RNA-Based Next-Generation Sequencing in the Somatic Molecular Testing of Non-Small-Cell Lung Cancer (NSCLC) in a Centralized Model: Real-World Data to Suggest It Is Time to Reconsider Testing Options
Abstract
1. Introduction
2. RNA Sequencing: The Real-World Experience of a Centralized Model of Clinical Somatic Testing
2.1. Failure Rate of RNA Sequencing
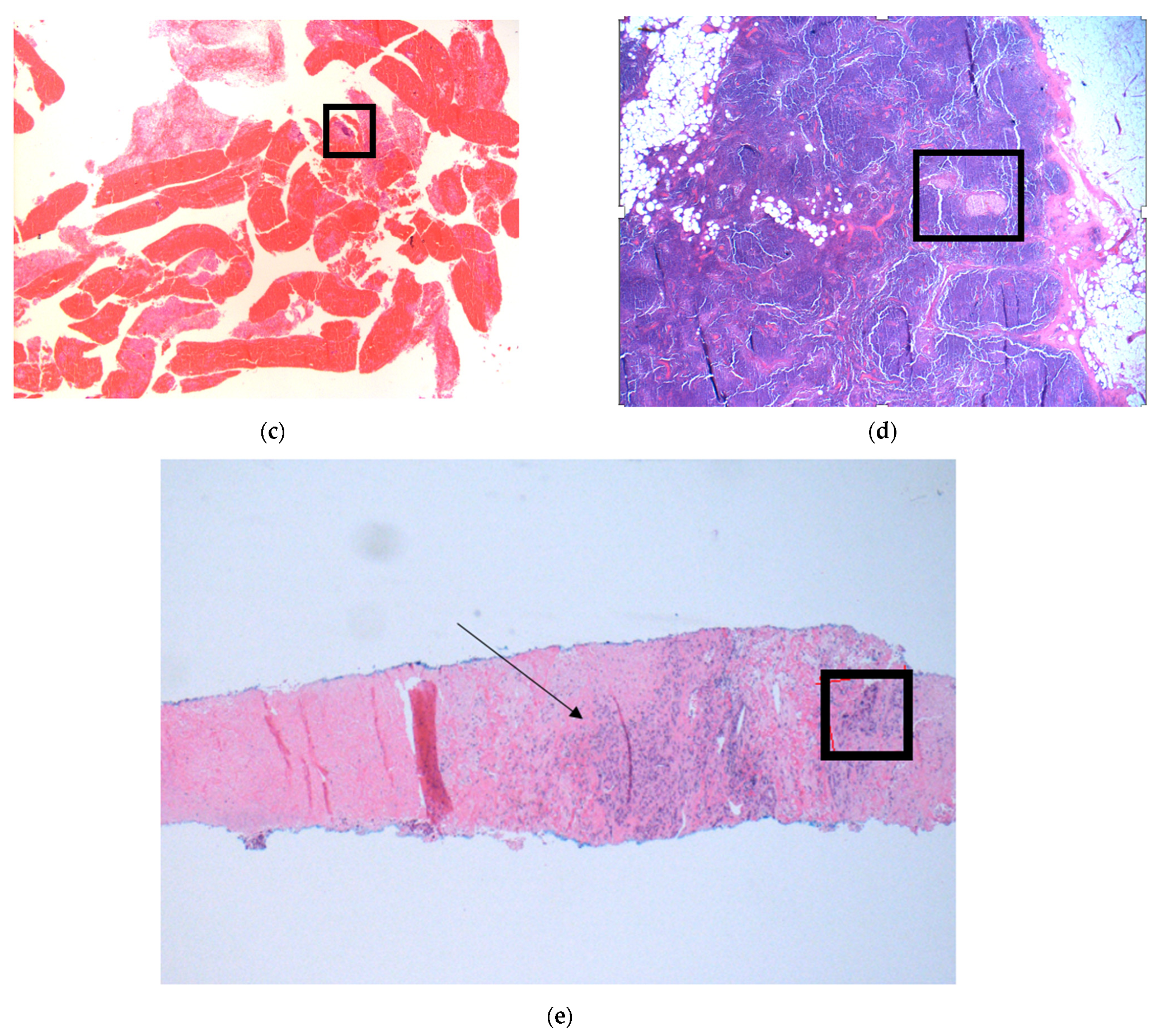
2.2. Pre-Analytical Considerations
2.3. Timeliness of RNA Sequencing
2.4. Tissue Consumption
2.5. Further Consequences of Failed RNA NGS
2.6. Why Does RNA Sequencing Fail So Frequently in Our Experience?
2.7. Practical Alternatives to Centralized NGS Testing
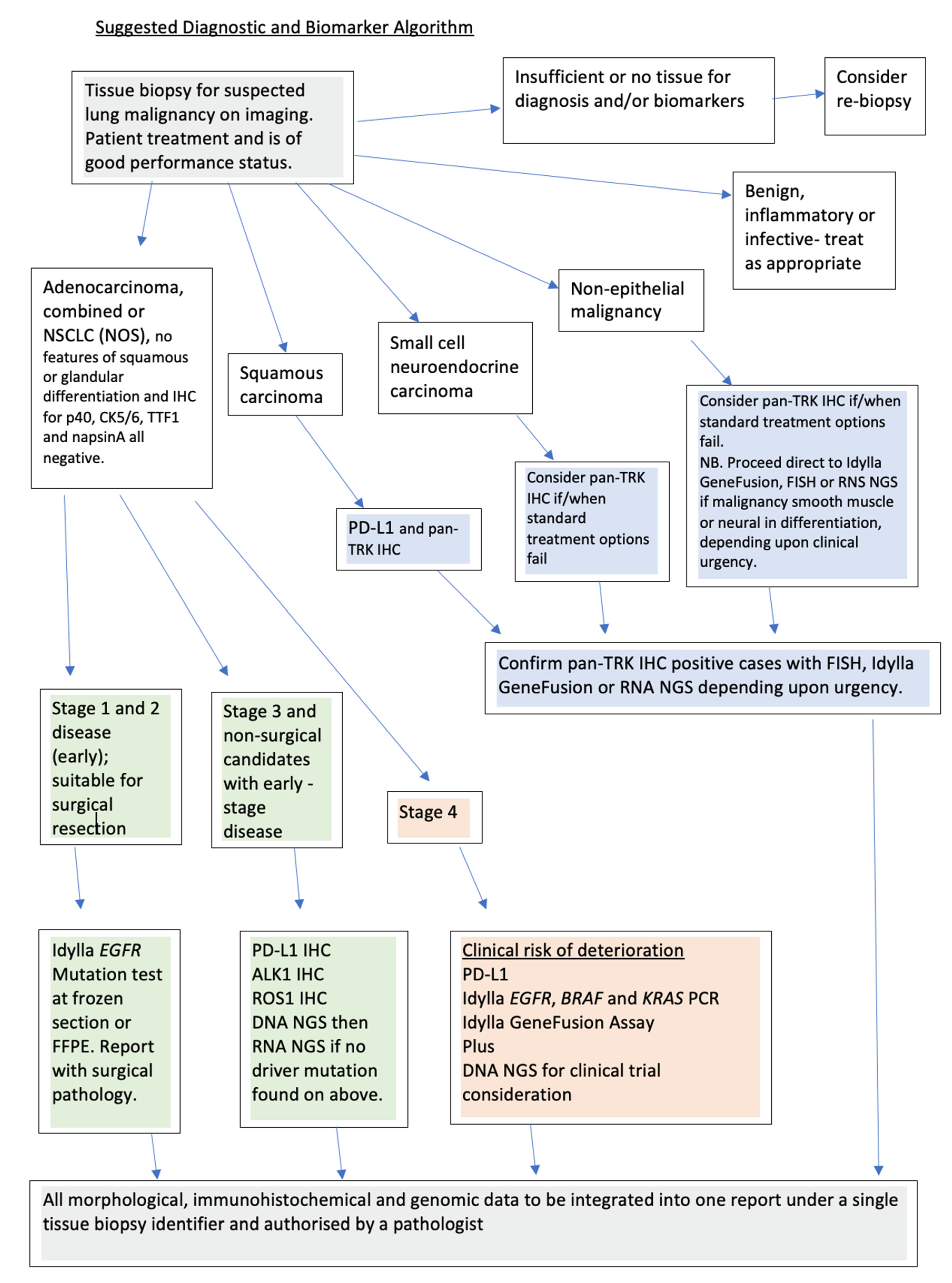
2.8. Suggestions for Improved Care Pathways Incorporating Molecular Biomarker Identification
3. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arnold, M.; Rutherford, M.J.; Bardot, A.; Ferlay, J.; Andersson, T.M.; Myklebust, T.; Tervonen, H.; Thursfield, V.; Ransom, D.; Shacl, L.; et al. Progress in cancer survival, mortality, and incidence in seven high-income countries 1995–2014 (ICBP SURVMARK-2): A population-based study. Lancet Oncol. 2019, 20, 1493–1505. [Google Scholar] [CrossRef]
- Malvezzi, M.; Bosetti, C.; Rosso, T.; Bertuccio, P.; Chatenoud, L.; Levi, F.; Romano, C.; Negri, E.; La Vecchia, C. Lung cancer mortality in European men: Trends and predictions. Lung Cancer 2013, 80, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, C.; Malvezzi, M.; Rosso, T.; Bertuccio, P.; Gallus, S.; Chatenoud, L.; Levi, F.; Romano, C.; Negri, E.; La Vecchia, C. Lung cancer mortality in European women: Trends and predictions. Lung Cancer 2012, 78, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Davidson, M.R.; Gazdar, A.F.; Clarke, B.E. The pivotal role of pathology in the management of lung cancer. J. Thorac. Dis. 2013, 5 (Suppl. 5), S463–S478. [Google Scholar] [PubMed]
- Giles, C. Having both patient advocates and patients at the MDT meeting might be useful. BMJ 2015, 351, h5285. [Google Scholar] [CrossRef] [PubMed]
- Garrido, P.; Conde, E.; de Castro, J.; Gómez-Román, J.J.; Felip, E.; Pijuan, L.; Isla, D.; Sanz, J.; Paz-Ares, L.; Lopez-Rios, F. Updated guidelines for predictive biomarker testing in advanced non-small-cell lung cancer: A National Consensus of the Spanish Society of Pathology and the Spanish Society of Medical Oncology. Clin. Transl. Oncol. 2020, 22, 989–1003. [Google Scholar] [CrossRef]
- Malapelle, U.; Pisapia, P.; Iaccarino, A.; Barberis, M.; Bellevicine, C.; Brunnström, H.; de Biase, H.; de Maglio, G.; Lindqvist, K.; Fassan, M.; et al. Predictive molecular pathology in the time of coronavirus disease (COVID-19) in Europe. J. Clin. Pathol. 2021, 74, 234–237. [Google Scholar] [CrossRef]
- Kerr, K.M.; Bibeau, F.; Thunnissen, E.; Botling, J.; Ryška, A.; Wolf, J. The evolving landscape of biomarker testing for non-small cell lung cancer in Europe. Lung Cancer 2021, 154, 161–175. [Google Scholar] [CrossRef]
- Lantuejoul, S.; Sound-Tsao, M.; Cooper, W.A.; Girard, N.; Hirsch, F.R.; Roden, A.C.; Lopez-Rios, F.; Jain, D.; Chou, T.J.; Motoi, N.; et al. PD-L1 Testing for Lung Cancer in 2019: Perspective From the IASLC Pathology Committee. J. Thorac. Oncol. 2020, 15, 499–519. [Google Scholar] [CrossRef]
- Lindeman, N.I.; Cagle, P.T.; Aisner, D.L.; Arcila, M.E.; Beasley, M.B.; Bernicker, E.H.; Colasacco, C.; Dacic, S.; Hirsch, F.R.; Kerr, K.; et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J. Mol. Diagn. 2018, 20, 129–159. [Google Scholar]
- López-Castro, R.; García-Peña, T.; Mielgo-Rubio, X.; Riudavets, M.; Teixidó, C.; Vilariño, N.; Vilariño, N.; Counago, T.; Mezquita, L. Targeting molecular alterations in non-small-cell lung cancer: What’s next? Per. Med. 2022, 19, 341–359. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, M.G.O.; Jacob, M.; Martins, N.; Moura, C.S.; Guimarães, S.; Reis, J.P.; Justino, A.; Pina, M.J.; Cirnes, L.; Sousa, C.; et al. Targeted Gene Next-Generation Sequencing Panel in Patients with Advanced Lung Adenocarcinoma: Paving the Way for Clinical Implementation. Cancers 2019, 11, 1229. [Google Scholar] [CrossRef] [PubMed]
- Beckett, P.; Navani, N.; Harden, S.; Tweedie, J.; Tebay, R.; Rodgers, H. National Lung Cancer Audit: Spotlight on Molecular Testing in Advanced Lung Cancer; Healthcare Quality Improvement Partnership (HQIP): London, UK, 2020. [Google Scholar]
- Mino-Kenudson, M.; Le Stang, N.; Daigneault, J.B.; Nicholson, A.G.; Cooper, W.A.; Roden, A.C.; Moreira, A.L.; Thunnissen, E.; Papotti, M.; Pelosi, G.; et al. IASLC Global Survey on PD-L1 Testing for Non-Small Cell Lung Cancer. J. Thorac. Oncol. 2021, 16, 686. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, G.; Andrini, E.; Sisi, M.; Rizzo, A.; Parisi, C.; Di Federico, A.; Gelsomino, F.; Ardizzoni, A. Beyond EGFR, ALK and ROS1: Current evidence and future perspectives on newly targetable oncogenic drivers in lung adenocarcinoma. Crit. Rev. Oncol. Hematol. 2020, 156, 103119. [Google Scholar] [CrossRef]
- De Luca, C.; Pepe, F.; Iaccarino, A.; Pisapia, P.; Righi, L.; Listì, A.; Greco, L.; Gragnano, G.; Campione, S.; Dominicis, G.; et al. RNA-Based Assay for Next-Generation Sequencing of Clinically Relevant Gene Fusions in Non-Small Cell Lung Cancer. Cancers 2021, 13, 139. [Google Scholar] [CrossRef]
- Zhao, R.; Han, Y.; Xiang, C.; Chen, S.; Zhao, J.; Guo, L.; Yu, A.; Shao, J.; Zhu, L.; Tian, Y.; et al. RNA sequencing effectively identifies gene fusions undetected by DNA sequencing in lung adenocarcinomas. J. Clin. Oncol. 2021, 39, 3052. [Google Scholar] [CrossRef]
- Deveson, I.W.; Brunck, M.E.; Blackburn, J.; Tseng, E.; Hon, T.; Clark, T.A.; Clark, M.B.; Crawford, J.; Dinger, M.E.; Nielsen, L.K.; et al. Universal Alternative Splicing of Noncoding Exons. Cell Syst. 2018, 6, 245–255.e5. [Google Scholar] [CrossRef]
- Kirchner, M.; Neumann, O.; Volckmar, A.L.; Stögbauer, F.; Allgäuer, M.; Kazdal, D.; Budczies, J.; Rempel, E.; Brandt, R.; Talla, S.B.; et al. RNA-Based Detection of Gene Fusions in Formalin-Fixed and Paraffin-Embedded Solid Cancer Samples. Cancers 2019, 11, 1309. [Google Scholar] [CrossRef]
- Matter, M.S.; Chijioke, O.; Savic, S.; Bubendorf, L. Narrative review of molecular pathways of kinase fusions and diagnostic approaches for their detection in non-small cell lung carcinomas. Transl. Lung Cancer Res. 2020, 9, 2645–2655. [Google Scholar] [CrossRef]
- Tsao, M.S.; Hirsch, F.R.; Yatabe, Y. IASLC Atlas of ALK and ROS1 Testing in Lung Cancer. IASLC. Available online: https://www.iaslc.org/Research-Education/Publications/IASLC-Atlases2016 (accessed on 27 October 2022).
- Zhao, R.; Yao, F.; Xiang, C.; Zhao, J.; Shang, Z.; Guo, L.; Ding, W.; Guo, L.; Ma, S.; Shao, J.; et al. Identification of NTRK gene fusions in lung adenocarcinomas in the Chinese population. J. Pathol. Clin. Res. 2021, 7, 375–384. [Google Scholar] [CrossRef]
- Doebele, R.C.; Drilon, A.; Paz-Ares, L.; Siena, S.; Shaw, A.T.; Farago, A.F.; Blakely, C.M.; Seto, T.; Cho, B.C.; Tosi, D.; et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: Integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020, 21, 271–282. [Google Scholar] [CrossRef]
- Jalal, S.I.; Guo, A.; Ahmed, S.; Kelley, M.J. Analysis of actionable genetic alterations in lung carcinoma from the VA National Precision Oncology Program. Semin Oncol. 2022, 49, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Sakai, H.; Morise, M.; Kato, T.; Matsumoto, S.; Sakamoto, T.; Kumagai, T.; Tokito, T.; Atagi, S.; Kozuki, S.; Tanaka, H.; et al. Tepotinib in patients with NSCLC harbouring MET exon 14 skipping: Japanese subset analysis from the Phase II VISION study. Jpn. J. Clin. Oncol. 2021, 51, 1261–1268. [Google Scholar] [CrossRef] [PubMed]
- Piton, N.; Lanic, M.D.; Marguet, F.; Lamy, A.; Blanchard, F.; Guisier, F.; Viennot, M.; Salaun, M.; Thiberville, L.; Jardin, F.; et al. An improved assay for detection of theranostic gene translocations and MET exon 14 skipping in thoracic oncology. Lab. Investig. 2021, 101, 648–660. [Google Scholar] [CrossRef] [PubMed]
- Drusbosky, L.M.; Rodriguez, E.; Dawar, R.; Ikpeazu, C.V. Therapeutic strategies in RET gene rearranged non-small cell lung cancer. J. Hematol. Oncol. 2021, 14, 50. [Google Scholar] [CrossRef] [PubMed]
- Mok, T.; Carbonne, D.; Hirsch, F. IASLC Atlas of EGFR Testing in Lung Cancer; International Association of the Study of Lung Cancer (IASLC): Denver, CO, USA, 2017. [Google Scholar]
- Yatabe, Y.; Dacic, S.; Borczuk, A.C.; Warth, A.; Russell, P.A.; Lantuejoul, S.; Beasley, M.B.; Thunnissen, E.; Pelosi, G.; Rekhtman, N.; et al. Best Practices Recommendations for Diagnostic Immunohistochemistry in Lung Cancer. J. Thorac. Oncol. 2019, 14, 377–407. [Google Scholar] [CrossRef]
- Ilie, M.; Hofman, P. Pitfalls in lung cancer molecular pathology: How to limit them in routine practice? Curr. Med. Chem. 2012, 19, 2638–2651. [Google Scholar] [CrossRef]
- Navani, N.; Brown, J.M.; Nankivell, M.; Woolhouse, I.; Harrison, R.N.; Jeebun, V.; Munavvar, M.; Ng, B.J.; Rassl, D.M.; Falzon, M.; et al. Suitability of endobronchial ultrasound-guided transbronchial needle aspiration specimens for subtyping and genotyping of non-small cell lung cancer: A multicenter study of 774 patients. Am. J. Respir Crit. Care Med. 2012, 185, 1316–1322. [Google Scholar] [CrossRef]
- Medford, A.R.; Agrawal, S.; Free, C.M.; Bennett, J.A. A performance and theoretical cost analysis of endobronchial ultrasound-guided transbronchial needle aspiration in a UK tertiary respiratory centre. QJM 2009, 102, 859–864. [Google Scholar] [CrossRef]
- Moore, D.A.; Benafif, S.; Poskitt, B.; Argue, S.; Lee, S.; Ahmad, T.; Papadatos-Pastos, D.; Jamal-Hanjani, M.; Bennett, P.; Forster, M.D. Optimising fusion detection through sequential DNA and RNA molecular profiling of non-small cell lung cancer. Lung Cancer 2021, 161, 55–59. [Google Scholar] [CrossRef]
- Faber, E.; Grosu, H.; Sabir, S.; San Lucas, F.A.; Barkoh, B.A.; Bassett, R.L.; Lthra, R.; Stwart, J.; Roy-Chowdhuri, S. Adequacy of small biopsy and cytology specimens for comprehensive genomic profiling of patients with non-small cell lung cancer to determine eligibility for immune checkpoint inhibitor and targeted therapy. J. Clin. Pathol. 2022, 75, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Talarchek, J.N.; Huang, M.; Gong, Y.; Du, F.; Ehya, H.; Flieder, D.B.; Patchefsky, A.S.; Wasik, M.A.; Pei, J. Cell block-based RNA next generation sequencing for detection of gene fusions in lung adenocarcinoma: An institutional experience. Cytopathology 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shi, S.R.; Liu, C.; Taylor, C.R. Standardization of immunohistochemistry for formalin-fixed, paraffin-embedded tissue sections based on the antigen-retrieval technique: From experiments to hypothesis. J. Histochem Cytochem. 2007, 55, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Thavarajah, R.; Mudimbaimannar, V.K.; Elizabeth, J.; Rao, U.K.; Ranganathan, K. Chemical and physical basics of routine formaldehyde fixation. J. Oral. Maxillofac. Pathol. 2012, 16, 400–405. [Google Scholar] [CrossRef]
- Ding, J.; Ichikawa, Y.; Ishikawa, T.; Shimada, H. Effect of formalin on extraction of mRNA from a formalin-fixed sample: A basic investigation. Scand. J. Clin. Lab. Investig. 2004, 64, 229–235. [Google Scholar] [CrossRef]
- Mullegama, S.V.; Alberti, M.O.; Au, C.; Li, Y.; Toy, T.; Tomasian, V.; Xian, R.R. Nucleic Acid Extraction from Human Biological Samples. Methods Mol. Biol. 2019, 1897, 359–383. [Google Scholar]
- Hedegaard, J.; Thorsen, K.; Lund, M.K.; Hein, A.M.; Hamilton-Dutoit, S.J.; Vang, S.; Nordentoft, I.; Birkenkamp-Demtroder, K.; Kruhoffer, M.; Hager, H.; et al. Next-generation sequencing of RNA and DNA isolated from paired fresh-frozen and formalin-fixed paraffin-embedded samples of human cancer and normal tissue. PLoS ONE 2014, 9, e98187. [Google Scholar] [CrossRef]
- Norton, N.; Sun, Z.; Asmann, Y.W.; Serie, D.J.; Necela, B.M.; Bhagwate, A.; Jen, J.; Eckloff, B.W.; Kalari, K.R.; Thompson, K.J.; et al. Gene expression, single nucleotide variant and fusion transcript discovery in archival material from breast tumors. PLoS ONE 2013, 8, e81925. [Google Scholar] [CrossRef]
- Kap, M.; Smedts, F.; Oosterhuis, W.; Winther, R.; Christensen, N.; Reischauer, B.; Viertler, C.; Groelz, D.; Becker, K.F.; Zatloual, K.; et al. Histological assessment of PAXgene tissue fixation and stabilization reagents. PLoS ONE 2011, 6, e27704. [Google Scholar] [CrossRef]
- Mathieson, W.; Marcon, N.; Antunes, L.; Ashford, D.A.; Betsou, F.; Frasquilho, S.G.; Kofanova, O.A.; McKay, S.C.; Pericleous, S.; Smith, C.; et al. A Critical Evaluation of the PAXgene Tissue Fixation System: Morphology, Immunohistochemistry, Molecular Biology, and Proteomics. Am. J. Clin. Pathol. 2016, 146, 25–40. [Google Scholar] [CrossRef]
- Sanchez, I.; Betsou, F.; Culot, B.; Frasquilho, S.; McKay, S.C.; Pericleous, S.; Smith, C.; Thomas, G.; Mathieson, W. RNA and microRNA Stability in PAXgene-Fixed Paraffin-Embedded Tissue Blocks After Seven Years’ Storage. Am. J. Clin. Pathol. 2018, 149, 536–547. [Google Scholar] [CrossRef] [PubMed]
- Frasquilho, S.G.; Sanchez, I.; Yoo, C.; Antunes, L.; Bellora, C.; Mathieson, W. Do Tissues Fixed in a Non-crosslinking Fixative Require a Dedicated Formalin-free Processor? J. Histochem Cytochem. 2021, 69, 389–405. [Google Scholar] [CrossRef]
- Finall, A.; Davies, G.; Jones, T.; Emlyn, G.; Huey, P.; Mullard, A. Integration of rapid PCR testing as an adjunct to NGS in diagnostic pathology services within the UK: Evidence from a case series of non-squamous, non-small cell lung cancer (NSCLC) patients with follow-up. J. Clin. Pathol. 2022, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rybarczyk-Kasiuchnicz, A.; Ramlau, R.; Stencel, K. Treatment of Brain Metastases of Non-Small Cell Lung Carcinoma. Int. J. Mol. Sci. 2021, 22, 593. [Google Scholar] [CrossRef] [PubMed]
- Hardtstock, F.; Myers, D.; Li, T.; Cizova, D.; Maywald, U.; Wilke, T.; Griesinger, F. Real-world treatment and survival of patients with advanced non-small cell lung Cancer: A German retrospective data analysis. BMC Cancer 2020, 20, 260. [Google Scholar] [CrossRef]
- Smith, R.E.; Johnson, M.; Gordan, L.N.; Xue, M.; Varughese, P.; Dorrow, N.; Wang, B.; Vaidya, V.; Gart, M.; Gierman, H.J.; et al. Evaluation of outcomes in patients with stage 4 non-small cell lung cancer (NSCLC 4) harbouring actionable oncogenic drivers when treated prior to report of mutation without tyrosine kinase inhibitors: An Integra Connect Database retrospective observational study. J. Clin. Oncol. 2022, 40, 1530. [Google Scholar]
- Finall, A.; Jones, K. Applying bioethical principles for directing investment in precision medicine. Clin. Ethics 2020, 15, 23–28. [Google Scholar] [CrossRef]
- Melosky, B.; Wheatley-Price, P.; Juergens, R.A.; Sacher, A.; Leighl, N.B.; Tsao, M.S.; Cheema, P.; Snow, S.; Liu, G.; Card, P.; et al. The rapidly evolving landscape of novel targeted therapies in advanced non-small cell lung cancer. Lung Cancer 2021, 160, 136–151. [Google Scholar] [CrossRef]
- Ståhl, P.L.; Salmén, F.; Vickovic, S.; Lundmark, A.; Navarro, J.F.; Magnusson, J.; Giacomello, S.; Asp, M.; Westholm, J.O.; Huss, M.; et al. Visualization and analysis of gene expression in tissue sections by spatial transcriptomics. Science 2016, 353, 78–82. [Google Scholar] [CrossRef]
- Sorber, L.; Van Dorst, B.; Bellon, E.; Zwaenepoel, K.; Lambin, S.; De Winne, K.; Lardon, F.; Pauwels, P.; Siozopoulou, V. NTRK Gene Fusion Detection in a Pan-Cancer Setting Using the Idylla GeneFusion Assay. J. Mol. Diagn. 2022, 24, 750–759. [Google Scholar] [CrossRef]
- Depoilly, T.; Garinet, S.; van Kempen, L.C.; Schuuring, E.; Clavé, S.; Bellosillo, B.; Ercolani, C.; Buglioni, S.; Siemanowski, J.; Merkelbach-Bruse, S.; et al. Multicenter Evaluation of the Idylla GeneFusion in Non-Small-Cell Lung Cancer. J. Mol. Diagn. 2022, 24, 1021–1030. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.H.; Barbee, J.; Yang, S.R.; Chang, J.C.; Liang, P.; Mullaney, K.; Chan, R.; Salazar, P.; Benayed, R.; Offin, M.; et al. Clinical Utility and Performance of an Ultrarapid Multiplex RNA-Based Assay for Detection of ALK, ROS1, RET, and NTRK1/2/3 Rearrangements and MET Exon 14 Skipping Alterations. J. Mol. Diagn. 2022, 24, 642–654. [Google Scholar] [CrossRef] [PubMed]
- NICE. Entrectinib for Treating NTRK Fusion-Positive Solid Tumours. Available online: https://www.nice.org.uk/guidance/ta6442021 (accessed on 27 October 2022).
- NICE. Larotrectinib for Treating NTRK Fusion-Positive Solid Tumours. Available online: https://www.nice.org.uk/guidance/ta6302021 (accessed on 27 October 2022).
- Strohmeier, S.; Brcic, I.; Popper, H.; Liegl-Atzwanger, B.; Lindenmann, J.; Brcic, L. Applicability of pan-TRK immunohistochemistry for identification of NTRK fusions in lung carcinoma. Sci. Rep. 2021, 11, 9785. [Google Scholar] [CrossRef] [PubMed]
- Elfving, H.; Broström, E.; Moens, L.N.J.; Almlöf, J.; Cerjan, D.; Lauter, G.; Nord, H.; Mattsson, J.S.M.; Ullenhag, G.J.; Strell, C.; et al. Evaluation of NTRK immunohistochemistry as a screening method for NTRK gene fusion detection in non-small cell lung cancer. Lung Cancer 2021, 151, 53–59. [Google Scholar] [CrossRef]
- Yang, S.C.; Yeh, Y.C.; Chen, Y.L.; Chiu, C.H. Economic Analysis of Exclusionary EGFR Test Versus Up-Front NGS for Lung Adenocarcinoma in High EGFR Mutation Prevalence Areas. J. Natl. Compr. Canc. Netw. 2022, 20, 774–782.e4. [Google Scholar] [CrossRef]
- Houseley, J.; Tollervey, D. The many pathways of RNA degradation. Cell 2009, 136, 763–776. [Google Scholar] [CrossRef]
- Elliott, D.; Ladomery, M. Molecular Biology of RNA; Oxford University Press: Oxford, UK, 2011. [Google Scholar]
- Sheffield, B.S.; Beharry, A.; Diep, J.; Perdrizet, K.; Iafolla, M.A.J.; Raskin, W.; Dudani, S.; Brett, M.A.; Starova, B.; Olsen, B.; et al. Point of Care Molecular Testing: Community-Based Rapid Next-Generation Sequencing to Support Cancer Care. Curr. Oncol. 2022, 29, 30113. [Google Scholar] [CrossRef]
- Uguen, A.; Troncone, G. A review on the Idylla platform: Towards the assessment of actionable genomic alterations in one day. J. Clin. Pathol. 2018, 71, 757–762. [Google Scholar] [CrossRef]
- Adizie, J.B.; Tweedier, J.; Khakwani, A.; Peach, E.; Hubbard, R.; Wood, N.; Gosney, J.R.; Harden, S.V.; Beckett, P.; Popat, S.; et al. Biomarker Testing for People with Advanced Lung Cancer in England. J. Thorac. Oncol. Clin. Res. Rep. 2021, 2, 100176. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Finall, A. RNA-Based Next-Generation Sequencing in the Somatic Molecular Testing of Non-Small-Cell Lung Cancer (NSCLC) in a Centralized Model: Real-World Data to Suggest It Is Time to Reconsider Testing Options. J. Mol. Pathol. 2022, 3, 307-318. https://doi.org/10.3390/jmp3040026
Finall A. RNA-Based Next-Generation Sequencing in the Somatic Molecular Testing of Non-Small-Cell Lung Cancer (NSCLC) in a Centralized Model: Real-World Data to Suggest It Is Time to Reconsider Testing Options. Journal of Molecular Pathology. 2022; 3(4):307-318. https://doi.org/10.3390/jmp3040026
Chicago/Turabian StyleFinall, Alison. 2022. "RNA-Based Next-Generation Sequencing in the Somatic Molecular Testing of Non-Small-Cell Lung Cancer (NSCLC) in a Centralized Model: Real-World Data to Suggest It Is Time to Reconsider Testing Options" Journal of Molecular Pathology 3, no. 4: 307-318. https://doi.org/10.3390/jmp3040026
APA StyleFinall, A. (2022). RNA-Based Next-Generation Sequencing in the Somatic Molecular Testing of Non-Small-Cell Lung Cancer (NSCLC) in a Centralized Model: Real-World Data to Suggest It Is Time to Reconsider Testing Options. Journal of Molecular Pathology, 3(4), 307-318. https://doi.org/10.3390/jmp3040026




