Abstract
Acrodermatitis chronica atrophicans (ACA) is not an infrequent condition in Europe. However, the characteristic skin lesions are often confused by non-dermatologists with other conditions. We report three unusual cases in which we made a definitive diagnosis of ACA complicated by cutaneous marginal zone lymphoma, juxta-articular fibrotic nodules, or bilateral sensory polyneuropathy. In all cases, correct diagnosis and adequate treatment was delayed over a period of at least 12 months. We initiated systemic antibiotics resulting in full recovery in these patients. The present case reports underscore that ACA may be associated with unusual clinical presentation which potentially result in delay of correct diagnosis and treatment. Hence, ACA diagnosis may be considerably delayed leading to inappropriate therapy exposure, prolonged patients’ suffering, and causing unnecessary cost. Thus, physicians who are not familiar with skin conditions should seek a timely dermatologist consultation.
1. Introduction
The spirochete Borrelia burgdorferi (B. burgdorferi) sensu lato (Lyme group) represents the pathogenic germ of Lyme disease (LD), transmitted to humans by tick bites. Three dermatological presentations of LD can be distinguished. Stage 1 (early stage) of LD, known as erythema migrans, is characterized by a distinctive “bull’s eye rash.” If untreated, this initial stage may progress to an early disseminated infection. In stage 2, borrelial lymphocytoma/lymphadenosis cutis benigna can develop, sometimes also alongside neurological and cardiac symptoms. Late infection (stage 3) is also observed, particularly manifesting with arthritis in North America and acrodermatitis chronica atrophicans (ACA) in Europe [1]. Around 20% of patients with ACA have previously experienced spontaneously healed erythema migrans, typically on an extremity where the ACA lesion appeared 6 months to 8 years later [1]. Hence, ACA represents a late and chronic manifestation of LD in European [1]. ACA was initially documented in 1883 by Buchwald, who characterized it as a “diffuse idiopathic skin atrophy”, which was later termed ACA in 1902 [2]. Therefore, ACA was identified in Europe a century prior to LD identification in the United States in 1983 [2].
The initial phase of ACA involves a gradual enlargement of reddish-blue discoloration and skin swelling in the distal, extensor areas of the affected extremities (indicating an inflammatory stage) [2]. Left untreated, ACA can evolve into chronic atrophy and fibrosis. In stage 3, LD may affect cardiovascular, musculoskeletal, neurological, and dermatologic systems, thus defined as a multisystem disorder. In an advanced stage, LD may also become resistant to antibiotic treatment [1].
The diagnosis of LD is based on its characteristic clinical appearance, histopathology, and serology [3]. The most common laboratory test used to diagnose LD is the detection of B. burgdorferi-specific IgM and IgG serum antibodies. In a two-tiered approach, an ELISA (Enzyme-Linked Immunosorbent Assay) serves as the screening test. If the ELISA result is positive or equivocal, confirmation is required through a specific immunoblot test. The sensitivity of this method reaches 80–95% [3]. Even after receiving appropriate antibiotic treatment, however, a positive serological result can persist for many years. The continued presence of positive IgG and/or IgM antibody titers does not necessarily indicate antibiotic treatment, in the absence of typical symptoms of LD. Moreover, PCR tests may be performed to detect B. burgdorferi-DNA in various tissues, including the skin and cerebrospinal fluid. Other diagnostic tests include the lymphocyte transformation test and CD57+ natural killer cell determination. [3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. Histopathologic findings may vary depending on where in the lesion the specimen is taken from, but they typically consist of superficial and deep perivascular and interstitial lymphocytic infiltrates with eosinophils centrally and with histiocytes and plasma cells at the periphery [23]. Differential diagnoses of LD depends on the stage of the disease. In the case of ACA, acrocyanosis, acute arthritis, cellulitis, livedo reticularis, complex regional pain syndrome, hypodermitis in chronic venous insufficiency, eosinophilic fasciitis, and erythromelalgia may be considered differential diagnoses [24]. In accordance with a recent review on international guidelines for LD treatment, recommendations for antibiotic choice are relatively homogeneous across the countries [25]. Doxycycline (200 mg/d) is recommended to treat ACA in all guidelines and ceftriaxone (2 g/d) in almost all guidelines, particularly if associated with neuroborreliosis. The recommended duration is homogenous with at least 21 days. With respect to childhood LD, the recommended antibiotics follow the schemes for adults in all guidelines with dose adaptation. However, there is no explicit recommendation for ACA in this setting. In pregnancy, amoxicillin is the first-line agent in all published guidelines, whereas azithromycin is the second-line agent according to French guidelines and penicillin G or ceftriaxone is the second-line therapy according to German guidelines [25].
We here describe three unusual cases of ACA in which the clinical diagnosis was not straightforward and thus considerably delayed.
2. Case Presentations
2.1. Case 1
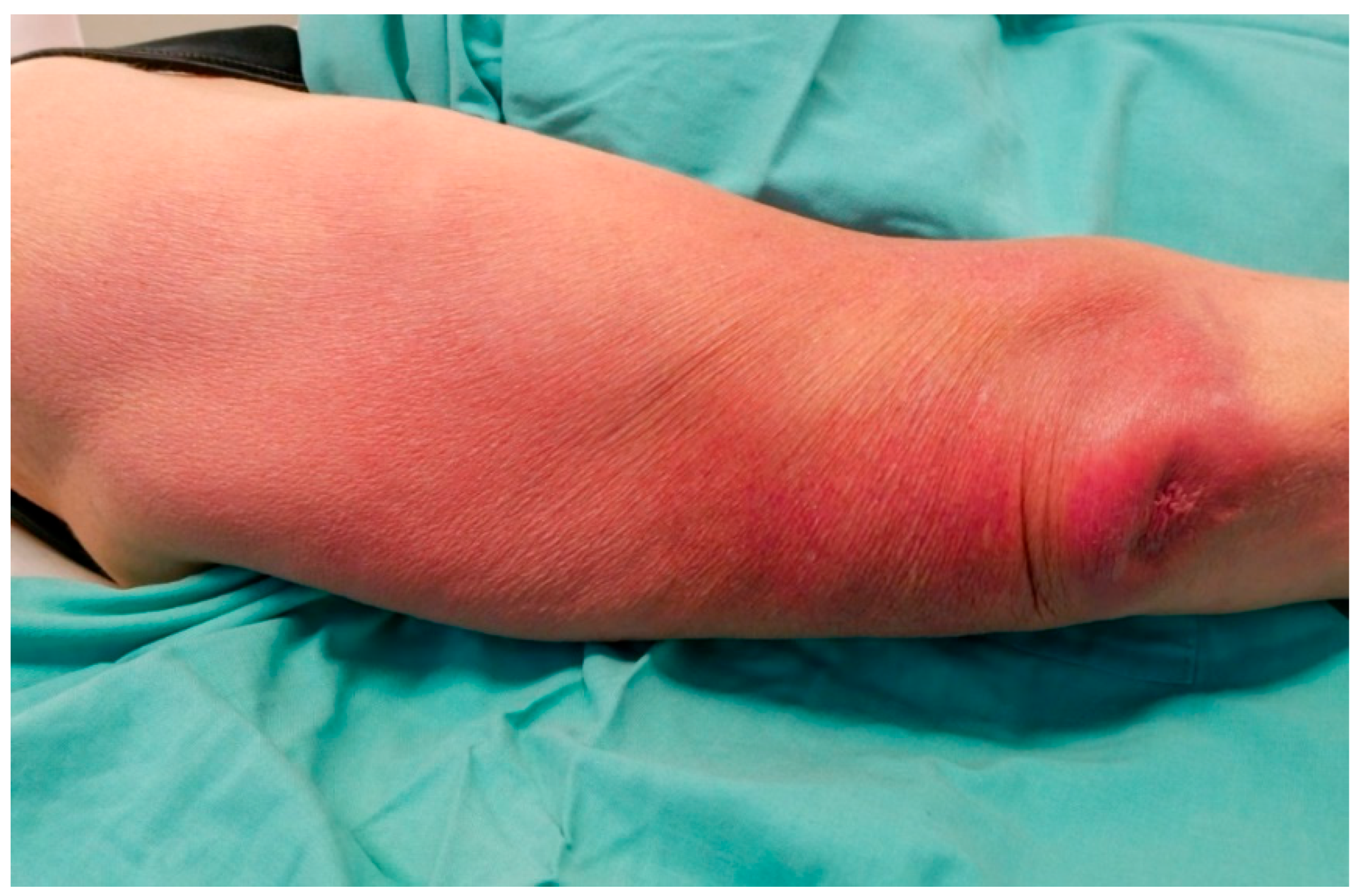
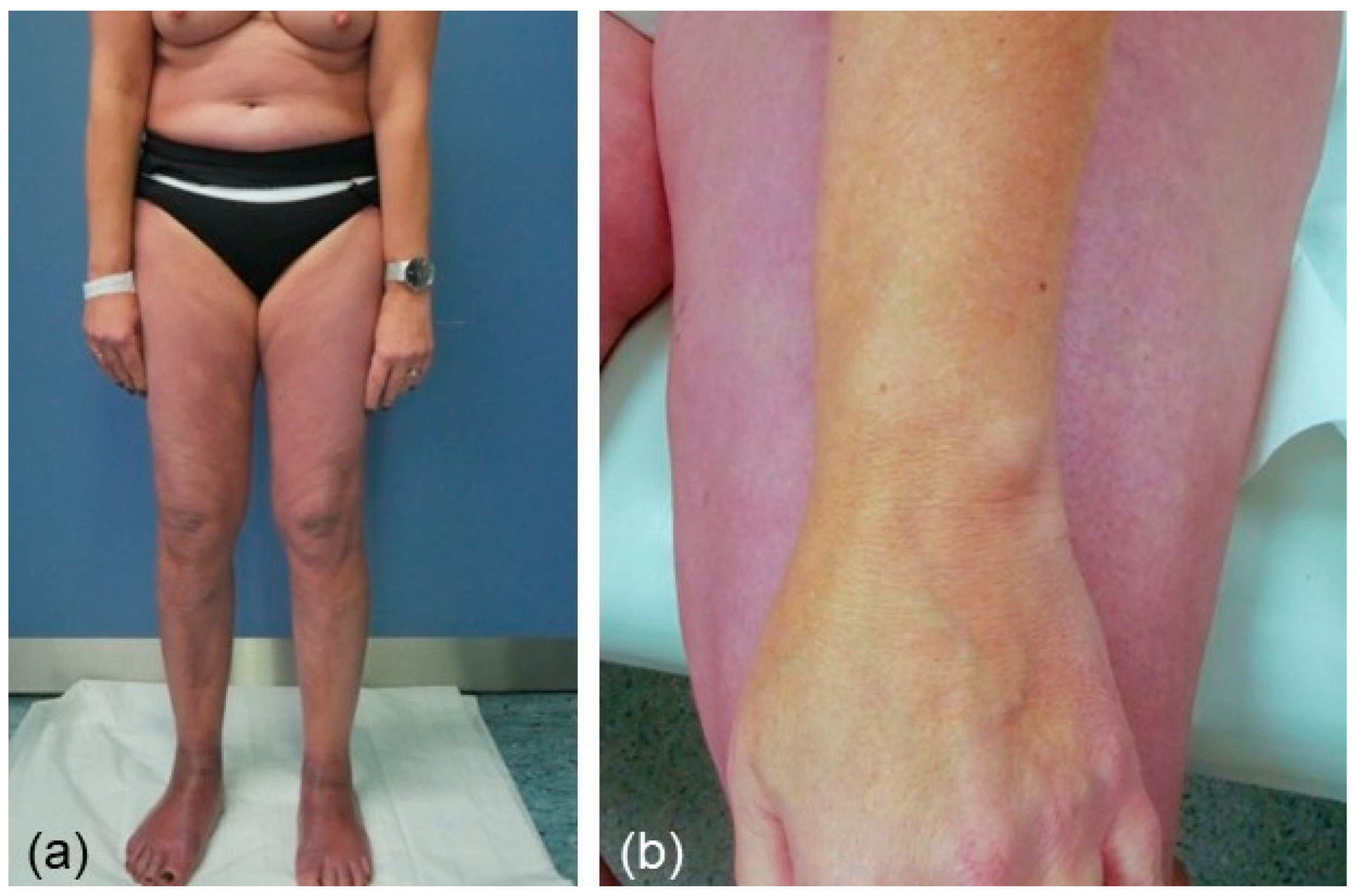
A 71-year-old female presented with a 1.5-year history of increasing erythematous and atrophic lesions on her right elbow and upper arm which were accompanied by warmth and slight pain on pressure (Figure 1).
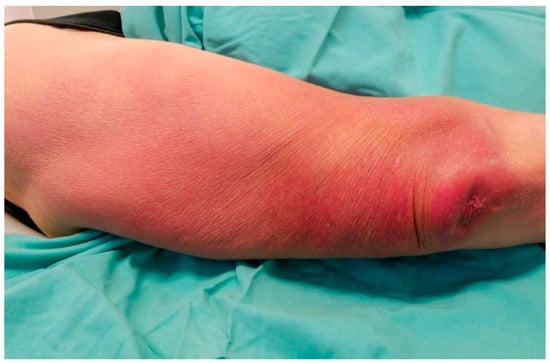
Figure 1.
Heliotrope erythema and atrophic skin on the elbow and upper arm of a patient who was referred because of recalcitrant chronic bursitis.
A tumorous lesion was noticed over the elbow as well. Her orthopedist diagnosed chronic bursitis and treated her with cooling and topical as well as systemic non-steroidal anti-phlogistics. However, her condition did not improve at all. Otherwise, she was a healthy woman without medications.
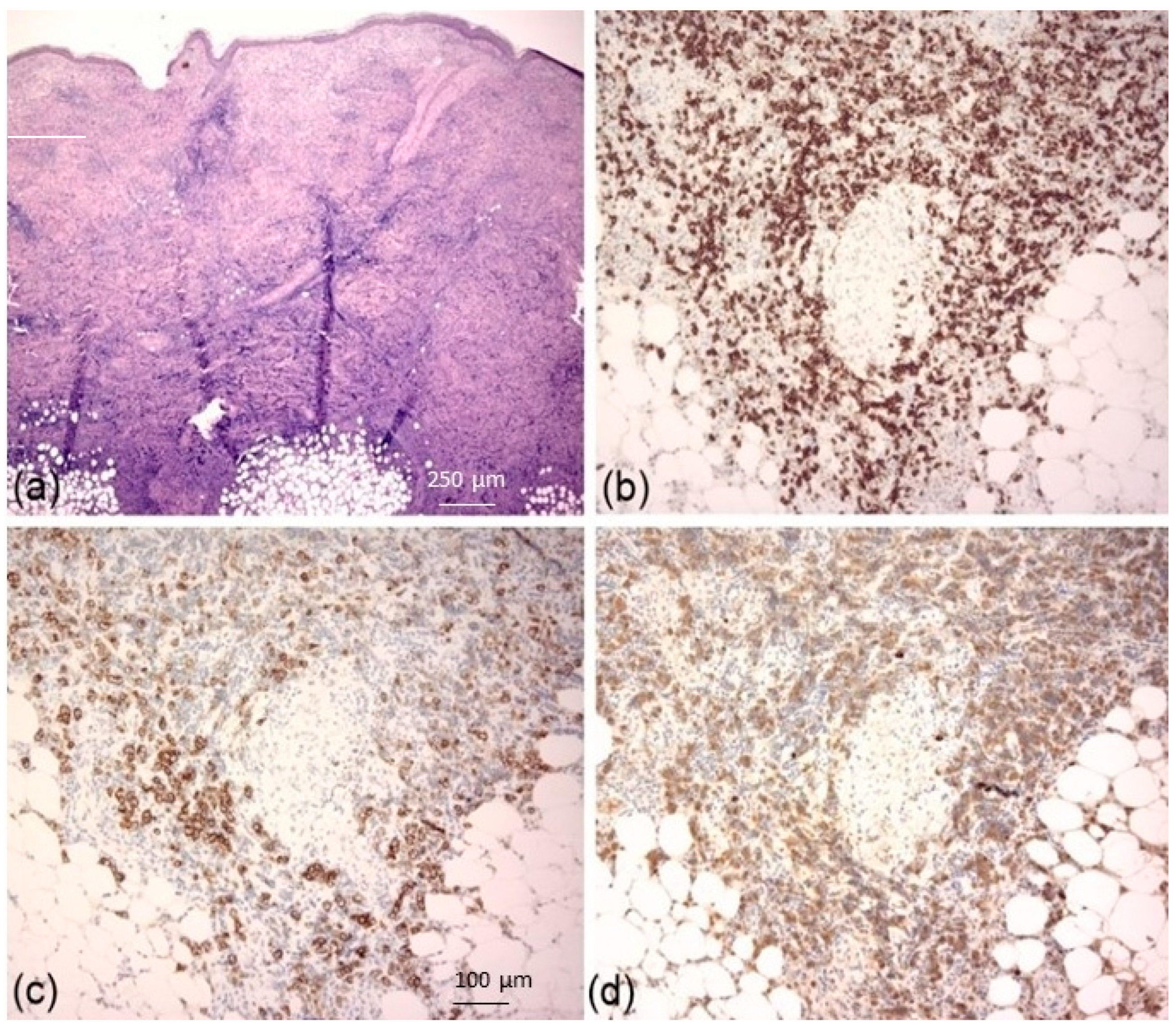
On admission, we performed two skin biopsies, one taken from the erythema on her lateral upper arm and one from the tumorous lesion on her elbow. Histopathological examination of the biopsy taken from the upper arm revealed a classic plasma cell-rich perivascular and interstitial pattern consistent with a diagnosis of ACA. RT-PCR confirmed the presence of B. burgdorferi-DNA. However, histopathological and immunohistochemical examination of the biopsy taken from the tumorous lesion revealed mixed infiltrates of small T and B lymphocytes (CD20+, CD5+) with intermingled CD138+ plasma cells also showing light-chain restriction of the lambda type. Ki-67 staining revealed a low proliferation index of 5%. We diagnosed a B. burgdorferi-associated cutaneous marginal zone lymphoma (CMZL) with clonal plasma cells which might have been developed from preexisting B. burgdorferi-associated pseudolymphoma (Figure 2).
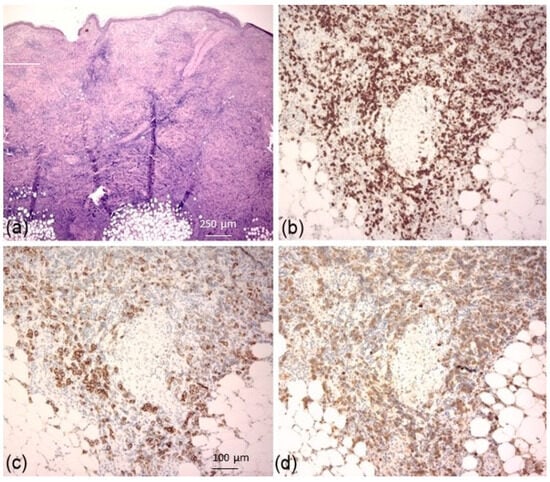
Figure 2.
Hematoxylin-eosin stain showing in the dermis and subcutis infiltrates of small lymphocytes ((a); HE, ×100). CD20 staining revealed abundance of B lymphocytes in the dermis/subcutis ((b); ×200), intermingled with CD138+ plasma cells ((c); ×200), showing light-chain restriction of lambda type ((d); ×200). A diagnosis of cutaneous marginal zone lymphoma with plasma cell differentiation was made.
Serology for B. burgdorferi (immunoblot) was negative for IgM but highly positive for IgG [>240 AU/mL (<10), positive recombinant antigens: VIsE, p58, p43]. Differential blood count, lymphocyte subpopulations, rheumatoid factor, anti-citrullin autoantibodies, antinuclear autoantibodies, immune electrophoresis, immunoglobulins, β1-microglobulin, neopterin, abdomen and lymph node ultrasound and thoracic X-ray did not reveal pathological findings. Treatment with doxycycline 100 mg twice daily over 3 weeks resulted in complete remission. Follow-up 6 months later confirmed the complete clearance of her condition with persistent high B. burgdorferi-specific IgG titers.
2.2. Case 2
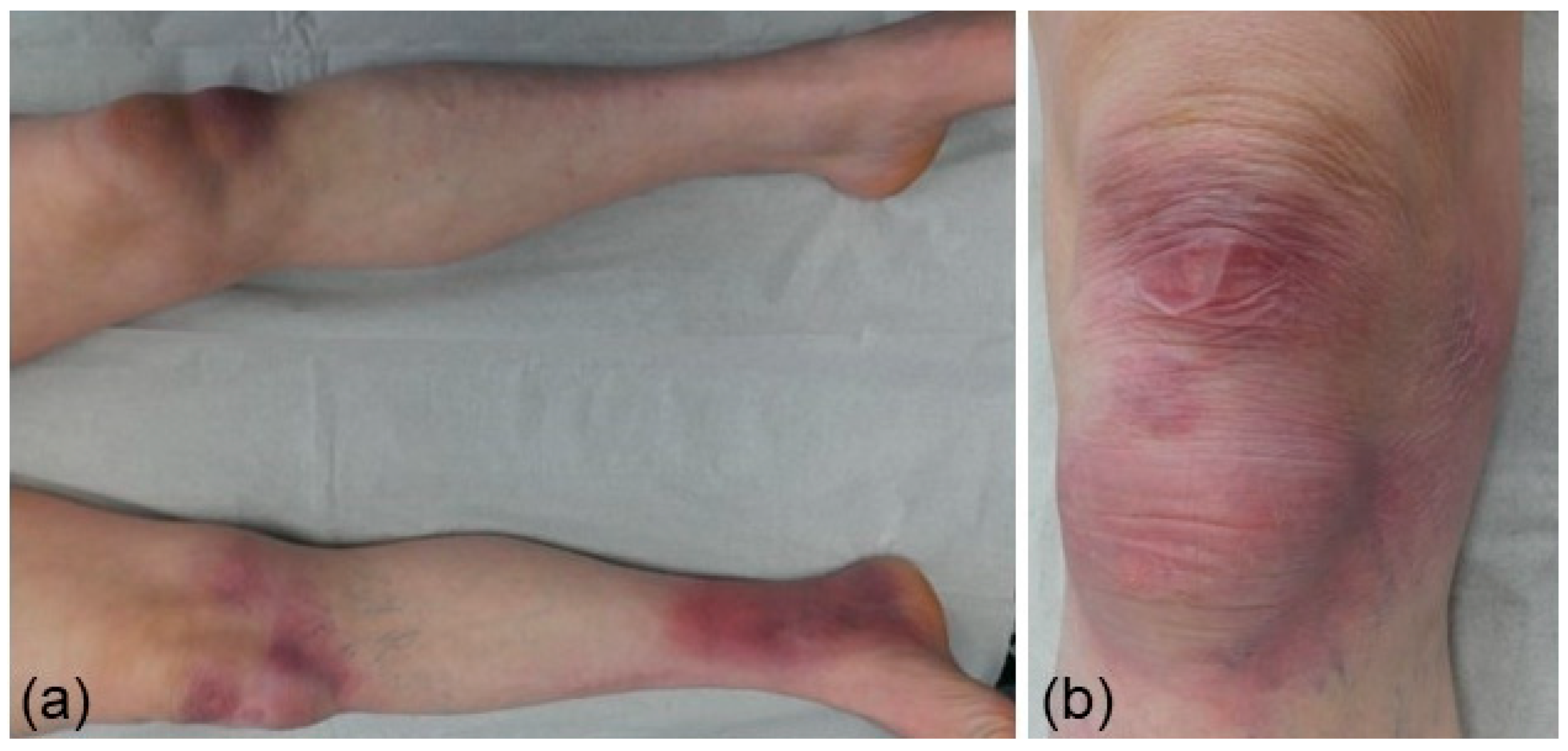
A 66-year-old male presented with a 2-year history of increasing violaceous lesions on his right ankle and both knees—the latter also showed atrophic skin and slight edema. The patient complained of a moderate pain in his right ankle (Figure 3). His orthopedist and rheumatologist diagnosed arthritis which was treated using cooling, topical as well as systemic corticosteroids, and pulsed radiofrequency. However, the patient did not
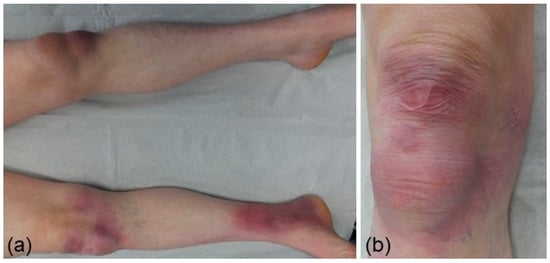
Figure 3.
Violaceous, partly atrophic, patches and plaques on the knees and right ankle of a patient referred to our hospital diagnosed with arthralgia/arthritis (a,b).
Notice any improvement of his condition. He had no history of rheumatic disorders or other chronic conditions, except for arterial hypertension. On admission, we performed two skin biopsies, one taken from the erythema on his ankle and one from the left knee revealing epidermis atrophy and plasma cell-rich inflammatory infiltrate, whereas the lesion on the left knee showed a more diffuse dermal plasma cell-rich infiltrate with adnexal atrophy and fibrosis (Figure 4).
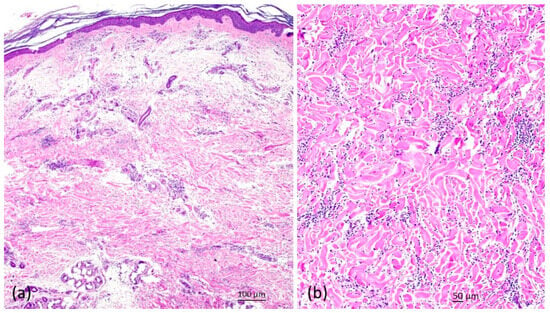
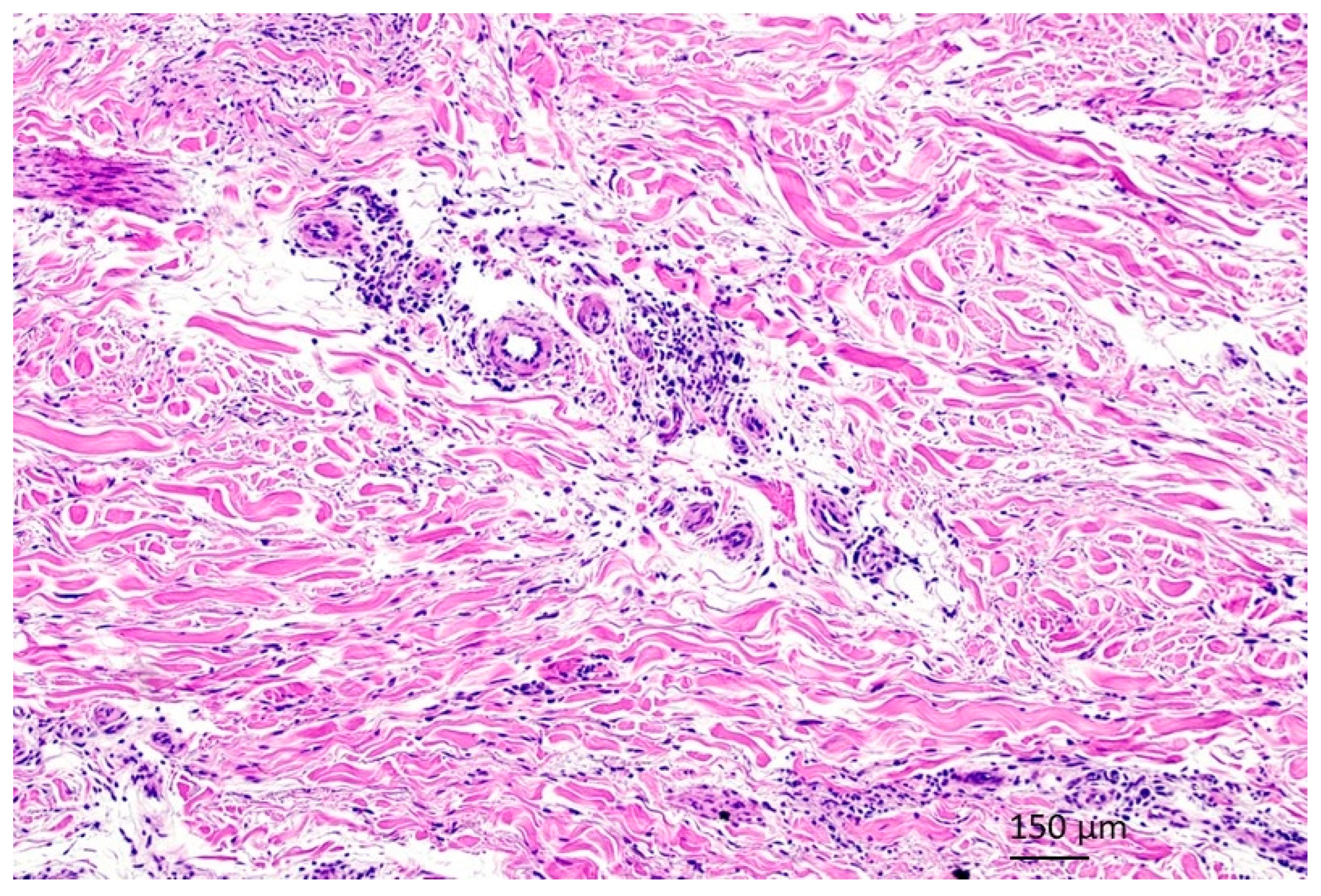
Figure 4.
Hematoxylin and eosin staining of a skin biopsy revealing slightly atrophic epidermis, perivascular and periadnexal infiltrates with intermingled plasma cells and sclerotizing dermatitis partly with homogenized collagen fibers ((a); HE, ×40; (b); ×100).
Serology for B. burgdorferi (immunoblot) was negative for IgM but highly positive for IgG [>240 AU/mL (<10), positive recombinant antigens: VIsE, p43, p14]. A diagnosis of ACA associated with juxta-articular fibrotic nodules was made. Initial treatment with doxycycline (100 mg twice daily) over 3 weeks did not result in the complete clearance of skin lesions and arthralgia. Hence, the patient was treated with intravenous ceftriaxon 2 g daily over a 3-week period resulting in complete remission of skin symptoms and arthralgia. Three months later, the patient was in complete remission, whereas B. burgdorferi-specific IgG was still over 240 AU/mL.
2.3. Case 3
A 55-year-old female presented with a 12-month history of ascending violaceous erythema on both legs which was accompanied by slight edema (Figure 5). Since this time, she also suffered from stinging pain as well as hypoesthesia of both feet and lower legs. Neurologists diagnosed sensory polyneuropathy in both legs. Neurographic findings revealed sensory axonal polyneuropathy of both legs. Neurologists suggested that her neurological symptoms have likely been caused by previous chemotherapy of her non-Hodgkin lymphoma using vincristin, doxorubicin, cyclophosphamide, and prednisolone (CHOP). Magnetic resonance imaging of the lumbar region did show a correlation for her lower leg complaints.
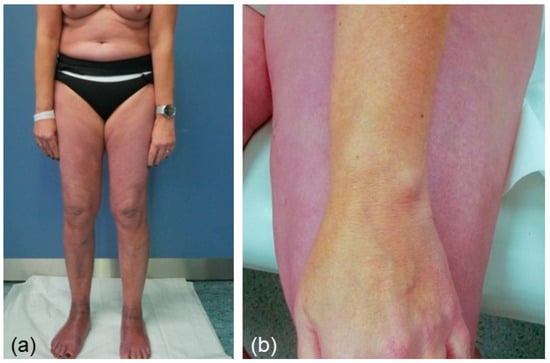
Figure 5.
Showing a female patient with symmetrically ascending erythema on both legs (a). The contrast between affected and unaffected skin is also highlighted (b).
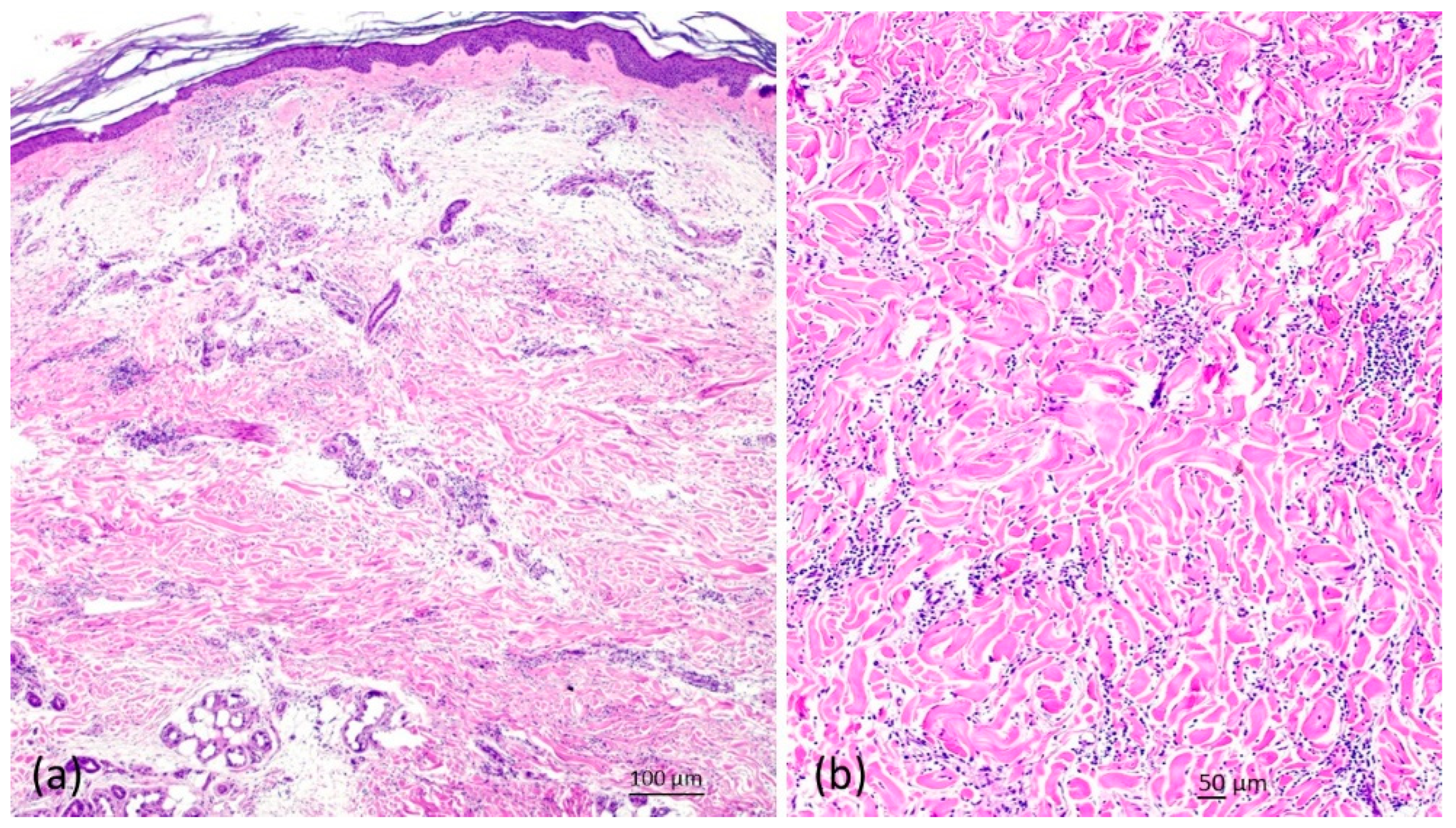
However, the chemotherapy was discontinued about one year prior to the onset of her cutaneous and neurological symptoms. Finally, the neurologists referred the patient to our dermatology outpatient department for counselling because of her unclear skin symptoms. A histology of a biopsy taken from the right ankle revealed a plasma cell-rich perivascular and interstitial pattern consistent with a diagnosis of ACA (Figure 6).
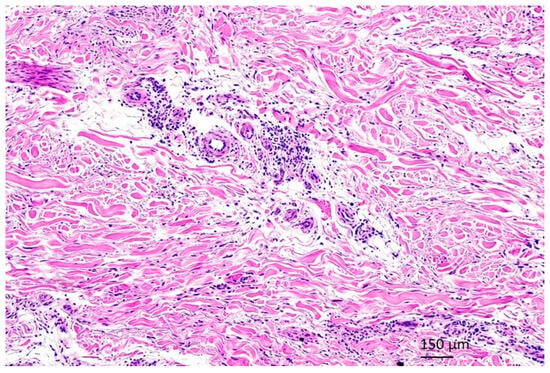
Figure 6.
Showing histopathology (HE, ×100) of a biopsy taken from the right ankle revealed a plasma cell-rich perivascular and interstitial pattern consistent with a diagnosis of ACA.
Serology for B. burgdorferi (immunoblot) was negative for IgM but highly positive for IgG [179 AU/mL (<10), and positive for recombinant antigens VIsE and Osp17/DpbA, p14]. Lumbar puncture revealed pleocytosis without the increase in protein. Intrathecal production of borrelia-specific IgM and/or IgG antibodies was not observed. A diagnosis of symmetrically ascending ACA with accompanied sensory polyneuropathy of both legs was made. Because of the widespread disease, the patient was treated with intravenous ceftriaxon 2 g daily over a 3-week period. Three months later, the erythema on her abdomen and legs was resolved. More importantly, her neurological symptoms had disappeared. B. burgdorferi-specific IgG was still 169 AU/mL.
3. Discussion
The presented case reports highlight the wide spectrum of clinical presentation, distribution, and symptomatology of ACA. The association of ACA and malignant lymphomas was often reported in Europe before B. burgdorferi was detected. Hence, a relation between B. burgdorferi infection and the development of cutaneous B cell lymphomas CBCL is obvious. Therefore, infection with B. burgdorferi should be considered in patients with CBCL, in particular in geographic regions where infected ticks are present. In rare cases, however, Lyme borreliosis can also histopathologically show T cell-rich infiltrates mimicking cutaneous T cell lymphoma. Awareness of this clinicopathologic constellation is crucial to avoid under-recognition of this unusual situation representing a B. burgdorferi-associated T cell pseudolymphoma [6,7,8,9,10,11,12]. Notably, ACA can be associated with pseudolymphoma showing a T cell as well as, less frequently, a B cell pattern. The association between primary CMZL and ACA has been previously observed in two patients who presented with monomelic erythema showing abundant plasma cells on histopathology [6]. Similar to the present case, the skin infiltrates of both patients showed a kappa monotypic light-chain and cutaneous B cell clones, whereas the clinical findings were evocative of LD. Diagnosis of B. burgdorferi-associated PCMZL was confirmed by positive serology. As also observed in case 1, clinical cure was achieved after 3-week oral tetracyclines without disease recurrence [6].
There are few existing reports on patients who presented with nodular or discoid fibrotic lesions in association with ACA. Juxta-articular fibrotic nodules may develop within a few months of the onset of ACA. Nodular/discoid morphea-like as well as disseminated cutaneous fibroses in chronic Lyme borreliosis can be induced by radiation or trauma such as surgery [13,14,15,16,17]. Marsch et al. [15,16] suggested that juxta-articular fibrotic nodules in chronic borreliosis offer a good in vivo model for investigating the evolution of immunologically induced fibrosis. As previously shown by Marsch et al. [15,16], B. burgdorferi-infection induced fibrosis in the upper subcutaneous tissue of the elbow region which was histopathologically characterized by broad hyalinized collagen bundles and perivascular infiltrates of lymphocytes and plasma cells. The latter vanished completely after five days of antibiotic therapy, whereas fibroblasts discharged matrix vesicles and elastic fibers. As also observed in the present case, juxta-articular fibrotic nodules in chronic borreliosis usually resolve rapidly under adequate antibiotic treatment [13,14,15,16,17].
Involvement of the peripheral nervous system is not infrequently observed in patients with longstanding ACA, in particular sensory polyneuropathy, which is typically asymmetric. A bilateral symmetrically ascending polyneuropathy, as shown in case 3 of the present report, is unusual, in particular the involvement of the lower part of the trunk. Most previous investigators have discovered a definite sex-predominance with women comprising about 70% of the patient population [18,19,20]. Frequent complaints reported are burning pain, skin hypersensitivity, feeling of furriness/numbness, and sensations of heaviness, or muscle weakness. Whereas alterations of sensibility are observed in the dermatologically healthy-appearing limbs, they can, however, be shown to be very severe and disseminated in the limbs with severely affected skin [18]. Apart from sensory polyneuropathy, other neuro-borreliosis complications (3–15%) may present as polyradiculitis, meningitis or—very rarely—as encephalomyelitis [18]. Antibiotic therapy of neuro-borreliosis consists of doxycycline, ceftriaxone, or penicillin G. Resolution of neurological complications in ACA patients such as sensory polyneuropathy is possible; however, some patients may be resistant to antimicrobial treatment. In the present case, skin symptoms as well as polyneuropathy fortunately fully recovered after the correct diagnosis and adequate treatment was performed. Importantly, the clearance of her neurological symptoms following antibiotic therapy was highly suggestive for borreliosis-induced and not chemotherapy-induced polyneuropathy. Indeed, vincristine-induced peripheral neuropathy (VIPN), remains a major complication of lymphoma patients treated with CHOP. However, VIPN is commonly a sensorimotor neuropathy developing in almost all cases during treatment of lymphoma [21].
4. Conclusions
The presented series of cases underscore that ACA may be associated with unusual clinical presentations which potentially result in delay of correct diagnosis and treatment [6,13,18,22]. Hence, in all cases presented here, ACA diagnosis was considerably delayed leading to inappropriate therapy exposure, prolonged patients’ suffering, and costs. Thus, physicians who are not familiar with skin conditions should seek a timely consultation with a dermatologist in order to enhance the probability of a correct diagnosis in such unusual cases.
Author Contributions
Conceptualization, T.G.; data interpretation, T.G., investigation, S.B., R.J. and T.G.; writing—original draft preparation, T.G. and R.J.; visualization, T.G., H.-W.B. and A.v.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This case study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Ruhr-University Bochum (#4222-12, date of the approval: 30 November 2015).
Informed Consent Statement
Informed consent was obtained from the patients presented.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gade, A.; Matin, T.; Rubenstein, R.; Robinson, C.A. Acrodermatitis Chronica Atrophicans. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Ogrinc, K.; Maraspin, V.; Lusa, L.; Cerar Kišek, T.; Ružić-Sabljić, E.; Strle, F. Acrodermatitis chronica atrophicans: Clinical and microbiological characteristics of a cohort of 693 Slovenian patients. J. Intern. Med. 2021, 290, 335–348. [Google Scholar] [CrossRef] [PubMed]
- Glatz, M.; Müllegger, R.R. Cutaneous manifestations of Lyme disease: Pitfalls in the serological diagnostic workup. Hautarzt 2017, 68, 329–339. [Google Scholar] [CrossRef] [PubMed]
- Müllegger, R.R.; Glatz, M. Is serological follow-up useful for patients with cutaneous Lyme borreliosis? Curr. Probl. Dermatol. 2009, 37, 178–182. [Google Scholar] [PubMed]
- National Guideline Centre (UK). Evidence Review for Management of Acrodermatitis Chronica Atrophicans: Lyme Disease: Diagnosis and Management: Evidence Review H; National Institute for Health and Care Excellence (NICE): London, UK, 2018. [Google Scholar] [PubMed]
- Bertolotti, A.; Pham-Ledard, A.; Petrot, D.; Coindre, M.C.; Brecheteau, P.; Mendes, I.; Vergier, B.; Beylot-Barry, M. Two cases of proliferation of monoclonal and monotypic lymphocytes and plasma cells corresponding to acrodermatitis chronica atrophicans. Ann. Dermatol. Venereol. 2014, 141, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Jelić, S.; Filipović-Ljesković, I. Positive serology for Lyme disease borrelias in primary cutaneous B-cell lymphoma: A study in 22 patients; is it a fortuitous finding? Hematol. Oncol. 1999, 17, 107–116. [Google Scholar] [CrossRef]
- Garbe, C.; Stein, H.; Gollnick, H.; Taud, W.; Orfanos, C.E. Cutaneous B cell lymphoma in chronic Borrelia burgdorferi infection. Report of 2 cases and a review of the literature. Hautarzt 1988, 39, 717–726. [Google Scholar]
- Tee, S.I.; Martínez-Escanamé, M.; Zuriel, D.; Fried, I.; Wolf, I.; Massone, C.; Cerroni, L. Acrodermatitis chronica atrophicans with pseudolymphomatous infiltrates. Am. J. Dermatopathol. 2013, 35, 338–342. [Google Scholar] [CrossRef]
- Gambichler, T.; Kreuter, J.A.; Stücker, M.; Kobyletzki, G.V.; Altmeyer, P.; Hoffmann, K. Guess what! Cutaneous lymphoid hyperplasia. Eur. J. Dermatol. 2000, 10, 635–636. [Google Scholar]
- Mitteldorf, C.; Neesse, A.K.; Hoffmann, J.C.; Schön, M.P.; Kempf, W. Acrodermatitis chronica atrophicans with clonal light chains and heavy chain rearrangement. J. Eur. Acad. Dermatol. Venereol. 2023, 37, e415–e417. [Google Scholar] [CrossRef]
- Kempf, W.; Kazakov, D.V.; Hübscher, E.; Gugerli, O.; Gerbig, A.W.; Schmid, R.; Palmedo, G.; Kutzner, H. Cutaneous borreliosis associated with T cell-predominant infiltrates: A diagnostic challenge. J. Am. Acad. Dermatol. 2015, 72, 683–689. [Google Scholar] [CrossRef]
- Kluge, K.; Krahl, D.; Kramer, K.; Yaguboglu, R. Juxta-articular fibroid nodules and acrodermatitis chronica atrophicans in late stage Lyme borreliosis. Hautarzt 2000, 51, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Lübbe, J.; Schlüpen, E.M.; Fierz, W.; Panizzon, R.G.; Burg, G. Identification of Borrelia afzelii in a juxta-articular fibroid nodule from a human immunodeficiency virus-positive patient with acrodermatitis chronica atrophicans. Arch. Dermatol. 1995, 131, 1341–1342. [Google Scholar] [CrossRef]
- Marsch, W.C.; Wolter, M.; Mayet, A. Juxta-articular fibrotic nodules in Borrelia infection--ultrastructural details of therapy-induced regression. Clin. Exp. Dermatol. 1994, 19, 394–398. [Google Scholar] [CrossRef] [PubMed]
- Messer, L.; Felten, R.; Moreau, P.; Freisz, M.C.; Mahé, A. Fibrous nodules over the patella revealing acrodermatitis chronica atrophicans. Jt. Bone Spine 2015, 82, 208. [Google Scholar] [CrossRef] [PubMed]
- Marsch, W.C.; Mayet, A.; Wolter, M. Cutaneous fibroses induced by Borrelia burgdorferi. Br. J. Dermatol. 1993, 128, 674–678. [Google Scholar] [CrossRef]
- Hopf, H.C. Peripheral neuropathy in acrodermatitis chronica atrophicans (Herxheimer). J. Neurol. Neurosurg. Psychiatry 1975, 38, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Kindstrand, E.; Nilsson, B.Y.; Hovmark, A.; Nennesmo, I.; Pirskanen, R.; Solders, G.; Asbrink, E. Polyneuropathy in late Lyme borreliosis—A clinical, neurophysiological and morphological description. Acta Neurol. Scand. 2000, 101, 47–52. [Google Scholar] [CrossRef]
- Kindstrand, E.; Nilsson, B.Y.; Hovmark, A.; Pirskanen, R.; Asbrink, E. Peripheral neuropathy in acrodermatitis chronica atrophicans—A late Borrelia manifestation. Acta Neurol. Scand. 1997, 95, 338–345. [Google Scholar] [CrossRef]
- Hatzl, S.; Posch, F.; Rezai, A.; Gornicec, M.; Beham-Schmid, C.; Magnes, T.; Wangner, S.; Deutsch, A.; Greinix, H.; Uhl, B.; et al. Vinorelbine as substitute for vincristine in patients with diffuse large B cell lymphoma and vincristine-induced neuropathy. Support Care Cancer 2021, 29, 5197–5207. [Google Scholar] [CrossRef]
- Brzonova, I.; Wollenberg, A.; Prinz, J.C. Acrodermatitis chronica atrophicans affecting all four limbs in an 11-year-old girl. Br. J. Dermatol. 2002, 147, 375–378. [Google Scholar] [CrossRef]
- Brem, C.E.; Goldberg, L.J. Early Erythema Migrans: Do Not Count on Plasma Cells. Am. J. Dermatopathol. 2022, 44, e23–e25. [Google Scholar] [CrossRef] [PubMed]
- Kjær, M.; Jensen, B.; Clemmensen, A. Acrodermatitis chronica atrophicans-probably an overlooked differential diagnosis for arthritis. Rheumatology 2017, 56, 398. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nguala, S.; Baux, E.; Patrat-Delon, S.; Saunier, F.; Schemoul, J.; Tattevin, P.; Cazorla, C.; Eldin, C.; Bouiller, K.; Raffetin, A. Methodological Quality Assessment with the AGREE II Scale and a Comparison of European and American Guidelines for the Treatment of Lyme Borreliosis: A Systematic Review. Pathogens 2021, 10, 972. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).