1. Introduction
IgA vasculitis, formerly Henoch-Schönlein purpura (HSP), is a form of systemic vasculitis that most commonly affects children. It targets small vessels and is characterized by IgA1-dominant immune deposition at diseased vessel walls, leading to leukocytoclastic vasculitis. This can restrict blood flow and damage vital organs and tissues [
1]. Cutaneous IgA vasculitis is the most characteristic manifestation of this disease. It typically presents as purpura, which is the clinical expression of red blood cell extravasation in the dermis. Although not always the case, palpable purpura usually reflects the presence of an inflammatory cell infiltrate [
2].
We present a case of hard-to-heal lower extremity lesions in a patient with confirmed IgA vasculitis or HSP. A bacterial presence at loads that impeded healing and promoted infection was identified, located, and addressed with the help of fluorescence imaging. Clinically it was not possible to reach this finding. Furthermore, targeting the bacterial presence resulted in the complete resolution of these lesions.
Fluorescence imaging was performed using a point-of-care imaging device (MolecuLight®, MolecuLight, Toronto, ON, Canada) that can detect bacterial loads >104 CFU/g. The imaging device is FDA-approved and used primarily in wound care. This case demonstrates additional areas in which bacterial fluorescent imaging may be valuable.
3. Case Report
A morbidly obese 21-year-old female patient was referred to our Wound Care Clinic at the Madigan Army Medical Center in Tacoma, WA, USA.
In April 2021, the patient presented to Dermatology with a history of polycystic ovarian syndrome. She had started spironolactone 25 mg daily 3.5 weeks prior and had subsequently developed a folliculitis-like eruption that originated in the groin and then became diffuse. The eruption was improved with PO Doxycycline 100 mg BID for 10 days, but the rash on her legs worsened. The patient also reported taking Cephalexin tablets with no relief. Dermatology took a punch biopsy of the skin. Clobetasol 0.5% was prescribed to be applied topically BID. Eleven days post-biopsy, the patient was instructed to care for the site daily with Vaseline.
Upon her visit to Rheumatology in May, the patient was instructed to manage with topical clobetasol 0.05%. In mid-May, the patient received biopsy results of IgA vasculitis/HSP. The patient was placed on a long-term tapering regimen of high-dose oral Prednisone initiated in June. The taper was 80 mg for 1 week, then 40 mg for 1 week, then 30 mg for 1 week, then 20 mg for 1 week, then 10 mg for 1 week, and concluded with 5 mg for 1 week as prescribed by Dermatology and Rheumatology. In late June, the patient began taking Dapsone 50 mg daily, as prescribed by Rheumatology. According to the patient, topical steroids had no effect, and she experienced no significant improvement in the ulcerative/necrotic purpura and vesiculobullous lesions on her legs while on steroids.
She presented on 29 June 2021 for her initial visit to Wound Care with several eroded papules and plaques on bilateral lower extremities (
Figure 1a,c,e). The lesions were reportedly growing in size. The patient was assessed by experienced wound care clinicians (a vascular surgeon and a wound care nurse), and all the wounds were found to be negative for clinical signs and symptoms of infection (e.g. no purulent drainage or odor).
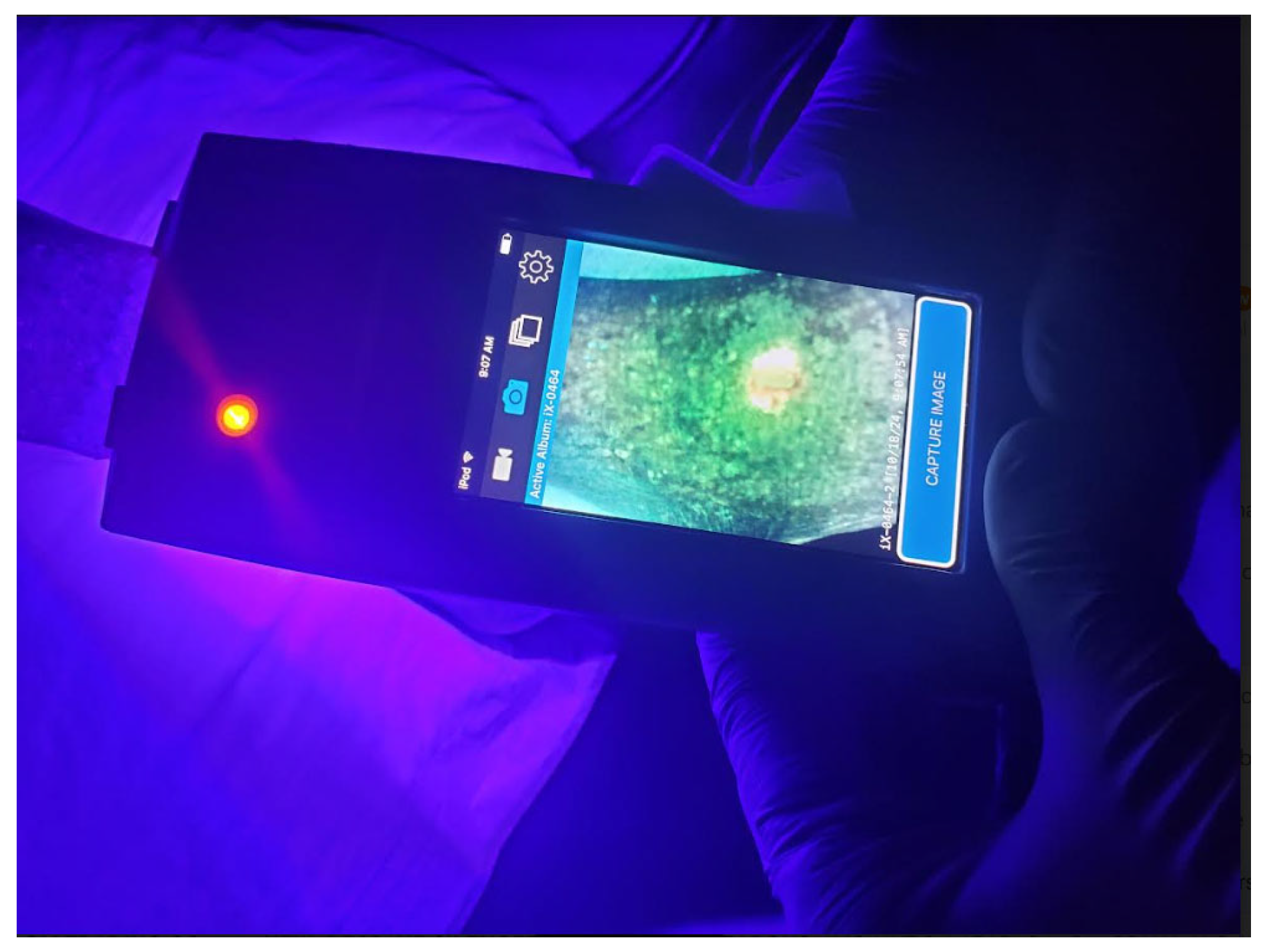
Fluorescence imaging (MolecuLight i:X) was used for wound assessment on all the wounds/lesions, and revealed the presence of red fluorescence, primarily in the peri-wound (
Figure 1b,d,f). These findings represent the presence of gram+/− aerobe/anaerobe bacterial loads greater than 10
4 CFU/g.
Based on the fluorescence findings, a treatment plan with a focus on the mechanical removal of bacterial loads was outlined. Wound cleansing was performed with Dakin’s 0.25% percent-soaked gauze; however, the red fluorescence persisted. No sharp debridement was deemed necessary. As per our workflow algorithm, because the post-cleansing or post-debridement scan was still positive for bacterial fluorescence the patient was prescribed a 1-month course of oral Doxycycline (100 mg BID).
Under the discretion of the Wound Care Clinic, the patient was scheduled to return every 2 weeks. Doxycycline was continued, in addition to Mupirocin ointment and a Mepilex dressing changed every 3 days. Rheumatology managed the Prednisone taper.
During the 1-month follow-up on 22 July 2021 all the wounds appeared to be improving. Once again, no clinical signs and symptoms of infection were noted. However, as noted in
Figure 2, this yellow and red bacterial fluorescence was evidenced through the MolecuLight® device. Yellow fluorescence is a variation of red fluorescence that represents subsurface bacteria. This yellow fluorescence area was much smaller than that observed in the fluorescence images a month prior. (
Figure 1).Some wounds had epithelialized with only a few remaining. Based on FL imaging findings, we performed wound cleansing with Dakin’s soaked gauze once again. In addition, we applied an antibiotic ointment post-cleansing (Mupirocin) and continued with the oral course of Doxycycline for 2 weeks. It is worth noting that throughout the previous month, the patient had been tapered off from all steroids.
Three months after her initial visit, the patient presented to the Wound Care Clinic. She had visible clinical improvement on inspection (
Figure 3a), and under fluorescence imaging, no signals indicating high bacterial loads were noted. All the lesions were considered negative for pathogenic bacteria and/or infection (
Figure 3b). The patient reported being symptom-free.
No further treatments were determined to be necessary, and the patient was discharged from our care. She was not taking steroids or antibiotics at that time. No recurrences have been noted almost 3 years after her initial visit.
According to The American College of Rheumatology, the natural history of HSP is a brief illness, but it is one that can cause distress to those affected [
3]. As demonstrated in this case, the disease is only present for a few months, but it is puzzling to treat until it seemingly spontaneously resolves. Due to the additional complication of bacterial colonization in this specific case, antibiotics were used to aid in wound closure so resolution could be achieved.
4. Discussion
IgA vasculitis is characterized by palpable purpura, arthralgia, and abdominal pain. It accounts for 10% of cutaneous vasculitis [
4]. It is the most common form of vasculitis in children, with an annual incidence of 3 to 26 per 100,000 children. It is most common between 4 and 7 years of age [
5] and is often preceded by an upper respiratory tract infection, normally related to Beta-hemolytic streptococci. However, other associations have been found, including previous use of certain medications, such as ACE inhibitors, angiotensin II receptor antagonists, clarithromycin, and non-steroidal anti-inflammatories.
Clinical manifestations mainly involve cutaneous palpable purpura, arthralgias and/or arthritis, acute enteritis, and glomerulonephritis. Fatal cases are most often related to renal and gastrointestinal compromise [
6]. In adults, it is significantly more uncommon than in children, with an estimated incidence between 0.1 and 1.8 per 100,000 individuals [
6], and most cases of this pathology have a benign course and are self-limited.
Treatment is controversial and is considered difficult because the correlation between the clinical severity of the initial presentation and the likelihood of long-term serious outcomes or spontaneous remission is inaccurate [
7]. Papular or polymorphic purpura is usually the clinical expression of leukocytoclastic vasculitis. However, some vasculitis may result in nonpalpable purpura. Polymorphic purpura preferentially affects the lower extremities. Due to the lack of clinical evidence of infection, bacterial wound care was delayed. As soon as bacterial colonization was identified by fluorescence imaging (seen in
Figure 4), the wounds were appropriately treated, and with antibiotics, the trajectory began to improve. Other imaging techniques, such as optical coherence tomography, may prove to be useful, but these are not available at MAMC.