Abstract
Background: Due to social behavior modulation contribution, synthetic oxytocin (synOT) has been routinely used to augment or induce labor. Aim: The present study examined the association between intrapartum synOT administration and maternal postpartum depression (PPD) using an observational prospective study on women who delivered in our department on the 2nd day postpartum. Methods: This study was conducted in our University Emergency County Hospital between August 2019 and April 2021. We included 904 women, of whom 609 (67.36%) received synOT and 295 (32.63%) did not receive synOT during the intrapartum period. Using the Edinburgh Postpartum Depression Scale, we showed that 26.10% of women had PPD and 73.89% of women did not have PPD. Demographic participant characteristics (i.e., age, parity, ethnicity, delivery type, and postpartum hospitalization days) were assessed. Results: Our results show that the rate of PPD was lower in women with synOT administration in comparison with women without synOT administration (p < 0.001). Younger age and shorter hospitalization days of the women with synOT were statistically significant in comparison with women without synOT administration (p < 0.001). Further, primiparous women with spontaneous delivery were positively associated with synOT administration (p < 0.001). Conclusions: Our study sustained that synOT could represent a potential mediator on the PPD prevalence. These results suggest that intrapartum synOT administration may offer a potential benefit to mothers at risk of PPD.
1. Introduction
The rate of postpartum depression (PPD) together with other disorders reaches from 12.9 to 20.4% [1,2]. When not diagnosed in time, PPD could cause harmful effects to mothers, newborns, and their relatives. Starting with the 1950s, synthetic oxytocin (synOT) has been used for the augmentation of labor induction including postpartum hemorrhage prevention [3]. Although many studies explore different roles of the natural or synOT hormone in the intrapartum period, to the present, no other studies are convincing regarding the association between OT and PPD [4].
Considering the antidepressant mechanisms of serotonin [5] and functional connectivity, there is a gap in that response knowledge on sex differences [6]. The neuroendocrine system could be altered by the experience of pregnancy and parturition, which may alter the antidepressive effect [7]. Therefore, a higher interest in the impact of antidepressants on neuroendocrine systems relevant to PPD is growing. OT, which is a neuropeptide that mediates social behaviors such as maternal [8] and sexual behaviors [9], may play a role in PPD [10]. The reorganization of key neural structures in the hypothalamus and hippocampus by OT was shown to have taken place more postpartum [11].
Recently, OT has been identified as a potential mediator of PPD and anxiety [11]. Research studies have noted the relationship between maternal plasma OT and depressive symptomology and found that decreased OT synthesized during pregnancy is associated with increased depressive symptoms, suggesting that administering synOT, such as the synOT Pitocin, could prevent PPD [12]. Some studies noted that low endogenous OT has been associated with a higher risk of PPD [10], and synOT administration has been proposed as a primary treatment [13]. In the common depressed population, the role of OT was shown to be different from that of depressed mothers, leading to better OT effect determination, especially in PPD [14]. OT is mostly produced in the paraventricular and supraoptic nuclei in the hypothalamus and is necessary in both labor and lactation [15]. It also has been bounded on different neuropsychiatric conditions [16]. Some studies found that the increasing release of OT during pregnancy could be involved in the prevention of PPD [11]. The results of Apter-Levy and contributors showed that OT-based intervention had the potential to improve mother-to-child connection under the negative influence of chronic maternal depression [17].
The literature on the role of synOT administration immediately after delivery results is still conflicting. Another study found that the dose of synOT given during labor was positively correlated with both endogenous levels of OT and depressive symptoms at 2 months postpartum [18]. However, the literature provides maintenance that higher OT values are related to positive postpartum maternal behaviors [19]. Furthermore, the level of OT in maternal human plasma has been associated with emotional binding [20], including mother-to-child attachment. Studies exist that accentuate the role of OT in perinatal stages and depression binding [21]. Although there is an interest in OT use as a potential target in PPD, little information exists on the use of synOT in clinical practice. For these reasons, there is a growing demand for improving PPD therapies. Today, first-line therapies include psychotherapy or talk therapy along with social healthcare [22], although available therapies have less than a 50% rate of success in severe cases [23]. Together with these therapies, synOT is included, which is a hormone with different potential in promoting positive behavior and social memories [24]. It was shown that in patients with anxiety, a single synOT does attenuate negative thoughts in stressful situations [25]. With all this, the World Health Organization recommends that synOT should be used only in the active phase of labor [26].
Given the importance of PPD, the critical role of synOT in the postpartum period, and the high frequency of synOT administration in the peripartum period, updated data on synOT and PPD are needed. The objective of this study was to examine the association between intrapartum synOT administration and maternal development of PPD by using the Edinburgh Postnatal Depression Scale (EPDS) as a screening test on the 2nd day postpartum. We hypothesized that women exposed to intrapartum synOT would have a reduced risk of PPD compared to those without synOT administration.
2. Materials and Methods
2.1. Study Design and Participants
We conducted an observational prospective study on women in the intrapartum and postpartum periods who delivered in the Obstetrics and Gynecology Department of the “Sf. Apostle Andrei” University Emergency County Hospital Constanta, in Romania. All participants were informed regarding the aims and procedures, and the questionnaire was voluntary and confidential. The participants had the possibility to withdraw from this study at any point. Before this study started, we obtained informed consent from all participants in this study. Between August 2019 and April 2021, we included 904 women from the 2nd day after delivery. Considering the fact that maternity blues, which include low mood and mild depressive symptoms, can be developed in the first days after delivery, we choose to better differentiate the depression state because a shared definition is still not available. Moreover, maternity blues is a well-established risk factor for shifting to more severe postpartum mood disorders, such as PPD [27]. The EPDS is commonly the most widely used scale to assess depressive symptoms in the postpartum period. Recently, Zanardo and contributors showed that women with potential maternity blues represent a distinct subgroup of postpartum women at increased risk of depression symptoms [28]. Participants were recruited by convenience, and EPDS was used as a screening test for women at risk of PPD [29]. According to the EPDS score, in which a score of ≥10 could indicate PPD (i.e., possible depression), we allocated the mothers in two groups: women with PPD (n = 236) and controls (i.e., women without PPD, n = 668) for better differentiation of symptoms. This allowed us to select patients who needed a closer follow-up during the immediate postpartum period.
2.2. Demographic Characteristics
The demographic and clinical features of the analyzed women concerning age, parity, ethnicity, delivery type, and postpartum hospitalization days were extracted from electronic and medical file records.
2.3. Inclusion and Exclusion Criteria
We included 18–45-year-old women who delivered a single baby. We excluded women with (1) age less than 18 and more than 45; (2) women with multiple pregnancies; (3) women who had a psychiatric disorder that required treatment or not; (4) women with alcohol or drug abuse; and (5) women who could not read or speak the Romanian language. All the participants completed the EPDS questionnaire.
2.4. Intrapartum Synthetic Oxytocin
In the intrapartum period, synOT was intravenously administered to selected women, including but not limited to augmentation or labor induction by synOT when natural labor had begun. This was registered as ‘yes’ and ‘no’, and the exact dose was provided depending on medical need. These data were extracted from medical file records entered by our specialists.
All participants were informed of the aims and procedures and had the option to withdraw from this study at any time. This study was conducted in accordance with the Helsinki Declaration on Human Rights, and the informed consent from all participants in this study as well as the Agreement of the Ethics Commission (No. 29726/31.05.2021) were obtained.
2.5. Statistical Analysis
The statistical analysis in this study was carried out utilizing IBM SPSS statistics software version 28 (Armonk, NY, USA: IBM Corp) as well as Microsoft Excel. The analytical techniques employed included descriptive statistics, represented in the form of graphs, and statistical assessments. Data are presented as mean, standard deviation, median, minimum and maximum for continuous variables, or as percentages for categorical variables. For hypothesis testing, an independent samples T-test or the Wilcoxon sum rank test was used, as appropriate. For testing associations between variables, the Chi-squared test or Fisher’s exact test was used. For rxc tables with r, c > 2, we used the Fisher–Freeman–Halton exact test, depending on the type of analyzed variables and the data. For contingency tables with multiple rows or columns, we used the pairwise z-test with Bonferroni correction for comparing column proportions. The significance level was set at 0.05.
3. Results
From the total number of patients (n = 904), the presence of PPD was detected in 26.10% (n = 236) women. Our results showed that from the total of 904 women involved in this study, 609 (67.36%) women received synOT, and 295 (32.63%) women did not receive synOT. Therefore, it was shown that the rate of PPD was lower in women with synOT administration, in comparison with the women without synOT administration (21% vs. 37%, p < 0.001), being statistically significant. In our study, synOT was administered to selected women for induction of labor (Figure 1).
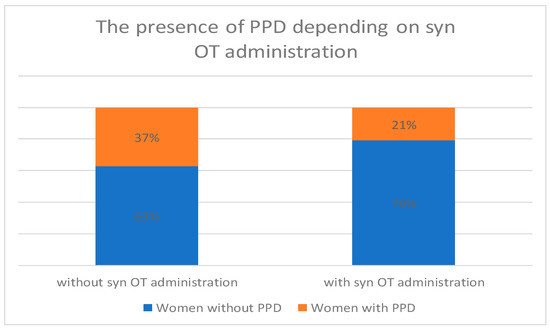
Figure 1.
The rate of intrapartum synOT administration in women with or without PPD.
The demographic characteristics of participants with or without intrapartum synOT administration are represented in Table 1.

Table 1.
Demographic characteristics of participants with or without intrapartum synOT administration.
The mean age of the women with synOT administration was younger in comparison with women without synOT administration (27.4 vs. 29.23, p < 0.001), being statistically significant, sustaining that synOT administration could have different implications in such a group of women.
We also observed a higher percentage of primiparous women in the group with synOT administration compared to women in the without synOT group (53.85% vs. 36.94%, p < 0.001). These results suggest a higher proportion of primiparous women who received synOT. From the women with synOT administration, 25.94% were secundipara and 20.19% were women with three or more deliveries. From the women without synOT administration, 49.83% were secundipara and only 13.21% were women with three or more deliveries.
In terms of ethnicity, the differences in distribution were also statistically significant (p < 0.001). The percentage of Romanian women was significantly higher in the without synOT group (86%) compared to women with synOT administration (80%). From the women with synOT administration, 13.3% were Gypsy, and Russian and Syrian women had the same percentages (i.e., 0.16%), and 5.9% were Turkish women. From the women without synOT administration, there were seen similar percentages for Gypsy and Turkish women (i.e., 6.77%), without any Russian or Syrian women.
There was also a statistical significance between delivery types from both women groups. The majority of the women with synOT administration had a spontaneous vaginal delivery compared with the women without synOT administration (i.e., 74.38% vs. 6.77%, p < 0.001). The rate of cesarean section was 25.91% for women with synOT administration and 93.22% for women without synOT administration.
It was noted that women with synOT administration were having fewer hospitalization days in comparison with women without synOT administration (i.e., 2.65 vs. 2.77, p < 0.001). This also shows that fewer hospitalization days were associated with synOT administration, as the hospitalization time was shorter for women receiving synOT.
4. Discussion
There is still an aversion to the use of antidepressants in PPD treatments, knowing the side effects or the incapability in using it during breastfeeding [30]. Such reasons make OT an important candidate in mothers with PPD, being a natural hormone involved in birth, mother–newborn bonding, and breastfeeding. Currently, OT is involved in emotion regulation [31], emotion recognition [32], facial communication [33], or eye contact [34]. After daily OT administration together with 12 sessions of a weekly course of psychotherapy, Clarici and contributors [35] assessed depression symptoms, without any significant differences in low mood between synOT administration and controls.
When used as advised, synOT has immediate medical benefits. By mimicking the body’s natural OT system, it stimulates contractions and prevents postpartum hemorrhage. No evidence-based guidelines regarding the dose or patient response exist, and the decision to administer synOT is taken more subjectively [36]. Possible synOT risks associated include uterine hyperstimulation and fetal distress, including abnormal fetal heart rate and uterine rupture [37].
The effect of synOT as an antidepressive and anxiolytic mediator could be due to many results achieved with intranasal administration in which clinical trials used a dose ranging from 18 to 40 IU [38]. It could be possible that the effects of synOT on different receptors are moderated by gender, dose, and the time of application. Interestingly, the effects of synOT on social cognition and social integration are nuanced, depending in the end on the individual’s personal behavior [39]. This synOT feature could also inform future policy concerning usage in labor management at specific doses and timings [40].
Another study sustained the opposite effect of synOT, in which women exposed to synOT were more likely to have depressive symptoms in the postpartum period. The results show that there was a difference between natural oxytocin and synOT, in which synOT does not present effects on neuroendocrine mechanisms of the brain, without influencing the maternal mood [41]. Therefore, only synOT showed to be able to cross the placenta and downregulate fetal OT receptors. Further, synOT has also been shown to elicit uterine hyperstimulation, giving a reverse impact on fetal oxygen saturation [42]. However, there is mixed evidence until the present [43], although synOT administered intrapartum showed that it does not immediately affect maternal mood but only weeks after childbirth. The same study suggests that women exposed to intrapartum synOT would be at a lower risk of the early postpartum mood named maternity blues and then PPD, compared to women without such exposure. Further, this study showed that the effects of synOT would be more obvious immediately after delivery, which attenuates over time [43].
The exact role of synOT administration in the intrapartum period and the association with PPD are still scarce nowadays. Some studies investigated the bond between maternal plasma OT and depressive symptoms [44]. One study aimed to use lactation as a physiologic challenge to quantify the extent to which feelings, stress, and anxiety symptoms are associated with reduced OT during breastfeeding. The authors followed the expected OT levels in all breastfeeding women, in which OT rose immediately after the beginning of the feed [44]. It was shown that one single dose of synOT administered during labor was firmly correlated with both endogenous OT levels and depression at 2 months postpartum. Furthermore, in breastfeeding women, lower doses of synOT were observed compared with exclusively formula-feeding women at 2 months postpartum. In contrast, a higher synOT dose was associated with significantly greater symptoms of depression, anxiety, and somatization at 2 months postpartum [20]. The data suggest that intrapartum synOT administration may have negative effects on the mother’s mood only several weeks after birth [45]. Considering the fact that 22% of births are induced by using synOT administration from 4 million total births in the United States since 2014 [46], little research has been carried out on the follow-up around synOT impact or as potential mediation on PPD. Our study showed that intrapartum exposure to synOT may alleviate the risk of developing PPD symptoms in new mothers with higher impact (p < 0.001). Therefore, women with synOT administration were much younger, and the majority of them were primiparous in comparison with those without synOT administration (p < 0.001); and the majority of the women had spontaneous delivery and had fewer postpartum hospitalization days compared with women without synOT administration (p < 0.001). Interestingly, the administration of synOT showed not to have such an impact on ethnicity participants.
In contradiction with our study, Kroll-Desrosiers and contributors [40] and Gu and contributors [18] found that women with intrapartum synOT administration were at a higher risk of depression and anxiety than women without synOT administration. This mismatch could be explained by a different synOT dosage in the intrapartum period. When synOT was suboptimally used, it led to an excessively short and painful labor or, on the contrary, to a longer labor with complications associated with PPD [47]. Therefore, the association between synOT administration and PPD appearance could be indicated by each birth experience. The study of Hinshaw et al. [48] showed that nulliparous women with primary dysfunctional labor and synOT induction showed that it does not reduce cesarean section or short-term postnatal depression.
Our study did not measure endogenous OT also in the analyzed women with or without synOT administration. It has been wise to compare the endogenous and synOT in the same women’s sample, considering the fact that the endogenous level of OT is at higher risk of PPD than recommended synOT administration. Larger studies should assess PPD at different time points, in which the results could shed more light on the association between synOT and PPD.
5. Conclusions
The results show that women exposed to intrapartum synOT would have a reduced risk of PPD compared with those without synOT administration. Our study sustained that synOT could represent a potential mediator for PPD prevalence, which could be clinically safer in different labor conditions.
Author Contributions
Conceptualization, S.O. and V.T.; methodology, S.O. and D.B.; validation, S.O. and V.T.; formal analysis, S.O. and M.R.; data curation, S.O. and D.B.; writing—original draft preparation, S.O. and D.B.; writing—review and editing, S.O., C.D. and V.T.; supervision, V.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Helsinki Declaration on Human Rights. The informed consent from all participants in this study as well as the Agreement of the Ethics Commission from University Emergency County Hospital Constanta were obtained (No. 29726/31.05.2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Andersson, A.; Garcia-Argibay, M.; Viktorin, A.; Ghirardi, L.; Butwicka, A.; Skoglund, C.; Bang Madsen, K.; D’onofrio, B.M.; Lichtenstein, P.; Tuvblad, C.; et al. Depression and anxiety disorders during the postpartum period in women diagnosed with attention deficit hyperactivity disorder. J. Affect. Disord. 2023, 325, 817–823. [Google Scholar] [CrossRef]
- Kendall-Tackett, K.A. Screening for perinatal depression: Barriers, guidelines, and measurement scales. J. Clin. Med. 2024, 13, 6511. [Google Scholar] [CrossRef]
- Fields, H.; Greene, J.W.J.; Franklin, R.R. Intravenous pitocin in induction and stimulation of labor: A study of 3754 cases. Obstet. Gynecol. 1959, 13, 353–359. [Google Scholar] [PubMed]
- Biaggi, A.; Conroy, S.; Pawlby, S.; Pariante, C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016, 191, 62–77. [Google Scholar] [CrossRef]
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. Evolving knowledge of sex differences in brain structure, function, and chemistry. Biol. Psychiatry 2007, 62, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Keers, R.; Aitchison, K.J. Gender differences in antidepressant drug response. Int. Rev. Psychiatry 2010, 22, 485–500. [Google Scholar] [CrossRef] [PubMed]
- Le’vy, F. Neuroendocrine control of maternal behavior in non-human and human mammals. Ann. Endocrinol. 2016, 77, 114–125. [Google Scholar] [CrossRef]
- Carter, C.S. Oxytocin pathways and the evolution of human behavior. Annu. Rev. Psychol. 2014, 65, 17–39. [Google Scholar] [CrossRef]
- Borrow, A.P.; Cameron, N.M. The role of oxytocin in mating and pregnancy. Horm. Behav. 2012, 61, 266–276. [Google Scholar] [CrossRef]
- McQuaid, R.J.; McInnis, O.A.; Abizaid, A.; Anisman, H. Making room for oxytocin in understanding depression. Neurosci. Biobehav. Rev. 2014, 45, 305–322. [Google Scholar] [CrossRef]
- Skrundz, M.; Bolten, M.; Nast, I.; Hellhammer, D.H.; Meinlschmidt, G. Plasma oxytocin concentration during pregnancy is associated with development of postpartum depression. Neuropsychopharmacology 2011, 36, 1886–1893. [Google Scholar] [CrossRef] [PubMed]
- Garfield, L.; Giurgescu, C.; Carter, C.S.; Holditch-Davis, D.; McFarlin, B.L.; Schwertz, D.; Seng, J.S.; White-Traut, R. Depressive symptoms in the second trimester relate to low oxytocin levels in African-American women: A pilot study. Arch. Women’s Ment. Health 2015, 18, 123–129. [Google Scholar] [CrossRef][Green Version]
- Kim, S.; Soeken, T.A.; Cromer, S.J.; Martinez, S.R.; Hardy, L.R.; Strathearn, L. Oxytocin and postpartum depression: Delivering on what’s known and what’s not. Brain Res. 2014, 1580, 219–232. [Google Scholar] [CrossRef]
- Mah, B.L. Oxytocin, postnatal depression, and parenting: A systematic review. Harv. Rev. Psychiatry 2016, 24, 1–13. [Google Scholar] [CrossRef]
- Zagrean, A.M.; Georgescu, I.A.; Iesanu, M.I.; Ionescu, R.B.; Haret, R.M.; Panaitescu, A.M.; Zagrean, L. Oxytocin and vasopressin in the hippocampus. Vitam. Horm. 2022, 118, 83–127. [Google Scholar] [PubMed]
- Liu, N.; Yang, H.; Han, L.; Ma, M. Oxytocin in women’s health and disease. Front. Endocrinol. 2022, 13, 786271. [Google Scholar] [CrossRef] [PubMed]
- Apter-Levy, Y.; Feldman, M.; Vakart, A.; Ebstein, R.P.; Feldman, R. Impact of maternal depression across the first 6 years of life on the child’s mental health, social engagement, and empathy: The moderating role of oxytocin. Am. J. Psychiatry 2013, 170, 1161–1168. [Google Scholar] [CrossRef]
- Gu, V.; Feeley, N.; Gold, I.; Hayton, B.; Robins, S.; Mackinnon, A.; Samuel, S.; Carter, C.S.; Zelkowitz, P. Intrapartum synthetic oxytocin and Iis effects on maternal well-being at 2 months postpartum. Birth 2016, 43, 28–35. [Google Scholar] [CrossRef]
- Feldman, R.; Gordon, I.; Zagoory-Sharon, O. Maternal and paternal plasma, salivary, and urinary oxytocin and parent- infant synchrony: Considering stress and affiliation components of human bonding. Dev. Sci. 2011, 14, 752–761. [Google Scholar] [CrossRef]
- Pierzynowska, K.; Gaffke, L.; Żabińska, M.; Cyske, Z.; Rintz, E.; Wiśniewska, K.; Podlacha, M.; Węgrzyn, G. Roles of the oxytocin receptor (OXTR) in human diseases. Int. J. Mol. Sci. 2023, 24, 3887. [Google Scholar] [CrossRef]
- Mohiyeddini, C.; Opacka-Juffry, J. Disentangling the link between depressive symptoms and plasma oxytocin in men: The role of brooding rumination. Horm. Behavior. 2015, 75, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Batt, M.M.; Duffy, K.A.; Novick, A.M.; Metcalf, C.A.; Epperson, C.N. Is postpartum depression different from depression occurring outside of the perinatal period? A review of the evidence. Focus 2020, 18, 106–119. [Google Scholar] [CrossRef] [PubMed]
- Dimcea, D.A.M.; Petca, R.C.; Dumitrașcu, M.C.; Șandru, F.; Mehedințu, C.; Petca, A. Postpartum depression: Etiology, treatment, and Consequences for Maternal Care. Diagnostics 2024, 14, 865. [Google Scholar] [CrossRef] [PubMed]
- Stroobants, S.; Creemers, J.; Bosmans, G.; D’Hooge, R. Post-weaning infant-to-mother bonding in nutritionally independent female mice. PLoS ONE 2020, 15, e0227034. [Google Scholar] [CrossRef]
- Jones, C.; Barrera, I.; Brothers, S.; Ring, R.; Wahlestedt, C. Oxytocin and social functioning. Dialogues Clin. Neurosci. 2017, 19, 193–201. [Google Scholar] [CrossRef]
- Westhoff, G.; Cotter, A.M.; Tolosa, J.E. Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database Syst. Rev. 2013, 10, 1–93. [Google Scholar] [CrossRef]
- Tosto, V.; Ceccobelli, M.; Lucarini, E.; Tortorella, A.; Gerli, S.; Parazzini, F.; Favilli, A. Maternity Blues: A Narrative Review. J. Pers. Med. 2023, 13, 154. [Google Scholar] [CrossRef]
- Zanardo, V.; Volpe, F.; de Luca, F.; Giliberti, L.; Giustardi, A.; Parotto, M.; Straface, G.; Soldera, G. Maternity Blues: A Risk Factor for Anhedonia, Anxiety, and Depression Components of Edinburgh Postnatal Depression Scale. J. Matern. Fetal Neonatal. Med. 2019, 33, 3962–3968. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Pettman, D.; O’Mahen, H.; Blomberg, O.; Svanberg, A.S.; von Essen, L.; Woodford, J. Effectiveness of cognitive behavioural therapy-based interventions for maternal perinatal depression: A systematic review and meta-analysis. BMC Psychiatry 2023, 23, 208. [Google Scholar] [CrossRef]
- Shahrestani, S.; Kemp, A.H.; Guastella, A.J. The impact of a single administration of intranasal oxytocin on the recognition of basic emotions in humans: A meta-analysis. Neuropsychopharmacology 2013, 38, 1929–1936. [Google Scholar] [CrossRef]
- Whitley, J.; Wouk, K.; Bauer, A.E.; Grewen, K.; Gottfredson, N.C.; Meltzer-Brody, S.; Propper, C.; Mills-Koonce, R.; Pearson, B.; Stuebe, A. Oxytocin during breastfeeding and maternal mood symptoms. Psychoneuroendocrinology 2020, 113, 104581. [Google Scholar] [CrossRef] [PubMed]
- Daughters, K.; Manstead, A.S.R.; van der Schalk, J. Oxytocin and emotion recognition: Investigating the possible roles of facial synchrony and eye gaze. Curr. Res. Ecol. Soc. Psychol. 2021, 2, 100019. [Google Scholar] [CrossRef]
- Auyeung, B.; Lombardo, M.V.; Heinrichs, M.; Chakrabarti, B.; Sule, A.; Deakin, J.B.; Bethlehem, R.A.; Dickens, L.; Mooney, N.; Sipple, J.A.; et al. Oxytocin increases eye contact during a real-time, naturalistic social interaction in males with and without autism. Transl. Psychiatry 2015, 5, e507. [Google Scholar] [CrossRef]
- Clarici, A.; Pellizzoni, S.; Guaschino, S.; Alberico, S.; Bembich, S.; Giuliani, R.; Short, A.; Guarino, G.; Panksepp, J. Intranasal administration of oxytocin in postnatal depression: Implications for psychodynamic psychotherapy from a randomized double-blind pilot study. Front. Psychol. 2015, 6, 426. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.L.; Simpson, K.R.; Knox, G.E.; Garite, T.J. Oxytocin: New perspectives on an old drug. Am. J. Clin. Exp. Obstet. Gynecol. 2009, 200, 31–36. [Google Scholar]
- Buckley, S.J. Undisturbed birth: Nature’s blueprint for ease and ecstasy. J. Prenat. Perinat. Psychol. Health. 2003, 17, 261–288. [Google Scholar]
- MacDonald, E.; Dadds, M.R.; Brennan, J.L.; Williams, K.; Levi, F.; Cauchi, A.J. A review of safety, side-effects and subjective reactions to intranasal oxytocin in human research. Psychoneuroendocrinology 2011, 36, 1114–1126. [Google Scholar] [CrossRef]
- Bartz, J.A.; Zaki, J.; Bolger, N.; Ochsner, K.N. Social effects of oxytocin in humans: Context and person matter. Trends. Cogn. Sci. 2011, 15, 301–309. [Google Scholar] [CrossRef]
- Kroll-Desrosiers, A.R.; Nephew, B.C.; Babb, J.A.; Guilarte-Walker, Y.; Moore Simas, T.A.; Deligiannidis, K.M. Association of peripartum synthetic oxytocin administration and depressive and anxiety disorders within the first postpartum year. Depress. Anxiety 2017, 34, 137–146. [Google Scholar] [CrossRef]
- Nilvér, H.; Berg, M. The birth companions’ experience of the birthing room and how it influences the supportive role: A qualitative study. HERD Health Environ. Res. Des. J. 2023, 16, 156–167. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Liu, W.; Xu, Y.; Zhang, X.; Miao, Y.; Wang, A.; Zhang, Y. Effects of different doses of synthetic oxytocin on neonatal instinctive behaviors and breastfeeding. Sci. Rep. 2022, 12, 16434. [Google Scholar] [CrossRef] [PubMed]
- Takács, L.; Seidlerová, J.M.; Štěrbová, Z.; Čepický, P.; Havlíček, J. The effects of intrapartum synthetic oxytocin on maternal postpartum mood: Findings from a prospective observational study. Arch. Women’s Ment. Health 2019, 22, 485–491. [Google Scholar] [CrossRef]
- Nagel, E.M.; Howland, M.A.; Pando, C.; Stang, J.; Mason, S.M.; Fields, D.A.; Demerath, E.W. Maternal psychological distress and lactation and breastfeeding outcomes: A narrative review. Clin. Ther. 2022, 44, 215–227. [Google Scholar] [CrossRef] [PubMed]
- Cuthbert, B.N.; Insel, T.R. Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Med. 2013, 11, 126. [Google Scholar] [CrossRef]
- Hamilton, B.E.; Martin, J.A.; Osterman, M.J.; Curtin, C.S.; Matthews, T.J. Births: Final data for 2014. Natl. Vital Stat. Rep. 2014, 64, 1–63. [Google Scholar]
- Simkin, P. Just another day in a woman’s life? Women’s long-term perceptions of their first birth experience. Part I. Birth 1991, 18, 203–210. [Google Scholar] [CrossRef]
- Hinshaw, K.; Simpson, S.; Cummings, S.; Hildreth, A.; Thornton, J. A randomised controlled trial of early versus delayed oxytocin augmentation to treat primary dysfunctional labour in nulliparous women. BJOG 2008, 115, 1289–1295. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).