova, M.; Kazakova, O. Microneedle patch based on dissolving, detachable microneedle technology for improved skin quality of the periorbital region. Part 2: Clinical Evaluation. Int. J. Cosmet. Sci. 2020, 42, 429–435. [Google Scholar] [CrossRef]
- Yalcintas, E.P.; Ackerman, D.S.; Korkmaz, E.; Telmer, C.A.; Jarvik, J.W.; Campbell, P.G.; Bruchez, M.P.; Ozdoganlar, O.B. Analysis of In Vitro Cytotoxicity of Carbohydrate-Based Materials Used for Dissolvable Microneedle Arrays. Pharm. Res. 2020, 37, 1–18. [Google Scholar] [CrossRef]
- Reineccius, G. 9-Controlled release of flavour in food products. In Modifying Flavour in Food; Taylor, A., Hort, J., Eds.; Woodhead Publishing Series in Food Science, Technology and Nutrition; Woodhead Publishing: Sawston, Cambridge, 2007; pp. 169–184. [Google Scholar] [CrossRef]
- Lee, B.-M.; Lee, C.; Lahiji, S.F.; Jung, U.-W.; Chung, G.; Jung, H. Dissolving Microneedles for Rapid and Painless Local Anesthesia. Pharmaceutics 2020, 12, 366. [Google Scholar] [CrossRef] [PubMed]
- Ono, A.; Ito, S.; Sakagami, S.; Asada, H.; Saito, M.; Quan, Y.-S.; Kamiyama, F.; Hirobe, S.; Okada, N. Development of Novel Faster-Dissolving Microneedle Patches for Transcutaneous Vaccine Delivery. Pharmaceutics 2017, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Yu, H.; Wang, L.; Shen, D.; Ni, Z.; Ren, S.; Lu, Y.; Chen, X.; Yang, J.; Hong, Y. Research progress on cosmetic microneedle systems: Preparation, property and application. Eur. Polym. J. 2022, 163, 110942. [Google Scholar] [CrossRef]
- Ke, C.-L.; Deng, F.-S.; Chuang, C.-Y.; Lin, C.-H. Antimicrobial Actions and Applications of Chitosan. Polymers 2021, 13, 904. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-C.; Huang, S.-F.; Lai, K.-Y.; Ling, M.-H. Fully embeddable chitosan microneedles as a sustained release depot for intradermal vaccination. Biomaterials 2013, 34, 3077–3086. [Google Scholar] [CrossRef]
- Chiu, Y.-H.; Chen, M.-C.; Wan, S.-W. Sodium Hyaluronate/Chitosan Composite Microneedles as a Single-Dose Intradermal Immunization System. Biomacromolecules 2018, 19, 2278–2285. [Google Scholar] [CrossRef]
- Kean, T.; Thanou, M. Biodegradation, biodistribution and toxicity of chitosan. Adv. Drug Deliv. Rev. 2010, 62, 3–11. [Google Scholar] [CrossRef]
- Zhang, L.; Guo, R.; Wang, S.; Yang, X.; Ling, G.; Zhang, P. Fabrication, evaluation and applications of dissolving microneedles. Int. J. Pharm. 2021, 604, 120749. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, D.F.S.; Vilela, C.; Silvestre, A.J.D.; Freire, C.S.R. A compendium of current developments on polysaccharide and protein-based microneedles. Int. J. Biol. Macromol. 2019, 136, 704–728. [Google Scholar] [CrossRef] [PubMed]
- Désévaux, C.; Dubreuil, P.; Lenaerts, V.; Girard, C. Tissue reaction and biodegradation of implanted cross-linked high amylose starch in rats. J. Biomed. Mater. Res. 2002, 63, 772–779. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Wang, B. Biodegradation of Silk Biomaterials. Int. J. Mol. Sci. 2009, 10, 1514–1524. [Google Scholar] [CrossRef]
- Wang, S.; Zhu, M.; Zhao, L.; Kuang, D.; Kundu, S.C.; Lu, S. Insulin-Loaded Silk Fibroin Microneedles as Sustained Release System. ACS Biomater. Sci. Eng. 2019, 5, 1887–1894. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Park, S.H.; Seo, I.H.; Lee, K.J.; Ryu, W. Rapid and repeatable fabrication of high A/R silk fibroin microneedles using thermally-drawn micromolds. Eur. J. Pharm. Biopharm. 2015, 94, 11–19. [Google Scholar] [CrossRef]
- Zhu, M.; Liu, Y.; Jiang, F.; Cao, J.; Lu, S. Combined Silk Fibroin Microneedles for Insulin Delivery. ACS Biomater. Sci. Eng. 2020, 6, 3422–3429. [Google Scholar] [CrossRef] [PubMed]
- Tsioris, K.; Raja, W.K.; Pritchard, E.M.; Panilaitis, B.; Kaplan, D.L.; Omenetto, F.G. Fabrication of Silk Microneedles for Controlled-Release Drug Delivery. Adv. Funct. Mater. 2012, 22, 330–335. [Google Scholar] [CrossRef]
- Stinson, J.A.; Raja, W.K.; Lee, S.; Kim, H.B.; Diwan, I.; Tutunjian, S.; Panilaitis, B.; Omenetto, F.G.; Tzipori, S.; Kaplan, D.L. Silk Fibroin Microneedles for Transdermal Vaccine Delivery. ACS Biomater. Sci. Eng. 2017, 3, 360–369. [Google Scholar] [CrossRef]
- Mao, J.; Wang, H.; Xie, Y.; Fu, Y.; Li, Y.; Liu, P.; Du, H.; Zhu, J.; Dong, L.; Hussain, M.; et al. Transdermal delivery of rapamycin with poor water-solubility by dissolving polymeric microneedles for anti-angiogenesis. J. Mater. Chem. B 2020, 8, 928–934. [Google Scholar] [CrossRef]
- Yu, K.; Yu, X.; Cao, S.; Wang, Y.; Zhai, Y.; Yang, F.; Yang, X.; Lu, Y.; Wu, C.; Xu, Y. Layered dissolving microneedles as a need-based delivery system to simultaneously alleviate skin and joint lesions in psoriatic arthritis. Acta Pharm. Sin. B 2021, 11, 505–519. [Google Scholar] [CrossRef] [PubMed]
- Vicente-Perez, E.M.; Larrañeta, E.; McCrudden, M.T.C.; Kissenpfennig, A.; Hegarty, S.; McCarthy, H.O.; Donnelly, R.F. Repeat application of microneedles does not alter skin appearance or barrier function and causes no measurable disturbance of serum biomarkers of infection, inflammation or immunity in mice in vivo. Eur. J. Pharm. Biopharm. 2017, 117, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Shim, W.S.; Hwang, Y.M.; Park, S.G.; Lee, C.K.; Kang, N.G. Role of Polyvinylpyrrolidone in Dissolving Microneedle for Efficient Transdermal Drug Delivery: In vitro and Clinical Studies. Bull. Korean Chem. Soc. 2018, 39, 789–793. [Google Scholar] [CrossRef]
- EFSA Panel on Food Additives and Flavourings (FAF); Younes, M.; Aquilina, G.; Castle, L.; Engel, K.; Fowler, P.; Fürst, P.; Gürtler, R.; Gundert-Remy, U.; Husøy, T.; et al. Re-evaluation of polyvinylpyrrolidone (E 1201) and polyvinylpolypyrrolidone (E 1202) as food additives and extension of use of polyvinylpyrrolidone (E 1201). EFSA J. 2020, 18, e06215. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.Z.; Ashfaq, M.; Zhang, X.P.; Zhang, J.N.; Guo, X.D. In vitro and in vivo assessment of polymer microneedles for controlled transdermal drug delivery. J. Drug Target. 2018, 26, 720–729. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.P.; Wang, B.B.; Li, W.X.; Fei, W.M.; Cui, Y.; Guo, X.D. In vivo safety assessment, biodistribution and toxicology of polyvinyl alcohol microneedles with 160-day uninterruptedly applications in mice. Eur. J. Pharm. Biopharm. 2021, 160, 1–8. [Google Scholar] [CrossRef]
- Arya, J.; Henry, S.; Kalluri, H.; McAllister, D.V.; Pewin, W.P.; Prausnitz, M.R. Tolerability, usability and acceptability of dissolving microneedle patch administration in human subjects. Biomaterials 2017, 128, 1–7. [Google Scholar] [CrossRef]
- Schmidt, S.J.; Holt, B.D.; Arnold, A.M.; Sydlik, S.A. Polyester functional graphenic materials as a mechanically enhanced scaffold for tissue regeneration. RSC Adv. 2020, 10, 8548–8557. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Y.; Jin, J.Y.; Degan, S.; Hall, R.P.; Boehm, R.D.; Jaipan, P.; Narayan, R.J. Use of Drawing Lithography-Fabricated Polyglycolic Acid Microneedles for Transdermal Delivery of Itraconazole to a Human Basal Cell Carcinoma Model Regenerated on Mice. JOM 2016, 68, 1128–1133. [Google Scholar] [CrossRef]
- Li, W.; Tang, J.; Terry, R.N.; Li, S.; Brunie, A.; Callahan, R.L.; Noel, R.K.; Rodríguez, C.A.; Schwendeman, S.P.; Prausnitz, M.R. Long-acting reversible contraception by effervescent microneedle patch. Sci. Adv. 2023, 5, eaaw8145. [Google Scholar] [CrossRef]
- Tran, K.T.M.; Gavitt, T.D.; Farrell, N.J.; Curry, E.J.; Mara, A.B.; Patel, A.; Brown, L.; Kilpatrick, S.; Piotrowska, R.; Mishra, N.; et al. Transdermal microneedles for the programmable burst release of multiple vaccine payloads. Nat. Biomed. Eng. 2021, 5, 998–1007. [Google Scholar] [CrossRef]
- Eum, J.; Kim, Y.; Um, D.J.; Shin, J.; Yang, H.; Jung, H. Solvent-Free Polycaprolactone Dissolving Microneedles Generated via the Thermal Melting Method for the Sustained Release of Capsaicin. Micromachines 2021, 12, 167. [Google Scholar] [CrossRef]
- Sonetha, V.; Majumdar, S.; Shah, S. Step-wise micro-fabrication techniques of microneedle arrays with applications in transdermal drug delivery—A review. J. Drug Deliv. Sci. Technol. 2022, 68, 103119. [Google Scholar] [CrossRef]
- Zhao, L.; Mu, J.; Du, P.; Wang, H.; Mao, Y.; Xu, Y.; Xin, X.; Zang, F. Ultrasound-guided core needle biopsy in the diagnosis of neuroblastic tumors in children: A retrospective study on 83 cases. Pediatr. Surg. Int. 2017, 33, 347–353. [Google Scholar] [CrossRef]
- Yang, D.; Chen, M.; Sun, Y.; Jin, Y.; Lu, C.; Pan, X.; Quan, G.; Wu, C. Microneedle-mediated transdermal drug delivery for treating diverse skin diseases. Acta Biomater. 2021, 121, 119–133. [Google Scholar] [CrossRef]
- Sharma, S.; Hatware, K.; Bhadane, P.; Sindhikar, S.; Mishra, D.K. Recent advances in microneedle composites for biomedical applications: Advanced drug delivery technologies. Mater. Sci. Eng. C 2019, 103, 109717. [Google Scholar] [CrossRef]
- Turner, J.G.; White, L.R.; Estrela, P.; Leese, H.S. Hydrogel-Forming Microneedles: Current Advancements and Future Trends. Macromol. Biosci. 2021, 21, e2000307. [Google Scholar] [CrossRef] [PubMed]
- Aung, N.N.; Ngawhirunpat, T.; Rojanarata, T.; Patrojanasophon, P.; Pamornpathomkul, B.; Opanasopit, P. Fabrication, characterization and comparison of α-arbutin loaded dissolving and hydrogel forming microneedles. Int. J. Pharm. 2020, 586, 119508. [Google Scholar] [CrossRef]
- Lee, K.J.; Jeong, S.S.; Roh, D.H.; Kim, D.Y.; Choi, H.-K.; Lee, E.H. A practical guide to the development of microneedle systems—In clinical trials or on the market. Int. J. Pharm. 2020, 573, 118778. [Google Scholar] [CrossRef] [PubMed]
- Le, Z.; Yu, J.; Quek, Y.J.; Bai, B.; Li, X.; Shou, Y.; Myint, B.; Xu, C.; Tay, A. Design principles of microneedles for drug delivery and sampling applications. Mater. Today 2023, 63, 137–169. [Google Scholar] [CrossRef]
- Prausnitz, M.R.; Langer, R. Transdermal drug delivery. Nat. Biotechnol. 2008, 26, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Holbrook, K.A.; Odland, G.F. Regional Differences in the Thickness (Cell Layers) of the Human Stratum Corneum: An Ultrastructural Analysis. J. Investig. Dermatol. 1974, 62, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Planz, V.; Lehr, C.-M.; Windbergs, M. In vitro models for evaluating safety and efficacy of novel technologies for skin drug delivery. J. Control. Release 2016, 242, 89–104. [Google Scholar] [CrossRef] [PubMed]
- Verbaan, F.J.; Bal, S.M.; Van den Berg, D.J.; Groenink, W.H.H.; Verpoorten, H.; Lüttge, R.; Bouwstra, J.A. Assembled microneedle arrays enhance the transport of compounds varying over a large range of molecular weight across human dermatomed skin. J. Control. Release 2007, 117, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, R.F.; Garland, M.J.; Morrow, D.I.; Migalska, K.; Singh, T.R.R.; Majithiya, R.; Woolfson, A.D. Optical coherence tomography is a valuable tool in the study of the effects of microneedle geometry on skin penetration characteristics and in-skin dissolution. J. Control. Release 2010, 147, 333–341. [Google Scholar] [CrossRef]
- Davidson, A.; Al-Qallaf, B.; Das, D.B. Transdermal drug delivery by coated microneedles: Geometry effects on effective skin thickness and drug permeability. Chem. Eng. Res. Des. 2008, 86, 1196–1206. [Google Scholar] [CrossRef]
- Badran, M.; Kuntsche, J.; Fahr, A. Skin penetration enhancement by a microneedle device (Dermaroller®) in vitro: Dependency on needle size and applied formulation. Eur. J. Pharm. Sci. 2009, 36, 511–523. [Google Scholar] [CrossRef] [PubMed]
- Xiu, X.; Gao, G.; Liu, Y.; Ma, F. Drug delivery with dissolving microneedles: Skin puncture, its influencing factors and improvement strategies. J. Drug Deliv. Sci. Technol. 2022, 76, 103653. [Google Scholar] [CrossRef]
- Gill, H.S.; Denson, D.D.; Burris, B.A.B.; Prausnitz, M.R. Effect of Microneedle Design on Pain in Human Volunteers. Clin. J. Pain 2008, 24, 585–594. [Google Scholar] [CrossRef]
- Kochhar, J.S.; Quek, T.C.; Soon, W.J.; Choi, J.; Zou, S.; Kang, L. Effect of Microneedle Geometry and Supporting Substrate on Microneedle Array Penetration into Skin. J. Pharm. Sci. 2013, 102, 4100–4108. [Google Scholar] [CrossRef]
- Olatunji, O.; Das, D.B.; Garland, M.J.; Belaid, L.; Donnelly, R.F. Influence of Array Interspacing on the Force Required for Successful Microneedle Skin Penetration: Theoretical and Practical Approaches. J. Pharm. Sci. 2013, 102, 1209–1221. [Google Scholar] [CrossRef]
- Prausnitz, M.R. Microneedles for transdermal drug delivery. Adv. Drug Deliv. Rev. 2004, 56, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Davis, S.P.; Landis, B.J.; Adams, Z.H.; Allen, M.G.; Prausnitz, M.R. Insertion of microneedles into skin: Measurement and prediction of insertion force and needle fracture force. J. Biomech. 2004, 37, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Bal, S.M.; Kruithof, A.C.; Zwier, R.; Dietz, E.; Bouwstra, J.A.; Lademann, J.; Meinke, M.C. Influence of microneedle shape on the transport of a fluorescent dye into human skin in vivo. J. Control. Release 2010, 147, 218–224. [Google Scholar] [CrossRef]
- Park, J.-H.; Yoon, Y.-K.; Choi, S.-O.; Prausnitz, M.R.; Allen, M.G. Tapered Conical Polymer Microneedles Fabricated Using an Integrated Lens Technique for Transdermal Drug Delivery. IEEE Trans. Biomed. Eng. 2007, 54, 903–913. [Google Scholar] [CrossRef]
- Römgens, A.; Bader, D.; Bouwstra, J.; Baaijens, F.; Oomens, C. Monitoring the penetration process of single microneedles with varying tip diameters. J. Mech. Behav. Biomed. Mater. 2014, 40, 397–405. [Google Scholar] [CrossRef]
- Sabri, A.H.; Kim, Y.; Marlow, M.; Scurr, D.J.; Segal, J.; Banga, A.K.; Kagan, L.; Lee, J.B. Intradermal and transdermal drug delivery using microneedles—Fabrication, performance evaluation and application to lymphatic delivery. Adv. Drug Deliv. Rev. 2020, 153, 195–215. [Google Scholar] [CrossRef]
- Bao, L.; Park, J.; Bonfante, G.; Kim, B. Recent advances in porous microneedles: Materials, fabrication, and transdermal applications. Drug Deliv. Transl. Res. 2022, 12, 395–414. [Google Scholar] [CrossRef]
- Park, J.-H.; Prausnitz, M. Analysis of mechanical failure of polymer microneedles by axial force. J. Korean Phys. Soc. 2010, 56, 1223–1227. [Google Scholar] [CrossRef]
- Chang, K.-T.; Shen, Y.-K.; Fan, F.-Y.; Lin, Y.; Kang, S.-C. Optimal design and fabrication of a microneedle arrays patch. J. Manuf. Process. 2020, 54, 274–285. [Google Scholar] [CrossRef]
- Gittard, S.D.; Chen, B.; Xu, H.; Ovsianikov, A.; Chichkov, B.N.; Monteiro-Riviere, N.A.; Narayan, R.J. The effects of geometry on skin penetration and failure of polymer microneedles. J. Adhes. Sci. Technol. 2013, 27, 227–243. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Hu, X.; Dong, Z.; Chen, Y.; Zhao, W.; Wang, Y.; Zhang, L.; Chen, M.; Wu, C.; Wang, Q. Dissolving Microneedle Arrays with Optimized Needle Geometry for Transcutaneous Immunization. Eur. J. Pharm. Sci. 2020, 151, 105361. [Google Scholar] [CrossRef] [PubMed]
- Loizidou, E.Z.; Inoue, N.T.; Ashton-Barnett, J.; Barrow, D.A.; Allender, C.J. Evaluation of geometrical effects of microneedles on skin penetration by CT scan and finite element analysis. Eur. J. Pharm. Biopharm. 2016, 107, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Lyu, S.; Dong, Z.; Xu, X.; Bei, H.-P.; Yuen, H.-Y.; Cheung, C.-W.J.; Wong, M.-S.; He, Y.; Zhao, X. Going below and beyond the surface: Microneedle structure, materials, drugs, fabrication, and applications for wound healing and tissue regeneration. Bioact. Mater. 2023, 27, 303–326. [Google Scholar] [CrossRef] [PubMed]
- Aldawood, F.K.; Andar, A.; Desai, S. A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications. Polymers 2021, 13, 2815. [Google Scholar] [CrossRef] [PubMed]
- Bariya, S.H.; Gohel, M.C.; Mehta, T.A.; Sharma, O.P. Microneedles: An emerging transdermal drug delivery system. J. Pharm. Pharmacol. 2012, 64, 11–29. [Google Scholar] [CrossRef]
- Tucak, A.; Sirbubalo, M.; Hindija, L.; Rahić, O.; Hadžiabdić, J.; Muhamedagić, K.; Čekić, A.; Vranić, E. Microneedles: Characteristics, Materials, Production Methods and Commercial Development. Micromachines 2020, 11, 961. [Google Scholar] [CrossRef]
- Razali, A.R.; Qin, Y. A Review on Micro-manufacturing, Micro-forming and their Key Issues. Procedia Eng. 2013, 53, 665–672. [Google Scholar] [CrossRef]
- Nuxoll, E. BioMEMS in drug delivery. Adv. Drug Deliv. Rev. 2013, 65, 1611–1625. [Google Scholar] [CrossRef]
- Kathuria, H.; Kang, K.; Cai, J.; Kang, L. Rapid microneedle fabrication by heating and photolithography. Int. J. Pharm. 2020, 575, 118992. [Google Scholar] [CrossRef]
- Pérennès, F.; Marmiroli, B.; Matteucci, M.; Tormen, M.; Vaccari, L.; Di Fabrizio, E. Sharp beveled tip hollow microneedle arrays fabricated by LIGA and 3D soft lithography with polyvinyl alcohol. J. Micromech. Microeng. 2006, 16, 473–479. [Google Scholar] [CrossRef]
- Madou, M. Fundamentals Of Microfabrication and Nanotechnology, 1st ed.; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- Chaudhri, B.P.; Ceyssens, F.; Guan, T.; La Manna, A.; Neves, H.P.; Van Hoof, C.; Puers, R. High Strength, Polymer Microneedles for Transdermal Drug Delivery. Procedia Eng. 2011, 25, 1377–1380. [Google Scholar] [CrossRef][Green Version]
- Moon, S.J.; Lee, S.S.; Lee, H.S.; Kwon, T.H. Fabrication of microneedle array using LIGA and hot embossing process. Microsyst. Technol. 2005, 11, 311–318. [Google Scholar] [CrossRef]
- Takahashi, H.; Heo, Y.J.; Arakawa, N.; Kan, T.; Matsumoto, K.; Kawano, R.; Shimoyama, I. Scalable fabrication of microneedle arrays via spatially controlled UV exposure. Microsyst. Nanoeng. 2016, 2, 16049. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Heo, Y.J.; Shimoyama, I. Scalable Fabrication of PEGDA Microneedles Using UV Exposure via a Rotating Prism. J. Microelectromech. Syst. 2017, 26, 990–992. [Google Scholar] [CrossRef]
- Tomono, T. A new way to control the internal structure of microneedles: A case of chitosan lactate. Mater. Today Chem. 2019, 13, 79–87. [Google Scholar] [CrossRef]
- Dharadhar, S.; Majumdar, A.; Dhoble, S.; Patravale, V. Microneedles for transdermal drug delivery: A systematic review. Drug Dev. Ind. Pharm. 2019, 45, 188–201. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, R.F.; Singh, T.R.R.; Tunney, M.M.; Morrow, D.I.J.; McCarron, P.A.; O’Mahony, C.; Woolfson, A.D. Microneedle Arrays Allow Lower Microbial Penetration Than Hypodermic Needles In Vitro. Pharm. Res. 2009, 26, 2513–2522. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Li, Y.; Liu, M.; Cui, L.; Yu, Y. Microneedle Electrode Array for Electrical Impedance Myography to Characterize Neurogenic Myopathy. Ann. Biomed. Eng. 2016, 44, 1566–1575. [Google Scholar] [CrossRef]
- Li, Y.-C.; Feng, S.-J.; Chen, H.-X.; Chen, Z.-L.; Zhang, D.-M. Random vibration of train-track-ground system with a poroelastic interlayer in the subsoil. Soil Dyn. Earthq. Eng. 2019, 120, 1–11. [Google Scholar] [CrossRef]
- Wilke, N.; Mulcahy, A.; Ye, S.-R.; Morrissey, A. Process optimization and characterization of silicon microneedles fabricated by wet etch technology. Microelectron. J. 2005, 36, 650–656. [Google Scholar] [CrossRef]
- Liu, Y.; Eng, P.F.; Guy, O.J.; Roberts, K.; Ashraf, H.; Knight, N. Advanced deep reactive-ion etching technology for hollow microneedles for transdermal blood sampling and drug delivery. IET Nanobiotechnol. 2013, 7, 59–62. [Google Scholar] [CrossRef] [PubMed]
- Roxhed, N.; Gasser, T.C.; Griss, P.; Holzapfel, G.A.; Stemme, G. Penetration-Enhanced Ultrasharp Microneedles and Prediction on Skin Interaction for Efficient Transdermal Drug Delivery. J. Microelectromech. Syst. 2007, 16, 1429–1440. [Google Scholar] [CrossRef]
- Henry, S.; McAllister, D.V.; Allen, M.G.; Prausnitz, M.R. Microfabricated Microneedles: A Novel Approach to Transdermal Drug Delivery. J. Pharm. Sci. 1998, 87, 922–925. [Google Scholar] [CrossRef]
- Wang, P.-C.; Wester, B.A.; Rajaraman, S.; Paik, S.-J.; Kim, S.-H.; Allen, M.G. Hollow polymer microneedle array fabricated by photolithography process combined with micromolding technique. In Proceedings of the 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Minneapolis, MN, USA, 3–6 September 2009; pp. 7026–7029. [Google Scholar] [CrossRef]
- Paik, S.-J.; Byun, S.; Lim, J.-M.; Park, Y.; Lee, A.; Chung, S.; Chang, J.; Chun, K.; Cho, D. In-plane single-crystal-silicon microneedles for minimally invasive microfluid systems. Sens. Actuators A Phys. 2004, 114, 276–284. [Google Scholar] [CrossRef]
- Ma, B.; Liu, S.; Gan, Z.; Liu, G.; Cai, X.; Zhang, H.; Yang, Z. A PZT insulin pump integrated with a silicon microneedle array for transdermal drug delivery. Microfluidics Nanofluidics 2006, 2, 417–423. [Google Scholar] [CrossRef]
- Wang, J.; Wang, H.; Lai, L.; Li, Y. Preparation of Microneedle Array Mold Based on MEMS Lithography Technology. Micromachines 2021, 12, 23. [Google Scholar] [CrossRef]
- Chen, Z.; He, J.; Qi, J.; Zhu, Q.; Wu, W.; Lu, Y. Long-acting microneedles: A progress report of the state-of-the-art techniques. Drug Discov. Today 2020, 25, 1462–1468. [Google Scholar] [CrossRef]
- Ita, K. Ceramic microneedles and hollow microneedles for transdermal drug delivery: Two decades of research. J. Drug Deliv. Sci. Technol. 2018, 44, 314–322. [Google Scholar] [CrossRef]
- Chang, H.; Cui, Y. Image Classification Algorithm Based on Big Data and Multilabel Learning of Improved Convolutional Neural Network. Wirel. Commun. Mob. Comput. 2021, 2021, 3138398. [Google Scholar] [CrossRef]
- Boks, M.A.; Unger, W.W.; Engels, S.; Ambrosini, M.; van Kooyk, Y.; Luttge, R. Controlled release of a model vaccine by nanoporous ceramic microneedle arrays. Int. J. Pharm. 2015, 491, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Bystrova, S.; Luttge, R. Micromolding for ceramic microneedle arrays. Microelectron. Eng. 2011, 88, 1681–1684. [Google Scholar] [CrossRef]
- Yuan, W.; Yang, S.; Feng, Y.; Zhang, L.; Chen, N.; Jin, T. A scalable fabrication process of polymer microneedles. Int. J. Nanomed. 2012, 7, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Jiang, G.; Yu, W.; Liu, D.; Xu, B. Microneedles fabricated from alginate and maltose for transdermal delivery of insulin on diabetic rats. Mater. Sci. Eng. C 2018, 85, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Allen, M.G.; Prausnitz, M.R. Biodegradable polymer microneedles: Fabrication, mechanics and transdermal drug delivery. J. Control. Release 2005, 104, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, D.-H.; Lee, K.J.; Seo, I.H.; Park, S.H.; Jang, E.H.; Park, Y.; Youn, Y.-N.; Ryu, W. Transfer-molded wrappable microneedle meshes for perivascular drug delivery. J. Control. Release 2017, 268, 237–246. [Google Scholar] [CrossRef]
- Moga, K.A.; Bickford, L.R.; Geil, R.D.; Dunn, S.S.; Pandya, A.A.; Wang, Y.; Fain, J.H.; Archuleta, C.F.; O’Neill, A.T.; DeSimone, J.M. Rapidly–Dissolvable Microneedle Patches Via a Highly Scalable and Reproducible Soft Lithography Approach. Adv. Mater. 2013, 25, 5060–5066. [Google Scholar] [CrossRef]
- Lee, M.-T.; Lee, I.-C.; Tsai, S.-W.; Chen, C.-H.; Wu, M.-H.; Juang, Y.-J. Spin coating of polymer solution on polydimethylsiloxane mold for fabrication of microneedle patch. J. Taiwan Inst. Chem. Eng. 2017, 70, 42–48. [Google Scholar] [CrossRef]
- McGrath, M.G.; Vucen, S.; Vrdoljak, A.; Kelly, A.; O’mahony, C.; Crean, A.M.; Moore, A. Production of dissolvable microneedles using an atomised spray process: Effect of microneedle composition on skin penetration. Eur. J. Pharm. Biopharm. 2014, 86, 200–211. [Google Scholar] [CrossRef]
- Vrdoljak, A.; Allen, E.A.; Ferrara, F.; Temperton, N.J.; Crean, A.M.; Moore, A.C. Induction of broad immunity by thermostabilised vaccines incorporated in dissolvable microneedles using novel fabrication methods. J. Control. Release 2016, 225, 192–204. [Google Scholar] [CrossRef]
- Kim, M.J.; Park, S.C.; Rizal, B.; Guanes, G.; Baek, S.-K.; Park, J.-H.; Betz, A.R.; Choi, S.-O. Fabrication of Circular Obelisk-Type Multilayer Microneedles Using Micro-Milling and Spray Deposition. Front. Bioeng. Biotechnol. 2018, 6, 54. [Google Scholar] [CrossRef] [PubMed]
- Gill, H.S.; Prausnitz, M.R. Coated microneedles for transdermal delivery. J. Control. Release 2007, 117, 227–237. [Google Scholar] [CrossRef]
- Martanto, W.; Davis, S.P.; Holiday, N.R.; Wang, J.; Gill, H.S.; Prausnitz, M.R. Transdermal Delivery of Insulin Using Microneedles in Vivo. Pharm. Res. 2004, 21, 947–952. [Google Scholar] [CrossRef] [PubMed]
- Gill, H.S.; Prausnitz, M.R. Coating Formulations for Microneedles. Pharm. Res. 2007, 24, 1369–1380. [Google Scholar] [CrossRef]
- Indermun, S.; Luttge, R.; Choonara, Y.E.; Kumar, P.; du Toit, L.C.; Modi, G.; Pillay, V. Current advances in the fabrication of microneedles for transdermal delivery. J. Control. Release 2014, 185, 130–138. [Google Scholar] [CrossRef]
- Nagarkar, R.; Singh, M.; Nguyen, H.X.; Jonnalagadda, S. A review of recent advances in microneedle technology for transdermal drug delivery. J. Drug Deliv. Sci. Technol. 2020, 59, 101923. [Google Scholar] [CrossRef]
- Omatsu, T.; Chujo, K.; Miyamoto, K.; Okida, M.; Nakamura, K.; Aoki, N.; Morita, R. Metal microneedle fabrication using twisted light with spin. Opt. Express 2010, 18, 17967–17973. [Google Scholar] [CrossRef]
- Evens, T.; Malek, O.; Castagne, S.; Seveno, D.; Van Bael, A. A novel method for producing solid polymer microneedles using laser ablated moulds in an injection moulding process. Manuf. Lett. 2020, 24, 29–32. [Google Scholar] [CrossRef]
- Aoyagi, S.; Izumi, H.; Isono, Y.; Fukuda, M.; Ogawa, H. Laser fabrication of high aspect ratio thin holes on biodegradable polymer and its application to a microneedle. Sens. Actuators A Phys. 2007, 139, 293–302. [Google Scholar] [CrossRef]
- Albarahmieh, E.; AbuAmmouneh, L.; Kaddoura, Z.; AbuHantash, F.; Alkhalidi, B.A.; Al-Halhouli, A. Fabrication of Dissolvable Microneedle Patches Using an Innovative Laser-Cut Mould Design to Shortlist Potentially Transungual Delivery Systems: In Vitro Evaluation. AAPS PharmSciTech 2019, 20, 215. [Google Scholar] [CrossRef]
- Nejad, H.R.; Sadeqi, A.; Kiaee, G.; Sonkusale, S. Low-cost and cleanroom-free fabrication of microneedles. Microsyst. Nanoeng. 2018, 4, 17073. [Google Scholar] [CrossRef]
- Tu, K.T.; Chung, C.K. Rapid prototyping of biodegradable microneedle arrays by integrating CO2 laser processing and polymer molding. J. Micromech. Microeng. 2016, 26, 65015. [Google Scholar] [CrossRef]
- Demir, Y.K.; Akan, Z.; Kerimoglu, O. Characterization of Polymeric Microneedle Arrays for Transdermal Drug Delivery. PLoS ONE 2013, 8, e77289. [Google Scholar] [CrossRef]
- Anbazhagan, G.; Suseela, S.B.; Sankararajan, R. Design, analysis and fabrication of solid polymer microneedle patch using CO2 laser and polymer molding. Drug Deliv. Transl. Res. 2023, 13, 1813–1827. [Google Scholar] [CrossRef]
- Adarkwa, E.; Desai, S. Scalable Droplet Based Manufacturing Using In-Flight Laser Evaporation. J. Nanoeng. Nanomanuf. 2016, 6, 87–92. [Google Scholar] [CrossRef]
- Yang, M.; Xu, Z.; Desai, S.; Kumar, D.; Sankar, J. Fabrication of Micro Single Chamber Solid Oxide Fuel Cell Using Photolithography and Pulsed Laser Deposition. J. Fuel Cell Sci. Technol. 2015, 12, 021004. [Google Scholar] [CrossRef]
- Esho, T.; Desai, S. Laser based microdroplet evaporation towards scalable micro and nano manufacturing. In Proceedings of the 62nd IIE Annual Conference and Expo, Orlando, FL, USA, 19–23 May 2012; pp. 1750–1757. [Google Scholar]
- Parupelli, S.K.; Desai, S. Understanding Hybrid Additive Manufacturing of Functional Devices. Am. J. Eng. Appl. Sci. 2017, 10, 264–271. [Google Scholar] [CrossRef][Green Version]
- McKenzie, J.; Desai, S. Investigating Sintering Mechanisms for Additive Manufacturing of Conductive Traces. Am. J. Eng. Appl. Sci. 2018, 11, 652–662. [Google Scholar] [CrossRef]
- Desai, S.; Craps, M.; Esho, T. Direct writing of nanomaterials for flexible thin-film transistors (fTFTs). Int. J. Adv. Manuf. Technol. 2013, 64, 537–543. [Google Scholar] [CrossRef]
- Ahmed, M.; El-Naggar, M.E.; Aldalbahi, A.; El-Newehy, M.H.; Menazea, A. Methylene blue degradation under visible light of metallic nanoparticles scattered into graphene oxide using laser ablation technique in aqueous solutions. J. Mol. Liq. 2020, 315, 113794. [Google Scholar] [CrossRef]
- Ismail, A.; El-Newehy, M.H.; El-Naggar, M.E.; Moydeen, A.M.; Menazea, A. Enhancement the electrical conductivity of the synthesized polyvinylidene fluoride/polyvinyl chloride composite doped with palladium nanoparticles via laser ablation. J. Mater. Res. Technol. 2020, 9, 11178–11188. [Google Scholar] [CrossRef]
- Menazea, A.; El-Newehy, M.H.; Thamer, B.M.; El-Naggar, M.E. Preparation of antibacterial film-based biopolymer embedded with vanadium oxide nanoparticles using one-pot laser ablation. J. Mol. Struct. 2021, 1225, 129163. [Google Scholar] [CrossRef]
- Tu, K.-T.; Chung, C.-K. Fabrication of biodegradable polymer microneedle array via CO2 laser ablation. In Proceedings of the 2015 IEEE 10th International Conference on Nano/Micro Engineered and Molecular Systems (NEMS), Xi’an, China, 7–11 April 2015; pp. 494–497. [Google Scholar] [CrossRef]
- Chen, Y.-T.; Ma, K.-J.; Tseng, A.A.; Chen, P. Projection ablation of glass-based single and arrayed microstructures using excimer laser. Opt. Laser Technol. 2005, 37, 271–280. [Google Scholar] [CrossRef]
- Zheng, H.; Lam, Y.; Sundarraman, C.; Tran, D. Influence of substrate cooling on femtosecond laser machined hole depth and diameter. Appl. Phys. A 2007, 89, 559–563. [Google Scholar] [CrossRef]
- Lutton, R.E.; Larrañeta, E.; Kearney, M.-C.; Boyd, P.; Woolfson, A.; Donnelly, R.F. A novel scalable manufacturing process for the production of hydrogel-forming microneedle arrays. Int. J. Pharm. 2015, 494, 417–429. [Google Scholar] [CrossRef] [PubMed]
- Zaied, M.; Miraoui, I.; Boujelbene, M.; Bayraktar, E. Analysis of heat affected zone obtained by CO2 laser cutting of low carbon steel (S235). In AIP Conference Proceedings; American Institute of Physics: College Park, MD, USA, 2013. [Google Scholar] [CrossRef]
- Wang, Q.L.; Zhu, D.D.; Chen, Y.; Guo, X.D. A fabrication method of microneedle molds with controlled microstructures. Mater. Sci. Eng. C 2016, 65, 135–142. [Google Scholar] [CrossRef]
- Chen, B.Z.; He, M.C.; Zhang, X.P.; Fei, W.M.; Cui, Y.; Guo, X.D. A novel method for fabrication of coated microneedles with homogeneous and controllable drug dosage for transdermal drug delivery. Drug Deliv. Transl. Res. 2022, 12, 2730–2739. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.M.; Cornwell, M.; Hill, J.; Prausnitz, M.R. Precise Microinjection into Skin Using Hollow Microneedles. J. Investig. Dermatol. 2006, 126, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Gupta, J.; Felner, E.I.; Prausnitz, M.R. Rapid Pharmacokinetics of Intradermal Insulin Administered Using Microneedles in Type 1 Diabetes Subjects. Diabetes Technol. Ther. 2011, 13, 451–456. [Google Scholar] [CrossRef]
- Martanto, W.; Moore, J.S.; Kashlan, O.; Kamath, R.; Wang, P.M.; O’Neal, J.M.; Prausnitz, M.R. Microinfusion Using Hollow Microneedles. Pharm. Res. 2006, 23, 104–113. [Google Scholar] [CrossRef]
- Mahadevan, G.; Sheardown, H.; Selvaganapathy, P. PDMS embedded microneedles as a controlled release system for the eye. J. Biomater. Appl. 2012, 28, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.D.; Kim, M.; Yang, H.; Lee, K.; Jung, H. Droplet-born air blowing: Novel dissolving microneedle fabrication. J. Control. Release 2013, 170, 430–436. [Google Scholar] [CrossRef]
- Wu, M.; Zhang, Y.; Huang, H.; Li, J.; Liu, H.; Guo, Z.; Xue, L.; Liu, S.; Lei, Y. Assisted 3D printing of microneedle patches for minimally invasive glucose control in diabetes. Mater. Sci. Eng. C 2020, 117, 111299. [Google Scholar] [CrossRef]
- Kim, J.D.; Bae, J.-H.; Kim, H.K.; Jeong, D.H. Droplet-born Air Blowing (DAB) Technology for the Industrialization of Dissolving Microneedle. In Proceedings of the World Congress on Recent Advances in Nanotechnology, Prague, Czech Republic, 1–2 April 2016. [Google Scholar] [CrossRef]
- Wu, L.; Takama, N.; Park, J.; Kim, B.; Kim, J.; Jeong, D. Shadow mask assisted droplet-born air-blowing method for fabrication of dissoluble microneedle. In Proceedings of the 2017 IEEE 12th International Conference on Nano/Micro Engineered and Molecular Systems (NEMS), Los Angeles, CA, USA, 9–12 April 2017; pp. 456–459. [Google Scholar]
- Lin, Y.-H.; Lee, I.-C.; Hsu, W.-C.; Hsu, C.-H.; Chang, K.-P.; Gao, S.-S. Rapid fabrication method of a microneedle mold with controllable needle height and width. Biomed. Microdevices 2016, 18, 85. [Google Scholar] [CrossRef]
- Vecchione, R.; Coppola, S.; Esposito, E.; Casale, C.; Vespini, V.; Grilli, S.; Ferraro, P.; Netti, P.A. Electro-Drawn Drug-Loaded Biodegradable Polymer Microneedles as a Viable Route to Hypodermic Injection. Adv. Funct. Mater. 2014, 24, 3515–3523. [Google Scholar] [CrossRef]
- Lee, S.; Fakhraei Lahiji, S.; Jang, J.; Jang, M.; Jung, H. Micro-Pillar Integrated Dissolving Microneedles for Enhanced Transdermal Drug Delivery. Pharmaceutics 2019, 11, 402. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Park, S.C.; Choi, S.-O. Dual-nozzle spray deposition process for improving the stability of proteins in polymer microneedles. RSC Adv. 2017, 7, 55350–55359. [Google Scholar] [CrossRef]
- Juster, H.; van der Aar, B.; de Brouwer, H. A review on microfabrication of thermoplastic polymer-based microneedle arrays. Polym. Eng. Sci. 2019, 59, 877–890. [Google Scholar] [CrossRef]
- Lhernould, M.S.; Deleers, M.; Delchambre, A. Hollow polymer microneedles array resistance and insertion tests. Int. J. Pharm. 2015, 480, 152–157. [Google Scholar] [CrossRef]
- Nair, K.J. Micro-Injection Molded Microneedles for Drug Delivery. Ph.D. Thesis, University of Bradford, Bradford, UK, 2016. [Google Scholar]
- Sammoura, F.; Kang, J.; Heo, Y.-M.; Jung, T.; Lin, L. Polymeric microneedle fabrication using a microinjection molding technique. Microsyst. Technol. 2007, 13, 517–522. [Google Scholar] [CrossRef]
- Bediz, B.; Korkmaz, E.; Khilwani, R.; Donahue, C.; Erdos, G.; Falo, L.D.; Ozdoganlar, O.B. Dissolvable Microneedle Arrays for Intradermal Delivery of Biologics: Fabrication and Application. Pharm. Res. 2014, 31, 117–135. [Google Scholar] [CrossRef] [PubMed]
- Malek-Khatabi, A.; Rad, Z.F.; Rad-Malekshahi, M.; Akbarijavar, H. Development of dissolvable microneedle patches by CNC machining and micromolding for drug delivery. Mater. Lett. 2023, 330, 133328. [Google Scholar] [CrossRef]
- García-López, E.; Siller, H.R.; Rodríguez, C.A. Study of the fabrication of AISI 316L microneedle arrays. Procedia Manuf. 2018, 26, 117–124. [Google Scholar] [CrossRef]
- Parupelli, S.K.; Desai, S. A Comprehensive Review of Additive Manufacturing (3D Printing): Processes, Applications and Future Potential. Am. J. Appl. Sci. 2019, 16, 244–272. [Google Scholar] [CrossRef]
- Adarkwa, E.; Kotoka, R.; Desai, S. 3D printing of polymeric Coatings on AZ31 Mg alloy Substrate for Corrosion Protection of biomedical implants. Med. Devices Sens. 2021, 4, e10167. [Google Scholar] [CrossRef]
- Altubaishe, B.; Clarke, J.; McWilliams, C.; Desai, S. Comparative Analysis of Risk Management Strategies for Additive Manufacturing Supply Chains. Am. J. Appl. Sci. 2019, 16, 273–282. [Google Scholar] [CrossRef]
- Aldawood, F.K.; Chang, S.X.; Desai, S. Design and manufacture of a high precision personalized electron bolus device for radiation therapy. Med. Devices Sens. 2020, 3, e10077. [Google Scholar] [CrossRef]
- Haeberle, G.; Desai, S. Investigating Rapid Thermoform Tooling Via Additive Manufacturing (3D Printing). Am. J. Appl. Sci. 2019, 16, 238–243. [Google Scholar] [CrossRef]
- Parupelli, S.K.; Desai, S. Hybrid additive manufacturing (3D printing) and characterization of functionally gradient materials via in situ laser curing. Int. J. Adv. Manuf. Technol. 2020, 110, 543–556. [Google Scholar] [CrossRef]
- Economidou, S.N.; Lamprou, D.A.; Douroumis, D. 3D printing applications for transdermal drug delivery. Int. J. Pharm. 2018, 544, 415–424. [Google Scholar] [CrossRef]
- Alhnan, M.A.; Okwuosa, T.C.; Sadia, M.; Wan, K.-W.; Ahmed, W.; Arafat, B. Emergence of 3D Printed Dosage Forms: Opportunities and Challenges. Pharm. Res. 2016, 33, 1817–1832. [Google Scholar] [CrossRef] [PubMed]
- Jamróz, W.; Szafraniec, J.; Kurek, M.; Jachowicz, R. 3D Printing in Pharmaceutical and Medical Applications—Recent Achievements and Challenges. Pharm. Res. 2018, 35, 176. [Google Scholar] [CrossRef] [PubMed]
- Prasad, L.K.; Smyth, H. 3D Printing technologies for drug delivery: A review. Drug Dev. Ind. Pharm. 2016, 42, 1019–1031. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.H.; Kathuria, H.; Tan, J.J.Y.; Kang, L. 3D printed drug delivery and testing systems—A passing fad or the future? Adv. Drug Deliv. Rev. 2018, 132, 139–168. [Google Scholar] [CrossRef] [PubMed]
- Goole, J.; Amighi, K. 3D printing in pharmaceutics: A new tool for designing customized drug delivery systems. Int. J. Pharm. 2016, 499, 376–394. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.; Trenfield, S.J.; Gaisford, S.; Basit, A.W. 3D printed medicines: A new branch of digital healthcare. Int. J. Pharm. 2018, 548, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Camović, M.; Biščević, A.; Brčić, I.; Borčak, K.; Bušatlić, S.; Ćenanović, N.; Dedović, A.; Mulalić, A.; Osmanlić, M.; Sirbubalo, M.; et al. Coated 3D Printed PLA Microneedles as Transdermal Drug Delivery Systems. In Proceedings of the International Conference on Medical and Biological Engineering, Banja Luka, Bosnia and Herzegovina, 16–18 May 2019; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; pp. 735–742. [Google Scholar] [CrossRef]
- Luzuriaga, M.A.; Berry, D.R.; Reagan, J.C.; Smaldone, R.A.; Gassensmith, J.J. Biodegradable 3D printed polymer microneedles for transdermal drug delivery. Lab Chip 2018, 18, 1223–1230. [Google Scholar] [CrossRef] [PubMed]
- Allen, E.A.; O’mahony, C.; Cronin, M.; O’mahony, T.; Moore, A.C.; Crean, A.M. Dissolvable microneedle fabrication using piezoelectric dispensing technology. Int. J. Pharm. 2016, 500, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Derakhshandeh, H.; Aghabaglou, F.; McCarthy, A.; Mostafavi, A.; Wiseman, C.; Bonick, Z.; Ghanavati, I.; Harris, S.; Kreikemeier-Bower, C.; Basri, S.M.M.; et al. A Wirelessly Controlled Smart Bandage with 3D-Printed Miniaturized Needle Arrays. Adv. Funct. Mater. 2020, 30, 1905544. [Google Scholar] [CrossRef]
- Barnum, L.; Quint, J.; Derakhshandeh, H.; Samandari, M.; Aghabaglou, F.; Farzin, A.; Abbasi, L.; Bencherif, S.; Memic, A.; Mostafalu, P.; et al. 3D-Printed Hydrogel-Filled Microneedle Arrays. Adv. Health Mater. 2021, 10, 2001922. [Google Scholar] [CrossRef]
- Yeung, C.; Chen, S.; King, B.; Lin, H.; King, K.; Akhtar, F.; Diaz, G.; Wang, B.; Zhu, J.; Sun, W.; et al. A 3D-printed microfluidic-enabled hollow microneedle architecture for transdermal drug delivery. Biomicrofluidics 2019, 13, 064125. [Google Scholar] [CrossRef]
- Uddin, J.; Scoutaris, N.; Economidou, S.N.; Giraud, C.; Chowdhry, B.Z.; Donnelly, R.F.; Douroumis, D. 3D printed microneedles for anticancer therapy of skin tumours. Mater. Sci. Eng. C 2020, 107, 110248. [Google Scholar] [CrossRef]
- Economidou, S.N.; Pere, C.P.P.; Reid, A.; Uddin, J.; Windmill, J.F.; Lamprou, D.A.; Douroumis, D. 3D printed microneedle patches using stereolithography (SLA) for intradermal insulin delivery. Mater. Sci. Eng. C 2019, 102, 743–755. [Google Scholar] [CrossRef]
- Krieger, K.J.; Bertollo, N.; Dangol, M.; Sheridan, J.T.; Lowery, M.M.; O’cearbhaill, E.D. Simple and customizable method for fabrication of high-aspect ratio microneedle molds using low-cost 3D printing. Microsyst. Nanoeng. 2019, 5, 42. [Google Scholar] [CrossRef] [PubMed]
- Farias, C.; Lyman, R.; Hemingway, C.; Chau, H.; Mahacek, A.; Bouzos, E.; Mobed-Miremadi, M. Three-Dimensional (3D) Printed Microneedles for Microencapsulated Cell Extrusion. Bioengineering 2018, 5, 59. [Google Scholar] [CrossRef]
- Xenikakis, I.; Tzimtzimis, M.; Tsongas, K.; Andreadis, D.; Demiri, E.; Tzetzis, D.; Fatouros, D.G. Fabrication and finite element analysis of stereolithographic 3D printed microneedles for transdermal delivery of model dyes across human skin in vitro. Eur. J. Pharm. Sci. 2019, 137, 104976. [Google Scholar] [CrossRef] [PubMed]
- Gittard, S.D.; Miller, P.R.; Jin, C.; Martin, T.N.; Boehm, R.D.; Chisholm, B.J.; Stafslien, S.J.; Daniels, J.W.; Cilz, N.; Monteiro-Riviere, N.A.; et al. Deposition of antimicrobial coatings on microstereolithography-fabricated microneedles. JOM 2011, 63, 59–68. [Google Scholar] [CrossRef]
- Lu, Y.; Mantha, S.N.; Crowder, D.C.; Chinchilla, S.; Shah, K.N.; Yun, Y.H.; Wicker, R.B.; Choi, J.-W. Microstereolithography and characterization of poly(propylene fumarate)-based drug-loaded microneedle arrays. Biofabrication 2015, 7, 045001. [Google Scholar] [CrossRef]
- El-Sayed, N.; Vaut, L.; Schneider, M. Customized fast-separable microneedles prepared with the aid of 3D printing for nanoparticle delivery. Eur. J. Pharm. Biopharm. 2020, 154, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.H.; Tiew, W.J.; Zhang, J.; Ho, P.C.-L.; Kachouie, N.N.; Kang, L. Geometrical optimisation of a personalised microneedle eye patch for transdermal delivery of anti-wrinkle small peptide. Biofabrication 2020, 12, 035003. [Google Scholar] [CrossRef]
- Johnson, A.R.; Caudill, C.L.; Tumbleston, J.R.; Bloomquist, C.J.; Moga, K.A.; Ermoshkin, A.; Shirvanyants, D.; Mecham, S.J.; Luft, J.C.; DeSimone, J.M. Single-Step Fabrication of Computationally Designed Microneedles by Continuous Liquid Interface Production. PLoS ONE 2016, 11, e0162518. [Google Scholar] [CrossRef] [PubMed]
- Caudill, C.; Perry, J.L.; Iliadis, K.; Tessema, A.T.; Lee, B.J.; Mecham, B.S.; Tian, S.; DeSimone, J.M. Transdermal vaccination via 3D-printed microneedles induces potent humoral and cellular immunity. Proc. Natl. Acad. Sci. USA 2021, 118, e2102595118. [Google Scholar] [CrossRef] [PubMed]
- Gittard, S.D.; Ovsianikov, A.; Chichkov, B.N.; Doraiswamy, A.; Narayan, R.J. Two-photon polymerization of microneedles for transdermal drug delivery. Expert Opin. Drug Deliv. 2010, 7, 513–533. [Google Scholar] [CrossRef] [PubMed]
- Trautmann, A.; Roth, G.-L.; Nujiqi, B.; Walther, T.; Hellmann, R. Towards a versatile point-of-care system combining femtosecond laser generated microfluidic channels and direct laser written microneedle arrays. Microsyst. Nanoeng. 2019, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Aksit, A.; Arteaga, D.N.; Arriaga, M.; Wang, X.; Watanabe, H.; Kasza, K.E.; Lalwani, A.K.; Kysar, J.W. In-vitro perforation of the round window membrane via direct 3-D printed microneedles. Biomed. Microdevices 2018, 20, 47. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Park, J.; Kamaki, Y.; Kim, B. Optimization of the fused deposition modeling-based fabrication process for polylactic acid microneedles. Microsyst. Nanoeng. 2021, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Antonara, L.; Dallas, P.P.; Rekkas, D.M. A novel 3D printing enabled method for fast and reliable construction of polymeric microneedles using experimental design. J. Drug Deliv. Sci. Technol. 2022, 68, 102888. [Google Scholar] [CrossRef]
- Loh, J.M.; Lim, Y.J.L.; Tay, J.T.; Cheng, H.M.; Tey, H.L.; Liang, K. Design and fabrication of customizable microneedles enabled by 3D printing for biomedical applications. Bioact. Mater. 2024, 32, 222–241. [Google Scholar] [CrossRef] [PubMed]
- Uddin, J.; Scoutaris, N.; Klepetsanis, P.; Chowdhry, B.; Prausnitz, M.R.; Douroumis, D. Inkjet printing of transdermal microneedles for the delivery of anticancer agents. Int. J. Pharm. 2015, 494, 593–602. [Google Scholar] [CrossRef]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.Q.; Hui, D. Additive Manufacturing (3D Printing): A Review of Materials, Methods, Applications and Challenges. Compos. Part B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Yadav, V.; Sharma, P.K.; Murty, U.S.; Mohan, N.H.; Thomas, R.; Dwivedy, S.K.; Banerjee, S. 3D printed hollow microneedles array using stereolithography for efficient transdermal delivery of rifampicin. Int. J. Pharm. 2021, 605, 120815. [Google Scholar] [CrossRef] [PubMed]
- Choo, S.; Jin, S.; Jung, J. Fabricating High-Resolution and High-Dimensional Microneedle Mold through the Resolution Improvement of Stereolithography 3D Printing. Pharmaceutics 2022, 14, 766. [Google Scholar] [CrossRef] [PubMed]
- Vinayakumar, K.B.; Silva, M.D.; Martins, A.; Mundy, S.; González-Losada, P.; Sillankorva, S. Levofloxacin-Loaded Microneedles Produced Using 3D-Printed Molds for Klebsiella Pneumoniae Biofilm Control. Adv. Ther. 2023, 6, 2200320. [Google Scholar] [CrossRef]
- Yang, Q.; Zhong, W.; Liu, Y.; Hou, R.; Wu, Y.; Yan, Q.; Yang, G. 3D-printed morphology-customized microneedles: Understanding the correlation between their morphologies and the received qualities. Int. J. Pharm. 2023, 638, 122873. [Google Scholar] [CrossRef]
- Turner, J.G.; Laabei, M.; Li, S.; Estrela, P.; Leese, H.S. Antimicrobial releasing hydrogel forming microneedles. Mater. Sci. Eng. C 2023, 151, 213467. [Google Scholar] [CrossRef]
- Yao, W.; Li, D.; Zhao, Y.; Zhan, Z.; Jin, G.; Liang, H.; Yang, R. 3D Printed Multi-Functional Hydrogel Microneedles Based on High-Precision Digital Light Processing. Micromachines 2020, 11, 17. [Google Scholar] [CrossRef]
- Mathew, E.; Pitzanti, G.; dos Santos, A.L.G.; Lamprou, D.A. Optimization of Printing Parameters for Digital Light Processing 3D Printing of Hollow Microneedle Arrays. Pharmaceutics 2021, 13, 1837. [Google Scholar] [CrossRef]
- Shin, D.; Hyun, J. Silk fibroin microneedles fabricated by digital light processing 3D printing. J. Ind. Eng. Chem. 2021, 95, 126–133. [Google Scholar] [CrossRef]
- Sachan, R.; Nguyen, A.K.; Lu, J.; Erdmann, D.; Zhang, J.Y.; Narayan, R.J. Digital light processing-based 3D printing of polytetrafluoroethylene solid microneedle arrays. MRS Commun. 2021, 11, 896–901. [Google Scholar] [CrossRef]
- Wu, X.; Sun, Q.; Qiao, W.; Cui, J.; Chen, L. Rapid fabrication of customizable microneedle molds using digital light processing 3D printing methods. In Proceedings of the First Optics Frontier Conference, Hangzhou, China, 18 June 2021; p. 118500N. [Google Scholar] [CrossRef]
- Monou, P.K.; Andriotis, E.G.; Tsongas, K.; Tzimtzimis, E.K.; Katsamenis, O.L.; Tzetzis, D.; Anastasiadou, P.; Ritzoulis, C.; Vizirianakis, I.S.; Andreadis, D.; et al. Fabrication of 3D Printed Hollow Microneedles by Digital Light Processing for the Buccal Delivery of Actives. ACS Biomater. Sci. Eng. 2023, 9, 5072–5083. [Google Scholar] [CrossRef]
- Erkus, H.; Bedir, T.; Kaya, E.; Tinaz, G.B.; Gunduz, O.; Chifiriuc, M.-C.; Ustundag, C.B. Innovative transdermal drug delivery system based on amoxicillin-loaded gelatin methacryloyl microneedles obtained by 3D printing. Materialia 2023, 27, 101700. [Google Scholar] [CrossRef]
- Lee, B.J.; Hsiao, K.; Lipkowitz, G.; Samuelsen, T.; Tate, L.; DeSimone, J.M. Characterization of a 30 µm pixel size CLIP-based 3D printer and its enhancement through dynamic printing optimization. Addit. Manuf. 2022, 55, 102800. [Google Scholar] [CrossRef]
- Rajesh, N.U.; Coates, I.; Driskill, M.M.; Dulay, M.T.; Hsiao, K.; Ilyin, D.; Jacobson, G.B.; Kwak, J.W.; Lawrence, M.; Perry, J.; et al. 3D-Printed Microarray Patches for Transdermal Applications. JACS Au 2022, 2, 2426–2445. [Google Scholar] [CrossRef] [PubMed]
- Doraiswamy, A.; Jin, C.; Narayan, R.; Mageswaran, P.; Mente, P.; Modi, R.; Auyeung, R.; Chrisey, D.; Ovsianikov, A.; Chichkov, B. Two photon induced polymerization of organic–inorganic hybrid biomaterials for microstructured medical devices. Acta Biomater. 2006, 2, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Rad, Z.F.; Prewett, P.D.; Davies, G.J. Rapid prototyping and customizable microneedle design: Ultra-sharp microneedle fabrication using two-photon polymerization and low-cost micromolding techniques. Manuf. Lett. 2021, 30, 39–43. [Google Scholar] [CrossRef]
- Pillai, M.M.; Ajesh, S.; Tayalia, P. Two-photon polymerization based reusable master template to fabricate polymer microneedles for drug delivery. MethodsX 2023, 10, 102025. [Google Scholar] [CrossRef] [PubMed]
- Fakeih, E.; Aguirre-Pablo, A.A.; Thoroddsen, S.T.; Salama, K.N. Fabrication and Characterization of Porous Microneedles for Enhanced Fluid Injection and Suction: A Two-Photon Polymerization Approach. Adv. Eng. Mater. 2023, 25, 2300161. [Google Scholar] [CrossRef]
- He, Z.; Chen, F.; He, S. Fabrication of microneedles using two photon-polymerization with low numerical aperture. Opt. Commun. 2024, 553, 130093. [Google Scholar] [CrossRef]
- Economidou, S.N.; Uddin, J.; Marques, M.J.; Douroumis, D.; Sow, W.T.; Li, H.; Reid, A.; Windmill, J.F.; Podoleanu, A. A novel 3D printed hollow microneedle microelectromechanical system for controlled, personalized transdermal drug delivery. Addit. Manuf. 2021, 38, 101815. [Google Scholar] [CrossRef]
- Rodgers, A.M.; McCrudden, M.T.C.; Vincente-Perez, E.M.; Dubois, A.V.; Ingram, R.J.; Larrañeta, E.; Kissenpfennig, A.; Donnelly, R.F. Design and characterisation of a dissolving microneedle patch for intradermal vaccination with heat-inactivated bacteria: A proof of concept study. Int. J. Pharm. 2018, 549, 87–95. [Google Scholar] [CrossRef]
- Boopathy, A.V.; Mandal, A.; Kulp, D.W.; Menis, S.; Bennett, N.R.; Watkins, H.C.; Wang, W.; Martin, J.T.; Thai, N.T.; He, Y.; et al. Enhancing humoral immunity via sustained-release implantable microneedle patch vaccination. Proc. Natl. Acad. Sci. USA 2019, 116, 16473–16478. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kim, Y.-C. Topical delivery of 5-fluorouracil-loaded carboxymethyl chitosan nanoparticles using microneedles for keloid treatment. Drug Deliv. Transl. Res. 2020, 11, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Sun, B.; Guo, J.; Wang, M.; Cui, H.; Mao, H.; Wang, B.; Yan, F. Active pharmaceutical ingredient poly(ionic liquid)-based microneedles for the treatment of skin acne infection. Acta Biomater. 2021, 115, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Ning, X.; Wiraja, C.; Chew, W.T.S.; Fan, C.; Xu, C. Transdermal delivery of Chinese herbal medicine extract using dissolvable microneedles for hypertrophic scar treatment. Acta Pharm. Sin. B 2021, 11, 2937–2944. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Hu, X.; Lin, Z.; Mao, H.; Qiu, Z.; Xiang, K.; Ke, T.; Li, L.; Lu, L.; Xiao, L. Layered GelMA/PEGDA Hydrogel Microneedle Patch as an Intradermal Delivery System for Hypertrophic Scar Treatment. ACS Appl. Mater. Interfaces 2023, 15, 43309–43320. [Google Scholar] [CrossRef] [PubMed]
- Meng, S.; Wei, Q.; Chen, S.; Liu, X.; Cui, S.; Huang, Q.; Chu, Z.; Ma, K.; Zhang, W.; Hu, W.; et al. MiR-141-3p-Functionalized Exosomes Loaded in Dissolvable Microneedle Arrays for Hypertrophic Scar Treatment. Small 2023, 20, e2305374. [Google Scholar] [CrossRef]
- Huang, Y.; Li, J.; Wang, Y.; Chen, D.; Huang, J.; Dai, W.; Peng, P.; Guo, L.; Lei, Y. Intradermal delivery of an angiotensin II receptor blocker using a personalized microneedle patch for treatment of hypertrophic scars. Biomater. Sci. 2023, 11, 583–595. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Zheng, L.; Yang, J.; Li, Y.; Zhang, Y.; Ma, T.; Wang, Q. Dissolving microneedle patches-mediated percutaneous delivery of tetramethylpyrazine for rheumatoid arthritis treatment. Eur. J. Pharm. Sci. 2023, 184, 106409. [Google Scholar] [CrossRef]
- Ding, H.; Cui, Y.; Yang, J.; Li, Y.; Zhang, H.; Ju, S.; Ren, X.; Ding, C.; Zhao, J. ROS-responsive microneedles loaded with integrin avβ6-blocking antibodies for the treatment of pulmonary fibrosis. J. Control. Release 2023, 360, 365–375. [Google Scholar] [CrossRef]
- Ben David, N.; Richtman, Y.; Gross, A.; Ibrahim, R.; Nyska, A.; Ramot, Y.; Mizrahi, B. Design and Evaluation of Dissolvable Microneedles for Treating Atopic Dermatitis. Pharmaceutics 2023, 15, 1109. [Google Scholar] [CrossRef]
- Ye, G.; Jimo, R.; Lu, Y.; Kong, Z.; Axi, Y.; Huang, S.; Xiong, Y.; Zhang, L.; Chen, G.; Xiao, Y.; et al. Multifunctional natural microneedles based methacrylated Bletilla striata polysaccharide for repairing chronic wounds with bacterial infections. Int. J. Biol. Macromol. 2024, 254, 127914. [Google Scholar] [CrossRef] [PubMed]
- Long, L.-Y.; Liu, W.; Li, L.; Hu, C.; He, S.; Lu, L.; Wang, J.; Yang, L.; Wang, Y.-B. Dissolving microneedle-encapsulated drug-loaded nanoparticles and recombinant humanized collagen type III for the treatment of chronic wound via anti-inflammation and enhanced cell proliferation and angiogenesis. Nanoscale 2022, 14, 1285–1295. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Xu, X.; Wu, M.; Liu, J.; Feng, J.; Zhang, J. Multifunctional zwitterionic microneedle dressings for accelerated healing of chronic infected wounds in diabetic rat models. Biomater. Sci. 2023, 11, 2750–2758. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.; Zhang, X.; Xu, D.; Li, N.; Zhao, Y. Encoded Structural Color Microneedle Patches for Multiple Screening of Wound Small Molecules. Adv. Mater. 2023, 35, e2211330. [Google Scholar] [CrossRef]
- Samant, P.P.; Niedzwiecki, M.M.; Raviele, N.; Tran, V.; Mena-Lapaix, J.; Walker, D.I.; Felner, E.I.; Jones, D.P.; Miller, G.W.; Prausnitz, M.R. Sampling interstitial fluid from human skin using a microneedle patch. Sci. Transl. Med. 2020, 12, eaaw0285. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Zhang, S.; Liu, Q.; Xu, T.; Zhang, X. Microfluidic-based plasmonic microneedle biosensor for uric acid ultrasensitive monitoring. Sens. Actuators B Chem. 2024, 398, 134685. [Google Scholar] [CrossRef]
- Zheng, L.; Zhu, D.; Xiao, Y.; Zheng, X.; Chen, P. Microneedle coupled epidermal sensor for multiplexed electrochemical detection of kidney disease biomarkers. Biosens. Bioelectron. 2023, 237, 115506. [Google Scholar] [CrossRef]
- He, Q.-Y.; Zhao, J.-H.; Du, S.-M.; Li, D.-G.; Luo, Z.-W.; You, X.-Q.; Liu, J. Reverse iontophoresis generated by porous microneedles produces an electroosmotic flow for glucose determination. Talanta 2024, 267, 125156. [Google Scholar] [CrossRef]
- Huang, H.; Qu, M.; Zhou, Y.; Cao, W.; Huang, X.; Sun, J.; Sun, W.; Zhou, X.; Xu, M.; Jiang, X. A microneedle patch for breast cancer screening via minimally invasive interstitial fluid sampling. Chem. Eng. J. 2023, 472, 145036. [Google Scholar] [CrossRef]
- Park, W.; Maeng, S.-W.; Mok, J.W.; Choi, M.; Cha, H.J.; Joo, C.-K.; Hahn, S.K. Hydrogel Microneedles Extracting Exosomes for Early Detection of Colorectal Cancer. Biomacromolecules 2023, 24, 1445–1452. [Google Scholar] [CrossRef]
- Abd-El-Azim, H.; Tekko, I.A.; Ali, A.; Ramadan, A.; Nafee, N.; Khalafallah, N.; Rahman, T.; Mcdaid, W.; Aly, R.G.; Vora, L.K.; et al. Hollow microneedle assisted intradermal delivery of hypericin lipid nanocapsules with light enabled photodynamic therapy against skin cancer. J. Control. Release 2022, 348, 849–869. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Liu, Y.; Wang, Y.; Gao, P. Transdermal codelivery system of resveratrol nanocrystals and fluorouracil@ HP-β-CD by dissolving microneedles for cutaneous melanoma treatment. J. Drug Deliv. Sci. Technol. 2024, 91, 105257. [Google Scholar] [CrossRef]
- Xu, R.; Guo, H.; Chen, X.; Xu, J.; Gong, Y.; Cao, P.; Wei, C.; Xiao, F.; Wu, D.; Chen, W.; et al. Smart hydrothermally responsive microneedle for topical tumor treatment. J. Control. Release 2023, 358, 566–578. [Google Scholar] [CrossRef]
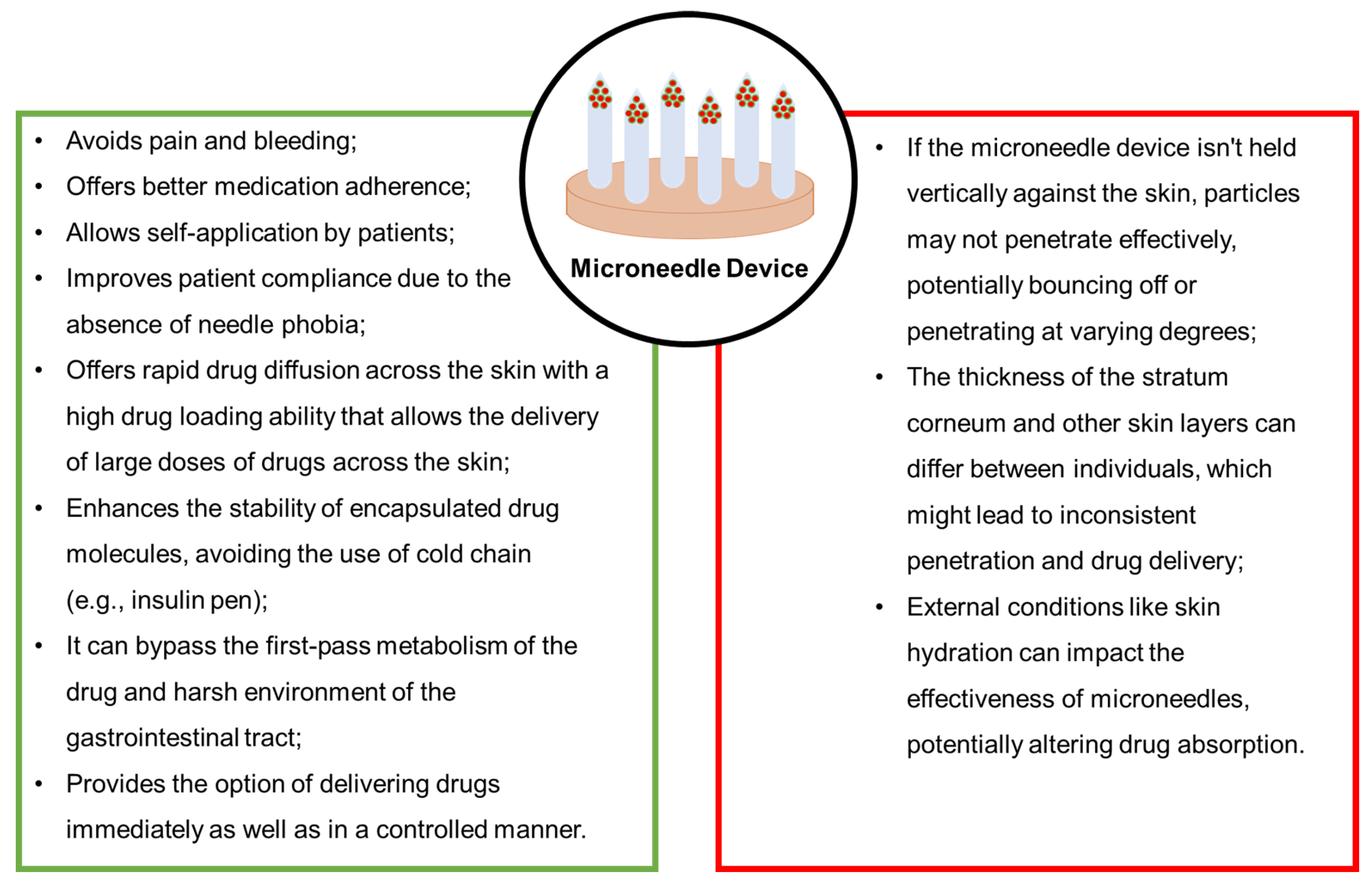


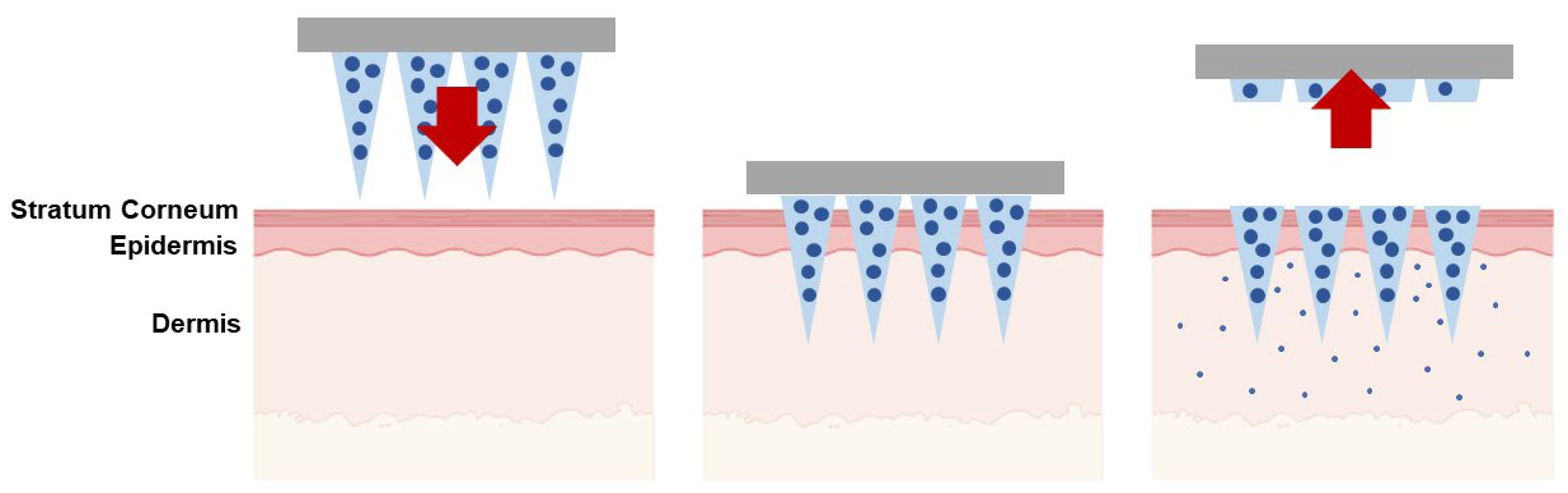


| Type of Microneedles | Delivery Strategies | Applications | References |
|---|---|---|---|
| Solid | The poke-and-patch method involves the application of numerous microneedles to create pores as a preparatory step. Following this, a traditional drug formulation is applied to the skin surface. | Skin pre-treatment for the delivery of potassium chloride, insulin, vaccines, cosmetics, and antipsychotic medication; monitoring of glucose and lactate levels; urea sensing. | [31,32,33,34,35,36,37] |
| Coated | The coat-and-poke technique involves applying a water-soluble drug coating on solid microneedles. This coating dissolves during administration, depositing the drug directly into the skin. | Delivery of proteins, vaccines, parathyroid hormone, insulin, desmopressin, and dexamethasone; sampling, isolation, and identification of biomarkers; monitoring of glucose. | [38,39,40,41,42,43,44,45] |
| Dissolving | The poke-and-dissolve method utilizes biodegradable or water-soluble microneedles encapsulating drugs. These microneedles dissolve upon application, releasing their therapeutic payload into the skin. | Delivery of vitamin B12, vaccines, therapeutic peptides, adenosine, doxorubicin, triamcinolone acetonide, near-IR photosensitizer (Redaporfin™), genes, and sodium nitroprusside in combination with sodium thiosulfate, tofacitinib, flurbiprofen axetil, epidermal growth factor, and ascorbic acid. | [46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] |
| Hollow | The poke-and-flow method involves microneedles with a hole in the center or side of their structure, allowing the drug to flow across the skin. | Delivery of teriflunomide, ceftriaxone sodium, mRNA, and vaccines; cell therapy; monitoring of glucose; synthetic amphetamine-type substance sensing; dermal interstitial fluid sampling and sensing. | [62,63,64,65,66,67,68,69] |
| Hydrogel-forming | The poke-and-release method utilizes water-insoluble microneedles injected into the skin, gradually releasing the encapsulated therapeutic molecule. The patch remains on the skin after application. | Delivery of albendazole, sildenafil citrate, metformin hydrochloride, methotrexate, and tuberculosis drugs; dermal interstitial fluid sampling. | [70,71,72,73,74,75] |
| Materials | Advantages | Limitations | References |
|---|---|---|---|
| Maltose | Biocompatible; No dermatological issues were noted on the human skin following insertion; High mechanical strength; Easy degradation; Fast dissolution; Controllable viscosity; Drug stability enhancer; Efficiently deliver protein drugs; Accelerate drug delivery. | High melting point is unfavorable for heat-sensitive drugs; The use of microneedles in a humid environment is limited due to the poor moisture resistance. | [95,96,97,98] |
| Hyaluronic acid (HA) | FDA-approved; Biocompatible; Biodegradable; Water solubility; Faster rate of dissolving; Enhance mechanical strength of dissolving microneedles; Quickly release drugs; Nontoxic and non-irritant; HA can be utilized for extended durations; No hypersensitivity effects or side effects associated with HA microneedles were identified in clinical studies. | Poor moisture resistance; Easy to shrink after microneedle fabrication. | [51,99,100,101,102,103] |
| 2-Hydroxypropyl-β-cyclodextrin (HP-β-CD) | Improve the solubility of poorly water-soluble drugs by forming inclusion compounds; Enhance mechanical strength of dissolving microneedles. | Selective inclusion. | [51,99,104] |
| Carboxymethylcellulose (CMC) | FDA-approved; Biocompatible; Biodegradable; Dissolve quickly in water; Can achieve slow and controllable release of drugs; In vitro cytotoxicity analysis and in vivo tissue response test did not show any side effects after treatment with CMC microneedles. | Poor moisture resistance; Poor mechanical strength. | [91,105,106] |
| Chitosan | Biocompatible, biodegradable, and nontoxic; It can either be cleared by the kidneys in vivo or degraded into fragments that are subsequently cleared by the kidneys; Antibacterial properties; Sufficient mechanical strength to penetrate porcine cadaver skin; Strong adsorption ability. | Limited raw materials; Negative water solubility. | [107,108,109,110,111] |
| Starch | Non-cytotoxic; Biodegradable; Higher mechanical strength than CMC. | Pure starch is more rigid and prone to fracturing and exhibits inferior film-forming characteristics. | [112,113,114] |
| Gelatin | Excellent biodegradability, biocompatibility, film formation, gelation, emulsification, water retention, and drug loading ability; Provides high safety and slow release. | Toughness of gelatin is poor, and it is easy to fracture; Low melting point and poor stability. | [107,112] |
| Silk fibroin | FDA-approved biomaterial; Non-cytotoxic, biocompatible, and the in vivo degradation products are non-inflammatory; Adequate mechanical force to pierce mouse skin for drug delivery; High tensile strength and toughness; Excellent mechanical characteristics, efficient gradual release of drugs, and favorable processing conditions. | Long fabrication time. | [115,116,117,118,119,120] |
| Poly(vinylpyrrolidone)(PVP) | Sufficient strength to pierce mouse skin; Enables the avoidance of organic solvents and high temperatures, aiding in the preservation of the drug’s stability and efficacy; Biocompatible and biodegradable; Low oral and transdermal toxicity; Non-irritating to skin; No adverse effects related to treatment were observed in a 6-month study. | Poor moisture resistance. | [112,121,122,123,124,125] |
| Polyvinyl alcohol (PVA) | Sufficient strength to penetrate both porcine cadaver skin and mouse skin; FDA-approved material; Biocompatible; Biodegradable; Good viscosity and toughness; Low cytotoxicity; Dissolve quickly in water. | Poor moisture resistance. | [107,126,127,128] |
| Polylactic acid (PLA) | FDA-approved biomaterial for the use of implants in humans; Biocompatible; Biodegradable; The in vivo degradation products are nontoxic; Excellent mechanical strength; High modulus of elasticity. | Fabrication of microneedles typically necessitates high temperatures (exceeding 170 °C) or organic solvents. | [31,107,129] |
| Polyglycolic acid (PGA) | FDA-approved biomaterial; Biocompatible; Biodegradable; The in vivo degradation products are nontoxic; Excellent mechanical strength to penetrate the regenerated human skin. | Fabrication of microneedles typically necessitates high temperatures or organic solvents. | [130] |
| Poly(lactide-co-glycolic acid) (PLGA) | Outstanding mechanical strength to pierce the murine skin; FDA-approved biomaterial; Biocompatible; Biodegradable; The in vivo degradation products are nontoxic. | Fabrication of microneedles typically necessitates high temperatures or organic solvents. | [129,131,132] |
| Polycaprolactone (PCL) | FDA-approved biomaterial; Biocompatible; Biodegradable; Non-cytotoxic; The in vivo degradation products are nontoxic; Sufficient mechanical strength to penetrate porcine cadaver skin for drug delivery. | The processing temperature is comparatively lower than PLA, PGA, and PLGA, yet still above 50 °C, which poses a constraint on incorporating heat-sensitive drugs such as insulin. | [129,133] |
| Fabrication Method | Advantages | Limitations | References |
|---|---|---|---|
| MEMS-based methods | Very precise geometries; Smooth vertical sidewall. | Time consuming; Expensive; Difficult to fabricate complex structures; Basic material limited to silicone and photocurable polymers. | [165,166] |
| Micromolding | High precision; Cost effective; Used for mass production; A large variety of basic material. | Difficult to fabricate complex structures; Drug load capacity; Mechanical behavior; Controls the depth of penetration. | [165,166] |
| Laser ablation | Less time consuming. | Might cause a crack or fatigue resistance on the substrate (microneedle array); Expensive; Not suitable for large fabrication. | [166] |
| Injection molding | Mass production; Cost effective. | High initial cost (machine equipment cost); Complex process. | [166] |
| Method | Advantages | Disadvantages |
|---|---|---|
| Mechanical force drawing | Cost effective | Time consuming Low precision Unable to produce complex structures Restricted to thermoplastic materials |
| Contact drawing | Cost effective Rapid | Low precision Unable to produce complex structures Viscosity of basic material requires adjustment |
| Electro-drawing | Cost effective Rapid | Low precision Unable to produce complex structures Conductivity of basic material requires adjustment |
| Centrifugal drawing | Cost effective Rapid | Low precision Unable to produce complex structures |
| Method | Advantages | Disadvantages |
|---|---|---|
| Fused deposition modelling (FDM) | Cost effective Less time consuming | Low precision Cannot fabricate complex structures Needs post treatment |
| Stereolithography (SLA) | Less time consuming Able to fabricate complex structures | Average precision |
| Two-photon polymerization (2PP) | High precision Easy to fabricate complex structures | Expensive Time consuming Difficult to fabricate objects with large volume |
| Microneedle System | Active Ingredient/Sampling | Application | Reference |
|---|---|---|---|
| Polymeric microneedles | Ovalbumin and CpG | Vaccine delivery | [285] |
| Hollow microneedles | Insulin | Vaccine delivery | [310] |
| Dissolving microneedle patches | Heat-inactivated bacteria | Vaccine delivery | [311] |
| Solid pyramidal microneedle | Stabilized HIV envelope trimer immunogen and adjuvant | Vaccine delivery | [312] |
| Microneedle patches | Acetyl-hexapeptide-3 | Wrinkle | [280] |
| Stainless solid microneedles | 5-Fluorouracil | Keloids | [313] |
| Poly(ionic liquid)-based microneedle patches | Salicylic acid | Acne | [314] |
| Dissolvable hyaluronic acid microneedles | Shikonin | Hypertrophic scars | [315] |
| Methacrylate gelatin/polyethylene glycol diacrylate double-network hydrogel microneedle patch | Betamethasone | Hypertrophic scars | [316] |
| Dissolving microneedle array | MiRNA-modified functional exosomes | Hypertrophic scars | [317] |
| Dissolving gelatin and starch microneedle patches | Losartan | Hypertrophic scars | [318] |
| Dissolving microneedle | Triamcinolone acetonide | Psoriasis | [50] |
| Dissolving microneedle patches | Tetramethylpyrazine | Rheumatoid arthritis | [319] |
| Hydrogen peroxide-responsive microneedle | Integrin αvβ6-blocking antibody | Pulmonary fibrosis | [320] |
| Dissolvable microneedles | Dexamethasone | Atopic dermatitis | [321] |
| Natural antimicrobial material microneedles | Peony leaf extract | Chronic wounds | [322] |
| Hyaluronic acid microneedle | Recombinant humanized collagen type III and naproxen loaded poly(lactic-co-glycolic acid) nanoparticle | Chronic wounds | [323] |
| Zwitterionic microneedle dressings | Zinc oxide nanoparticles and asiaticoside | Chronic wounds | [324] |
| Encoded structural color microneedle patches | Photonic crystals | Wound biomarker detection | [325] |
| Microneedle patches | Interstitial fluid | Sampling of interstitial fluid | [326] |
| Microfluidic-based wearable plasmonic microneedle sensor | Interstitial fluid | Uric acid monitoring | [327] |
| Polymeric-microneedle-coupled electrochemical sensor array | Interstitial fluid | Diagnosis of chronic kidney disease | [328] |
| Ion-conductive porous microneedle-based glucose sensing device combined with reverse ion electroosmosis | Interstitial fluid | Glucose determination (management of chronic diseases) | [329] |
| Gelatin methacrylate–acrylic acid microneedle patch | Interstitial fluid | Breast cancer screening | [330] |
| Hydrogel microneedles | Interstitial fluid | Colorectal cancer diagnosis | [331] |
| AdminPen™ hollow microneedle array | Hypericin lipid nanocapsules | Non-melanoma skin cancer | [332] |
| Dissolvable microneedle patch | Resveratrol nanocrystals and fluorouracil@hydroxypropyl-beta-cyclodextrin | Cutaneous melanoma | [333] |
| Hydrothermally responsive multi-round acturable microneedle | Docetaxel | Subcutaneous tumors | [334] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira, C.; Teixeira, J.A.; Oliveira, N.; Ferreira, S.; Botelho, C.M. Microneedles’ Device: Design, Fabrication, and Applications. Macromol 2024, 4, 320-355. https://doi.org/10.3390/macromol4020019
Oliveira C, Teixeira JA, Oliveira N, Ferreira S, Botelho CM. Microneedles’ Device: Design, Fabrication, and Applications. Macromol. 2024; 4(2):320-355. https://doi.org/10.3390/macromol4020019
Chicago/Turabian StyleOliveira, Cristiana, José A. Teixeira, Nelson Oliveira, Sónia Ferreira, and Cláudia M. Botelho. 2024. "Microneedles’ Device: Design, Fabrication, and Applications" Macromol 4, no. 2: 320-355. https://doi.org/10.3390/macromol4020019
APA StyleOliveira, C., Teixeira, J. A., Oliveira, N., Ferreira, S., & Botelho, C. M. (2024). Microneedles’ Device: Design, Fabrication, and Applications. Macromol, 4(2), 320-355. https://doi.org/10.3390/macromol4020019









