1. Introduction
A recent study carried out by the National Center for Health Statistics (NCHS) has uncovered a concerning statistic regarding obesity rates in the United States. The study’s findings indicate that, between the years 1999–2000 and 2017–2018, the prevalence of obesity has risen from 30.5% to 42.5%, with severe obesity rates increasing from 4.7% to 9.2%. Obesity is not only a disease in itself but it is associated with other significant health risks such as coronary heart disease and end-stage renal disease. If this trend continues at the same pace, it is projected that nearly 50% of the US population will be affected by obesity by 2030, and severe obesity will impact almost 12% of the population [
1].
Bariatric surgery is an elective procedure that is used to address severe obesity and help control the rising obesity epidemic and its associated health burdens in the US. The aftermath of these surgeries often includes an ER visit within a 30-day timeframe due to several complications. These complications are associated with various factors that can be mainly divided into three categories: preoperative, intraoperative, and postoperative. For example, the age and gender of a patient are preoperative factors that are known before the surgery; however, infection in the area of surgery is a postoperative factor that can only happen after the surgery has taken place. Similarly, a change in the type of surgery that is being performed on a patient during the surgery is an example of an intraoperative factor that is something that occurred during the time of the surgery.
With the rise in the application of artificial intelligence and predictive analytics in almost every field, this study was motivated by the hope of understanding the preemptive factors (i.e., preoperative factors in the context of bariatric surgery) and the study of these factors in hopes that they could be used to model a proactive approach (such as predictive modeling) to prevent preventable 30-day postoperative ER visits. The planning and coordination of care can occur before surgery takes place, because, unlike intraoperative and postoperative factors, preoperative factors can be known before surgery. Approximately 13% to 27% of ER visits in the United States are avoidable and have the potential to be handled in physician offices, clinics, and urgent care centers, leading to potential annual savings of USD 4.4 billion [
2]. These preventable ER visits can also turn into preventable readmissions, which comprise another area of concern in healthcare. Preventable readmissions are a large and growing concern throughout healthcare in the United States, representing as many as 20% of all hospitalizations (30-day post-discharge) and an estimated USD 17–USD 26 billion in unnecessary costs annually [
3].
2. Methodology
This systematic review, which was an integral component of a doctoral dissertation, was conducted to gather and summarize the relevant findings pertaining to preoperative and postoperative factors that significantly influenced the likelihood of patients returning to the ER within 30 days after undergoing bariatric surgery [
4]. A systematic literature review is a commonly employed method used by researchers to address specific research objectives. It involves various strategies of narrowing down the selection of articles, such as applying specific methodologies and inclusion and exclusion criteria [
5,
6,
7].
The systematic review in this research study aimed to achieve three primary objectives:
- ○
Explore, consolidate, and analyze the existing research conducted in the field of bariatric surgery regarding 30-day postoperative visits to the ER.
- ○
Identify and compile a selection of preoperative factors that previous studies have identified as potential and significant predictors of 30-day postoperative ER visits.
- ○
Highlight the gaps and limitations present in the current body of knowledge pertaining to this specific topic and propose recommendations.
The statement of the research question led by these three key objectives was narrowed down to the following: “What are the preoperative and postoperative factors associated with 30-day postoperative emergency room visits for bariatric patients in the US?” This systematic literature review made use of two prominent databases, namely SCOPUS and PubMed, to gather relevant articles. The same criteria were applied to both databases to identify articles of interest. The flowchart of this systematic review is outlined in
Figure 1.
Initially, a search was conducted using the keywords “bariatric” and “emergency” in the title or abstract, resulting in a total of 107 articles. To narrow down the selection, the exclusion criterion was set to exclude articles that were not journal articles, reducing the count to 93. Another criterion was applied based on the publication timeline, excluding articles published before 2010 and up until the year 2021 (as of 1 April 2021). The rationale behind this criterion was that data prior to 2010 might be outdated due to the rapid advancements and transformations in bariatric surgery and data recording methods. This further reduced the list to 73 articles.
An additional criterion was then applied to exclude articles published in languages other than English, resulting in a final count of 66 articles. These 66 articles were individually reviewed to assess the relevance of their journal abstracts and titles to the research being conducted, leading to a further reduction to 22 relevant articles. The content of these remaining 22 articles was thoroughly examined, and pertinent information, including the article title, authors, journal, objectives or focus of the publication, and factors significantly contributing to postoperative ER visits at different time intervals (30, 90, 120, 365, and 730+ days), as well as factors that can be assessed before the surgery, were documented.
Since this study was just a systematic review of the literature, Institutional Review Board (IRB) approval was not required as it did not involve any human subjects throughout the study. It is important to note that this study only covers the articles narrowed down based on the scope of the study, databases, and search criteria utilized for the purpose of this study.
3. Results
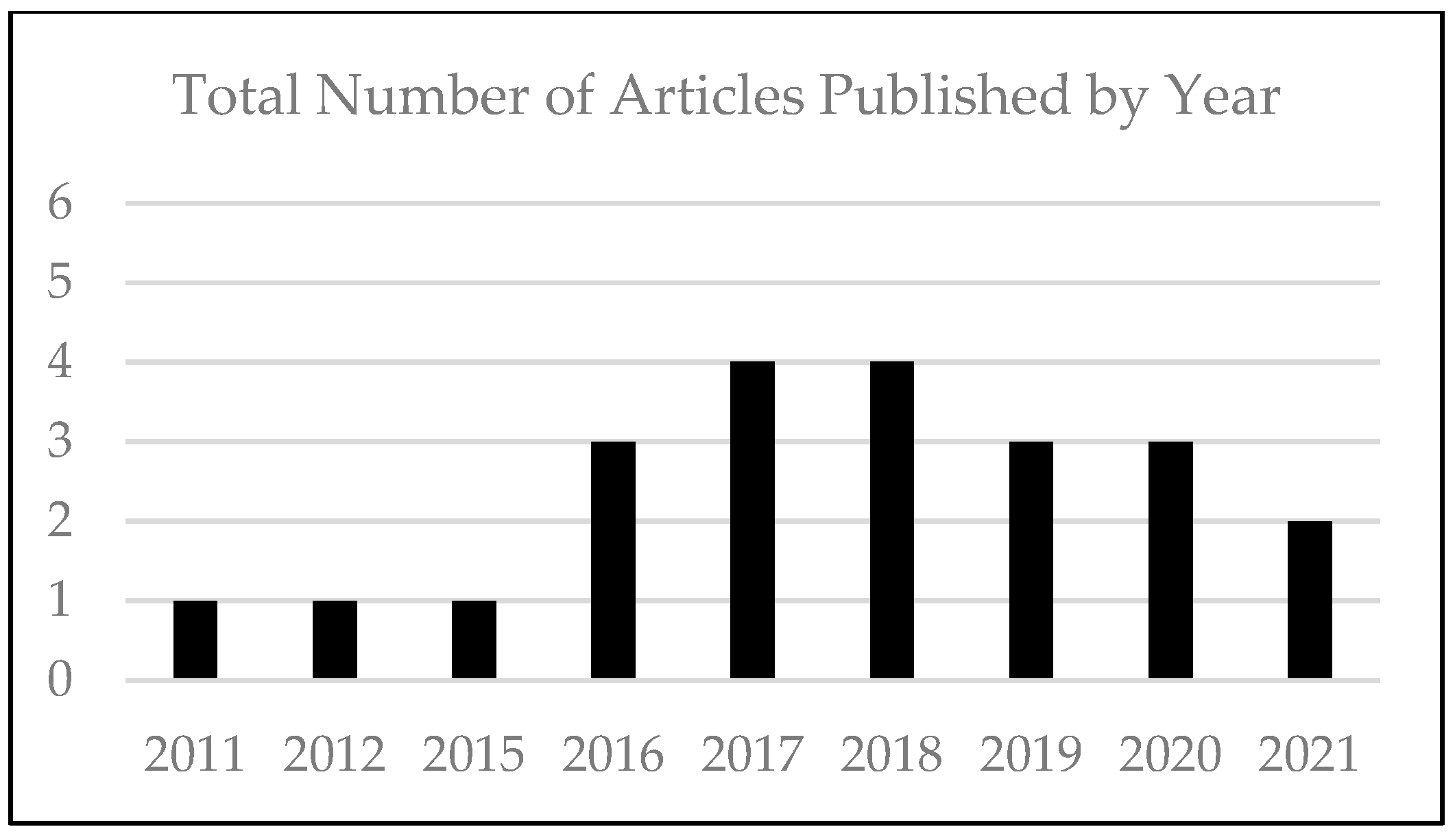
Of the 22 selected articles published, the majority of the articles were published between 2016 and 2020 (
Figure 2). The number of preoperative, intraoperative, and postoperative factors found to significantly impact the probability of patients returning to the ER within 30 days following bariatric surgery varied across studies. The range of significant factors identified in each study ranged between one and eight. The majority of the studies (above 90%) examined had fewer than eight significant factors influencing postoperative ER visits within the 30-day timeframe.
Similar to the approach taken by Gholami, Abu, Abdul-Nour, and Badar [
7], a basic Pareto analysis was conducted to ascertain the primary journals responsible for publishing articles within the scope of the study, which consisted of 22 selected articles. The outcome of this analysis revealed that
Surg Obes Related Dis Journal contributed 5 out of the 22 articles (22.7%). Additionally,
Annals of Surgery and
Emerg Med Australas journals each published two articles, accounting for 9.1% of the total. The remaining journals in the dataset each had a single article publication. These journals include
Adv Emerg Nurs J.,
Cirugía Española,
Emerg Med Pract.,
Journal of the American College of Cardiology,
Minerva Surg.,
Obes Res Clin Pract.,
Obesity Surgery,
ObesityFacts,
Pediatr Emerg Care,
Rev Esp Enferm Dig.,
Surg Endosc.,
Surgery, and
The American Journal of Cardiology.
After extracting the relevant information from the summary (shown in
Table A1 (
Appendix A)) of the literature search, the preoperative and postoperative factors that significantly influenced the likelihood of 30-day postoperative visits to the ER were identified and counted. Similar factors were only counted once.
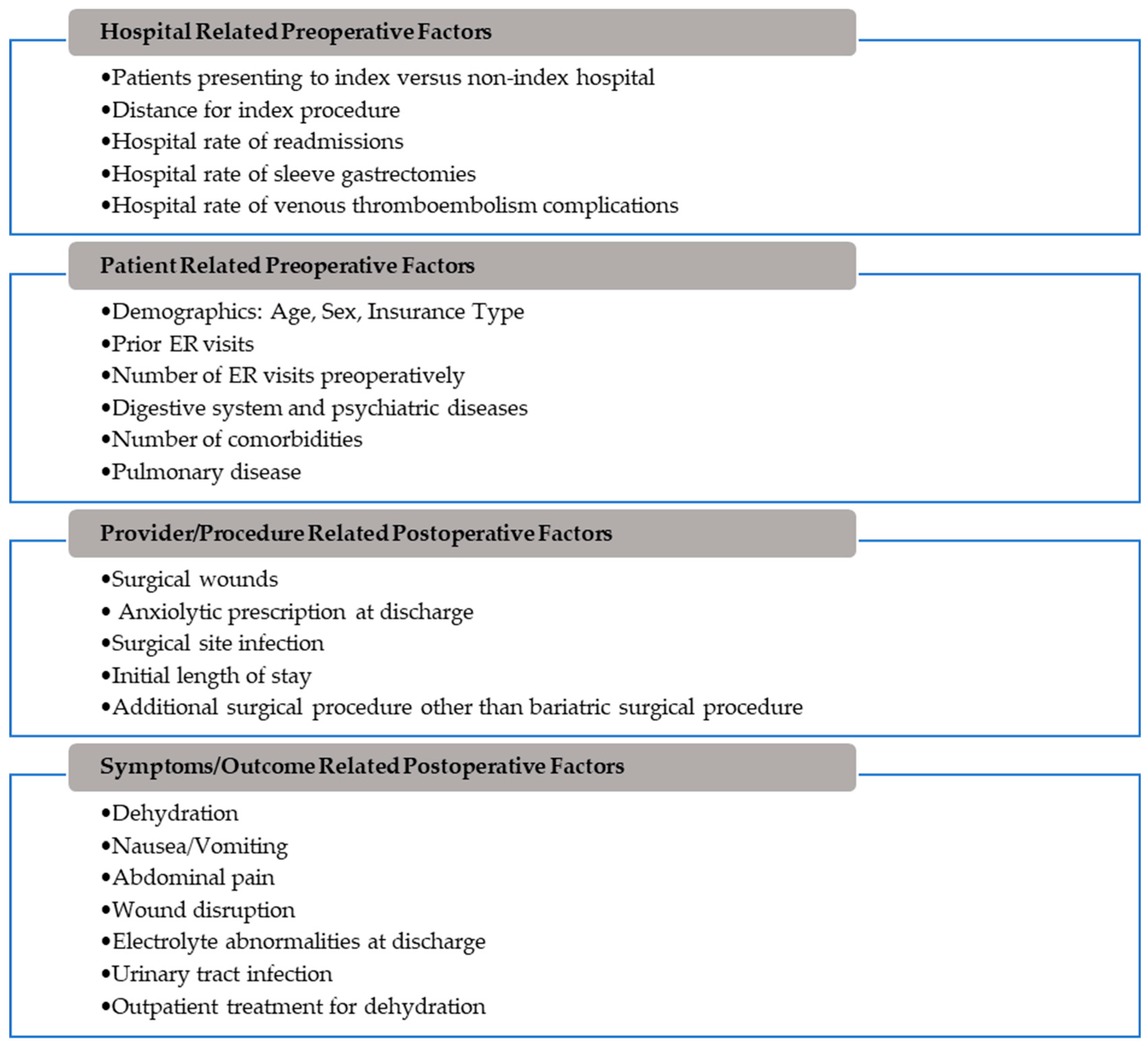
Figure 3 visually displays the breakdown of these factors, categorized into preoperative and postoperative factors, based on the previously published articles outlined in
Table A1 that were further classified into four subcategories: hospital-related preoperative factors, patient-related preoperative factors, provider/procedure-related postoperative factors, and symptoms/outcome-related postoperative factors.
To prevent undesirable events from occurring, it is important to understand the factors that contribute to their occurrence in advance, enabling the implementation of appropriate preventive measures. In the case of 30-day postoperative ER visits, which are undesirable for both patients and healthcare systems, proactive action plans can be developed to mitigate the likelihood of these visits. This may involve scheduling early clinical interventions based on the identified risk factors for patients who have a higher chance of returning to the ER within 30 days after bariatric surgery. By implementing preventive measures, high-risk patients can potentially avoid an avoidable ER visit altogether. Minimizing or reducing such undesirable events can be considered a “defective” outcome, particularly if they are preventable and unnecessary. Controlling and preventing these defects can be termed “quality control”, drawing inspiration from concepts and theories used in product development and improvement within the industrial engineering sector.
Quality control strategies can be broadly categorized into two main approaches: reactive and proactive. This study advocates for a proactive approach that institutionalizes processes and systems to control and maintain the desired quality. One research study outlines the Juran Trilogy, which encompasses quality planning, quality control, and quality improvement, as the underlying concept of quality management. Within the quality control process, reactive measures such as corrective actions play a critical role in managing and controlling quality in the long run [
8]. However, it is crucial that these actions are continuous and sustainable. This is where the concept of quality improvement, the third aspect of the Juran Trilogy, becomes essential in the realm of quality management.
Short, Badar, Kluse, and Schafer highlight an important point that reactive or corrective actions in quality improvement projects are often more readily accepted and rewarded due to their financial implications [
9]. However, a proactive approach can also yield positive economic and safety outcomes for patients, their families, and the healthcare teams involved in their care. It is essential to recognize the value of a proactive approach and its potential to improve patient outcomes and overall quality of care.
As additional support to this systematic literature review, a search was conducted on the ProQuest database, which is recognized as the largest collection of dissertations and theses worldwide, consisting of around 90,000 authoritative sources and approximately 6 billion digital pages and articles. Based on this database, as of 1 April 2021, there have been only two dissertations and theses published that were related to the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). The first dissertation, published in 2014, explored the lived experience of couples following bariatric surgery through a qualitative description. The second dissertation, published in 2018, focused on examining factors that predict the maintenance of excess weight loss two or more years after bariatric surgery [
10]. None of these publications focused on preoperative factors associated with 30-day postoperative ER visits.
4. Discussion
The findings from this systematic literature review provide valuable insights into a wide range of factors influencing the preoperative and postoperative phases of bariatric surgery. It was also evident that the research in this space was very limited and only a handful of articles were published. This discussion section will further delve into the key preoperative and postoperative factors identified within the four categories: hospital-related preoperative factors, patient-related preoperative factors, provider/procedure-related postoperative factors, and symptoms/outcome-related postoperative factors.
In terms of hospital-related preoperative factors, the study highlighted the significance of the hospital where the procedure is performed. Patients presenting to index hospitals demonstrated distinct patterns compared to those attending non-index hospitals. The distance for the index procedure also emerged as a notable factor, influencing patient accessibility, and potentially affecting preoperative preparation. Hospital-specific rates of readmissions, sleeve gastrectomies, and venous thromboembolism complications were found to be relevant indicators of hospital performance in the context of bariatric surgery.
Patient-related preoperative factors play a crucial role in predicting outcomes. Demographic variables such as age, sex, and insurance type were associated with diverse patterns of preoperative care and postoperative outcomes. The number of prior ER visits, as well as the total number of ER visits preoperatively, emerged as strong predictors of complications, reflecting the overall health status of patients. The presence of digestive system and psychiatric diseases, along with the number of comorbidities and the presence of pulmonary disease, underscored the complex health profiles of bariatric surgery candidates. A recent study also showed similar results where non-Hispanic Black patients were at higher risk of serious complications within 30 days of the bariatric surgical procedure [
11]. Another recent study in the US through the Michigan Bariatric Surgery Collaborative brought forward the astonishing fact that nearly one-third of the patients undergoing bariatric surgery have some level of depression which was also associated with a higher rate of prescription opiates, alcohol, and smoking [
12].
Provider/procedure-related postoperative factors encompassed various aspects of surgical care. The occurrence of surgical wounds and surgical site infections, along with anxiolytic prescription at discharge, highlighted the importance of postoperative care protocols. The initial length of stay and the occurrence of additional surgical procedures beyond the bariatric surgery itself demonstrated the multidimensional nature of postoperative management and its potential impact on patient outcomes.
Finally, symptoms/outcome-related postoperative factors addressed specific postoperative complications and their management. Issues such as dehydration, nausea/vomiting, abdominal pain, wound disruption, and electrolyte abnormalities at discharge were identified as potential concerns. Additionally, urinary tract infections and outpatient treatment for dehydration emerged as important aspects of postoperative care, warranting attention in the management of patients following bariatric surgery. A recent study conducted by a publicly funded Canadian center also found similar results where postoperative factors such as infection, pain, nausea, or vomiting were some of the leading causes of 30-day readmissions [
13]. Another recent study conducted by researchers in Saudi Arabia, which is claimed to be the first study of its kind in the region, suggests that the level of patients’ knowledge regarding surgical site infection (SSI) was fair, which would mean gaps in knowledge regarding specific signs, symptoms, and preventive measures [
14].
Approximately 13% to 27% of ER visits in the United States are avoidable and have the potential to be handled in physician offices, clinics, and urgent care centers, leading to potential annual savings of USD 4.4 billion [
15]. These preventable ER visits can also turn into preventable readmissions, which is also another area of concern in healthcare. Preventable readmissions are a large and growing concern throughout healthcare in the United States, representing as many as 20% of all hospitalizations (30-day post-discharge) and an estimated USD 17–USD 26 billion in unnecessary costs annually [
16]. A crowded ER does not only mean depriving critical patients of receiving timely care at the ER but also means busier emergency medical services (EMS) which could mean delayed care for critical patients which can sometimes result in even the death of the patient [
17]. Because all the processes and systems are very much interconnected between ER, hospital, and operating rooms (ORs) in the context of healthcare systems, chaos in one setting such as ER can also have a negative impact on how patients receive care in the inpatient setting (hospital) and OR [
18]. Approximately 40 to 60 million patients in the US go through major surgeries which makes patients going through bariatric surgery just a fraction of the overall surgeries [
19]. However, knowing the positive upward trending and exponential growth of both obesity and bariatric surgeries performed each year as discussed earlier, it is not too late to prepare for the dooming future that is just a few years away from the present time. Especially during this time when artificial intelligence is on the rise and healthcare systems are on the cusp of transforming their processes and systems toward more automation and predictive approach to healthcare, studies like this can help organizations to plan and prepare for their ongoing work [
20].
5. Conclusions and Recommendations
In summary, this systematic literature review highlights the multifaceted nature of bariatric surgery outcomes, influenced by various hospital-, patient-, provider-, and symptom-related factors. This comprehensive understanding provides a foundation for developing targeted interventions and optimizing the entire spectrum of bariatric surgery care, ultimately leading to improved patient outcomes and more efficient healthcare resource utilization. Further research and collaboration among healthcare stakeholders are essential to harness the potential benefits of these findings that mainly focus on preoperative factors that can be used to help predict the likelihood of patients presenting to the ER within 30 days of discharge after a bariatric surgery procedure. This study sought to integrate preoperative factors, suggesting a need for further exploration into how they intersect with intraoperative and postoperative factors to enhance understanding of patient care continuity, suggesting avenues for future research.
6. Limitations of Study
The articles that were reviewed and summarized were extracted on 1 April 2021, and the articles are limited to these two databases: SCOPUS and PubMed. The articles that were part of this study were primarily published in the US. Due to the types of studies found and the limitation on the available data, meta-analysis was not conducted in this study. Although this study covered an important topic in healthcare, it was limited to a narrower topic, i.e., 30-day postoperative ER visit for bariatric patients, and the window of the years the articles were chosen was between 2010 and 1 April 2021.
7. Conflict of Interest and Financial Disclosure
The authors declare that there are no conflicts of interest and financial disclosures to make regarding this article.
Author Contributions
Conceptualization, M.A.B.; methodology, P.B., M.A.B. and C.K.; software, P.B.; validation, S.R.; formal analysis, P.B. and M.A.B.; investigation, P.B.; resources, P.B.; data curation, P.B.; writing—original draft preparation, P.B., M.A.B., C.K. and S.R.; writing—review and editing, C.K. and S.R.; visualization, P.B. and M.A.B.; supervision, M.A.B.; project administration, P.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were generated or analyzed in this study; all data used are cited in the referenced literature and are publicly available from their original sources.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Table A1.
Summary of selected articles from the literature review (only the first two pages of the summary table are shown here due to page length limitations of this article).
Table A1.
Summary of selected articles from the literature review (only the first two pages of the summary table are shown here due to page length limitations of this article).
| Article Title | Authors | Journal | Objective or Focus of the Article | Factors Significantly Contributing to (30-dayx30, 90-dayx90, 120-dayx120 1-yearx365, 2-yearx730+, or Unknown-daysxu) Postoperative ED Visit | Factors That Are Available or Can Be Known Prior to the Surgery |
|---|
| Emergency Department Care of the PostMetabolic and Bariatric Surgery Patient | [21] | Pediatr Emerg Care | Review of complications associated with bariatric surgery patients and appropriate management of care when patient show up in ED after the surgery | None | None |
| Emergency department management of patients with complications of bariatric surgery | [22] | Emerg Med Pract. | Overview of potential complications of bariatric procedures and recommendations regarding patient management and disposition in ED | None | None |
Characterizing the preventable emergency department visit after bariatric surgery
| [23] | Surg Obes Relat Dis. | Characterization of patients who present to the ED but could have been treated in an alternative setting | Factorsx30
- -
Anxiolytic prescription at discharge - -
Electrolyte abnormalities at discharge - -
Leukocytosis at discharge - -
Number of ED visits preoperatively
| - -
Anxiolytic prescription at discharge - -
Number of ED visits preoperatively
|
| Hospitalizations and emergency department visits in heart failure patients after bariatric surgery | [24] | Surg Obes Relat Dis. | To assess the impact of bariatric surgery on hospital-based healthcare utilization for patients with heart failure | None | Not applicable |
| Rates and reasons for emergency department presentations of patients wait-listed for public bariatric surgery in Tasmania, Australia | [25] | Obes Res Clin Pract. | To describe and evaluate public ED presentation rates and reasons for presenting in a cohort of patients wait-listed for public surgery in Tasmania, Australia | Factorsx30
- -
Digestive system and psychiatric diseases
| - -
Digestive system and psychiatric diseases
|
| Predictors of postoperative emergency department visits after laparoscopic bariatric surgery | [26] | Surg Obes Relat Dis. | To identify predictors of ED visits in patients without readmission after laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (LRYGB) | Factorsx30
- -
Outpatient treatment for dehydration - -
Urinary tract infection - -
Wound disruption - -
Surgical site infection
| None |
| Unplanned emergency department consultations and readmissions within 30 and 90 days of bariatric surgery | [27] | Cirugía Española | To determine the incidence, causes, and risk factors related to emergency consultations and readmissions within 30 and 90 days in patients undergoing laparoscopic gastric bypass and laparoscopic sleeve gastrectomy | Factorsx90
- -
Noninfectious problems related to surgical wound - -
Abdominal pain - -
Postoperative complications - -
Reintervention - -
Associated surgery type - -
Depression
| - -
Depression
|
| Patient perspectives on emergency department self-referral after bariatric surgery | [28] | Surg Obes Relat Dis. | To understand the circumstances surrounding patient self-referral to the ED after elective, primary bariatric surgery | Factorsx30
- -
Abdominal pain - -
Nausea/vomiting
| None |
| Emergency department visits and readmissions within 1 year of bariatric surgery: A statewide analysis using hospital discharge records | [29] | Surgery | Analysis of emergency department visits and readmissions to all facilities in Wisconsin within 1 year of bariatric surgery and identified their predictors | Factorsx365
- -
Gender - -
Procedure type - -
More than 4 comorbidities - -
Insurance type - -
Teaching versus nonteaching hospital - -
Inpatient complications
| - -
Gender - -
More than 4 comorbidities - -
Insurance type - -
Teaching versus nonteaching hospital
|
| Review article: Postoperative bariatric patients in the emergency department: Review of surgical complications for the emergency physician | [30] | Emerg Med Australas. | Common bariatric procedures being performed and complications, clinical presentations, and management of the bariatric patients | None | None |
| Site-specific Approach to Reducing Emergency Department Visits Following Surgery | [31] | Annals of Surgery | Efficacy exploration of current bariatric perioperative measures at reducing emergency department (ED) visits following bariatric surgery in the state of Michigan | Factorsx30
- -
Hospital’s rate of sleeve gastrectomies - -
Hospital’s rate of readmissions - -
Hospital’s rate of venous thromboembolism complications
| None |
| Effect of Bariatric Surgery on Emergency Department Visits and Hospitalizations for Atrial Fibrillation | [32] | The American Journal of Cardiology | Association of bariatric surgery with an increased risk of Atrial fibrillation episodes requiring an ED visit or hospitalization for at least 2 years after surgery among obese patients with Atrial fibrillation | Factorsx365
- -
Obese patients with Atrial fibrillation
| - -
Obese patients with Atrial fibrillation
|
References
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. 2020. Available online: https://www.cdc.gov/nchs/data/databriefs/db360-h.pdf (accessed on 3 April 2021).
- Weinick, R.M.; Burns, R.M.; Mehrotra, A. How many emergency department visits could be managed at urgent care centers and retail clinics? Health Affairs. 2010, 29, 1630–1636. [Google Scholar] [CrossRef] [PubMed]
- Wan, H.; Zhang, L.; Witz, S.; Musselman, K.J.; Yi, F.; Mullen, C.J.; Benneyan, J.C.; Zayas-Castro, J.L.; Rico, F.; Cure, L.N.; et al. A literature review of preventable hospital readmissions: Preceding the Readmissions Reduction Act. IIE Trans. Healthc. Syst. Eng. 2016, 6, 193–211. [Google Scholar] [CrossRef]
- Bhandari, P. Preoperative Predictors for 30-Day Postoperative Emergency Department Visit After a Bariatric Surgery. Ph.D. Thesis, Indiana State University, Terre Haute, IN, USA, 2022. [Google Scholar]
- Al-Odeh, M.; Smallwood, J.; Badar, M.A. A framework for implementing sustainable supply chain management. Int. J. Adv. Oper. Manag. 2021, 13, 212–233. [Google Scholar] [CrossRef]
- Guraja, P.K.; Badar, M.A.; Moayed, F.A.; Kluse, C.J. Systematic Literature Review of the Impact of State Budget Cuts on Public Higher Education Institutions in the U.S. In Proceedings of the IEOM Proceedings of the 12th International Conference on Industrial Engineering and Operations Management, Istanbul, Turkey, 7–10 March 2022. [Google Scholar]
- Gholami, H.; Abu, F.; Sharif, S.; Abdul-Nour, G.; Badar, M.A. A Review of Global Research Trends on Sustainable Manufacturing. In Sustainable Manufacturing in Industry 4.0: Pathways and Practices; Gholami, H., Abdul-Nour, G., Sharif, S., Streimikiene, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2023. [Google Scholar] [CrossRef]
- DeFeo, J.A. The Juran Trilogy: Quality Planning. Juran. 2019. Available online: https://www.juran.com/blog/the-juran-trilogy-quality-planning/ (accessed on 3 April 2021).
- Short, C.G.; Badar, M.A.; Kluse, C.J.; Schafer, M.D. Comparing Functions, Costs, and Rewards of Quality Engineers and Six Sigma Black Belts. J. Technol. Stud. 2020, 46, 52–64. Available online: https://www.jstor.org/stable/48647053 (accessed on 3 April 2021). [CrossRef]
- ProQuest. 2021. Available online: https://about.proquest.com/en/about/who-we-are/ (accessed on 3 April 2021).
- Rahimi, A.O.; Soliman, D.; Hsu, C.H.; Ghaderi, I. The impact of gender, race, and ethnicity on Bariatric Surgery Outcomes. Surg. Obes. Relat. Dis. 2024, 20, 454–461. [Google Scholar] [CrossRef]
- Ramirez, J.L.; Kim, E.; Fregenal, A.C.; Vigran, H.J.; Hughes, S.E.; Reynolds, C.W.; Varban, O.A.; Carlin, A.M.; Ehlers, A.P.; Bonham, A.J.; et al. Depression as a risk factor for adverse outcomes and increased healthcare utilization in Bariatric Surgery Patients. Surg. Endosc. 2023, 37, 9582–9590. [Google Scholar] [CrossRef]
- Dang, J.T.; Tavakoli, I.; Switzer, N.; Mocanu, V.; Shi, X.; de Gara, C.; Birch, D.W.; Karmali, S. Factors that predict 30-day readmission after Bariatric surgery: Experience of a publicly funded Canadian Centre. Can. J. Surg. 2020, 63, E174. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.S.; Al Shaikh, H.A.; Naik, B.R.; Alsalameen, A.A.; Alkhuwaytim, R.A.; Alsaleh, A.H.T.; Alsalman, B.A.; Alethan, A.M.; Almusaulem, Z.J. Knowledge Regarding Surgical Site Infection Among Postoperative Bariatric Surgical Patients in Al Ahsa City. J. Surg. 2023, 2, 79–86. [Google Scholar]
- Jaramillo, C.M. Reducing low-acuity preventable emergency room visits by utilizing urgent care center services via mobile health unit diversion program. J. Urgent Care Med. 2022, 16, 37–48. [Google Scholar]
- Shams, I.; Ajorlou, S.; Yang, K. A predictive analytics approach to reducing 30-day avoidable readmissions among patients with heart failure, acute myocardial infarction, pneumonia, or COPD. Health Care Manag. Sci. 2015, 18, 19–34. [Google Scholar] [CrossRef]
- Yavari, M.; Maihami, R.; Esmaeili, M. Ambulance dispatching and relocation problem considering overcrowding of emergency departments. IISE Trans. Healthc. Syst. Eng. 2022, 12, 263–274. [Google Scholar] [CrossRef]
- Ferrand, Y.B.; Magazine, M.J.; Rao, U.S. Partially flexible operating rooms for elective and emergency surgeries. Decis. Sci. 2014, 45, 819–847. [Google Scholar] [CrossRef]
- Dobson, G.P. Trauma of major surgery: A global problem that is not going away. Int. J. Surg. 2020, 81, 47–54. [Google Scholar] [CrossRef]
- Li, J.; Carayon, P. Health care 4.0: A vision for smart and connected health care. IISE Trans. Healthc. Syst. Eng. 2021, 11, 171–180. [Google Scholar] [CrossRef]
- Sacchetti, A. Emergency department care of the post-metabolic and bariatric surgery patient. Pediatr. Emerg. Care 2020, 36, 158–162. [Google Scholar] [CrossRef]
- Ogunniyi, A. Emergency department management of patients with complications of bariatric surgery. Emerg. Med. J. 2019, 21, 1–28. [Google Scholar]
- Khouri, A.; Alvarez, R.; Matusko, N.; Varban, O. Characterizing the preventable emergency department visit after bariatric surgery. Surg. Obes. Relat. Dis. 2020, 16, 48–55. [Google Scholar] [CrossRef]
- Tsui, S.T.; Yang, J.; Zhang, X.; Docimo, S.; Spaniolas, K.; Pryor, A.D. Hospitalizations and emergency department visits in heart failure patients after bariatric surgery. Surg. Obes. Relat. Dis. 2021, 17, 489–497. [Google Scholar] [CrossRef]
- Kuzminov, A.; Wilkinson, S.; Palmer, A.J.; Otahal, P.; Hensher, M.; Venn, A.J. Rates and reasons for emergency department presentations of patients wait-listed for public bariatric surgery in Tasmania, Australia. Obes. Res. Clin. Pract. 2019, 13, 184–190. [Google Scholar] [CrossRef]
- Leonard-Murali, S.; Nasser, H.; Ivanics, T.; Genaw, J. Predictors of postoperative emergency department visits after laparoscopic bariatric surgery. Surg. Obes. Relat. Dis. 2020, 16, 1483–1489. [Google Scholar] [CrossRef]
- Iskra, M.P.; Ramón, J.M.; Martínez-Serrano, A.; Serra, C.; Goday, A.; Trillo, L.; Lanzarini, E.; Pera, M.; Grande, L. Unplanned emergency department consultations and readmissions within 30 and 90 days of bariatric surgery. Cir. Esp. (Engl. Ed.) 2018, 96, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Stevens, H.; Wells, E.; Ross, R.; Stricklen, A.; Ghaferi, A.A. Patient perspectives on emergency department self-referral after bariatric surgery. Surg. Obes. Relat. Dis. 2018, 14, 674–681. [Google Scholar] [CrossRef]
- Mora-Pinzon, M.C.; Henkel, D.; Miller, R.E.; Remington, P.L.; Gould, J.C.; Kothari, S.N.; Funk, L.M. Emergency department visits and readmissions within 1 year of bariatric surgery: A statewide analysis using hospital discharge records. Surgery 2017, 162, 1155–1162. [Google Scholar] [CrossRef]
- Windish, R.; Wong, J. Review article: Postoperative bariatric patients in the emergency department: Review of surgical complications for the emergency physician. Emerg. Med. Australas. 2019, 31, 309–313. [Google Scholar] [CrossRef]
- Abdel Khalik, H.; Stevens, H.; Carlin, A.M.; Stricklen, A.; Ross, R.; Pesta, C.; Finks, J.F.; Ibrahim, A.; Ghaferi, A.A. Site-specific approach to reducing emergency department visits following surgery. Ann. Surg. 2018, 267, 721–726. [Google Scholar] [CrossRef]
- Shimada, Y.J.; Tsugawa, Y.; Camargo, C.A.; Brown, D.F.; Hasegawa, K. Effect of bariatric surgery on emergency department visits and hospitalizations for atrial fibrillation. Am. J. Cardiol. 2017, 120, 947–952. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).