Mindfulness Interventions for Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
1.1. Drug Treatments for ADHD
1.2. Non-Drug Treatments for ADHD
1.3. Alternative Approaches
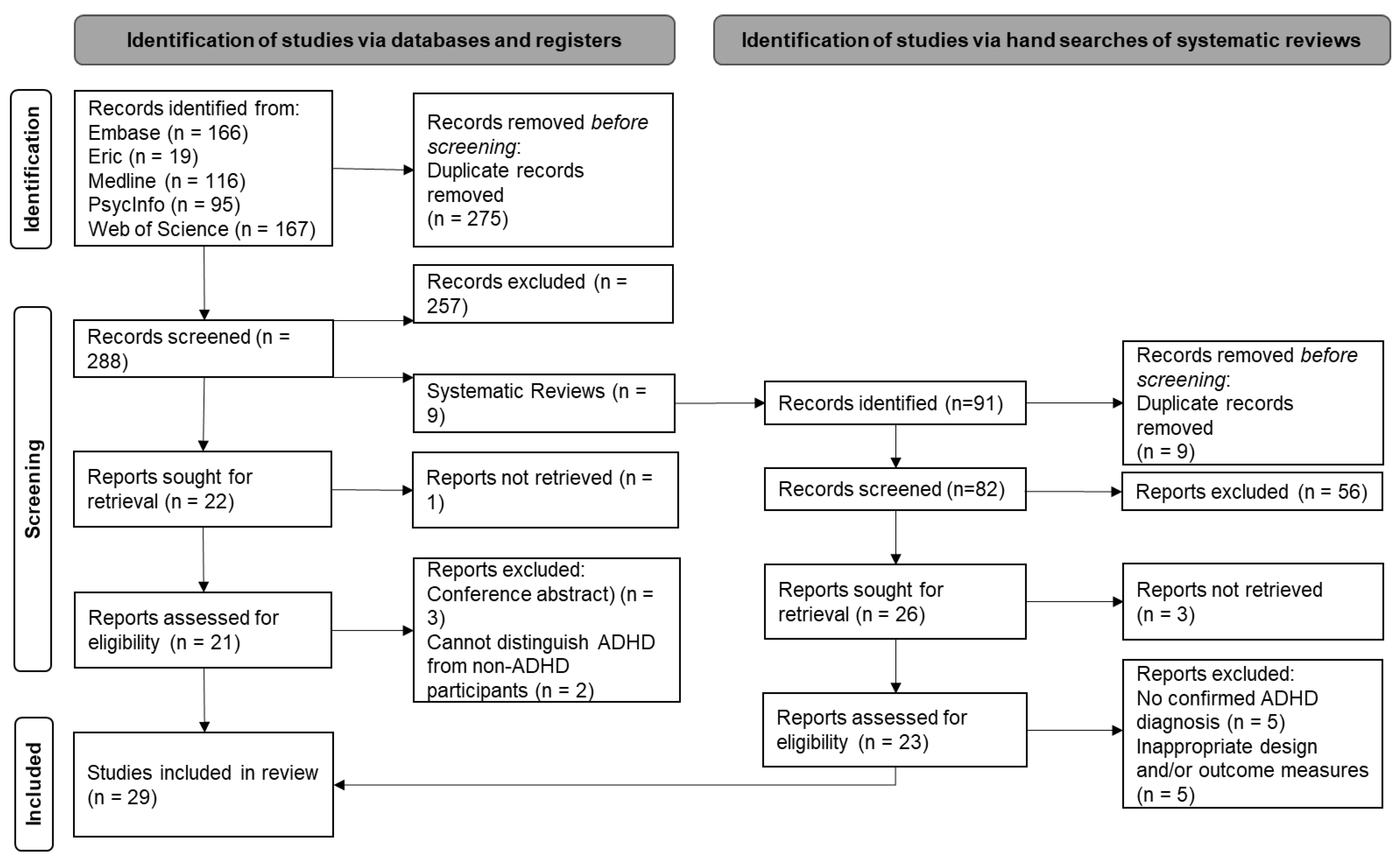
2. Materials and Methods
2.1. Protocol Registration
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Collection
2.5. Quality Assessment
2.6. Data Analysis
3. Results
3.1. Risk of Bias and Quality Assessment
3.2. Study Design
3.3. Participants
3.4. Intervention Approaches
3.5. Outcome Measures
3.5.1. Adult Studies
3.5.2. Child Studies
3.5.3. Family Studies
3.5.4. Parent Studies
3.6. The Effects of Mindfulness Interventions
3.6.1. ADHD Symptoms Scales
3.6.2. Executive Function Scales
3.6.3. Emotional Dysregulation Scales
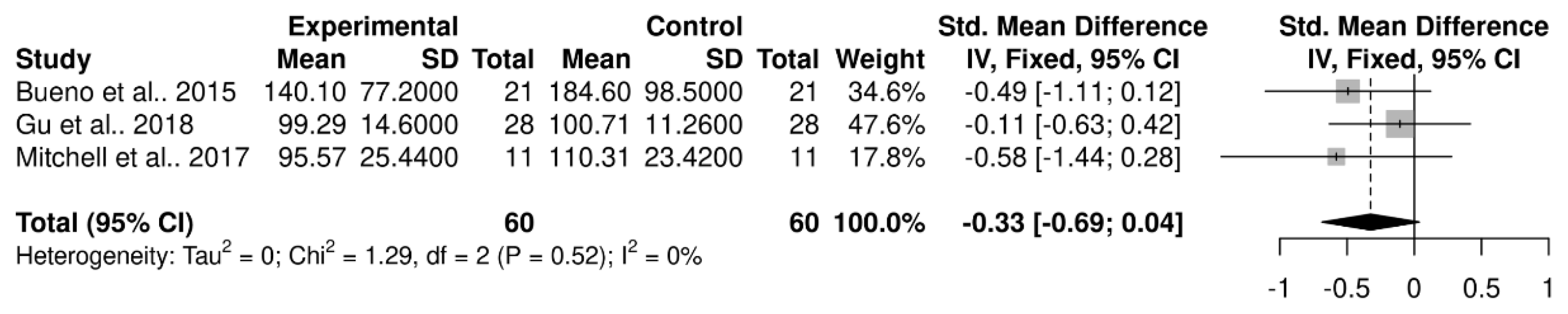
3.6.4. Objective Measures of ADHD-Related Behaviours
3.6.5. Wider Health Outcomes
- Quality of Life
- Depression and Anxiety
- Stress
- General behaviour
- Self-compassion
- Wellbeing
- Sleep
- Social skills
- Parenting Style
- Family Functioning
3.6.6. Mindfulness Practice
3.6.7. Intervention Feasibility and Satisfaction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Polanczyk, G.V.; Willcutt, E.G.; Salum, G.A.; Kieling, C.; Rohde, L.A. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int. J. Epidemiol. 2014, 43, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.; Sanders, S.; Doust, J.; Beller, E.; Glasziou, P. Prevalence of Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-analysis. Pediatrics 2015, 135, e994–e1001. [Google Scholar] [CrossRef] [PubMed]
- Faraone, S.V.; Biederman, J.; Mick, E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychol. Med. 2005, 36, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Moffitt, T.E.; Houts, R.; Asherson, P.; Belsky, D.W.; Corcoran, D.L.; Hammerle, M.; Harrington, H.; Hogan, S.; Meier, M.H.; Polanczyk, G.V.; et al. Is Adult ADHD a Childhood-Onset Neurodevelopmental Disorder? Evidence From a Four-Decade Longitudinal Cohort Study. Am. J. Psychiatry 2015, 172, 967–977. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, K.L.; Katz, S.J.; Lee, S.S.; Hammen, C.; Brennan, P.A.; Najman, J.M. The association of ADHD and depression: Mediation by peer problems and parent–child difficulties in two complementary samples. J. Abnorm. Psychol. 2013, 122, 854–867. [Google Scholar] [CrossRef]
- Ruiz-Goikoetxea, M.; Cortese, S.; Aznarez-Sanado, M.; Magallon, S.; Alvarez-Zallo, N.; Luis, E.O.; de Castro-Manglano, P.; Soutullo, C.; Arrondo, G. Risk of unintentional injuries in children and adolescents with ADHD and the impact of ADHD medications: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2018, 84, 63–71. [Google Scholar] [CrossRef]
- Jangmo, A.; Stålhandske, A.; Chang, Z.; Chen, Q.; Almqvist, C.; Feldman, I.; Bulik, C.M.; Lichtenstein, P.; D’Onofrio, B.; Kuja-Halkola, R. Attention-deficit/hyperactivity disorder, school performance, and effect of medication. J. Am. Acad. Child Adolesc. Psychiatry 2019, 58, 423–432. [Google Scholar] [CrossRef]
- Danckaerts, M.; Sonuga-Barke, E.J.S.; Banaschewski, T.; Buitelaar, J.; Döpfner, M.; Hollis, C.; Santosh, P.; Rothenberger, A.; Sergeant, J.; Steinhausen, H.-C.; et al. The quality of life of children with attention deficit/hyperactivity disorder: A systematic review. Eur. Child Adolesc. Psychiatry 2009, 19, 83–105. [Google Scholar] [CrossRef]
- Burke, J.D.; Loeber, R.; Lahey, B.B. Which aspects of ADHD are associated with tobacco use in early adolescence? J. Child Psychol. Psychiatry Allied. 2001, 42, 493–502. [Google Scholar] [CrossRef]
- Sarver, D.E.; McCart, M.R.; Sheidow, A.J.; Letourneau, E.J. ADHD and risky sexual behavior in adolescents: Conduct problems and substance use as mediators of risk. J. Child Psychol. Psychiatry 2014, 55, 1345–1353. [Google Scholar] [CrossRef]
- Hua, M.-H.; Huang, K.-L.; Hsu, J.-W.; Bai, Y.-M.; Su, T.-P.; Tsai, S.-J.; Li, C.-T.; Lin, W.-C.; Chen, T.-J.; Chen, M.-H. Early Pregnancy Risk Among Adolescents With ADHD: A Nationwide Longitudinal Study. J. Atten. Disord. 2020, 25, 1199–1206. [Google Scholar] [CrossRef]
- McClemont, A.J.; Morton, H.E.; Gillis, J.M.; Romanczyk, R.G. Brief Report: Predictors of School Refusal Due to Bullying in Children with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder. J. Autism Dev. Disord. 2020, 51, 1781–1788. [Google Scholar] [CrossRef]
- Vaa, T. ADHD and relative risk of accidents in road traffic: A meta-analysis. Accid. Anal. Prev. 2014, 62, 415–425. [Google Scholar] [CrossRef]
- Li, L.; Chang, Z.; Sun, J.; Jangmo, A.; Zhang, L.; Andersson, L.M.; Werner-Kiechle, T.; Ahnemark, E.; D’Onofrio, B.M.; Larsson, H. Association Between Pharmacological Treatment of Attention-Deficit/Hyperactivity Disorder and Long-term Unemployment Among Working-Age Individuals in Sweden. JAMA Netw. Open 2022, 5, e226815. [Google Scholar] [CrossRef]
- Humphreys, K.L.; Galán, C.A.; Tottenham, N.; Lee, S.S. Impaired Social Decision-Making Mediates the Association Between ADHD and Social Problems. J. Abnorm. Child Psychol. 2015, 44, 1023–1032. [Google Scholar] [CrossRef]
- Michielsen, M.; Comijs, H.C.; Semeijn, E.J.; Beekman, A.T.; Deeg, D.J.; Kooij, J.S. The comorbidity of anxiety and depressive symptoms in older adults with attention-deficit/hyperactivity disorder: A longitudinal study. J. Affect. Disord. 2013, 148, 220–227. [Google Scholar] [CrossRef]
- Tistarelli, N.; Fagnani, C.; Troianiello, M.; Stazi, M.A.; Adriani, W. The nature and nurture of ADHD and its comorbidities: A narrative review on twin studies. Neurosci. Biobehav. Rev. 2019, 109, 63–77. [Google Scholar] [CrossRef]
- NICE. Attention Deficit Hyperactivity Disorder: Diagnosis and Management. Available online: https://www.nice.org.uk/guidance/ng87 (accessed on 22 June 2022).
- Barkley, R.A.; DuPaul, G.J.; McMurray, M.B. Attention Deficit Disorder With and Without Hyperactivity: Clinical Response to Three Dose Levels of Methylphenidate. Pediatrics 1991, 87, 519–531. [Google Scholar] [CrossRef]
- Dittmann, R.W.; Cardo, E.; Nagy, P.; Anderson, C.S.; Adeyi, B.; Caballero, B.; Hodgkins, P.; Civil, R.; Coghill, D. Treatment Response and Remission in a Double-Blind, Randomized, Head-to-Head Study of Lisdexamfetamine Dimesylate and Atomoxetine in Children and Adolescents with Attention-Deficit Hyperactivity Disorder. CNS Drugs 2014, 28, 1059–1069. [Google Scholar] [CrossRef]
- Milich, R.; Balentine, A.C.; Lynam, D.R. ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clin. Psychol. Sci. Pract. 2001, 8, 463–488. [Google Scholar] [CrossRef]
- Mariani, J.J.; Levin, F.R. Treatment Strategies for Co-Occurring ADHD and Substance Use Disorders. Am. J. Addict. 2007, 16, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Aadil, M.; Cosme, R.M.; Chernaik, J. Mindfulness-Based Cognitive Behavioral Therapy as an Adjunct Treatment of Attention Deficit Hyperactivity Disorder in Young Adults: A Literature Review. Cureus 2017, 9, e1269. [Google Scholar] [CrossRef] [PubMed]
- Laviola, G.; Adriani, W.; Terranova, M.; Gerra, G. Psychobiological risk factors for vulnerability to psychostimulants in human adolescents and animal models. Neurosci. Biobehav. Rev. 1999, 23, 993–1010. [Google Scholar] [CrossRef] [PubMed]
- Schenk, S.; Davidson, E.S. Stimulant preexposure sensitizes rats and humans to the rewarding effects of cocaine. NIDA Res. Monogr. 1998, 169, 56–82. [Google Scholar] [PubMed]
- Darredeau, C.; Barrett, S.P.; Jardin, B.; Pihl, R.O. Patterns and predictors of medication compliance, diversion, and misuse in adult prescribed methylphenidate users. Hum. Psychopharmacol. Clin. Exp. 2007, 22, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Doggett, A.M. ADHD and drug therapy: Is it still a valid treatment? J. Child Health Care. 2004, 8, 69–81. [Google Scholar] [CrossRef]
- Childress, A.C.; Sallee, F.R. Attention-Deficit/Hyperactivity Disorder with Inadequate Response to Stimulants: Approaches to Management. CNS Drugs 2014, 28, 121–129. [Google Scholar] [CrossRef]
- Brinkman, W.B.; Simon, J.O.; Epstein, J.N. Reasons Why Children and Adolescents With Attention-Deficit/Hyperactivity Disorder Stop and Restart Taking Medicine. Acad. Pediatr. 2018, 18, 273–280. [Google Scholar] [CrossRef]
- Swanson, J.M. Debate: Are Stimulant Medications for Attention-Deficit/Hyperactivity Disorder Effective in the Long Term? (Against). J. Am. Acad. Child Adolesc. Psychiatry 2019, 58, 936–938. [Google Scholar] [CrossRef]
- Dittmann, R.W.; Cardo, E.; Nagy, P.; Anderson, C.S.; Bloomfield, R.; Caballero, B.; Higgins, N.; Hodgkins, P.; Lyne, A.; Civil, R.; et al. Efficacy and Safety of Lisdexamfetamine Dimesylate and Atomoxetine in the Treatment of Attention-Deficit/Hyperactivity Disorder: A Head-to-Head, Randomized, Double-Blind, Phase IIIb Study. CNS Drugs 2013, 27, 1081–1092. [Google Scholar] [CrossRef]
- Cortese, S.; Adamo, N.; Del Giovane, C.; Mohr-Jensen, C.; Hayes, A.J.; Carucci, S.; Atkinson, L.Z.; Tessari, L.; Banaschewski, T.; Coghill, D.; et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. Lancet Psychiatry 2018, 5, 727–738. [Google Scholar] [CrossRef]
- Vidal, R.; Bosch, R.; Nogueira, M.; Gómez-Barros, N.; Valero, S.; Palomar, G.; Corrales, M.; Richarte, V.; Mena, B.; Casas, M.; et al. Psychoeducation for Adults with Attention Deficit Hyperactivity Disorder vs. Cognitive Behavioral Group Therapy. J. Nerv. Ment. Dis. 2013, 201, 894–900. [Google Scholar] [CrossRef]
- Buitelaar, J.K.; Kooij, J.J. Attention deficit hyperactivity disorder (ADHD): Etiology, diagnosis and treatment. Ned. Tijdschr. Voor Geneeskd. 2000, 144, 1716–1723. [Google Scholar]
- Dalrymple, R.A.; Maxwell, L.M.; Russell, S.; Duthie, J. NICE guideline review: Attention deficit hyperactivity disorder: Diagnosis and management (NG87). Arch. Dis. Child. Educ. Pract. Ed. 2019, 105, 289–293. [Google Scholar] [CrossRef]
- Daley, D.; Van der Oord, S.; Ferrin, M.; Danckaerts, M.; Doepfner, M.; Cortese, S.; Sonuga-Barke, E.J.; Group, E.A.G. Behavioral interventions in attention-deficit/hyperactivity disorder: A meta-analysis of randomized controlled trials across multiple outcome domains. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 835–847. [Google Scholar] [CrossRef]
- Willis, D.; Siceloff, E.R.; Morse, M.; Neger, E.; Flory, K. Stand-Alone Social Skills Training for Youth with ADHD: A Systematic Review. Clin. Child Fam. Psychol. Rev. 2019, 22, 348–366. [Google Scholar] [CrossRef]
- Young, Z.; Moghaddam, N.; Tickle, A. The Efficacy of Cognitive Behavioral Therapy for Adults With ADHD: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Atten. Disord. 2016, 24, 875–888. [Google Scholar] [CrossRef]
- Young, S.; Asherson, P.; Lloyd, T.; Absoud, M.; Arif, M.; Colley, W.A.; Cortese, S.; Cubbin, S.; Doyle, N.; Morua, S.D.; et al. Failure of Healthcare Provision for Attention-Deficit/Hyperactivity Disorder in the United Kingdom: A Consensus Statement. Front. Psychiatry 2021, 12, 324. [Google Scholar] [CrossRef]
- Cheung, K.K.; Wong, I.C.; Ip, P.; Chan, P.K.; Lin, C.H.; Wong, L.Y.; Chan, E.W. Experiences of adolescents and young adults with ADHD in Hong Kong: Treatment services and clinical management. BMC Psychiatry 2015, 15, 95. [Google Scholar] [CrossRef]
- Cochrane, W.G.; Dinu, L.M.; Kika, N.B.; Dommett, E.J. Attitudes and preferences toward exercise interventions in adults with attention deficit hyperactivity disorder: A survey study. Int. J. Ment. Health 2022, 51, 267–285. [Google Scholar] [CrossRef]
- Dinu, L.M.; Phattharakulnij, N.; Dommett, E.J. Tryptophan modulation in individuals with attention deficit hyperactivity disorder: A systematic review. J. Neural Transm. 2022, 129, 361–377. [Google Scholar] [CrossRef] [PubMed]
- Xu, G.; Strathearn, L.; Liu, B.; Yang, B.; Bao, W. Twenty-Year Trends in Diagnosed Attention-Deficit/Hyperactivity Disorder Among US Children and Adolescents, 1997–2016. JAMA Netw. Open 2018, 1, e181471. [Google Scholar] [CrossRef]
- Househam, A.M.; Solanto, M.V. Mindfulness as an Intervention for ADHD. ADHD Rep. 2016, 24, 1–13. [Google Scholar] [CrossRef]
- Roberts, L.R.; Neece, C.L. Feasibility of Mindfulness-based Stress Reduction Intervention for Parents of Children with Developmental Delays. Issues Ment. Health Nurs. 2015, 36, 592–602. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J. Mindfulness Meditation in Everyday Life; Hyperion: New York, NY, USA, 1994. [Google Scholar]
- Roychowdhury, D. Moving Mindfully: The Role of Mindfulness Practice in Physical Activity and Health Behaviours. J. Funct. Morphol. Kinesiol. 2021, 6, 19. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living; Delta: New York, NY, USA, 1990. [Google Scholar]
- Niazi, A.K.; Niazi, S.K. Mindfulness-based stress reduction: A non-pharmacological approach for chronic illnesses. N. Am. J. Med. Sci. 2011, 3, 20–23. [Google Scholar] [CrossRef]
- Seidman, L.J. Neuropsychological functioning in people with ADHD across the lifespan. Clin. Psychol. Rev. 2006, 26, 466–485. [Google Scholar] [CrossRef]
- Nigg, J.T.; Casey, B.J. An integrative theory of attention-deficit/ hyperactivity disorder based on the cognitive and affective neurosciences. Dev. Psychopathol. 2005, 17, 785–806. [Google Scholar] [CrossRef]
- Barranco-Ruiz, Y.; Etxabe, B.E.; Ramírez-Vélez, R.; Villa-González, E. Interventions Based on Mind–Body Therapies for the Improvement of Attention-Deficit/Hyperactivity Disorder Symptoms in Youth: A Systematic Review. Medicina 2019, 55, 325. [Google Scholar] [CrossRef]
- Evans, S.; Ling, M.; Hill, B.; Rinehart, N.; Austin, D.; Sciberras, E. Systematic review of meditation-based interventions for children with ADHD. Eur. Child Adolesc. Psychiatry 2017, 27, 9–27. [Google Scholar] [CrossRef]
- Chimiklis, A.L.; Dahl, V.; Spears, A.P.; Goss, K.; Fogarty, K.; Chacko, A. Yoga, Mindfulness, and Meditation Interventions for Youth with ADHD: Systematic Review and Meta-Analysis. J. Child Fam. Stud. 2018, 27, 3155–3168. [Google Scholar] [CrossRef]
- Tercelli, I.; Ferreira, N. A systematic review of mindfulness based interventions for children and young people with ADHD and their parents. Glob. Psychiatry 2019, 2, 79–95. [Google Scholar] [CrossRef]
- Nimmo-Smith, V.; Merwood, A.; Hank, D.; Brandling, J.; Greenwood, R.; Skinner, L.; Law, S.; Patel, V.; Rai, D. Non-pharmacological interventions for adult ADHD: A systematic review. Psychol. Med. 2020, 50, 529–541. [Google Scholar] [CrossRef]
- Poissant, H.; Mendrek, A.; Talbot, N.; Khoury, B.; Nolan, J. Behavioral and Cognitive Impacts of Mindfulness-Based Interventions on Adults with Attention-Deficit Hyperactivity Disorder: A Systematic Review. Behav. Neurol. 2019, 2019, 1–16. [Google Scholar] [CrossRef]
- López-Pinar, C.; Martínez-Sanchís, S.; Carbonell-Vayá, E.; Sánchez-Meca, J.; Fenollar-Cortés, J. Efficacy of Nonpharmacological Treatments on Comorbid Internalizing Symptoms of Adults with Attention-Deficit/Hyperactivity Disorder: A Meta-Analytic Review. J. Atten. Disord. 2019, 24, 456–478. [Google Scholar] [CrossRef]
- Zhang, J.; Díaz-Román, A.; Cortese, S. Meditation-based therapies for attention-deficit/hyperactivity disorder in children, adolescents and adults: A systematic review and meta-analysis. Évid. Based Ment. Health 2018, 21, 87–94. [Google Scholar] [CrossRef]
- Krisanaprakornkit, T.; Ngamjarus, C.; Witoonchart, C.; Piyavhatkul, N. Meditation therapies for attention-deficit/hyperactivity disorder (ADHD). Cochrane Database Syst. Rev. 2010, CD006507. [Google Scholar] [CrossRef]
- Mak, C.; Whittingham, K.; Cunnington, R.; Boyd, R.N. Efficacy of Mindfulness-Based Interventions for Attention and Executive Function in Children and Adolescents—A Systematic Review. Mindfulness 2017, 9, 59–78. [Google Scholar] [CrossRef]
- Cairncross, M.; Miller, C.J. The Effectiveness of Mindfulness-Based Therapies for ADHD: A Meta-Analytic Review. J. Atten. Disord. 2016, 24, 627–643. [Google Scholar] [CrossRef]
- Lee, C.S.; Ma, M.-T.; Ho, H.-Y.; Tsang, K.-K.; Zheng, Y.-Y.; Wu, Z.-Y. The Effectiveness of Mindfulness-Based Intervention in Attention on Individuals with ADHD: A Systematic Review. Hong Kong J. Occup. Ther. 2017, 30, 33–41. [Google Scholar] [CrossRef]
- Xue, J.; Zhang, Y.; Huang, Y. A meta-analytic investigation of the impact of mindfulness-based interventions on ADHD symptoms. Medicine 2019, 98, e15957. [Google Scholar] [CrossRef]
- Oliva, F.; Malandrone, F.; di Girolamo, G.; Mirabella, S.; Colombi, N.; Carletto, S.; Ostacoli, L. The efficacy of mindfulness-based interventions in attention-deficit/hyperactivity disorder beyond core symptoms: A systematic review, meta-analysis, and meta-regression. J. Affect. Disord. 2021, 292, 475–486. [Google Scholar] [CrossRef]
- Laugesen, B.; Groenkjaer, M. Parenting experiences of living with a child with attention deficit hyperactivity disorder: A systematic review of qualitative evidence. JBI Evid. Synth. 2015, 13, 169–234. [Google Scholar] [CrossRef]
- Marceau, K.; Laurent, H.K.; Neiderhiser, J.M.; Reiss, D.; Shaw, D.S.; Natsuaki, M.N.; Fisher, P.A.; Leve, L.D. Combined influences of genes, prenatal environment, cortisol, and parenting on the development of children’s internalizing versus externalizing problems. Behav. Gen. 2015, 45, 268–282. [Google Scholar] [CrossRef]
- Deault, L.C. A Systematic Review of Parenting in Relation to the Development of Comorbidities and Functional Impairments in Children with Attention-Deficit/Hyperactivity Disorder (ADHD). Child Psychiatry Hum. Dev. 2009, 41, 168–192. [Google Scholar] [CrossRef]
- Agha, S.S.; Zammit, S.; Thapar, A.; Langley, K. Maternal psychopathology and offspring clinical outcome: A four-year follow-up of boys with ADHD. Eur. Child Adolesc. Psychiatry 2016, 26, 253–262. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute (NHLBI) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 23 February 2022).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge Academic: New York, NY, USA, 1988. [Google Scholar]
- Beheshti, A.; Chavanon, M.-L.; Christiansen, H. Emotion dysregulation in adults with attention deficit hyperactivity disorder: A meta-analysis. BMC Psychiatry 2020, 20, 120. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, G.; Carpenter, J.R.; Rücker, G. Fixed Effect and Random Effects Meta-Analysis. In Meta-Analysis with R. Use R! Springer: Cham, Germany, 2015; pp. 21–53. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022). Cochrane, 2022. Available online: www.training.cochrane.org/handbook (accessed on 7 October 2022).
- Sibalis, A.; Milligan, K.; Pun, C.; McKeough, T.; Schmidt, L.A.; Segalowitz, S.J. An EEG Investigation of the Attention-Related Impact of Mindfulness Training in Youth with ADHD: Outcomes and Methodological Considerations. J. Atten. Disord. 2017, 23, 733–743. [Google Scholar] [CrossRef] [PubMed]
- Zylowska, L.; Ackerman, D.L.; Yang, M.H.; Futrell, J.L.; Horton, N.L.; Hale, T.S.; Pataki, C.; Smalley, S.L. Mindfulness meditation training in adults and adolescents with ADHD: A feasibility study. J. Atten. Disord. 2008, 11, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Converse, A.K.; Barrett, B.P.; Chewning, B.A.; Wayne, P.M. Tai Chi training for attention deficit hyperactivity disorder: A feasibility trial in college students. Complement. Ther. Med. 2020, 53, 102538. [Google Scholar] [CrossRef]
- Gershy, N.; Meehan, K.B.; Omer, H.; Papouchis, N.; Sapir, I.S. Randomized Clinical Trial of Mindfulness Skills Augmentation in Parent Training. Child Care Q. 2017, 46, 783–803. [Google Scholar] [CrossRef]
- Kratter, J. The Use of Meditation in the Treatment of Attention Deficit Disorder with Hyperactivity; St. John’s University: New York, NY, USA, 1983. [Google Scholar]
- Schoenberg, P.L.; Hepark, S.; Kan, C.C.; Barendregt, H.P.; Buitelaar, J.K.; Speckens, A.E. Effects of mindfulness-based cognitive therapy on neurophysiological correlates of performance monitoring in adult attention-deficit/hyperactivity disorder. Clin. Neurophysiol. 2014, 125, 1407–1416. [Google Scholar] [CrossRef]
- Sidhu, P. The Efficacy of Mindfulness Meditation in Increasing the Attention Span in Children with ADHD. Ph.D. Thesis, Pacifica Graduate Institute, Carpinteria, CA, USA, 2015. [Google Scholar]
- Bachmann, K.; Lam, A.P.; Sörös, P.; Kanat, M.; Hoxhaj, E.; Matthies, S.; Feige, B.; Müller, H.; Özyurt, J.; Thiel, C.M.; et al. Effects of mindfulness and psychoeducation on working memory in adult ADHD: A randomised, controlled fMRI study. Behav. Res. Ther. 2018, 106, 47–56. [Google Scholar] [CrossRef]
- Behbahani, M.; Zargar, F.; Assarian, F.; Akbari, H. Effects of Mindful Parenting Training on Clinical Symptoms in Children with Attention Deficit Hyperactivity Disorder and Parenting Stress: Randomized Controlled Trial. Iran. J. Med. Sci. 2018, 43, 596–604. [Google Scholar] [CrossRef]
- Bueno, V.F.; Kozasa, E.H.; Da Silva, M.A.; Alves, T.M.; Louzã, M.R.; Pompéia, S. Mindfulness Meditation Improves Mood, Quality of Life, and Attention in Adults with Attention Deficit Hyperactivity Disorder. BioMed Res. Int. 2015, 2015, 1–14. [Google Scholar] [CrossRef]
- Edel, M.-A.; Hölter, T.; Wassink, K.; Juckel, G. A comparison of mindfulness-based group training and skills group training in adults with ADHD: An open study. J. Atten. Disord. 2017, 21, 533–539. [Google Scholar] [CrossRef]
- Gu, Y.; Xu, G.; Zhu, Y. A Randomized Controlled Trial of Mindfulness-Based Cognitive Therapy for College Students With ADHD. J. Atten. Disord. 2016, 22, 388–399. [Google Scholar] [CrossRef]
- Haydicky, J.; Wiener, J.; Badali, P.; Milligan, K.; Ducharme, J.M. Evaluation of a Mindfulness-based Intervention for Adolescents with Learning Disabilities and Co-occurring ADHD and Anxiety. Mindfulness 2012, 3, 151–164. [Google Scholar] [CrossRef]
- Haydicky, J.; Shecter, C.; Wiener, J.; Ducharme, J.M. Evaluation of MBCT for Adolescents with ADHD and Their Parents: Impact on Individual and Family Functioning. J. Child Fam. Stud. 2015, 24, 76–94. [Google Scholar] [CrossRef]
- Hepark, S.; Janssen, L.; De Vries, A.; Schoenberg, P.L.A.; Donders, R.; Kan, C.C.; Speckens, A.E.M. The Efficacy of Adapted MBCT on Core Symptoms and Executive Functioning in Adults With ADHD: A Preliminary Randomized Controlled Trial. J. Atten. Disord. 2015, 23, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Hoxhaj, E.; Sadohara, C.; Borel, P.; D’Amelio, R.; Sobanski, E.; Müller, H.; Feige, B.; Matthies, S.; Philipsen, A. Mindfulness vs psychoeducation in adult ADHD: A randomized controlled trial. Eur. Arch. Psychiatry Clin. Neurosci. 2018, 268, 321–335. [Google Scholar] [CrossRef] [PubMed]
- Huguet, A.; Eguren, J.I.; Miguel-Ruiz, D.; Vallés, X.V.; Alda, J.A. Deficient Emotional Self-Regulation in Children with Attention Deficit Hyperactivity Disorder: Mindfulness as a Useful Treatment Modality. J. Dev. Behav. Pediatr. 2019, 40, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Janssen, L.; Kan, C.C.; Carpentier, P.J.; Sizoo, B.; Hepark, S.; Schellekens, M.P.; Donders, A.R.T.; Buitelaar, J.K.; Speckens, A.E. Mindfulness-based cognitive therapy v. treatment as usual in adults with ADHD: A multicentre, single-blind, randomised controlled trial. Psychol. Med. 2018, 49, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Kiani, B.; Hadianfard, H.; Mitchell, J.T. The impact of mindfulness meditation training on executive functions and emotion dysregulation in an Iranian sample of female adolescents with elevated attention-deficit/hyperactivity disorder symptoms. Aust. J. Psychol. 2017, 69, 273–282. [Google Scholar] [CrossRef]
- Liu, P.; Qiu, S.; Lo, H.H.M.; Song, X.; Qian, Q. Applying the Mindful Parenting Program Among Chinese Parents of Children with ADHD: A Randomized Control Trial. Mindfulness 2021, 12, 1473–1489. [Google Scholar] [CrossRef]
- Lo, H.H.M.; Wong, S.W.L.; Wong, J.Y.H.; Yeung, J.W.K.; Snel, E.; Wong, S.Y.S. The Effects of Family-Based Mindfulness Intervention on ADHD Symptomology in Young Children and Their Parents: A Randomized Control Trial. J. Atten. Disord. 2017, 24, 667–680. [Google Scholar] [CrossRef]
- Meyer, J.; Ramklint, M.; Hallerbäck, M.U.; Lööf, M.; Isaksson, J. Evaluation of a structured skills training group for adolescents with attention deficit/hyperactivity disorder (ADHD)–study protocol of a randomised controlled trial. BMC Psychiatry 2019, 19, 171. [Google Scholar] [CrossRef]
- Mitchell, J.T.; McIntyre, E.M.; English, J.S.; Dennis, M.F.; Beckham, J.C.; Kollins, S.H. A Pilot Trial of Mindfulness Meditation Training for ADHD in Adulthood: Impact on Core Symptoms, Executive Functioning, and Emotion Dysregulation. J. Atten. Disord. 2013, 21, 1105–1120. [Google Scholar] [CrossRef]
- Muratori, P.; Conversano, C.; Levantini, V.; Masi, G.; Milone, A.; Villani, S.; Bögels, S.; Gemignani, A. Exploring the Efficacy of a Mindfulness Program for Boys With Attention-Deficit Hyperactivity Disorder and Oppositional Defiant Disorder. J. Atten. Disord. 2020, 25, 1544–1553. [Google Scholar] [CrossRef]
- Rynczak, D. Effectiveness of Mindfulness in Reducing Impulsivity in Youth with Attention-Deficit/Hyperactivity Disorder. Ph.D. Thesis, The Chicago School of Professional Psychology, Chicago, IL, USA, 2011. [Google Scholar]
- Siebelink, N.M.; Bögels, S.M.; Speckens, A.E.M.; Dammers, J.T.; Wolfers, T.; Buitelaar, J.K.; Greven, C.U. A randomised controlled trial (MindChamp) of a mindfulness-based intervention for children with ADHD and their parents. J. Child Psychol. Psychiatry 2021, 63, 165–177. [Google Scholar] [CrossRef]
- Van de Weijer-Bergsma, E.; Formsma, A.R.; de Bruin, E.I.; Bögels, S.M. The effectiveness of mindfulness training on behavioral problems and attentional functioning in adolescents with ADHD. J. Child Fam. Stud. 2012, 21, 775–787. [Google Scholar] [CrossRef]
- Van der Oord, S.; Bögels, S.M.; Peijnenburg, D. The effectiveness of mindfulness training for children with ADHD and mindful parenting for their parents. J. Child Fam. Stud. 2012, 21, 139–147. [Google Scholar] [CrossRef]
- Zhang, D.; Chan, S.K.C.; Lo, H.H.M.; Chan, C.Y.H.; Chan, J.C.Y.; Ting, K.T.; Gao, T.T.; Lai, K.Y.C.; Bögels, S.M.; Wong, S.Y.S. Mindfulness-Based Intervention for Chinese Children with ADHD and Their Parents: A Pilot Mixed-Method Study. Mindfulness 2016, 8, 859–872. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Doyle, N. Neurodiversity at work: A biopsychosocial model and the impact on working adults. Br. Med. Bull. 2020, 135, 108–125. [Google Scholar] [CrossRef]
- Waschbusch, D.A.; Pelham, W.E.; Waxmonsky, J.; Johnston, C. Are There Placebo Effects in the Medication Treatment of Children with Attention-Deficit Hyperactivity Disorder? J. Dev. Behav. Pediatr. 2009, 30, 158–168. [Google Scholar] [CrossRef]
- Mayfield, A.R.; Parke, E.M.; Barchard, K.A.; Zenisek, R.P.; Thaler, N.S.; Etcoff, L.M.; Allen, D.N. Equivalence of mother and father ratings of ADHD in children. Child Neuropsychol. 2016, 24, 166–183. [Google Scholar] [CrossRef]
- Meppelink, R. Childhood ADHD: Meditation or Medication? University of Amsterdam: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Vanzin, L.; Crippa, A.; Mauri, V.; Valli, A.; Mauri, M.; Molteni, M.; Nobile, M. Does ACT-Group Training Improve Cognitive Domain in Children with Attention Deficit Hyperactivity Disorder? A Single-Arm, Open-Label Study. Behav. Chang. 2020, 37, 1–12. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Sawyer, A.T.; Witt, A.A.; Oh, D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J. Consult. Clin. Psychol. 2010, 78, 169–183. [Google Scholar] [CrossRef]

| Study | Design | Sample | Mindfulness Condition | Control Condition | ADHD Status | Medication Permitted (Y/N/NR) | Other Therapy Permitted (Y/N/NR) | Excluded Comorbidities | Age range of ADHD Patients (Years) * | Gender of ADHD Patients (M:F) | Analysed Sample Size (Initial Sample) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Bachmann et al., 2018 [84] | RCT | Adult patients | Mindfulness Meditation (MM) ** | PE | DSM-IV; combined or inattentive | N (3 mths med-free) | N | SZ, BPD, SUD, ASD, SUI, SH, NEURO. | 18–65 | 18:22 | 40 (74) |
| Behbahani et al., 2018 [85] | RCT | Mothers of child patients | Mindful Parenting training (MPT) | US control * | Child—US ADHD diagnosis | Y (risperi-done or Ritalin) | NR | DD, MOOD, PSY | 7–12 | 37:19 | 56 (60) |
| Bueno et al., 2015 [86] | P-P | Adult patients & HC | Mindfulness Awareness Practice (MAP) | US control * | DSM-IV | Y (Methylph-enidate) | NR | NEURO, PSY, OCD, TS, DEP, ANX | 18–45 | ADHD 23:20 HC 7:10 | ADHD 43 (48) HC 17 (20) |
| Edel et al., 2017 [87] | nRCT | Adult patients | Mindfulness-based training | Skills training | DSM-IV | Y | NR | DEP, BPD, PSY GAD or PD | MBT 33.8 ST 36.7 | 55:36 | 91 |
| Gu et al., 2018 [88] | RCT | Under-graduates w/ADHD | Mindfulness-based Cognitive Therapy (MCBT) | WL | DSM-5 | Y | NR | DEP, BPD, SUD, SUI, PSY, LD. | 19–24 | 30:24 | 54 (56) |
| Haydicky et al., 2012 [89] | nRCT | Children w/ADHD and LD | MBCT and martial arts training | WL | US ADHD diagnosis | Y | NR | All except LD and ANX | 12–18 | 28:0 | 28 |
| Haydicky et al., 2015 [90] | P-P | Families with child patients | MBCT (MyMind) | N/A | Child -US ADHD diagnosis | NR | NR | ASD, BEH | 13–18 | 13:5 | 18 children, 17 parents (20 children, 18 mothers, 6 fathers) |
| Hepark et al., 2019 [91] | RCT | Adult patients | MBCT | WL | DSM-IV | Y | N | SUD, PSY, PERS, LD, SUI, SH | 18–65 | 43:56 | 83 (103) |
| Hoxhaj et al., 2018 [92] | RCT | Adult patients | MAP | PE | DSM-IV | N | N | SZ, BPD, SUD, ASD, SUI, SH, NEURO | MAP 40.51 PE 38.50 | 39:42 | 64 (81) |
| Huguet et al., 2018 [93] | RCT | Child patients | Mindfulness programme based on MBCT and stress relief | TAU | DSM-5 | N | N | ASD, PSY, BPD | 7–12 | 51:19 | 55 (72) |
| Janssen et al., 2019 [94] | RCT | Adult patients | MBCT ** + TAU | TAU | DSM-IV | Y | Y (TAU) | DEP w/PSY SUI, mania, PERS, SUD, ASD, tic disorder, LD. | 18+ | 56:64 | 100 (120) |
| Kiani et al. (2017) [95] | RCT | Child patients | MM | WL | Elevated SNAP-IV scores | N | N | PSY, DEP, PERS, SUD, NEURO | 13–15 | 0:30 | 30 |
| Liu et al., 2021 [96] | RCT | Parents of child patients | MPT | TAU | Child—DSM-IV | Y | Y | None | MPT 9.84 TAU 10.27 | 87:26 | 113 |
| Lo et al., 2020 [97] | RCT | Families with child patients | Family-based mindfulness intervention (FBMI) | WL | Child score exceeds SWAN cut off and 74% US ADHD diagnosis | Y | NR | DD, ID, ASD | 5–7 | 83:17 | 100 children and parents |
| Meyer et al., 2021 [98] | RCT | Child patients | Structured skills training group including mindfulness | PE | Existing ICD-10 diagnosis with DSM-5 study check | Y | N | DEP, SUI, PSY, BPD, ID, brain injury, ASD, SUD | 15–18 | 164:105 | 164 (184) |
| Mitchell et al., 2017 [99] | RCT | Adult patients | MM ** | WL | DSM-IV | Y | NR | SUD, Axis I or II disorder, chronic medical problems, | 18–50 | 8:12 | 20 (22) |
| Muratori et al., 2021 [100] | RCT | Child patients + parents | Mindfulness training | WL | Child -US ADHD diagnosis + ODD | N | N | ASD | 8–12 | 50:0 | 50 children, 20 couples, 30 mothers, 3 fathers |
| Rynczak 2013 [101] | nRCT | Child patients | Mindfulness training | WL | DSM-IV-TR | Y | N | PSY, SUI, SUD | 12–15 | 8:4 | 12 |
| Siebelink et al., 2021 [102] | RCT | Child patients + one parent | Family mindfulness-based intervention (MBI) | TAU | Child—DSM-IV or DSM-5 | Y | No previous or current mindful. Therapy | PSY, BPD, SUI, PTSD, SUD | 8–16 | 72:31 | 93 children and 93 parents (103 children and 103 parents) |
| van de Weijer-Bergsma et al., 2012 [103] | P-P | Child patients + parents | Mindfulness training + Mindfulness Parent training | N/A | Child—DSM-IV | Y | NR | Not stated | 11–15 | 5:5 | 10 children, 10 mothers, 9 fathers |
| van der Oord et al., 2012 [104] | nRCT | Child patients + parents | Mindfulness training + Mindfulness Parent training | WL | Child—DSM-IV | Y | N | CD, ASD | 8–12 | 16:6 | 18 children (22 children 21 mothers, 1 father) |
| Zhang et al., 2017 [105] | P-P | Child patients + one parent | Mindfulness training + Mindfulness Parent training | N/A | Child -US ADHD diagnosis | Y | N | SUD, ASD, PERS, SUI, SH | 8–12 | 8:3 | 11 children, 11 parents |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Beuno et al., 2015 (Adult Study) [86] | Hit Reaction Time (RT) | −0.36 | −0.35 |
| Accuracy | 0.61 | 0.37 | |
| Omission | −0.68 | −0.70 | |
| Hit RT standard error (SE) | −0.45 | −0.88 | |
| Variability of SE | −0.31 | −0.46 | |
| Hit RT Block change | −0.71 | 0.54 | |
| Hit SE block change | −0.55 | −0.52 | |
| Gu et al., 2018 (Adult Study) [88] | Alerting error score (ES) | ||
| Immediate | −1.04 | 0.10 | |
| Follow-up | −1.15 | −0.11 | |
| Orienting ES | |||
| Immediate | −1.12 | −0.09 | |
| Follow-up | −1.16 | −0.09 | |
| Conflict ES | |||
| Immediate | −0.29 | −0.12 | |
| Follow-up | −0.45 | −0.11 |
| Study | Study/Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Beuno et al., 2015 (Adult Study) Connor’s CPT II [86] | Commission Errors | −0.54 | 0.04 |
| Omission Errors | −0.08 | −0.15 | |
| Hit RT | 0.14 | 0.01 | |
| Hit RT SE | −0.07 | 0.13 | |
| Variability of SE | 0.08 | 0.12 | |
| D prime | 0.07 | −0.15 | |
| HIT RT block change | −0.16 | 0.03 | |
| HIT SE block change | 0.23 | −0.17 | |
| Hit RT ISI Change | 0.09 | 0.24 | |
| Hit SE ISI Change | 0.11 | 0.39 | |
| Response style | −0.22 | −0.23 | |
| Perseverations | 0.39 | 0.20 | |
| Kiani et al., 2017 (Child Study) Unspecified CPT [95] | Commission Errors | −0.51 | −0.28 |
| Omission Errors | −0.21 | −0.30 | |
| Correct Responses | 0.36 | 0.32 | |
| Zhang et al., 2017 (Family Study) Connor’s CPT III [105] | Commission Errors | −2.19 | |
| Omission Errors | 0.41 | ||
| Hit RT | −0.05 | ||
| Hit RT Standard Deviation | 0.20 | ||
| Variability | 0.12 | ||
| D Prime | −0.70 | ||
| HIT RT block change | −0.27 | ||
| Hit RT ISI Change | 0.12 |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Bachman et al., 2018 (Adult Study) [84] | 1-Back Letter Test of WM * | ||
| Reaction Time | −0.55 | −0.54 | |
| Number of Correct Answers | 0.57 | 0.49 | |
| Kiani et al., 2017 (Child Study) [95] | Tower of London Task | ||
| Planning | 0.59 | 0.43 | |
| Digital Span Test | |||
| Backward span | 0.44 | 0.23 | |
| Forward span | −0.07 | 0.19 | |
| Total | 0.21 | 0.24 | |
| Stroop Inhibition | −0.65 | −0.11 | |
| Muratori et al., 2021 (Family Study) [100] | Bells-Test Revised | ||
| Speed | 0.41 | 0.32 | |
| Accuracy | 1.03 | 0.02 | |
| MFFT | |||
| Speed | −0.30 | −0.33 | |
| Accuracy | −0.29 | −0.72 | |
| Rynczak, 2013 [101] | Trail Making Task | ||
| Trail A | −0.81 | −0.04 | |
| Trail B | −0.39 | −0.08 | |
| Van de Weijer-Bergsma et al., 2012 (Child Study) ** [103] | Baseline Speed | 0.23 | |
| 0.06 | |||
| 0.25 | |||
| Sustained Attention Dots Task | |||
| Speed | −0.86 | ||
| −0.27 | |||
| −0.09 | |||
| Misses | −0.34 | ||
| −0.80 | |||
| −0.41 | |||
| False Alarms | 0.00 | ||
| −0.33 | |||
| −0.11 | |||
| Sustained Auditory Task | |||
| Speed | 0.09 | ||
| 0.01 | |||
| 0.03 | |||
| Misses | −0.22 | ||
| −0.81 | |||
| −0.34 | |||
| False Alarms | −0.46 | ||
| −0.65 | |||
| −0.77 | |||
| Zhang et al., 2017 (Family Study) [105] | TEA-Ch | ||
| Sky Search | |||
| No. correctly identified targets | −0.83 | ||
| Time per target | −1.46 | ||
| Attention score | −1.3 | ||
| Score! | −0.73 | ||
| Creature Counting | |||
| Total correct | 0.78 | ||
| Timing score | −0.75 | ||
| Sky Search DT | −0.16 | ||
| Map Mission | 1.22 | ||
| Walk, Do Not Walk | 0.43 | ||
| Opposite Worlds | |||
| Same World Total | 0.15 | ||
| Opposite World Total | −0.15 | ||
| Code Transmission | −0.23 |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Lui et al., 2021 (Parent Study) [96] | Hamilton Depression Scale | −0.47 | −0.18 |
| Sieberlink et al., 2012 (Parent measure in Family Study) * [102] | Brooding in response to sadness | −0.08 −0.24 | −0.09 0.08 |
| Study | Study/Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Gu et al., 2018 [88] * | BAI | −0.89 −0.88 | 0.15 −0.03 |
| Lui et al., 2021 (Parent Study) [96] | Hamilton Anxiety Scale | −0.39 | −0.26 |
| Study | Study/Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Behbahani et al., 2018 (Parent Study) * [85] | Total Score | −1.22 | −0.29 |
| −1.27 | −0.14 | ||
| Parent Distress | −1.87 | −0.95 | |
| −1.75 | −0.87 | ||
| Parent–Child Interactions | −0.83 | 0.17 | |
| −1.04 | 0.28 | ||
| Child Problematic Characteristics | −0.67 | 0.18 | |
| −0.82 | 0.20 | ||
| Lo et al., 2020 (Family Study) [97] | Total Score | −0.82 | 0.04 |
| Parent Distress | −0.15 | 0.06 | |
| Parent–Child Interactions | −0.12 | 0.04 | |
| Child Problematic Characteristics | −0.26 | 0.03 | |
| Lui et al., 2021 (Parent Study) [96] | Total Score | −0.41 | 0.03 |
| Zhang et al., 2017 (Family Study) [105] | Total Score | 0.16 | |
| Parent Distress | 0.28 | ||
| Parent–Child Interactions | 0.18 | ||
| Child Problematic Characteristics | −0.02 |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Haydicky et al., 2012 (Child Study) * [89] | Externalising | −0.54 | −0.38 |
| Social Problems | −0.68 | −0.40 | |
| Rule Breaking | −0.59 | −0.12 | |
| ADHD Problems | −0.19 | −0.44 | |
| Oppositional Defiant | −0.83 | −0.01 | |
| Conduct | −0.64 | −0.24 | |
| Huguet et al., 2019 (Child Study) [93] | AAA (anxiety/depression, aggression and attention) | −0.51 | −0.07 |
| Lo et al., 2020 (Family Study) [97] | Total | −0.37 | −0.04 |
| Anxiety | −0.28 | −0.04 | |
| Withdrawal/Depressed | −0.19 | −0.08 | |
| Somatic | −0.31 | 0.00 | |
| Attention | −0.49 | −0.05 | |
| Aggression | −0.32 | −0.09 | |
| Internalising | −0.31 | −0.04 | |
| Externalising | −0.29 | −0.10 | |
| Rynczak, 2013 (Child Study) [101] | Total | −1.72 | 0.00 |
| Van den Weijer-Bergsma et al., 2012 (Family Study) ** [103] | Attention (mother rating) | −0.09 | |
| −0.29 | |||
| Attention (father rating) | −0.58 | ||
| −1.43 | |||
| Externalising (mother rating) | 0.18 | ||
| −0.13 | |||
| Externalising (father rating) | −0.19 | ||
| −0.29 | |||
| Internalising (mother rating) | −0.10 | ||
| 0.01 | |||
| Internalising (father rating) | −0.42 | ||
| −0.43 |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Meyer et al., 2019 (Child Study) * [98] | Child Sheehan Disability Scale | ||
| Functional impairment (parent rated) | −0.27 | −0.09 | |
| −0.20 | −0.05 | ||
| Functional impairment (child rated) | −0.18 | −0.22 | |
| −0.30 | −0.14 | ||
| Muratori et al., 2021 (Family Study) [100] | Strengths & Difficulties Questionnaire | ||
| Conduct | −0.19 | −0.44 | |
| Avoidance and Fusion Questionnaire for Youth | −0.65 | 0.13 | |
| Modified Overt Aggression Scale | −1.12 | −0.91 | |
| Hoxhaj et al., 2018 (Adult Study) ** [92] | BSI | ||
| Somatization | −0.24 | −0.13 | |
| −0.17 | −0.17 | ||
| Obsession/Compulsion | −0.01 | −0.36 | |
| −0.28 | −0.43 | ||
| Interpersonal | −0.21 | −0.11 | |
| −0.24 | −0.31 | ||
| Depression | −0.08 | −0.25 | |
| −0.04 | −0.32 | ||
| Anxiety | −0.17 | −0.32 | |
| −0.31 | −0.39 | ||
| Hostility | −0.22 | −0.21 | |
| −0.21 | −0.42 | ||
| Phobic anxiety | −0.05 | −0.24 | |
| 0.08 | −0.27 | ||
| Paranoia | −0.12 | −0.26 | |
| 0.01 | −0.21 | ||
| Psychoticism | −0.27 | −0.36 | |
| −0.15 | −0.40 | ||
| Global Severity Index | −0.20 | −0.34 | |
| −0.19 | −0.41 | ||
| Positive symptom distress index | −0.30 | −0.29 | |
| −0.11 | −0.34 | ||
| Positive symptom total | −0.18 | −0.22 | |
| −0.33 | −0.31 | ||
| Zhang et al., 2017 (Family Study) [105] | Eyberg Child Behavior Inventory | ||
| Intensity | −0.34 | ||
| Problem | −0.24 |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Hoxhaj et al., 2018 (Adult Study) * [92] | Description | 0.15 | 0.14 |
| 0.15 | 0.24 | ||
| Observation | 0.52 | 0.01 | |
| 0.40 | 0.00 | ||
| Acting with awareness | 0.18 | 0.40 | |
| 0.48 | 0.39 | ||
| Non judging of inner experience | 0.19 | 0.18 | |
| 0.29 | 0.15 | ||
| Non reactivity to inner experience | 0.64 | 0.05 | |
| 0.46 | 0.19 | ||
| Lui et al., 2021 (Parent Study) [96] | Description | 0.14 | −0.07 |
| Observation | 0.52 | −0.05 | |
| Acting with awareness | −0.01 | −0.06 | |
| Non judging of inner experience | −0.01 | 0.18 | |
| Non reactivity to inner experience | 0.47 | −0.29 |
| Study | Measure | Mindfulness (g) | Control (g) |
|---|---|---|---|
| Haydicky et al., 2015 (Child Study) * [90] | Total | 0.73 | |
| 1.03 | |||
| Lo et al., 2020 (Family Study) [97] | Total | 0.02 | 0.02 |
| Sieberlink et al., 2021 (Family Study) ** [102] | Total | 0.51 | 0.03 |
| 0.46 | 0.10 | ||
| 0.53 | 0.12 | ||
| Lui et al., 2021 (Parent Study) [96] | Total | 0.08 | −0.09 |
| Compassion for child | −0.11 | −0.97 | |
| Emotional Awareness in parenting | 0.17 | −0.22 | |
| Listening with full attention | −0.05 | −0.18 | |
| Zhang et al., 2017 (Family Study) [105] | Compassion for child | 0.06 | |
| Emotional Awareness of the self | −0.31 | ||
| Emotional Awareness of the child | −0.09 | ||
| Emotional non-reactivity in parenting | −0.11 | ||
| Listening with full attention | −0.35 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kretschmer, C.R.; Göz Tebrizcik, B.; Dommett, E.J. Mindfulness Interventions for Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Psychiatry Int. 2022, 3, 363-399. https://doi.org/10.3390/psychiatryint3040031
Kretschmer CR, Göz Tebrizcik B, Dommett EJ. Mindfulness Interventions for Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Psychiatry International. 2022; 3(4):363-399. https://doi.org/10.3390/psychiatryint3040031
Chicago/Turabian StyleKretschmer, Clara R., Burcu Göz Tebrizcik, and Eleanor J. Dommett. 2022. "Mindfulness Interventions for Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis" Psychiatry International 3, no. 4: 363-399. https://doi.org/10.3390/psychiatryint3040031
APA StyleKretschmer, C. R., Göz Tebrizcik, B., & Dommett, E. J. (2022). Mindfulness Interventions for Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Psychiatry International, 3(4), 363-399. https://doi.org/10.3390/psychiatryint3040031







