Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Collection of Data
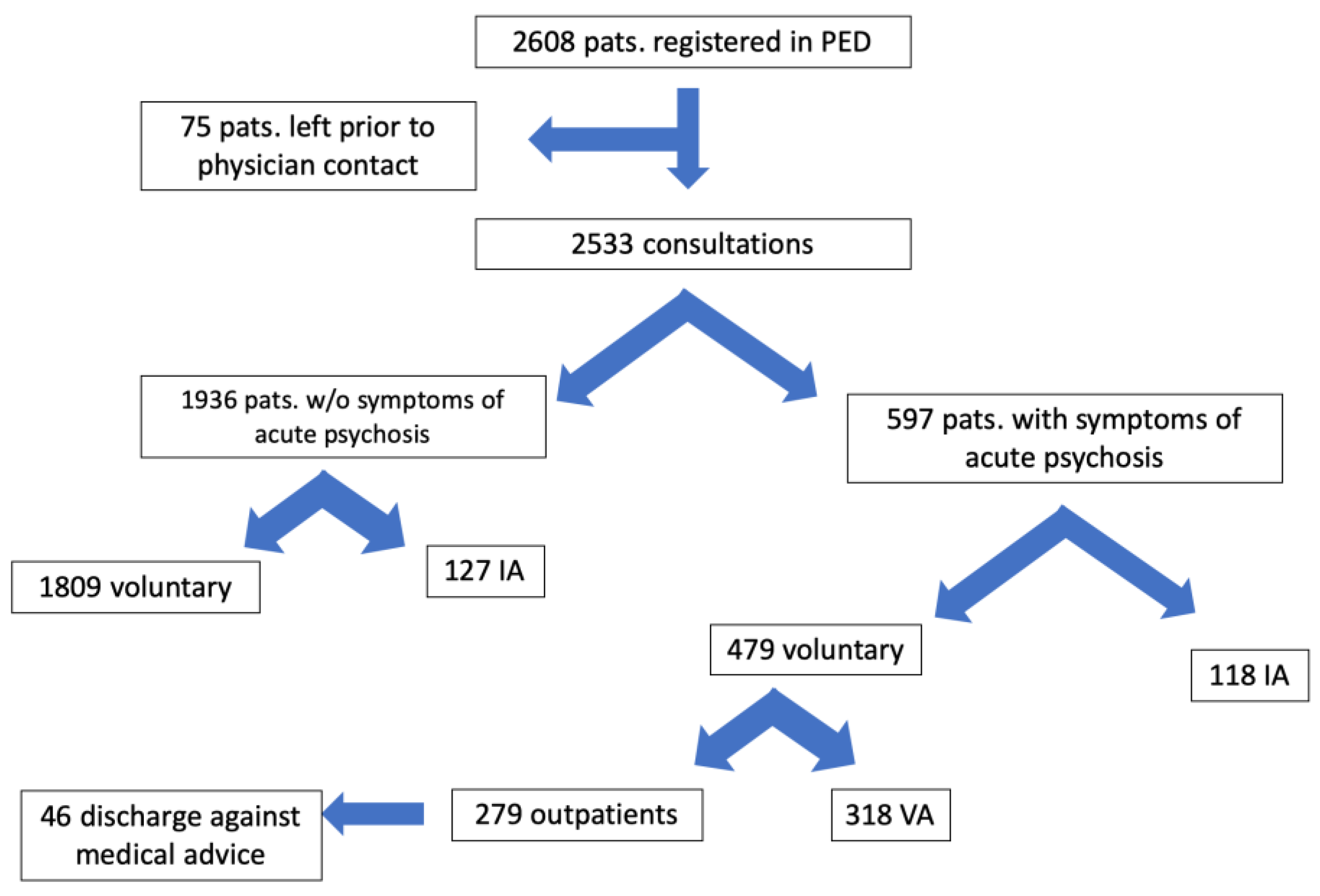
2.3. Selection of the Study Population
2.4. Data Analysis
2.5. Ethical Approval
3. Results
3.1. Sociodemographic and Circumstantial Characteristics of the Study Sample
3.2. Psychopathological Aspects of the Study Sample
3.3. Sociodemographic and Circumstantial Characteristics of the Study Sample
3.4. Psychopathological Predictors of Involuntary Admission of Psychiatric Care
4. Discussion
4.1. Sociodemographic and Circumstantial Characteristics of the Study Sample
4.2. Psychopathological Predictors of Involuntary Admission of Psychiatric Care
4.3. Limitations
5. Conclusions and Clinical Implications
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, S.; Mellsop, G.; Brink, J.; Wang, X. Involuntary admission and treatment of patients with mental disorder. Neurosci. Bull. 2015, 31, 99–112. [Google Scholar] [CrossRef]
- Arnold, B.D.; Moeller, J.; Hochstrasser, L.; Schneeberger, A.R.; Borgwardt, S.; Lang, U.E.; Huber, C.G. Compulsory Admission to Psychiatric Wards-Who Is Admitted, and Who Appeals Against Admission? Front. Psychiatry 2019, 10, 544. [Google Scholar] [CrossRef]
- Sheridan Rains, L.; Zenina, T.; Dias, M.C.; Jones, R.; Jeffreys, S.; Branthonne-Foster, S.; Lloyd-Evans, B.; Johnson, S. Variations in patterns of involuntary hospitalisation and in legal frameworks: An international comparative study. Lacent Psychiatry 2019, 6, 403–417. [Google Scholar] [CrossRef]
- Efkemann, S.A.; Ueberberg, B.; Haußleiter, I.S.; Hoffmann, K.; Juckel, G. Socio-economic impact on involuntary admissions and coercive measures in psychiatric hospitals in Germany. Int. J. Law Psychiatry 2020, 71, 101597. [Google Scholar] [CrossRef] [PubMed]
- Schmitz-Buhl, M.; Gairing, S.K.; Rietz, C.; Häussermann, P.; Zielasek, J.; Gouzoulis-Mayfrank, E. A retrospective analysis of determinants of involuntary psychiatric in-patient treatment. BMC Psychiatry 2019, 19, 127. [Google Scholar] [CrossRef]
- Kallert, T.W.; Glöckner, M.; Schützwohl, M. Involuntary vs. voluntary hospital admission. A systematic literature review on outcome diversity. Eur. Arch. Psychiatry Clin. Neurosci. 2008, 258, 195–209. [Google Scholar] [CrossRef]
- Kortrijk, H.E.; Staring, A.B.P.; van Baars, A.W.B.; Mulder, C.L. Involuntary admission may support treatment outcome and motivation in patients receiving assertive community treatment. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 245–252. [Google Scholar] [CrossRef]
- Balducci, P.M.; Bernardini, F.; Pauselli, L.; Tortorella, A.; Compton, M.T. Correlates of Involuntary Admission: Findings from an Italian Inpatient Psychiatric Unit. Psychiatr. Danub. 2017, 29, 490–496. [Google Scholar] [CrossRef] [PubMed]
- Maina, G.; Rosso, G.; Carezana, C.; Mehanović, E.; Risso, F.; Villari, V.; Gariglio, L.; Cardano, M. Factors associated with involuntary admissions: A register-based cross-sectional multicenter study. Ann. Gen. Psychiatry 2021, 20, 3. [Google Scholar] [CrossRef]
- Christina Katsakou, P.D.; Len Bowers, P.D.; Tim Amos, M.R.C.P.; Richard Morriss, M.D.; Diana Rose, P.D.; Til Wykes, P.D.; Stefan Priebe, F.R.C.P. Coercion and Treatment Satisfaction Among Involuntary Patients. Psychiatr. Serv. 2010, 61, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.Y.; Chan, H.Y.; Pan, Y.J. Risk factors for readmission in schizophrenia patients following involuntary admission. PLoS ONE 2017, 12, e0186768. [Google Scholar] [CrossRef] [PubMed]
- Priebe, S.; Bröker, M.; Gunkel, S. Involuntary admission and posttraumatic stress disorder symptoms in schizophrenia patients. Compr. Psychiatry 1998, 39, 220–224. [Google Scholar] [CrossRef]
- Xu, Z.; Lay, B.; Oexle, N.; Drack, T.; Bleiker, M.; Lengler, S.; Blank, C.; Müller, M.; Mayer, B.; Rössler, W.; et al. Involuntary psychiatric hospitalisation, stigma stress and recovery: A 2-year study. Epidemiol. Psychiatr. Sci. 2019, 28, 458–465. [Google Scholar] [CrossRef]
- Swartz, M.S.; Swanson, J.W.; Hannon, M.J. Does fear of coercion keep people away from mental health treatment? Evidence from a survey of persons with schizophrenia and mental health professionals. Behav. Sci. Law 2003, 21, 459–472. [Google Scholar] [CrossRef] [PubMed]
- Kaikoushi, K.; Middleton, N.; Chatzittofis, A.; Bella, E.; Alevizopoulos, G.; Karanikola, M. Socio-Demographic and Clinical Characteristics of Adults With Psychotic Symptomatology Under Involuntary Admission and Readmission for Compulsory Treatment in a Referral Psychiatric Hospital in Cyprus. Front. Psychiatry 2021, 12, 602274. [Google Scholar] [CrossRef]
- Hustoft, K.; Larsen, T.K.; Auestad, B.; Joa, I.; Johannessen, J.O.; Ruud, T. Predictors of involuntary hospitalizations to acute psychiatry. Int. J. Law Psychiatry 2013, 36, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Lebenbaum, M.; Chiu, M.; Vigod, S.; Kurdyak, P. Prevalence and predictors of involuntary psychiatric hospital admissions in Ontario, Canada: A population-based linked administrative database study. BJPsych Open 2018, 4, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.; Chen, H.; Zhong, S.; Guo, H.; Li, Q.; Cai, W.; de Girolamo, G.; Zhou, J.; Wang, X. Manic episode, aggressive behavior and poor insight are significantly associated with involuntary admission in patients with bipolar disorders. PeerJ 2019, 7, e7339. [Google Scholar] [CrossRef] [PubMed]
- Karasch, O.; Schmitz-Buhl, M.; Mennicken, R.; Zielasek, J.; Gouzoulis-Mayfrank, E. Identification of risk factors for involuntary psychiatric hospitalization: Using environmental socioeconomic data and methods of machine learning to improve prediction. BMC Psychiatry 2020, 20, 401. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Antunes, A.; Azeredo-Lopes, S.; Loureiro, A.; Saraceno, B.; Caldas-de-Almeida, J.M.; Cardoso, G. Factors associated with involuntary psychiatric hospitalization in Portugal. Int. J. Mental Health Syst. 2021, 15, 37. [Google Scholar] [CrossRef]
- Hotzy, F.; Hengartner, M.P.; Hoff, P.; Jaeger, M.; Theodoridou, A. Clinical and socio-demographic characteristics associated with involuntary admissions in Switzerland between 2008 and 2016: An observational cohort study before and after implementation of the new legislation. Eur. Psychiatry 2019, 59, 70–76. [Google Scholar] [CrossRef]
- Kelly, B.D.; Clarke, M.; Browne, S.; McTigue, O.; Kamali, M.; Gervin, M.; Kinsella, A.; Lane, A.; Larkin, C.; O’Callaghan, E. Clinical predictors of admission status in first episode schizophrenia. Eur. Psychiatry 2004, 19, 67–71. [Google Scholar] [CrossRef]
- Huber, C.G.; Schöttle, D.; Lambert, M.; Hottenrott, B.; Agorastos, A.; Naber, D.; Schroeder, K. Brief Psychiatric Rating Scale–Excited Component (BPRS-EC) and neuropsychological dysfunction predict aggression, suicidality, and involuntary treatment in first-episode psychosis. Schizophr. Res. 2012, 134, 273–278. [Google Scholar] [CrossRef]
- Rodrigues, R.; MacDougall, A.G.; Zou, G.; Lebenbaum, M.; Kurdyak, P.; Li, L.; Shariff, S.Z.; Anderson, K.K. Involuntary hospitalization among young people with early psychosis: A population-based study using health administrative data. Schizophr. Res. 2019, 208, 276–284. [Google Scholar] [CrossRef] [PubMed]
- WHO. The ICD-10 Classification of Mental and Behavioural Disorders; WHO: Geneva, Switzerland, 1992. [Google Scholar]
- AMDP. Das AMDP-System: Manual zur Dokumentation psychiatrischer Befunde, 10th ed.; Hogrefe: Göttingen, Germany, 2018. [Google Scholar]
- Lieberman, P.B.; Baker, F.M. The reliability of psychiatric diagnosis in the emergency room. Hosp. Community Psychiatry 1985, 36, 291–293. [Google Scholar] [CrossRef] [PubMed]
- Gebhardt, R.; Pietzcker, A. Zur Validierung der AMDP-Syndromskalen. Arch. Psychiatr. Nervenkrankh. 1983, 233, 509–523. [Google Scholar] [CrossRef] [PubMed]
- Gebhardt, R.; Pietzcker, A.; Strauss, A.; Stoeckel, M.; Langer, C.; Freudenthal, K. Skalenbildung im AMDP-System. Arch. Psychiatr. Nervenkrankh. 1983, 233, 223–245. [Google Scholar] [CrossRef]
- Newton, A.S.; Ali, S.; Johnson, D.W.; Haines, C.; Rosychuk, R.J.; Keaschuk, R.A.; Jacobs, P.; Cappelli, M.; Klassen, T.P. Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care. Acad. Emerg. Med. 2010, 17, 177–186. [Google Scholar] [CrossRef]
- Bursac, Z.; Gauss, C.H.; Williams, D.K.; Hosmer, D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008, 3, 17. [Google Scholar] [CrossRef]
- Silva, B.; Golay, P.; Morandi, S. Factors associated with involuntary hospitalisation for psychiatric patients in Switzerland: A retrospective study. BMC Psychiatry 2018, 18, 401. [Google Scholar] [CrossRef]
- Walker, S.; Mackay, E.; Barnett, P.; Sheridan Rains, L.; Leverton, M.; Dalton-Locke, C.; Trevillion, K.; Lloyd-Evans, B.; Johnson, S. Clinical and social factors associated with increased risk for involuntary psychiatric hospitalisation: A systematic review, meta-analysis, and narrative synthesis. Lancet Psychiatry 2019, 6, 1039–1053. [Google Scholar] [CrossRef]
- Khokhar, J.Y.; Dwiel, L.L.; Henricks, A.M.; Doucette, W.T.; Green, A.I. The link between schizophrenia and substance use disorder: A unifying hypothesis. Schizophr. Res. 2018, 194, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Swanson, L.R. Unifying Theories of Psychedelic Drug Effects. Front. Pharmacol. 2018, 9, 172. [Google Scholar] [CrossRef]
- Felson, R.B.; Staff, J. The Effects of Alcohol Intoxication on Violent Versus Other Offending. Crim. Justice Behav. 2010, 37, 1343–1360. [Google Scholar] [CrossRef]
- Degenhardt, L.; Hall, W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet 2012, 379, 55–70. [Google Scholar] [CrossRef]
- Opsal, A.; Clausen, T.; Kristensen, Ø.; Elvik, I.; Joa, I.; Larsen, T.K. Involuntary hospitalization of first-episode psychosis with substance abuse during a 2-year follow-up. Acta Psychiatr. Scand. 2011, 124, 198–204. [Google Scholar] [CrossRef][Green Version]
- Wilson, L.; Szigeti, A.; Kearney, A.; Clarke, M. Clinical characteristics of primary psychotic disorders with concurrent substance abuse and substance-induced psychotic disorders: A systematic review. Schizophr. Res. 2018, 197, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Canova Mosele, P.H.; Chervenski Figueira, G.; Antônio Bertuol Filho, A.; Ferreira de Lima, J.A.R.; Calegaro, V.C. Involuntary psychiatric hospitalization and its relationship to psychopathology and aggression. Psychiatry Res. 2018, 265, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Higashi, K.; Medic, G.; Littlewood, K.J.; Diez, T.; Granström, O.; De Hert, M. Medication adherence in schizophrenia: Factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther. Adv. Psychopharmacol 2013, 3, 200–218. [Google Scholar] [CrossRef] [PubMed]
- Levin, J.B.; Seifi, N.; Cassidy, K.A.; Tatsuoka, C.; Sams, J.; Akagi, K.K.; Sajatovic, M. Comparing medication attitudes and reasons for medication nonadherence among three disparate groups of individuals with serious mental illness. J. Nerv. Ment. Dis. 2014, 202, 769–773. [Google Scholar] [CrossRef]
- Anderson, R.L.; Lyons, J.S. Needs-based planning for persons with serious mental illness residing in intermediate care facilities. J. Behav. Health Serv. Res. 2001, 28, 104–110. [Google Scholar] [CrossRef]
- Britta Olofsson, L.J.F.G.A.N. Being in conflict: Physicians’ experience with using coercion in psychiatric care. Nord. J. Psychiatry 1999, 53, 203–210. [Google Scholar] [CrossRef]
- Zislin, J.; Kuperman, V.; Durst, R. “Ego-Dystonic” Delusions as a Predictor of Dangerous Behavior. Psychiatr. Quart. 2011, 82, 113–120. [Google Scholar] [CrossRef]
- Van Dongen, J.D.M.; Buck, N.M.L.; van Marle, H.J.C. Delusional distress partly explains the relation between persecutory ideations and inpatient aggression on the ward. Psychiatry Res. 2012, 200, 779–783. [Google Scholar] [CrossRef]
- Coid, J.W.; Ullrich, S.; Kallis, C.; Keers, R.; Barker, D.; Cowden, F.; Stamps, R. The Relationship Between Delusions and Violence: Findings From the East London First Episode Psychosis Study. JAMA Psychiatry 2013, 70, 465–471. [Google Scholar] [CrossRef]
- Freeman, D.; Garety, P.A.; Kuipers, E. Persecutory delusions: Developing the understanding of belief maintenance and emotional distress. Psychol. Med. 2001, 31, 1293–1306. [Google Scholar] [CrossRef] [PubMed]
- McNiel, D.E.; Eisner, J.P.; Binder, R.L. The Relationship Between Command Hallucinations and Violence. Psychiatr. Serv. 2000, 51, 1288–1292. [Google Scholar] [CrossRef]
- Buchanan, A.; Reed, A.; Wessely, S.; Garety, P.; Taylor, P.; Grubin, D.; Dunn, G. Acting on delusions. II: The phenomenological correlates of acting on delusions. Br. J. Psychiatry 1993, 163, 77–81. [Google Scholar] [CrossRef]
- Darrell-Berry, H.; Berry, K.; Bucci, S. The relationship between paranoia and aggression in psychosis: A systematic review. Schizophr. Res. 2016, 172, 169–176. [Google Scholar] [CrossRef]
- Roche, E.; Lyne, J.P.; O’Donoghue, B.; Segurado, R.; Kinsella, A.; Hannigan, A.; Kelly, B.D.; Malone, K.; Clarke, M. The factor structure and clinical utility of formal thought disorder in first episode psychosis. Schizophr. Res. 2015, 168, 92–98. [Google Scholar] [CrossRef]
- Manschreck, T.C.; Maher, B.A.; Winzig, L.; Candela, S.F.; Beaudette, S.; Boshes, R. Age Disorientation in Schizophrenia. J. Neuropsychiatry Clin. Neurosci. 2000, 12, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Owen, C.; Tarantello, C.; Jones, M.; Tennant, C. Violence and Aggression in Psychiatric Units. Psychiatr. Serv. 1998, 49, 1452–1457. [Google Scholar] [CrossRef]
- Zalon, M.L.; Sandhaus, S.; Kovaleski, M.; Roe-Prior, P. Hospitalized Older Adults With Established Delirium: Recognition, Documentation, and Reporting. J. Gerontol. Nurs. 2017, 43, 32–40. [Google Scholar] [CrossRef] [PubMed]
- Tarrier, N.; Kelly, J.; Maqsood, S.; Snelson, N.; Maxwell, J.; Law, H.; Dunn, G.; Gooding, P. The cognitive behavioural prevention of suicide in psychosis: A clinical trial. Schizophr. Res. 2014, 156, 204–210. [Google Scholar] [CrossRef] [PubMed]
| All Patients (n = 597) | Involuntary (n = 118) | Voluntary (n = 479) | Post-Hoc | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | df | p | df | p | |
| Sex | ||||||||||
| Male | 345 | 57.8% | 63 | 53.4% | 282 | 58.9% | 1 | 0.280 | ||
| Female | 252 | 42.2% | 55 | 46.6% | 197 | 41.1% | ||||
| Age in years | 45.02 | 17.59 SD | 48.45 | 19.17 SD | 44.15 | 17.07 SD | 596 | 0.016 * | ||
| Means of Presentation | ||||||||||
| By foot, accompanied | 132 | 22.1% | 13 | 11.0% | 119 | 24.8% | 3 | <0.001 ** | 1 | 0.001 * |
| By foot, alone | 199 | 33.3% | 7 | 5.9% | 192 | 40.1% | 1 | <0.001 ** | ||
| Ambulance | 203 | 34.0% | 58 | 49.2% | 145 | 30.3% | 1 | <0.001 ** | ||
| Police | 63 | 10.6% | 40 | 33.9% | 23 | 4.8% | 1 | <0.001 ** | ||
| Suicide Attempt Prior to Presentation | ||||||||||
| Yes | 21 | 3.5% | 3 | 2.5% | 18 | 3.8% | 1 | 0.521 | ||
| Use of Mechanical Restraint in the PED | ||||||||||
| Yes | 24 | 4.0% | 19 | 16.1% | 5 | 1.0% | 1 | <0.001 ** | ||
| Previous Psychiatric Treatment | ||||||||||
| Any indication | 514 | 86.1% | 99 | 83.9% | 415 | 86.6% | 1 | 0.441 | ||
| First episode of psychosis | 87 | 14.6% | 18 | 15.3% | 69 | 14.4% | 1 | 0.815 | ||
| (Co-morbid) Diagnosis of Substance Abuse Disorder | ||||||||||
| Substance abuse | 197 | 33.0% | 31 | 26.3% | 165 | 34.4% | 1 | 0.090 | ||
| Abuse of alcohol | 51 | 8.5% | 9 | 7.6% | 42 | 8.8% | 1 | 0.691 | ||
| Abuse of other substances | 145 | 24.3% | 22 | 18.6% | 123 | 25.7% | 1 | 0.111 | ||
| Current Use of Alcohol | ||||||||||
| Inebriation | 55 | 9.2% | 11 | 9.3% | 43 | 9.0% | 1 | 0.906 | ||
| BAC | 1.44 M | 0.97 SD | 1.83 M | 1.01 SD | 1.28 M | 0.95 SD | 29 | 0.163 | ||
| Non-Adherence to Medication | ||||||||||
| Yes | 128 | 21.4% | 45 | 38.1% | 83 | 17.3% | 1 | <0.001 ** | ||
| Living Situation | ||||||||||
| Homeless | 59 | 9.9% | 10 | 8.5% | 49 | 10.2% | 4 | 0.002 * | 1 | 0.567 |
| Lives alone | 237 | 39.7% | 36 | 30.5% | 201 | 42.0% | 1 | 0.023 | ||
| Lives with others | 161 | 27.0% | 28 | 23.7% | 133 | 27.8% | 1 | 0.376 | ||
| Psychiatric residency/nursing home | 120 | 20.1% | 39 | 33.1% | 81 | 16.9% | 1 | <0.001 ** | ||
| Refugee shelter | 12 | 2.0% | 2 | 1.7% | 10 | 2.1% | 1 | 0.786 | ||
| All Patients (n = 597) | Involuntary (n = 118) | Voluntary (N = 479) | Post-Hoc | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | df | p | df | p | |
| Organic mental disorders (F0) | 41 | 6.9% | 16 | 13.6% | 25 | 5.2% | 7 | 0.006 * | 1 | 0.004 * |
| Substance-related disorders (F1) | 62 | 10.4% | 9 | 7.6% | 53 | 11.1% | 1 | 0.273 | ||
| Schizophrenia, schizotypal, and delusional disorders (F2) | 407 | 68.2% | 83 | 70.3% | 324 | 67.6% | 1 | 0.573 | ||
| Mania and bipolar affective disorders (F30–F31) | 25 | 4.2% | 6 | 5.1% | 19 | 4.0% | 1 | 0.587 | ||
| Depressive disorders (F32–33) | 45 | 7.5% | 3 | 2.5% | 42 | 8.8% | 1 | 0.022 * | ||
| Neurotic, stress-related, and somatoform disorders (F4) | 7 | 1.2% | 0 | 0.0% | 7 | 1.5% | 1 | 0.187 | ||
| Personality and behavior disorders (F6) | 7 | 1.2% | 0 | 0.0% | 7 | 1.5% | 1 | 0.187 | ||
| “Others” (F5, 7–9) | 3 | 0.5% | 1 | 0.8% | 2 | 0.4% | 1 | 0.554 | ||
| Aspect of PPA | All Patients | Involuntary | Voluntary | chi | df | p | |||
|---|---|---|---|---|---|---|---|---|---|
| n = 597 | % | n = 118 | % | n = 479 | % | ||||
| Disturbances of Orientation | |||||||||
| Any disturbance of disorientation | 92 | 15.4% | 45 | 38.1% | 47 | 9.8% | 58.265 | 1 | <0.001 ** |
| Impairment of Cognition | |||||||||
| Any cognitive impairment | 439 | 73.5% | 97 | 82.2% | 342 | 71.4% | 5.679 | 1 | 0.017 * |
| Formal Thought Disorders | |||||||||
| Any formal thought disorder | 503 | 84.3% | 106 | 89.8% | 397 | 82.9% | 3.447 | 1 | 0.063 |
| Accelerated thinking | 92 | 15.4% | 18 | 15.3% | 74 | 15.4% | 0.003 | 1 | 0.956 |
| Inhibited/retarded thinking | 128 | 21.4% | 25 | 21.2% | 103 | 21.5% | 0.006 | 1 | 0.938 |
| Circumstantial thinking | 110 | 18.4% | 17 | 14.4% | 93 | 19.4% | 1.580 | 1 | 0.209 |
| Restricted thinking | 126 | 21.1% | 7 | 5.9% | 119 | 24.8% | 20.335 | 1 | <0.001 ** |
| Tangential thinking | 81 | 13.6% | 35 | 29.7% | 46 | 9.6% | 32.480 | 1 | <0.001 ** |
| Incoherence/derailment | 185 | 31.0% | 63 | 53.4% | 122 | 25.5% | 34.511 | 1 | <0.001 ** |
| Worries and Compulsions | |||||||||
| Any worry or compulsion | 335 | 56.1% | 49 | 41.5% | 286 | 59.7% | 12.710 | 1 | <0.001 ** |
| Suspiciousness | 151 | 25.3% | 46 | 39.0% | 105 | 21.9% | 14.587 | 1 | <0.001 ** |
| Fears | 255 | 42.7% | 17 | 14.4% | 238 | 49.7% | 48.160 | 1 | <0.001 ** |
| Delusions | |||||||||
| Any delusion | 520 | 87.1% | 104 | 88.1% | 416 | 86.8% | 0.140 | 1 | 0.708 |
| Delusions of reference | 114 | 19.1% | 19 | 16.1% | 95 | 19.8% | 0.853 | 1 | 0.356 |
| Delusions of persecution | 376 | 63.0% | 64 | 54.2% | 312 | 65.1% | 4.823 | 1 | 0.028 |
| Evidence of delusions | 64 | 10.7% | 25 | 21.2% | 39 | 8.1% | 16.832 | 1 | <0.001 ** |
| Disorders of Perception | |||||||||
| Any type of hallucination | 325 | 54.4% | 58 | 49.2% | 267 | 55.7% | 1.657 | 1 | 0.198 |
| Hearing voices | 165 | 27.6% | 17 | 14.4% | 148 | 30.9% | 12.874 | 1 | <0.001 ** |
| Visual hallucinations | 73 | 12.2% | 18 | 15.3% | 55 | 11.5% | 1.255 | 1 | 0.263 |
| Bodily hallucinations | 62 | 10.4% | 4 | 3.4% | 58 | 12.1% | 7.733 | 1 | 0.005 * |
| Evidence of hallucinations | 41 | 6.9% | 23 | 19.5% | 18 | 3.8% | 36.643 | 1 | <0.001 ** |
| Ego (Boundary) Disturbances | |||||||||
| Any ego disturbance | 148 | 24.8% | 19 | 16.1% | 129 | 26.9% | 5.955 | 1 | 0.015 * |
| Disturbances of Affect | |||||||||
| Any disturbance of affect | 525 | 87.9% | 106 | 89.8% | 419 | 87.5% | 0.496 | 1 | 0.481 |
| Blunted affect | 133 | 22.3% | 28 | 23.7% | 105 | 21.9% | 0.179 | 1 | 0.672 |
| Depressed mood | 278 | 46.6% | 24 | 20.3% | 254 | 53.0% | 40.657 | 1 | <0.001 ** |
| Anxiety | 72 | 12.1% | 4 | 3.4% | 68 | 14.2% | 10.425 | 1 | 0.001 * |
| Dysphoria/irritability | 175 | 29.3% | 69 | 58.5% | 106 | 22.1% | 60.358 | 1 | <0.001 ** |
| Inner restlessness | 61 | 10.2% | 5 | 4.2% | 56 | 11.7% | 5.734 | 1 | 0.017 * |
| Disorders of Drive and Psychomotor Activity | |||||||||
| Inhibition/lack of drive | 195 | 32.7% | 22 | 18.6% | 173 | 36.1% | 13.142 | 1 | <0.001 ** |
| Increased drive | 178 | 29.8% | 64 | 54.2% | 114 | 23.8% | 41.916 | 1 | <0.001 ** |
| Motor restlessness | 293 | 49.1% | 83 | 70.3% | 210 | 43.8% | 26.599 | 1 | <0.001 ** |
| Motor retardation | 61 | 10.2% | 13 | 11.0% | 48 | 10.0% | 0.102 | 1 | 0.749 |
| Mutism/poverty of speech | 74 | 6.8% | 35 | 29.7% | 39 | 8.1% | 40.374 | 1 | <0.001 ** |
| Logorrhea/pressure of speech | 68 | 11.4% | 20 | 16.9% | 48 | 10.0% | 4.503 | 1 | 0.034 * |
| Other Disturbances | |||||||||
| Social withdrawal | 29 | 4.9% | 3 | 2.5% | 26 | 5.4% | 1.706 | 1 | 0.192 |
| Excessive social contact | 51 | 8.5% | 26 | 22.0% | 25 | 5.2% | 34.262 | 1 | <0.001 ** |
| Aggressiveness | 90 | 15.1% | 57 | 48.3% | 33 | 6.9% | 126.845 | 1 | <0.001 ** |
| Suicidal thoughts | 139 | 23.3% | 28 | 23.7% | 111 | 23.2% | 0.016 | 1 | 0.899 |
| Suicidal intent | 34 | 5.7% | 13 | 11.0% | 21 | 4.4% | 7.755 | 1 | 0.005 * |
| Lack of insight | 153 | 25.6% | 90 | 76.3% | 63 | 13.5% | 197.895 | 1 | <0.001 ** |
| Sociodemographic and Circumstantial Characteristics | OR | 95% CI | p-Value | |
|---|---|---|---|---|
| LL | UL | |||
| Ambulance | 2.95 | 1.66 | 5.26 | <0.001 ** |
| Police escort | 10.84 | 5.12 | 22.93 | <0.001 ** |
| (Comorbid) substance use disorder | 0.53 | 0.28 | 0.99 | 0.048 * |
| Non-adherence to medication | 2.39 | 1.37 | 4.16 | 0.002 * |
| Psychiatric residency/nursing home | 2.76 | 1.56 | 4.90 | 0.001 * |
| Use of mechanical restraint in PED | 13.31 | 3.91 | 45.31 | <0.001 ** |
| Aspect of PPA | OR | 95% CI | p-Value | |
|---|---|---|---|---|
| LL | UL | |||
| Disorientation | 4.66 | 2.46 | 8.83 | <0.001 ** |
| Aggressiveness | 6.18 | 3.24 | 11.80 | <0.001 ** |
| Tangential thinking | 3.95 | 2.08 | 7.52 | <0.001 ** |
| Suspiciousness | 2.80 | 1.52 | 5.17 | 0.001 * |
| Fears | 0.25 | 0.13 | 0.49 | <0.001 ** |
| Suicidal intent | 5.54 | 2.29 | 13.43 | <0.001 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seifert, J.; Ihlefeld, C.; Zindler, T.; Eberlein, C.K.; Deest, M.; Bleich, S.; Toto, S.; Meissner, C. Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis. Psychiatry Int. 2021, 2, 310-324. https://doi.org/10.3390/psychiatryint2030024
Seifert J, Ihlefeld C, Zindler T, Eberlein CK, Deest M, Bleich S, Toto S, Meissner C. Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis. Psychiatry International. 2021; 2(3):310-324. https://doi.org/10.3390/psychiatryint2030024
Chicago/Turabian StyleSeifert, Johanna, Christian Ihlefeld, Tristan Zindler, Christian K. Eberlein, Maximilian Deest, Stefan Bleich, Sermin Toto, and Catharina Meissner. 2021. "Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis" Psychiatry International 2, no. 3: 310-324. https://doi.org/10.3390/psychiatryint2030024
APA StyleSeifert, J., Ihlefeld, C., Zindler, T., Eberlein, C. K., Deest, M., Bleich, S., Toto, S., & Meissner, C. (2021). Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis. Psychiatry International, 2(3), 310-324. https://doi.org/10.3390/psychiatryint2030024






