Abstract
Cannabis and opioids are substances that affect reproductive health. Opioids suppress testosterone and studies have shown that cannabis may increase testosterone. However, there is minimal research describing the endocrine effects of concurrent cannabis and opioid use. We hypothesize that cannabis use improves opioid-induced testosterone suppression. To test this hypothesis, we used cross-sectional data from a prospective cohort study including 122 men enrolled in methadone maintenance treatment (MMT). We measured serum testosterone with an enzyme-linked immunosorbent assay at study enrolment. Urine drug screens were collected for 15 months and identified 52.5% of participants (n = 64) as cannabis users. The association between cannabis use and testosterone level was examined using regression models with serum testosterone as the dependent variable. In our multivariable regression, methadone dose was associated with lower serum testosterone (β = −0.003, 95% CI-0.005, −0.001, p = 0.003). However, neither cannabis use as a dichotomous variable nor the percentage of cannabis-positive urine drug screens were significantly associated with serum testosterone (β = 0.143, 95% CI −0.110, 0.396, p = 0.266, and β = 0.002, 95% CI > −0.001, 0.005, p = 0.116, respectively). Therefore, it does not appear that cannabis has an association with testosterone levels in men on MMT.
1. Introduction
Testosterone levels in men are associated with many markers of general and reproductive health. This hormone is known to be positively correlated with bone mineral density, muscle mass, sex drive, sperm count, and energy levels [1]. Opioids are known to suppress testosterone levels, leading to a clinical syndrome defined as opioid-induced androgen deficiency (OPIAD) [2]. Furthermore, the prevalence of opioid use disorder (OUD) has led clinicians to employ harm-reduction strategies such as methadone maintenance treatment (MMT). Unfortunately, previous studies show that methadone dose is inversely correlated with testosterone levels in the MMT population [3]. Converse to the effect of opioids, there are some studies that report that cannabis use may elevate serum testosterone levels in men, [4,5] albeit inconsistently [6,7]. Further, it has been observed that the prevalence of cannabis use is higher in patients on opioids [8,9,10]. Therefore, it is worthwhile to understand the effect of concurrent opioid and cannabis use on serum testosterone.
The legalization of cannabis in many jurisdictions is occurring in the setting of an ongoing crisis of opioid use, opioid use disorder (OUD) and opioid-related deaths. Despite variability in the legality of its use, 18% of Canadians and 8.4% of Americans aged 15–64 years old reported past-year cannabis use in 2019 [11] and 2017 [12], respectively. Furthermore, an estimated 2.5% of the world’s population reports using this drug [13]. Altogether, cannabis is the most prevalent illicit drug worldwide [13]. Among patients prescribed chronic opioid therapy, rates of cannabis use are estimated to be up to 39%, compared to 5.8% of the general population [8]. Among patients receiving treatment for OUD, the prevalence of cannabis use is even higher at about 50% [9]. Nearly 30% of these patients meet the criteria for cannabis use disorder [10]. Despite concerns about the increasing prevalence of cannabis and opioids, there is a lack of research describing the endocrine effects of concurrent use.
The hypothalamic-pituitary-gonadal (HPG) axis controls the production of primary sex hormones testosterone and estradiol. Gonadotrophin-releasing hormone (GnRH) is released from the hypothalamus, which stimulates the anterior pituitary to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH). In men, LH stimulates the testes to produce testosterone and FSH stimulates spermatogenesis. Opioid-induced androgen deficiency (OPIAD) is a well-described clinical syndrome characterized by central hypogonadism [2]. These patients often present with fatigue, decreased libido, and erectile dysfunction. Opioids inhibit the HPG axis at all levels, causing decreased serum levels of GnRH, FSH, LH, and testosterone [2]. One systematic review and meta-analysis found that testosterone was 167.78 ng/dL lower in men who use opioids compared to controls (mean difference = −167.78; 95% CI = −247.47, −84.08, p < 0.0001) [14].
Overall, both cannabis and opioids have potentially detrimental effects on the endocrine system in men [2,6]. Interestingly, other studies showed that frequency and/or recency of cannabis use may be associated with elevated testosterone levels [4,5]. However, the clinical implications of concurrent opioid and cannabis use requires further study. To our knowledge, there have been no studies evaluating the effects of cannabis use in the MMT population. Using data from 122 men enrolled in MMT, we aimed to see if cannabis use was associated with serum testosterone. We hypothesized that cannabis use is associated with higher serum testosterone in patients enrolled in MMT.
2. Materials and Methods
2.1. Data and Outcome Measures
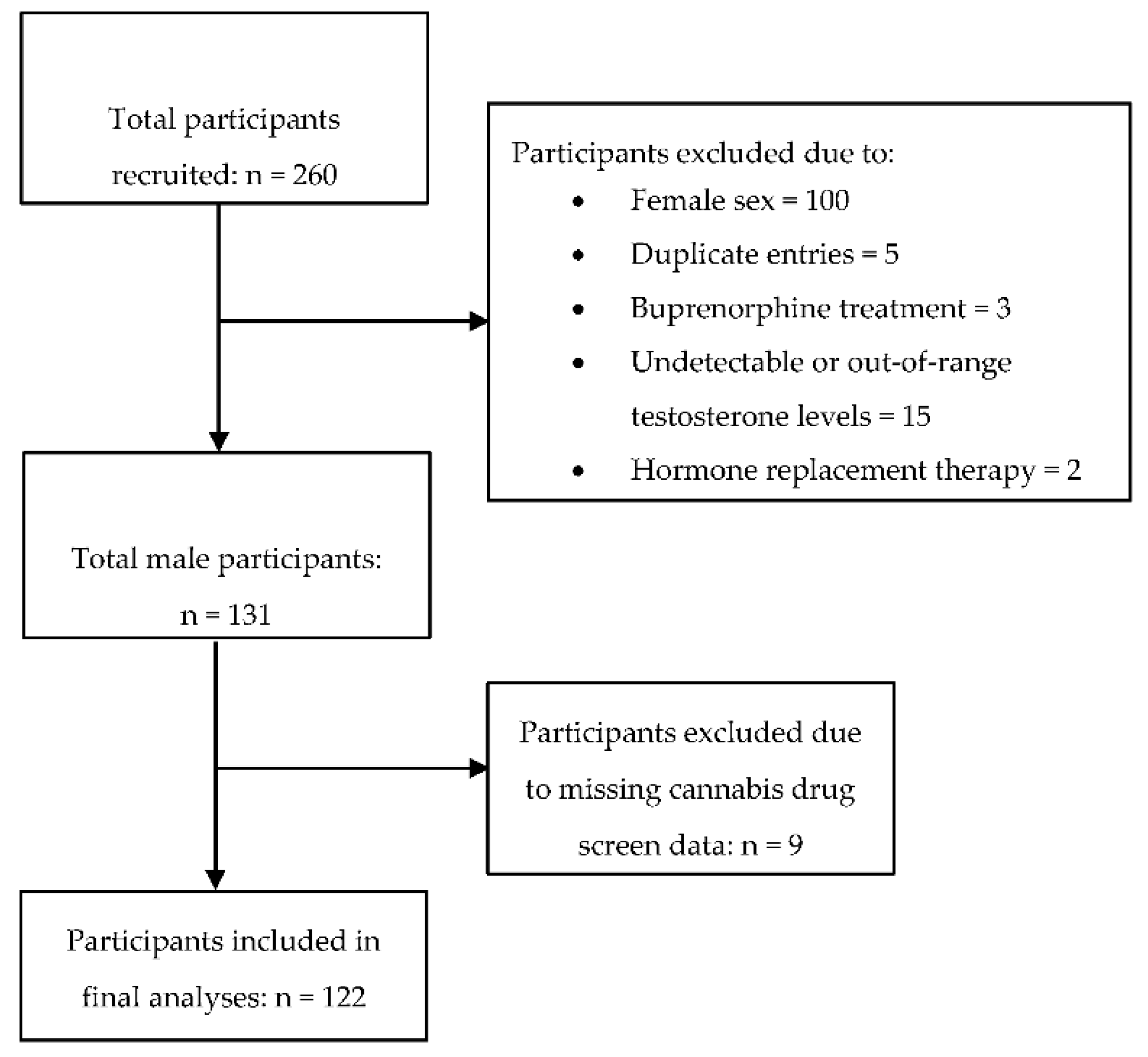
In this study, we used data from the GENetics of Opioid Addiction (GENOA) study for which the study protocol and methods have been previously described [3,15]. Participants were recruited from community-based addiction clinics in Southern Ontario, Canada between June and December 2011. Participants met the study inclusion criteria if they were age 18 years and older, had a diagnosis of OUD based on Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria [16], were enrolled in MMT, and were able to provide verbal and written informed consent. For the analyses in this study, we included only men (Figure 1; Study Flow Diagram). This study was carried out in accordance with ethical guidelines and approval by the Hamilton Integrated Research Ethics Board (HIREB) (GENOA project ID 11-056) and written informed consent was obtained from each study participant.

Figure 1.
Study flow diagram.
All participants completed an extensive assessment at study intake, in which they provided information on demographic variables, clinical history including current medications dose and duration, medical history, and psychiatric and substance use history. Participants provided serum samples at study entry for the assessment of testosterone levels. Serum total testosterone was measured using the enzyme-linked immunosorbent assay (ELISA) technique (Enzo Life Sciences, Plymouth Meeting, PA, USA); intra-assay variation is 3.3%, while inter-assay variation is 9.8%, with a sensitivity of 2.6%. Additionally, cannabis urine drug screens were available for up to 3 months before study enrolment. Finally, all participants were followed for 12 months with urine drug screen monitoring, as per the routine clinical protocol, such that we were able to calculate the percentage of opioid-positive urine and cannabis-positive drug screens for each participant.
2.2. Analysis
All analyses were conducted using Stata Version 16.0 (StataCorp LP, College Station, TX, USA). We summarized continuous variables as mean and standard deviation (SD) when normally distributed, and as median and interquartile range (IQR) when non-normally distributed. We summarized dichotomous variables using percentages. We assessed group differences using independent samples t-tests for continuous variables and chi-squared analysis for dichotomous variables.
To examine the association between cannabis use and serum testosterone level, we performed unadjusted and adjusted regression models with serum testosterone as the dependent variable. Participants were defined as “cannabis users” if cannabis was detected on one or more urine drug screens and “non-users” if it was not. Since testosterone levels followed a non-normal distribution, we transformed the data using the natural logarithm. Due to sample size limitations, we first conducted unadjusted regression analyses including each of the following independent variables: age, age of initial opioid use, cigarettes per day, methadone dose, duration on MMT, continuing illicit opioid use while on treatment with methadone during 12 months post enrolment, BMI, the presence of cannabis on any urine drug screen, and the percent of cannabis-positive urine drug screens during the 15 months for which this data was available. We then used the results of the unadjusted analyses to determine which variables to include in our adjusted multivariable models.
We removed continuing illicit opioid use and age of initial opioid use because of their presumed overlap with the effects of methadone treatment and duration on MMT, respectively. Our two models included either cannabis detected on any urine drug screen as a dichotomous variable or the percent of positive cannabis urine drug screens. All other variables were included. We reported the results of the regression analysis using Beta-coefficients (β) with a 95% confidence interval (CI) and associated p-value. For all analyses, the level of significance for hypothesis testing was set at alpha = 0.05 (Supplementary Materials). Our sample size of 122 participants was sufficiently powered to conduct the analyses described above, such that there were at least 10 participants per covariate included in the model [17]. The study is reported in adherence to the Strengthening of Reporting of Observational Studies in Epidemiology (STROBE) statement for observational studies [18].
3. Results
3.1. Demographic and Clinical Characteristics
Altogether, 122 participants were included in the analysis (Figure 1). Based on the urine drug screen results, 52.5% of participants were considered to be “cannabis users.” The mean percentage of cannabis-positive urine drug screens amongst cannabis users was 79.5% (SD = 29.4) (Table 1). Cannabis users did not differ from non-users in mean age (37.6 years (SD = 11) versus 40.1 years (SD = 11), p = 0.212; Table 1). However, cannabis users showed a trend towards higher serum testosterone than non-users (110.8 versus 88.2 ng/dL, p = 0.096; Table 1). They also showed a trend towards higher rates of polysubstance use than non-users (51.6% versus 35.1%, p = 0.062; Table 1). For all other variables examined, these groups did not differ significantly (Table 1).

Table 1.
Demographic and clinical characteristics (n = 122).
3.2. Factors Associated with Serum Testosterone
In our unadjusted analyses, serum testosterone was inversely correlated with methadone dose (estimated β = −0.003; 95% CI −0.005, >−0.001; p = 0.004) and positively correlated with the percentage of cannabis-positive urine drug screens (estimated β = 0.003; 95% CI < 0.001, 0.006; p = 0.035) (Table 2). However, the dichotomous presence or absence of cannabis on urine drug screen was not significantly associated with serum testosterone level (β = 0.20; 95% CI −0.057, 0.460; p = 0.124).

Table 2.
Unadjusted and adjusted models of factors associated with serum testosterone.
In our adjusted multivariable regression (Table 2), only methadone dose was significantly associated with testosterone, (estimated β = −0.0030; 95% CI = −0.0050, −0.0010; p < 0.003) indicating that higher doses of methadone suppress serum testosterone levels. Similarly, when we excluded cigarette smoking from the adjusted multivariable regression model, only methadone dose was significantly associated with testosterone (estimated β = −0.027; 95% CI = −0.005, −0.008, p = 0.006). No other variables were significantly associated with serum testosterone. The percentage of cannabis-positive urine drug screens was not associated with serum testosterone when included in the multivariable regression model (estimated β = 0.0022; 95% CI = −0.00056, 0.0050, p = 0.116). Furthermore, the dichotomous presence or absence of cannabis on urine drug screen was not associated with serum testosterone (β = 0.143, 95% CI = −0.11, 0.4, p = 0.266) when included in our multivariable regression model in place of the “percent of cannabis-positive urine drug screens” (Table 2).
4. Discussion
The objective of this study was to explore the association of cannabis on serum testosterone in men receiving MMT for OUD. Consistent with the previous literature on OPIAD [2,3,19], the results of our adjusted regression model confirm that MMT displays a dose-dependent suppression of serum testosterone. However, when controlling for other variables, neither cannabis-use nor the percentage of cannabis-positive urine drug screens within the 15-month study period were significantly associated with serum testosterone. These results suggest that cannabis use is not associated with serum testosterone levels in this population of men, despite findings from previous studies to suggest that frequency and/or recency of cannabis use may be associated with higher serum testosterone levels [4,5,6]. However, due to the limited literature in the field, it is unclear whether our results are generalizable outside of the male MMT population.
Previous studies investigated the association between cannabis use and testosterone level. However, most of the studies were conducted several decades ago before the current trend of increasing cannabis use and using modest sample sizes [7]. The variability in study design, sampling methods, and lack of consistent results render these studies inconclusive [7]. However, there are three larger and more recent questionnaire-based studies that reported correlations between cannabis use and serum testosterone levels [4,5,6]. In a study of 1215 Danish men aged 18–28, Gundersen et al. found that testosterone was 7% (95% CI: 0, 14) higher in those that used cannabis more than once weekly, compared to never users [4]. This relative increase in serum testosterone was found after controlling for BMI, tobacco smoking, and time of day of blood draw. However, they were not able to separate this finding from the effect of cigarette smoking [4], a variable known to elevate serum testosterone [20]. In a study of 1577 men from the 2011–2012 US National Health and Nutrition Examination Survey, time since the last regular use of cannabis was inversely correlated with serum testosterone (p < 0.02) [5]. This trend was strengthened (p < 0.01) when restricting for men aged 18–28 years old [5]. Together, these findings suggest that cannabis use and recency of use may be correlated with serum testosterone levels.
Given the lack of literature describing the effect of concurrent cannabis and opioid use on serum testosterone, there are several potential interpretations of our results. Assuming that cannabis use does elevate serum testosterone, we may not have been able to replicate this finding in our population for several reasons. Based on the previous literature [4,5], we know that cannabis use may acutely elevate testosterone in healthy men aged 18-28 years old. However, in our study, cannabis users and non-users had average ages of 37.6 (SD = 11.0) and 40.1 (SD = 11.0), respectively. In our model, we controlled for age as a variable directly correlated with serum testosterone. However, we cannot exclude the possibility that cannabis elevates serum testosterone through an age-dependent mechanism. Unfortunately, our sample size was not large enough to recreate this age-restricted analysis without our model becoming under-powered.
As Leydig cells age, their ability to produce testosterone decreases due to acquired defects in intracellular steroidogenic pathways [21]. Cannabis is known to mediate its effects primarily through its active component, THC. THC binds to CB1 and CB2 receptors in the testis, vas deferens, and anterior pituitary, etc. [22]. If cannabis does elevate serum testosterone, the distribution of receptors suggests that this effect may be through direct interaction with cannabinoid receptors in the testis and/or effects on the HPA axis. However, age-related Leydig cell dysfunction may also account for a decreased response in serum testosterone to cannabis use. If this hormonal elevation is an age-dependent phenomenon, the effect may have been diluted in our study due to the high proportion of older individuals.
To our knowledge, this is the first study of its kind to investigate the effects of cannabis use in a population of men with risk factors for testosterone deficiency (namely, opioid use). The mean serum testosterone levels of cannabis users and non-users in our study were 110.8 (SD = 83.9) and 88.2 ng/dL (SD = 61.6), respectively. Bawor et al. studied the effects of MMT on serum testosterone in men by comparing their study population to healthy controls aged 46.2 (SD = 13.1, n = 287) [3]. This control group had a mean serum testosterone of 414.74 ng/dL (SD = 141.8) [3]. In comparison, it is clear that testosterone levels are suppressed in our study population, regardless of cannabis use. Therefore, it is possible that the testosterone-suppressing effects of methadone are much stronger than any potential testosterone-elevating effects cannabis may have. This is an area that requires further investigation with larger sample sizes.
The results of our study raise the possibility that cannabis is not significantly associated with serum testosterone in men receiving MMT for OUD. Nassan et al. attempted to determine if cannabis use is associated with serum concentrations of reproductive hormones [6]. Overall, testosterone did not differ significantly between never, ever, past, and current users [6]. This finding is consistent with the results of our study. However, due to the inability to quantify the exact amount of cannabis use with urine drug screens, we were unable to determine if there is a critical dose above which cannabis elevates testosterone. Furthermore, removing cigarette smoking from our regression models did not significantly alter the findings of this study. The inconsistency within the literature regarding the impact of cannabis use on testosterone levels indicates the need for ongoing investigation. This investigation is particularly important considering the global trend towards legalizing cannabis, increasing rates of use (particularly among males), and the public perception that there are minimal adverse effects of cannabis use [23].
The primary strength of our study design was the use of objective parameters, such as urine drug screens, to define cannabis users. Previous studies [4,5,6] define and categorize cannabis users based on self-report questionnaires. These studies are subject to reporting bias, false information, and inaccurate recall of timelines by participants. By defining cannabis-users as those with positive urine drug screens, we can objectively confirm that all participants in that group used cannabis at least once within our 15-month study period. Finally, our longitudinal study design that included measuring drug use for 15 months rather than a cross-sectional association is also a strength of the current study.
The limitations of our study include variability in the measurement of serum testosterone; for example, we did not control for physical activity levels or time of day of blood draw. However, all serum samples were obtained between 8 am and 12 pm, minimizing any diurnal variation. Furthermore, some variables in this study, including smoking, were based on self-report. Although our definition of cannabis use was robust, we were not able to determine the dose of cannabis consumed or frequency of use based on the urine drug screen. Additionally, we did not have the data to perform a sub-analysis using only the urine drug screens collected before enrolment. Finally, our study is limited by it’s small sample size (n = 122). This sample size is approximately one-tenth of others who have previously studied the impact of cannabis on testosterone (n = 1215 [4], n = 1577 [5]).
The results of this study raise the question of whether or not cannabis is truly able to elevate serum testosterone and if so, how [4,5,6]? Future studies should focus on exploring a potential age-dependent mechanism of cannabis-induced serum testosterone elevation. We recommend that objective criteria, such as cannabis drug screens, should be combined with larger sample sizes to ensure that the methodology of future investigations is as robust as possible. Sample sizes should be large enough to ensure that all known confounders of serum testosterone can be accounted for with adequate power. Furthermore, it may be valuable to objectively quantify cannabis use to see if there is a dose-response relationship with serum testosterone. Finally, additional clinical and laboratory studies are needed to elucidate a potential mechanistic interaction between endogenous cannabinoid and opioid signaling pathways that may explain the results of this study.
5. Conclusions
As previously established, methadone dose appears to be inversely correlated with testosterone levels. However, in individuals who are on MMT, it does not appear that cannabis use can meaningfully elevate serum testosterone. The literature on the endocrine effects of cannabis is growing but currently inconclusive. Our results suggest that any potential association between cannabis use and testosterone level is insignificant compared to the testosterone-suppressing effects of opioids. Based on this information, cannabis is not a viable option to treat symptoms of hypogonadism in men with OPIAD. However, this interaction requires further study with larger sample sizes. As the cannabis literature continues to grow, clinicians ought to start weighing any potential benefit this drug may bring against its associated risks.
Supplementary Materials
The following are available online at https://www.mdpi.com/2673-5318/1/2/8/s1, Table S1: original data.
Author Contributions
Conceptualization, D.B.C. and T.R.; methodology, T.R., M.B., and Z.S.; software, D.B.C. and T.R.; validation, D.C., T.R., M.B., and Z.S.; formal analysis, Z.S.; investigation, D.B.C. and T.R.; resources, Z.S.; data curation, D.B.C. and T.R.; writing—original draft preparation, D.C.; writing—review and editing, T.R., M.B., and Z.S.; visualization, T.R.; supervision, T.R. and Z.S.; project administration, T.R. and Z.S.; funding acquisition, T.R., M.B., and Z.S. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Canadian Institutes of Health Research (CIHR) Drug Safety and Effectiveness Network (DSEN) grant (grant number 126639), the CIHR Award (grant number PJT-156306), and the CIHR Cannabis Catalyst grant (grant number SHI-155404). This work was also supported by an Innovation Award from the Department of Psychiatry and Behavioural Neurosciences, McMaster University (grant number 2-15311).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vineet, T.; Michael, S.; Richard, S.Y.; Frank, A.L.; Loren, W.G. Revisiting the role of testosterone: Are we missing something? Rev. Urol. 2017, 19, 16–24. [Google Scholar]
- O’Rourke, T.K.; Wosnitzer, M.S. Opioid-Induced Androgen Deficiency (OPIAD): Diagnosis, management, and literature review. Curr. Urol. Rep. 2016, 17, 76. [Google Scholar] [CrossRef] [PubMed]
- Bawor, M.; Dennis, B.B.; Samaan, M.C.; Plater, C.; Worster, A.; Varenbut, M.; Daiter, J.; Marsh, D.C.; Desai, D.; Steiner, M.; et al. Methadone induces testosterone suppression in patients with opioid addiction. Sci. Rep. 2014, 4, 6189. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, T.D.; Jørgensen, N.; Andersson, A.; Bang, A.K.; Nordkap, L.; Skakkebæk, N.E.; Priskorn, L.; Juul, A.; Jensen, T.K. Association between use of marijuana and male reproductive hormones and semen quality: A study among 1,215 healthy young men. Am. J. Epidemiol. 2015, 182, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Thistle, J.E.; Graubard, B.I.; Braunlin, M.; Vesper, H.; Trabert, B.; Cook, M.B.; McGlynn, K.A. Marijuana use and serum testosterone concentrations among U.S. males. Andrology 2017, 5, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Nassan, F.L.; Arvizu, M.; Mínguez-Alarcón, L.; Williams, P.L.; Attaman, J.; Petrozza, J.; Hauser, R.; Chavarro, J.; EARTH Study Team. Marijuana smoking and markers of testicular function among men from a fertility centre. Hum. Reprod. 2019, 34, 715–723. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, P.; Clavijo, R.I. Adverse effects of cannabis on male reproduction. Eur. Urol. Focus 2018, 4, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Reisfield, G.M.; Wasan, A.D.; Jamison, R.N. The prevalence and significance of cannabis use in patients prescribed chronic opioid therapy: A Review of the Extant Literature. Pain Med. 2009, 10, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Zielinski, L.; Bhatt, M.; Sanger, N.; Plater, C.; Worster, A.; Varenbut, M.; Daiter, J.; Pare, G.; Marsh, D.C.; Desai, D.; et al. Association between cannabis use and methadone maintenance treatment outcomes: An investigation into sex differences. Biol. Sex Differ. 2017, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Rosic, T.; Naji, L.; Bawor, M.; Dennis, B.B.; Plater, C.; Marsh, D.C.; Thabane, L.; Samaan, Z. The impact of comorbid psychiatric disorders on methadone maintenance treatment in opioid use disorder: A prospective cohort study. Neuropsychiatr. Dis. Treat. 2017, 13, 1399–1408. [Google Scholar] [CrossRef] [PubMed]
- Analysis of Trends in the Prevalence of Cannabis Use and Related Metrics in Canada. Government of Canada, Statistics Canada. Available online: https://www150.statcan.gc.ca/n1/pub/82-003-x/2019006/article/00001-eng.htm (accessed on 16 August 2020).
- United Nations. World Drug Report 2019 (Booklet 5); United Nations Publication: Vienna, Austria, 2019. [Google Scholar]
- Cannabis. World Health Organization. Available online: https://www.who.int/substance_abuse/facts/cannabis/en/ (accessed on 16 August 2020).
- Bawor, M.; Bami, H.; Dennis, B.B.; Plater, C.; Worster, A.; Varenbut, M.; Daiter, J.; Marsh, D.C.; Steiner, M.; Anglin, R.; et al. Testosterone suppression in opioid users: A systematic review and meta-analysis. Drug Alcohol Depend. 2015, 149, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Samaan, Z.; Bawor, M.; Dennis, B.B.; Plater, C.; Varenbut, M.; Daiter, J.; Worster, A.; Marsh, D.C.; Tan, C.; Desai, D.; et al. Genetic influence on methadone treatment outcomes in patients undergoing methadone maintenance treatment for opioid addiction: A pilot study. Neuropsychiatr. Dis. Treat. 2014, 10, 1503–1508. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Rhodin, A.; Stridsberg, M.; Gordh, T. Opioid Endocrinopathy: A clinical problem in patients with chronic pain and long-term oral opioid treatment. Clin. J. Pain 2010, 26, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Leung, J.Y.Y.; Lin, S.L.; Schooling, C.M. Cigarette smoking and testosterone in men and women: A systematic review and meta-analysis of observational studies. Prev. Med. 2016, 85, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Beattie, M.C.; Adekola, L.; Papadopoulos, V.; Chen, H.; Zirkin, B.R. Leydig cell aging and hypogonadism. Exp. Gerontol. 2015, 68, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Rossato, M.; Popa, F.I.; Ferigo, M.; Clari, G.; Foresta, C. Human sperm express cannabinoid receptor Cb1, the activation of which inhibits motility, acrosome reaction, and mitochondrial function. J. Clin. Endocrinol. Metab. 2005, 90, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Rottermann, M.; Langlois, K. Health Reports Prevalence and correlates of marijuana use in Canada, 2012. Health Rep. 2015, 26, 10–15. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).