Increased Radiation Dose Exposure in Thoracic Computed Tomography in Patients with Covid-19
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kwee, T.C.; Kwee, R.M. Chest CT in COVID-19: What the Radiologist Needs to Know. RadioGraphics 2020, 40, 1848–1865. [Google Scholar] [CrossRef]
- Albarello, F.; Pianura, E.; Di Stefano, F.; Cristofaro, M.; Petrone, A.; Marchioni, L.; Palazzolo, C.; Schininà, V.; Nicastri, E.; Petrosillo, N.; et al. 2019-novel Coronavirus severe adult respiratory distress syndrome in two cases in Italy: An uncommon radiological presentation. Int. J. Infect. Dis. 2020, 93, 192–197. [Google Scholar] [CrossRef]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.A.M.; Huisman, M.V.; et al. Confirmation of the high cumulative incidence of thromboticcomplications in critically ill ICU patients with COVID-19: An updated analysis. Thromb. Res. 2020, 191, 148–150. [Google Scholar] [CrossRef] [PubMed]
- Grillet, F.; Behr, J.; Calame, P.; Aubry, S.; Delabrousse, E. Acute Pulmonary Embolism Associated with COVID-19 Pneumonia Detected with Pulmonary CT Angiography. Radiology 2020, 296, E186–E188. [Google Scholar] [CrossRef] [PubMed]
- Kaminetzky, M.; Moore, W.; Fansiwala, K.; Babb, J.S.; Kaminetzky, D.; Horwitz, L.I.; McGuinness, G.; Knoll, A.; Ko, J.P. Pulmonary embolism on CTPA in COVID-19 patients. Radiol. Cardiothorac. Imaging 2020, 2, e200308. [Google Scholar] [CrossRef] [PubMed]
- Oudkerk, M.; Büller, H.R.; Di Kuijpers van Es, N.; Oudkerk, S.F.; McLoud, T.C.; Gommers, D.; van Dissel, J.; Ten Cate, H.; van Beek, E.J. Prevention, and Treatment of Thromboembolic Complications in COVID-19: Report of the National Institute for Public Health of the Netherlands. Radiology 2020, 297, E216–E222. [Google Scholar] [CrossRef]
- Chi, G.; Lee, J.J.; Jamil, A.; Gunnam, V.; Najafi, H.; Memar Montazerin, S.; Shojaei, F.; Marszalek, J. Venous Thromboembolism among Hospitalized Patients with COVID-19 Undergoing Thromboprophylaxis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2489. [Google Scholar] [CrossRef] [PubMed]
- Zhong, L.; Zhang, S.; Wang, J.; Zhao, X.; Wang, K.; Ding, W.; Xing, Z.; Shen, J. Analysis of Chest CT Results of Coronavirus Disease 2019 (COVID-19) Patients at First Follow-Up. Can. Respir. J. 2020, 2020. [Google Scholar] [CrossRef]
- Kang, Z.; Li, X.; Zhou, S. Recommendation of low-dose CT in the detection and management of COVID-2019. Eur. Radiol. 2020, 30, 4356–4357. [Google Scholar] [CrossRef] [PubMed]
- Pan, F.; Ye, T.; Sun, P.; Gui, S.; Liang, B.; Li, L.; Zheng, D.; Wang, J.; Hesketh, R.L.; Yang, L.; et al. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology 2020, 295, 715–721. [Google Scholar] [CrossRef]
- Huang, G.; Gong, T.; Wang, G.; Wang, J.; Guo, X.; Cai, E.; Li, S.; Li, X.; Yu, Y.; Lin, L. Timely Diagnosis and Treatment Shortens the Time to Resolution of Coronavirus Disease (COVID-19) Pneumonia and Lowers the Highest and Last CT Scores from Sequential Chest CT. Am. J. Roentgenol. 2020, 215, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Bernheim, A.; Mei, X.; Huang, M.; Yang, Y.; Fayad, Z.A.; Zhang, N.; Diao, K.; Lin, B.; Zhu, X.; Li, K.; et al. Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. Radiology 2020, 295, 463. [Google Scholar] [CrossRef] [PubMed]
- Busi Rizzi, E.; Schinina, V.; Gentile, F.P.; Bibbolino, C. Reduced computed tomography radiation dose in HIV-related pneumonia: Effect on diagnostic image quality. Clin. Imaging 2007, 31, 178–184. [Google Scholar] [CrossRef] [PubMed]
- Cristofaro, M.; Rizzi, E.B.; Piselli, P.; Pianura, E.; Petrone, A.; Fusco, N.; Di Stefano, F. Image quality and radiation dose reduction in chest CT in pulmonary infection. Radiol. Med. 2020, 125, 451–460. [Google Scholar] [CrossRef]
- Mayo-Smith, W.W.; Hara, A.K.; Mahesh, M.; Sahani, D.V.; Pavlicek, W. How I Do It: Managing Radiation Dose in CT. Radiology 2014, 273, 657–672. [Google Scholar] [CrossRef]
- Smith-Bindman, R.; Wang, Y.; Chu, P.; Chung, R.; Einstein, A.J.; Balcombe, J.; Cocker, M.; Das, M.; Delman, B.N.; Flynn, M.; et al. International variation in radiation dose for computed tomography examinations: Prospective cohort study. BMJ 2019, 364, k4931. [Google Scholar] [CrossRef]
- Lumbreras, B.; Salinas, J.M.; Gonzalez-Alvarez, I. Cumulative exposure to ionising radiation from diagnostic imaging tests: A 12-year follow-up population-based analysis in Spain. BMJ Open 2019, 9, e030905. [Google Scholar] [CrossRef]
- Stopsack, K.H.; Cerhan, J.R. Cumulative Doses of Ionizing Radiation from Computed Tomography: A Population-Based Study. Mayo Clinic Proc. 2019, 94, 2011–2021. [Google Scholar] [CrossRef] [PubMed]
- Rubin, G.D.; Ryerson, C.J.; Haramati, L.B.; Sverzellati, N.; Kanne, J.P.; Raoof, S.; Schluger, N.W.; Volpi, A.; Yim, J.J.; Martin, I.B.; et al. The Role of Chest Imaging in Patient Management during the COVID-19 Pandemic: A Multinational Consensus Statement from the Fleischner Society. Radiology 2020, 296, 106–116. [Google Scholar] [CrossRef]
- Kalra, M.K.; Homayounieh, F.; Arru, C.; Holmberg, O.; Vassileva, J. Chest CT practice and protocols for COVID-19 from radiation dose management perspective. Eur. Radiol. 2020, 30, 6554–6560. [Google Scholar] [CrossRef]
- Homayounieh, F.; Kalra, M.K. COVID-19 and chest CT: Protocol and Dose Optimization, Webinar 9 April 2020 of International Atomic Energy Agency. Available online: http://ns-files.iaea.org/video/rpop-webinar-apr2020 (accessed on 9 April 2020).
- Sakane, H.; Ishida, M.; Shi, L.; Fukumoto, W.; Sakai, C.; Miyata, Y.; Ishida, T.; Akita, T.; Okada, M.; Awai, K.; et al. Biological Effects of Low-Dose Chest CT on Chromosomal DNA. Radiology 2020, 295, 439–445. [Google Scholar] [CrossRef]
- Hauptmann, M.; Daniels, R.D.; Cardis, E.; Cullings, H.M.; Kendall, G.; Laurier, D.; Linet, M.S.; Little, M.P.; Lubin, J.H.; Preston, D.L.; et al. Epidemiological Studies of Low-Dose Ionizing Radiation and Cancer: Summary Bias Assessment and Meta-Analysis. JNCI Monogr. 2020, 56, 188–200. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, A.R.; Charbel, S. Radiation dose reduction considerations and imaging patterns of ground glass opacities in coronavirus: Risk of over exposure in computed tomography. Radiol. Med. 2020, 1–18. [Google Scholar] [CrossRef]
- Homayounieh, F.; Holmberg, O.; Umairi, R.A.; Aly, S.; Basevičius, A.; Costa, P.R.; Darweesh, A.; Gershan, V.; Ilves, P.; Kostova-Lefterova, D.; et al. Variations in CT Utilization, Protocols, and Radiation Doses in COVID-19 Pneumonia: Results from 28 Countries in the IAEA Study. Radiology 2020, 298, E141–E151. [Google Scholar] [CrossRef]
- Lee, C. Managing Radiation Dose from Chest CT in COVID-19 Patients. Radiology 2021, 298, E158–E159. [Google Scholar] [CrossRef] [PubMed]
- Ameri, A.; Ameri, P.; Rahnama, N.; Mokhtari, M.; Sedaghat, M.; Hadavand, F.; Bozorgmehr, R.; Haghighi, M.; Taghizadeh-Hesary, F. Low-dose Whole-lung Irradiation for COVID-19 Pneumonia: Final Results of a Pilot Study. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 859–866. [Google Scholar] [CrossRef]
- Sanmamed, N.; Alcantara, P.; Cerezo, E.; Gaztañaga, M.; Cabello, N.; Gómez, S.; Bustos, A.; Doval, A.; Corona, J.; Rodriguez, G.; et al. Low dose radiotherapy in the management of COVID-19 pneumonia (LOWRAD-Cov19). Preliminary report. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 880–885. [Google Scholar] [CrossRef]
- Prasanna, P.G.; Woloschak, G.E.; DiCarlo, A.L.; Buchsbaum, J.C.; Schaue, D.; Chakravarti, A.; Cucinotta, F.A.; Formenti, S.C.; Guha, C.; Hu, D.J.; et al. Low-Dose RadiationTherapy (LDRT) for COVID-19: Benefits or Risks? Radiat. Res. 2020, 194, 452–464. [Google Scholar] [CrossRef]
- Mortazavi, A.; Mortazavi, S.M.J.; Sihver, L. Selective Pressure-Free Treatments for COVID-19. Radiation 2021, 1, 3. [Google Scholar] [CrossRef]
- Li, J.; Wang, X.; Huang, X.; Chen, F.; Zhang, X.; Liu, Y.; Luo, G.; Xu, X. Application of Care Dose 4D combined with Karl 3D technology in the low dose computed tomography for the follow-up of COVID-19. BMC Med. Imaging 2020, 20, 56. [Google Scholar] [CrossRef]

| Age, Gender and Dose in COVID-19 Patients | |||||||
|---|---|---|---|---|---|---|---|
| Age | Male (no) | Male (%) | Female (no) | Female (%) | % TOT | Mean (mSv) | Median (mSv) |
| 21–30 | 13 | 59.09 | 9 | 40.91 | 2.29 | 11.01 | 7.86 |
| 31–40 | 52 | 74.29 | 18 | 25.71 | 7.29 | 11.80 | 9.71 |
| 41–50 | 120 | 82.19 | 26 | 17.81 | 15.21 | 11.01 | 8.95 |
| 51–60 | 212 | 75.18 | 70 | 24.82 | 29.38 | 11.71 | 9.97 |
| 61–70 | 118 | 71.08 | 48 | 28.92 | 17.29 | 11.31 | 9.19 |
| 71–80 | 108 | 62.79 | 64 | 37.21 | 17.92 | 11.12 | 8.64 |
| 81–90 | 48 | 52.17 | 44 | 47.83 | 9.58 | 10.33 | 7.64 |
| >90 | 2 | 20.00 | 8 | 80.00 | 1.04 | 10.91 | 9.99 |
| Age, Gender and Dose in Patients 2019 | |||||||
|---|---|---|---|---|---|---|---|
| Age | Male (no) | Male (%) | Female (no) | Female (%) | % TOT | Mean (mSv) | Median (mSv) |
| <20 | 5 | 71.43 | 2 | 28.57 | 0.73 | 5.72 | 3.45 |
| 21–30 | 37 | 68.52 | 17 | 31.48 | 5.63 | 5.90 | 5.38 |
| 31–40 | 64 | 71.91 | 25 | 28.09 | 9.27 | 7.03 | 5.40 |
| 41–50 | 77 | 60.63 | 50 | 39.37 | 13.23 | 7.19 | 6.01 |
| 51–60 | 176 | 67.95 | 83 | 32.05 | 26.98 | 8.62 | 7.38 |
| 61–70 | 135 | 67.84 | 64 | 32.16 | 20.73 | 7.41 | 6.58 |
| 71–80 | 97 | 57.74 | 71 | 42.26 | 17.50 | 8.20 | 8.00 |
| 81–90 | 47 | 65.28 | 25 | 34.72 | 7.50 | 7.78 | 7.14 |
| >90 | 0 | 0 | 3 | 100 | 0.31 | 8.05 | 6.68 |
| Dose Per Person Exposed in COVID-19 Patients and Control Group | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| COVID-19 Patients | No COVID Patients (2019) | ||||||||
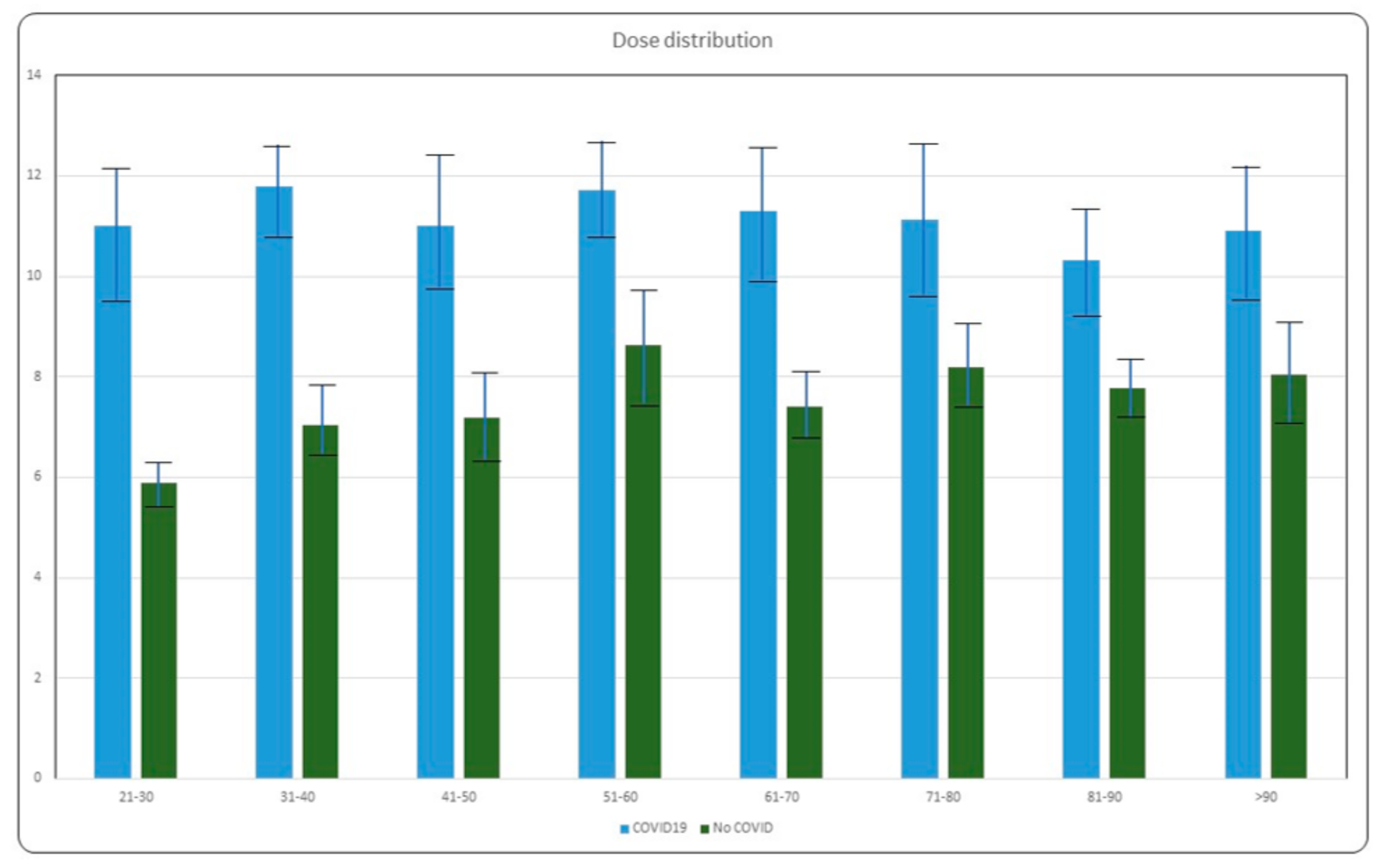
| Age | Mean (mSv) | Median (mSv) | Standard Deviation | 90 Percent | Mean (mSv) | Median (mSv) | Standard Deviation | 90 Percent | p Value |
| 21–30 | 11.01 | 7.86 | 7.29 | 5.38 | 5.90 | 5.38 | 3.78 | 1.53 | 0.022 |
| 31–40 | 11.80 | 9.71 | 9.71 | 5.43 | 7.03 | 5.40 | 4.40 | 2.55 | 0.051 |
| 41–50 | 11.01 | 8.95 | 6.41 | 5.20 | 7.19 | 6.01 | 4.57 | 2.51 | 0.001 |
| 51–60 | 11.71 | 9.97 | 5.66 | 5.40 | 8.62 | 7.38 | 4.75 | 3.31 | 0.042 |
| 61–70 | 11.31 | 9.19 | 6.07 | 5.38 | 7.43 | 6.58 | 3.75 | 3.35 | 0.001 |
| 71–80 | 11.12 | 8.64 | 4.40 | 5.38 | 8.20 | 8.00 | 3.84 | 3.40 | 0.001 |
| 81–90 | 10.33 | 7.64 | 6.23 | 4.31 | 7.78 | 7.14 | 3.61 | 3.42 | 0.002 |
| >90 | 10.91 | 9.99 | 5.18 | 10.73 | 8.05 | 6.68 | 3.53 | 5.38 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cristofaro, M.; Fusco, N.; Petrone, A.; Albarello, F.; Di Stefano, F.; Pianura, E.; Schininà, V.; Ianniello, S.; Campioni, P. Increased Radiation Dose Exposure in Thoracic Computed Tomography in Patients with Covid-19. Radiation 2021, 1, 153-161. https://doi.org/10.3390/radiation1020014
Cristofaro M, Fusco N, Petrone A, Albarello F, Di Stefano F, Pianura E, Schininà V, Ianniello S, Campioni P. Increased Radiation Dose Exposure in Thoracic Computed Tomography in Patients with Covid-19. Radiation. 2021; 1(2):153-161. https://doi.org/10.3390/radiation1020014
Chicago/Turabian StyleCristofaro, Massimo, Nicoletta Fusco, Ada Petrone, Fabrizio Albarello, Federica Di Stefano, Elisa Pianura, Vincenzo Schininà, Stefania Ianniello, and Paolo Campioni. 2021. "Increased Radiation Dose Exposure in Thoracic Computed Tomography in Patients with Covid-19" Radiation 1, no. 2: 153-161. https://doi.org/10.3390/radiation1020014
APA StyleCristofaro, M., Fusco, N., Petrone, A., Albarello, F., Di Stefano, F., Pianura, E., Schininà, V., Ianniello, S., & Campioni, P. (2021). Increased Radiation Dose Exposure in Thoracic Computed Tomography in Patients with Covid-19. Radiation, 1(2), 153-161. https://doi.org/10.3390/radiation1020014






