Abstract
The use of resin-based dental composites is multiplying through the years due to the increased demand for tooth-colored restorations. The choice of monomers strongly determines the viscosity, reactivity, mechanical property, water sorption and polymerization shrinkage of the composite material. It is desirable for all monomers to be converted into polymers (Degree of Conversion), but this does not occur clinically, resulting in a poor prognosis for restorations as well as an increase in systemic health risks. The release of monomers occurs due to erosion and degradation, as well as the release of leachable species from the restoration. The potential toxicity of free monomers to dental pulp cells is concerning. Free monomers are not only allergens but also have reported cytotoxic and genotoxic effects. Various methods and practices have thus been employed to counter the ill effects of free monomer release from dental composite restorations for better safety and healthy oral cavities.
1. Introduction
Due to the increased demand for tooth-colored restorations, the use of resin-based dental composites has grown significantly. Despite their popularity, these composites have an annual failure rate of up to 3–11%, leading to increased patient visits, higher treatment costs and complications from repeated procedures [1]. Their limited service life is attributed to dimensional changes during polymerization and poor abrasion resistance.
The choice of monomers relates to the properties of dental composites, including viscosity, reactivity and polymerization shrinkage. Incomplete monomer conversion can lead to restoration degradation, biocompatibility issues and systemic health risks [2].
This review aims to shed light on the release of free monomers from composite resin restorations, a suspected cause behind their high failure rate. Specifically, we seek to
- Understand the primary mechanisms leading to free monomer release in dental composites.
- Assess the impact of this monomer release on the overall longevity and reliability of the dental restorations.
- Explore the potential health risks associated with the release of these monomers and how to overcome them.
There is a gap between in vitro studies and clinical evaluations regarding the adverse effects of monomer release [3]. Through this review, we hope to bridge this gap, providing a comprehensive understanding of this rising concern in dental practice.
2. Methodology
Search strategy: A comprehensive literature search was conducted using databases such as PubMed, Scopus and Google Scholar. The keywords used for the search included “monomer release”, “dental composites”, “resin restorations”, “polymerization kinetics” and “monomer elution”.
Inclusion and exclusion criteria: The articles were selected based on their relevance to the topic of monomer release in dental composites. Studies that focused on other aspects of dental composites or were not in English were excluded.
Data extraction: relevant data, including types of monomers, polymerization methods, factors affecting monomer release and methods for assessing monomer elution, were extracted from the selected articles.
Data synthesis: The extracted data were synthesized to provide a comprehensive overview of the current understanding of monomer release in dental composites. This synthesis informs the sections of this review article.
3. Types of Monomers Commonly Employed in Dental Composite Resins
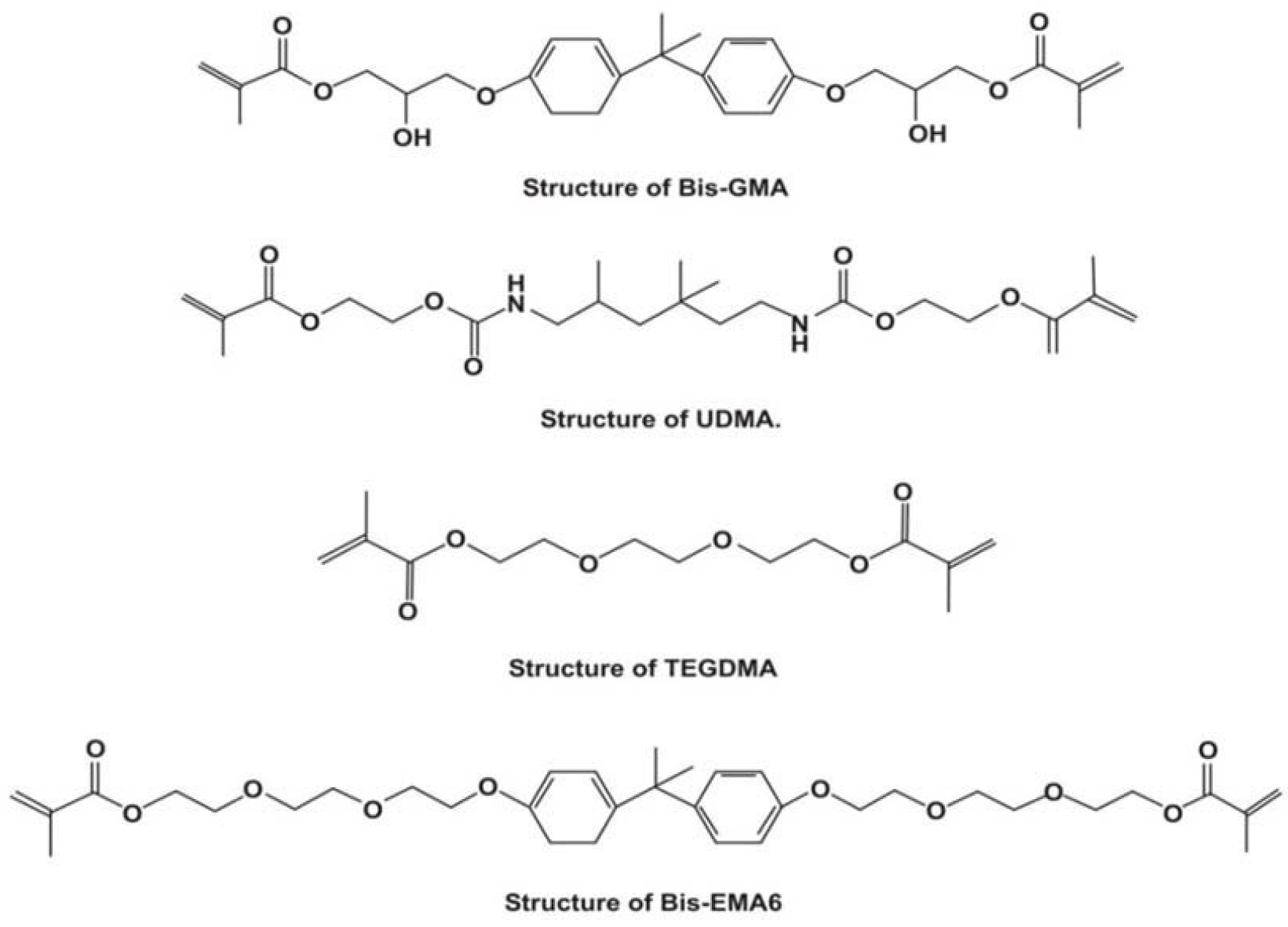
Bis-GMA: the primary monomer in dental composites known for its adhesive properties and high molecular weight, though it is viscous [4].
TEGDMA: paired with Bis-GMA to reduce viscosity, it is lighter and used in dental sealants [5].
UDMA: an alternative to Bis-GMA, it is less viscous and preferred for posterior restorations [6].
Bis-EMA: noted for reduced shrinkage and water absorption due to the absence of hydroxyl groups [7]. Figure 1 [8] shows the structural components of each monomer.
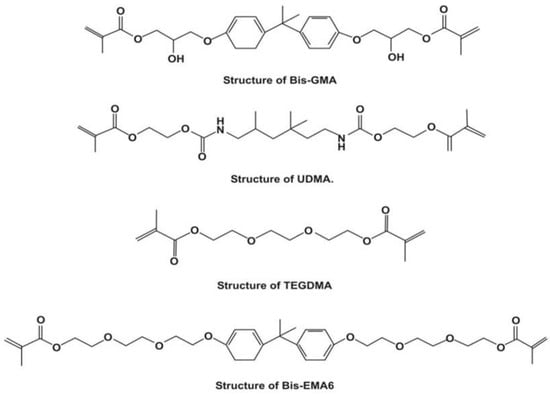
Figure 1.
Structural components of Bis-GMA, UDMA, TEGDMA and Bis-EMA.
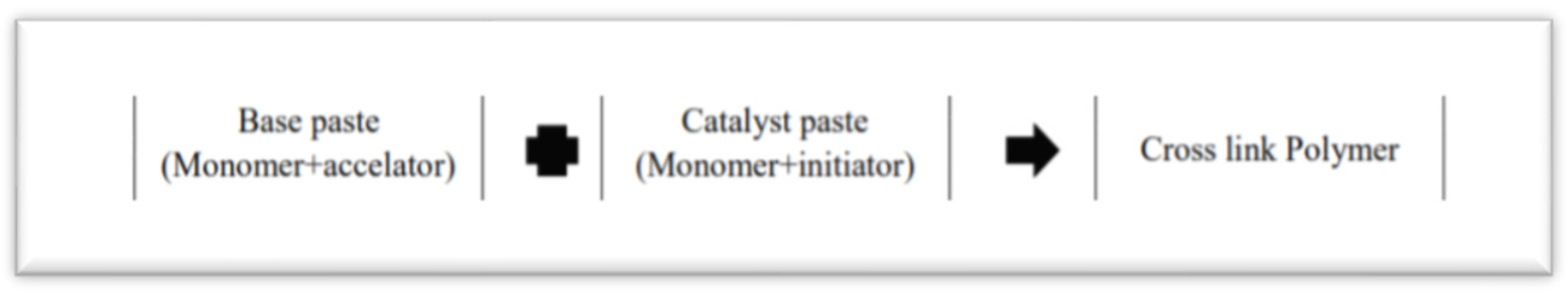
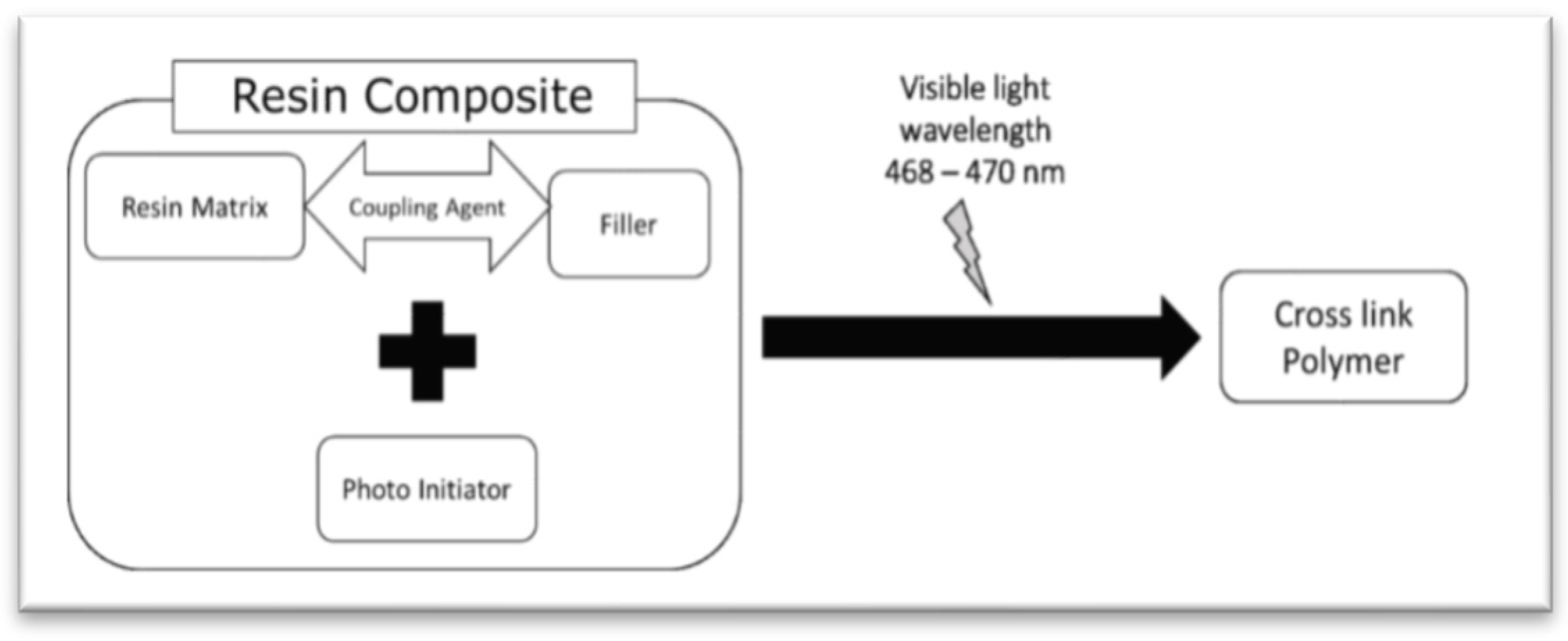
4. Polymerization Kinetics
Polymerization kinetics, the rate and sequence of monomer-to-polymer reactions, is vital in dental composites due to its influence on mechanical properties, the conversion degree and potential monomer release. Polymerization in dental composites begins when methacrylate monomers release free radicals upon exposure to external energy sources like heat or light. These radicals then bond with other monomers, forming a crosslinked polymer structure. Composite resins can be activated chemically or by light. Figure 2 [9] depicts the process of chemical polymerization and Figure 3 [9] shows the process of light polymerization.
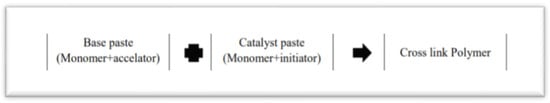
Figure 2.
Chemical Polymerization.
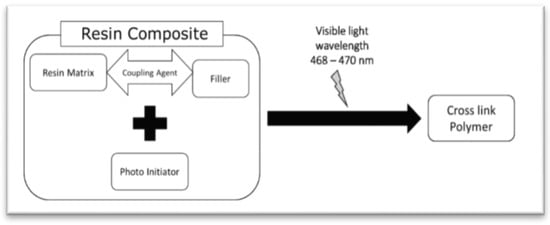
Figure 3.
Light polymerization.
5. Degree of Monomer Conversion (DC)
Residual monomers, the unreacted components in dental composites, remain despite the desired complete conversion of monomers to polymers. The DC indicates this conversion, with the ratio of carbon double bonds to single bonds revealing unreacted monomers. Typical conversion rates range between 35% and 77% [10]. Factors influencing the DC include monomer chemistry, concentration, initiator composition, polymerization conditions and filler effects. The optimal DC is crucial for ensuring the mechanical and color stability of composites [11].
6. Elution of Monomers
The elution of monomers from dental resin composites can arise from incomplete monomer conversions, polymerization conditions and composite degradation. Such elution can elevate systematic health risks, and while the DC influences composite mechanics, it does not directly predict monomer elution [2]. Composite resins can release over 30 chemicals, including residual monomers, initiators and impurities [12]. The polymer network’s structure can influence this monomer release. While the exact elution duration remains uncertain, some studies suggest a 1–7-day period for the complete elution of unreacted monomers [13].
Polydorou et al. [14] studied monomer elution in hybrid and flowable composites over varying polymerization and storage times. They found that BisGMA consistently released more than TEGDMA for up to 28 days, and hybrid resins released more monomers than flowable composites. The monomer elution from bulk fill composites is comparable to that of conventional materials [15]. Bleaching agents might cause filler loss in dental composites, affecting surface properties. A study confirmed increased monomer release post-bleaching, possibly due to damage from carbamide peroxide and hydrogen peroxide [16]. However, TEGDMA and BISGMA, being long-chain molecules, might resist oxidative decomposition, reducing monomer release. The evidence of monomer elution post-bleaching remains mixed.
6.1. Adverse Effects and Health Risks of Monomer Elution
Unreacted monomers and leachable species from dental composites pose potential biological risks. These free monomers can diffuse into the oral environment and may come into contact with soft tissues, leading to
- Local effects: monomers can irritate oral tissues, causing symptoms like burning, redness and ulcerations and may induce inflammation in gums [5,17].
- Systemic effects: monomers, once absorbed, present potential systemic threats, including cytotoxicity and endocrine disruption, though real-world implications are still under study [7].
- Allergic reactions: some individuals may exhibit allergic reactions to specific monomers, such as dermatitis or respiratory issues [12].
6.2. Methods to Determine Residual Monomer Elution
Various methods assess the type and amount of residual monomers eluted from dental composites, which is crucial for understanding their biological effects:
- High-performance liquid chromatography (HPLC) is a primary quantitative method for separating and quantifying monomers [4].
- Gas Chromatography (GC), another quantitative method, is apt for volatile monomers [17].
- Fourier-Transform Infrared Spectroscopy (FTIR) identifies the chemical structures of eluted monomers [7].
- Nuclear Magnetic Resonance offers detailed molecular insights and quantification [12].
- Direct Contact Tests gauge the biological impact by observing cytotoxic effects on cell cultures [5].
7. Impact of Filler Loading on Free Monomer Release from Composites
Micro/nanosized fillers in the composite matrix optimize polymerization, reducing free monomer release and enhancing physio-chemical and mechanical properties. The filler type, content, size and refractive index influence polymerization due to light transmission effects, with filler loading directly correlating to monomer elution [18]. The addition of high-refractive-index materials, like HA-ZrO2 and BaO, boosts polymerization and monomer conversion. Thus, matching the refractive indices of fillers and the organic matrix is crucial for the optimal depth of cure. The filler size affects light scattering during polymerization, impacting cure depth [19]. For instance, 250–500 nm spherical silica fillers had a lower DC compared to those with diameters between 100 and 1000 nm [20]. Despite agglomeration in nanoparticles, smaller fillers resulted in a decreased DC.
8. Effect of Monomer Elution on the Mechanical Properties of Composites
In direct restorations, monomers create a dense structure, resisting staining. However, unreacted monomers can weaken a material’s mechanical properties [21].
A higher DC leads to improved composite properties, including:
- Strength and durability: a higher DC results in a denser polymer network, boosting mechanical strength and wear resistance [6].
- Reduction in polymerization shrinkage: an increased conversion minimizes unreacted monomers, reducing polymerization shrinkage and enhancing marginal adaptation [22].
- Decreased solubility and water absorption: well-converted composites resist water absorption and degradation, ensuring durability [23].
- Improved aesthetics: a higher DC also improves composite aesthetics, enhancing color stability and translucency [19].
9. Effect of Curing on the Free Monomer Release
Incomplete conversion arises from vitrification, gelation and steric isolation. These factors reduce the diffusion rate in the organic matrix, obstructing the polymer network and affecting polymerization. The irradiation time and light intensity crucially impact polymerization and the DC. Shortening polymerization from 40 to 20 s increases the number of unbound monomers, while extending the irradiation time by 20 s reduces the number of residual monomers [13,24]. Maintaining close proximity between the light source and resin material is essential due to the direct proportionality of light intensity to distance [25].
10. Effect of Photoinitiators and Light Source
Out of the wide array of options, there is often a dilemma in making a choice of curing units. The options range from conventional units to tungsten halogen and plasma arc curing units. For optimal curing, an adequate amount of light intensity at the right wavelength must fall on all the parts of the restorative material. The intrinsic factors affecting the DC are the structure of the resin monomer as well as the concentration of photoinitiators, while the extrinsic factors include the distance of the source of light from the restorative material and the properties of the curing light [26]. Halogen lamps emit a broad wavelength range, while LEDs have a narrower 440–490 nm range, making LEDs more efficient. However, their efficacy is mainly effective for composites using camphorquinone as initiators. Plasma arc units, despite their high light intensity, are debated due to issues like heat generation and increased polymerization shrinkage.
11. Post-Cure Heating of Composites
The post-cure heating of composites, a popular restorative technique, involves the immediate heat treatment of light-cured composite inlays. This method not only enhances the material’s cure but also improves its properties [27]. It has been observed to increase the cure, reducing the amount of unreacted monomer compared to solely light-cured restorations.
12. Free Monomer Release Due to Long-Term Degradation and Erosion of Composites
Composites undergo chemical degradation through enzymatic catalysis and hydrolysis. Esterases from saliva and other enzymes interact with composites, leading to degradation [28]. Salivary water can penetrate the polymerized network, causing the diffusion of uncured monomers. Intraoral composite biodegradation can arise from masticatory forces, especially with pre-existing material voids and stresses. Eating- and drinking-induced thermal changes, differences in CTE and oral microbes further contribute to composite degradation [29].
13. Chromatic Instability Due to Free Monomer Release
Monomer elution from composites can lead to discoloration due to the oxidation of residual double bonds [30]. The oxygen inhibition layer, which hinders the final composite layer’s curing, plays a significant role in this chromatic instability [31]. Using mylar strips and glycerine before light curing can mitigate this effect.
14. Secondary Caries as a Result of Free Monomer Release
Free monomers serve as substrates for cariogenic bacteria, leading to secondary caries, especially when combined with polymerization shrinkage. Bacteria like Lactobacillus acidophilus and Streptococcus Sorbitans proliferate due to monomers like EGDMA and TEGDMA. Modern adhesive technologies form a hybrid layer with an interface of under 1 micrometer. Yet, microorganisms like Lactobacillus, being only 0.1 micrometer in size, can penetrate gaps from polymerization shrinkage [32]. Using monomers with minimized polymerization shrinkage can enhance a material’s longevity, reducing the risks of fractures and secondary caries.
15. Effect on Dental Pulp
Dental composites’ widespread use raises concerns about free monomers’ toxicity to dental pulp cells (DPCs). Even without direct pulp contact, these monomers interact with dental composites, diffusing through dentin and altering DPC physiology [33]. High concentrations of unpolymerized monomers, especially TEGDMA and HEMA, can disrupt DPC differentiation and essential mineralization processes [34]. While bacterial contamination was once blamed, recent studies point to eluted monomers, though the extent of their adverse effects remains debated.
16. Allergic Reactions to Residual Monomers
A four-year study in Norway found that 8% of patients had allergic reactions to resin-based materials out of 296 patients, primarily manifesting as skin and mucosal reactions [35]. Adverse reactions to methacrylate-based resins include dermatoses, fingertip paraesthesia and allergic pharyngitis [36]. TEGDMA inhibits oral epithelial cell growth, induces mitochondrial damage and is 2–5 times more cytotoxic than HEMA to pulmonary cells [37].
Molecular studies explore how dental composite monomers impact cellular health, particularly by inducing apoptosis in gingival and pulp cells. Apoptosis, a regulated process vital for tissue balance, can be disrupted by unreacted monomers. Monomers like BisGMA and TEGDMA trigger apoptosis in specific cells via the mitochondrial pathway. This leads to caspase activation and increased reactive oxygen species (ROS) production, damaging DNA, proteins and lipids [38]. Recognizing these mechanisms is essential to understanding dental composite effects and the need to reduce monomer release.
17. Genotoxic Effects
TEGDMA induces the deletion of significant DNA sequences in mammalian cells [39]. Using the Commet Assay, TEGDMA, UDMA and Bis-GMA monomers showed minor DNA migration enhancement, indicating potential genotoxicity [40]. There is also emerging evidence of tumor activity in human salivary glands [41].
18. Estrogenic Effects
In vitro studies indicate that bisphenol A dimethacrylate (BPA-DMA), when cleaved, forms BPA, causing estrogenic reactions. In vivo experiments on mice link BPA to reproductive system issues [42]. Yet, a human study found no BPA in blood or saliva 24 h post-exposure.
19. Methods to Counteract Free Monomer Content
Research has explored newer monomers to address the limitations of traditional ones. Alternatives to conventional TEGDMA, like Acet-GDMA, ISETMDA and PPGDMA, have shown similar viscosities but with less shrinkage and cytotoxicity. Efforts have also identified BisGMA alternatives to reduce bisphenol A exposure due to its cytotoxic effects. Biobased monomers derived from isosorbide showed reduced in vitro cytotoxicity [43]. Bis-GMA-analogous monomers, with hydroxyl-to-ester substitutions, achieved a higher monomer conversion due to increased hydrophobicity, reducing water solubility. New vinyl monomers, TEG-DVBE and Phene, outperformed methacrylate-based dental composites in terms of strength, shrinkage and the DC, extending the material lifespan [44]. Click chemistry introduced thiol-ene, thiol-michael and thio-urethane reactions to dental resins [45]. These offer rapid photopolymerization, fewer unreacted groups, minimal oxygen inhibition, delayed vitrification and a more uniform polymer network [46].
Ring-opening monomers, such as spiro orthocarbonates, vinylcyclopropanes, epoxies and siloranes, reduce volumetric and polymerization stress in dental composites due to their unique double ring-opening polymerization [47].
19.1. Implications of Advanced Strategies in Dental Composites
- Altered curing protocols: Stepped or ramped curing enhances the cure depth and conversion but demands more practitioner time and precision. Incorrect curing can lead to post-operative issues [48].
- Optimized polymerization: using varied light wavelengths improves monomer conversion but may require specialized equipment, impacting finances.
- Alternate monomers: While promising higher reactivity, alternative monomers need extensive study for biocompatibility, aesthetics and material interaction. They may also alter handling properties.
19.2. Recent Advancements to Reduce the Monomer Release
- Optimized curing: stepped curing protocols increase the cure depth and conversion [48].
- Nanofiller tech: using nanofillers enhances conversion [49].
- Photoinitiators: advanced systems bolster polymerization and reduce elution [50].
- Additives: thio-urethanes fortify the polymer, improving conversion and minimizing leaching [46].
19.3. Potential Risks of Altered Curing and Alternate Monomers
Advancements in curing protocols and alternate monomers, while promising, come with potential challenges:
Altered curing protocols:
- Over-curing: This may cause overheating, leading to pulpal damage or sensitivity [51].
- Under-curing: This can result in reduced mechanical properties and increased monomer release [48].
Alternate monomers: biocompatibility: New monomers might introduce unexplored tissue reactions or sensitivities. Their different handling characteristics and potential interactions with existing dental materials need consideration [50].
20. Conclusions
Though dental composites have many advantages and are the most preferred dental material for restorations today, the monomer selection and the ratio play an important role in the safety of the material. As free monomers have a deleterious effect on pulp, biological considerations should be given importance. The minimal leaching of free monomers can exhibit cytotoxic, genotoxic and estrogenic effects over a long period of time. If all protective and preventive measures to minimize free monomer release are selected, then composite materials may be a very safe choice as a restorative material in the oral cavity.
Author Contributions
Conceptualization, A.D. and S.R.A.; methodology, A.D., S.R.A. and A.M.; software, A.M.; validation, S.R.A. and S.K.; formal analysis, S.R.A., A.M. and V.H.; investigation, A.D. and S.R.A.; resources S.K. and V.H.; data curation, A.D., S.R.A. and A.M.; writing—original draft preparation, A.D., S.R.A. and S.K.; writing—review and editing, A.D., S.R.A., S.K. and V.H.; supervision, S.R.A. and S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data used are made available in the present work.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ástvaldsdóttir, Á.; Dagerhamn, J.; van Dijken, J.W.; Naimi-Akbar, A.; Sandborgh-Englund, G.; Tranæus, S.; Nilsson, M. Longevity of posterior resin composite restorations in adults—A systematic review. J. Dent. 2015, 43, 934–954. [Google Scholar] [CrossRef]
- Chang, M.C.; Lin, L.D.; Chuang, F.H.; Chan, C.P.; Wang, T.M.; Lee, J.J.; Jeng, P.Y.; Tseng, W.Y.; Lin, H.J.; Jeng, J.H. Carboxylesterase expression in human dental pulp cells: Role in regulation of BisGMA-induced prostanoid production and cytotoxicity. Acta Biomater. 2012, 8, 1380–1387. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G. The biocompatibility of non-amalgam dental filling materials. Eur. J. Oral Sci. 1998, 106, 696–706. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Elution of leachable components from composites. J. Oral Rehabil. 1994, 21, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Preiss, A.; Arenholt-Bindslev, D. Bisphenol-A content of resin monomers and related degradation products. Clin. Oral Investig. 1999, 3, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Peutzfeldt, A. Resin composites in dentistry: The monomer systems. Eur. J. Oral Sci. 1997, 105, 97–116. [Google Scholar] [CrossRef] [PubMed]
- Sideridou, I.; Tserki, V.; Papanastasiou, G. Study of water sorption, solubility and modulus of elasticity of light-cured dimethacrylate-based dental resins. Biomaterials 2003, 24, 655–665. [Google Scholar] [CrossRef]
- Zafar, M.; Liaqat, S.; Najeeb, S.; Khurshid, Z.; Alrahabi, M.; Zohaib, S. Resin Polymers based tooth coloured filling dental materials. In Polymer Science: Research Advances, Practical Applications and Educational Aspects; Formatex Research Center S.L.: Badajoz, Spain, 2016; pp. 461–469. [Google Scholar]
- Riva, Y.R.; Rahman, S.F. Dental composite resin: A review. AIP Conf. Proc. 2019, 2193, 020011. [Google Scholar]
- Ferracane, J.L. Current trends in dental composites. Crit. Rev. Oral Biol. Med. Off. Publ. Am. Assoc. Oral Biol. 1995, 6, 302–318. [Google Scholar] [CrossRef]
- Braga, R.R.; Ferracane, J.L. Contraction stress related to degree of conversion and reaction kinetics. J. Dent. Res. 2002, 81, 114–118. [Google Scholar] [CrossRef]
- Michelsen, V.B.; Lygre, H.; Skålevik, R.; Tveit, A.B.; Solheim, E. Identification of organic eluates from four polymer-based dental filling materials. Eur. J. Oral Sci. 2003, 111, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, K.; Taira, M.; Shintani, H.; Wakasa, K.; Yamaki, M. Residual monomers (TEGDMA and Bis-GMA) of a set visible-light-cured dental composite resin when immersed in water. J. Oral Rehabil. 1991, 18, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Polydorou, O.; Trittler, R.; Hellwig, E.; Kümmerer, K. Elution of monomers from two conventional dental composite materials. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2007, 23, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Alshali, R.Z.; Salim, N.A.; Sung, R.; Satterthwaite, J.D.; Silikas, N. Analysis of long-term monomer elution from bulk-fill and conventional resin-composites using high performance liquid chromatography. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2015, 31, 1587–1598. [Google Scholar] [CrossRef]
- Polydorou, O.; Hellwig, E.; Auschill, T.M. The effect of different bleaching agents on the surface texture of restorative materials. Oper. Dent. 2006, 31, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Geurtsen, W. Substances released from dental resin composites and glass ionomer cements. Eur. J. Oral Sci. 1998, 106, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Munksgaard, E.C.; Peutzfeldt, A.; Asmussen, E. Elution of TEGDMA and BisGMA from a resin and a resin composite cured with halogen or plasma light. Eur. J. Oral Sci. 2000, 108, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Ruyter, I.E.; Oysaed, H. Conversion in different depths of ultraviolet and visible light activated composite materials. Acta Odontol. Scand. 1982, 40, 179–192. [Google Scholar] [CrossRef]
- Turssi, C.P.; Ferracane, J.L.; Vogel, K. Filler features and their effects on wear and degree of conversion of particulate dental resin composites. Biomaterials 2005, 26, 4932–4937. [Google Scholar] [CrossRef]
- Prasanna, N.; Pallavi Reddy, Y.; Kavitha, S.; Lakshmi Narayanan, L. Degree of conversion and residual stress of preheated and room-temperature composites. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2007, 18, 173–176. [Google Scholar] [CrossRef]
- Braga, R.R.; Ballester, R.Y.; Ferracane, J.L. Factors involved in the development of polymerization shrinkage stress in resin-composites: A systematic review. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2005, 21, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Ferracane, J.L. Hygroscopic and hydrolytic effects in dental polymer networks. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2006, 22, 211–222. [Google Scholar] [CrossRef] [PubMed]
- AlShaafi, M.M. Factors affecting polymerization of resin-based composites: A literature review. Saudi Dent. J. 2017, 29, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Aravamudhan, K.; Rakowski, D.; Fan, P.L. Variation of depth of cure and intensity with distance using LED curing lights. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2006, 22, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Leprince, J.G.; Palin, W.M.; Hadis, M.A.; Devaux, J.; Leloup, G. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2013, 29, 139–156. [Google Scholar] [CrossRef] [PubMed]
- Asmussen, E. Restorative resins: Hardness and strength vs. quantity of remaining double bonds. Scand. J. Dent. Res. 1982, 90, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Geurtsen, W. Biocompatibility of resin-modified filling materials. Crit. Rev. Oral Biol. Med. Off. Publ. Am. Assoc. Oral Biol. 2000, 11, 333–355. [Google Scholar] [CrossRef]
- Bettencourt, A.F.; Neves, C.B.; de Almeida, M.S.; Pinheiro, L.M.; Oliveira, S.A.; Lopes, L.P.; Castro, M.F. Biodegradation of acrylic based resins: A review. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2010, 26, e171–e180. [Google Scholar] [CrossRef]
- Souza, R.O.; Ozcan, M.; Michida, S.M.; de Melo, R.M.; Pavanelli, C.A.; Bottino, M.A.; Soares, L.E.; Martin, A.A. Conversion degree of indirect resin composites and effect of thermocycling on their physical properties. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2010, 19, 218–225. [Google Scholar] [CrossRef]
- Marigo, L.; Nocca, G.; Fiorenzano, G.; Callà, C.; Castagnola, R.; Cordaro, M.; Paolone, G.; Sauro, S. Influences of Different Air-Inhibition Coatings on Monomer Release, Microhardness, and Color Stability of Two Composite Materials. BioMed Res. Int. 2019, 2019, 4240264. [Google Scholar] [CrossRef]
- Hashimoto, M.; Ito, S.; Tay, F.R.; Svizero, N.R.; Sano, H.; Kaga, M.; Pashley, D.H. Fluid movement across the resin-dentin interface during and after bonding. J. Dent. Res. 2004, 83, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Gerzina, T.M.; Hume, W.R. Diffusion of monomers from bonding resin-resin composite combinations through dentine in vitro. J. Dent. 1996, 24, 125–128. [Google Scholar] [CrossRef] [PubMed]
- About, I.; Camps, J.; Mitsiadis, T.A.; Bottero, M.J.; Butler, W.; Franquin, J.C. Influence of resinous monomers on the differentiation in vitro of human pulp cells into odontoblasts. J. Biomed. Mater. Res. 2002, 63, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Vamnes, J.S.; Lygre, G.B.; Grönningsaeter, A.G.; Gjerdet, N.R. Four years of clinical experience with an adverse reaction unit for dental biomaterials. Community Dent. Oral Epidemiol. 2004, 32, 150–157. [Google Scholar] [CrossRef]
- Hume, W.R.; Gerzina, T.M. Bioavailability of components of resin-based materials which are applied to teeth. Crit. Rev. Oral Biol. Med. Off. Publ. Am. Assoc. Oral Biol. 1996, 7, 172–179. [Google Scholar] [CrossRef]
- Reichl, F.X.; Walther, U.I.; Durner, J.; Kehe, K.; Hickel, R.; Kunzelmann, K.H.; Spahl, W.; Hume, W.R.; Benschop, H.; Forth, W. Cytotoxicity of dental composite components and mercury compounds in lung cells. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2001, 17, 95–101. [Google Scholar] [CrossRef]
- Krifka, S.; Spagnuolo, G.; Schmalz, G.; Schweikl, H. A review of adaptive mechanisms in cell responses towards oxidative stress caused by dental resin monomers. Biomaterials 2013, 34, 4555–4563. [Google Scholar] [CrossRef]
- Schweikl, H.; Schmalz, G. Triethylene glycol dimethacrylate induces large deletions in the hprt gene of V79 cells. Mutat. Res. 1999, 438, 71–78. [Google Scholar] [CrossRef]
- Kleinsasser, N.H.; Wallner, B.C.; Harréus, U.A.; Kleinjung, T.; Folwaczny, M.; Hickel, R.; Kehe, K.; Reichl, F.X. Genotoxicity and cytotoxicity of dental materials in human lymphocytes as assessed by the single cell microgel electrophoresis (comet) assay. J. Dent. 2004, 32, 229–234. [Google Scholar] [CrossRef]
- Kleinsasser, N.H.; Schmid, K.; Sassen, A.W.; Harréus, U.A.; Staudenmaier, R.; Folwaczny, M.; Glas, J.; Reichl, F.X. Cytotoxic and genotoxic effects of resin monomers in human salivary gland tissue and lymphocytes as assessed by the single cell microgel electrophoresis (Comet) assay. Biomaterials 2006, 27, 1762–1770. [Google Scholar] [CrossRef]
- Al-Hiyasat, A.S.; Darmani, H.; Elbetieha, A.M. Leached components from dental composites and their effects on fertility of female mice. Eur. J. Oral Sci. 2004, 112, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Herrera-González, A.M.; Pérez-Mondragón, A.A.; Cuevas-Suárez, C.E. Evaluation of bio-based monomers from isosorbide used in the formulation of dental composite resins. J. Mech. Behav. Biomed. Mater. 2019, 100, 103371. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Huyang, G.; Palagummi, S.V.; Liu, X.; Skrtic, D.; Beauchamp, C.; Bowen, R.; Sun, J. High performance dental resin composites with hydrolytically stable monomers. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2018, 34, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Cramer, N.B.; Couch, C.L.; Schreck, K.M.; Boulden, J.E.; Wydra, R.; Stansbury, J.W.; Bowman, C.N. Properties of methacrylate-thiol-ene formulations as dental restorative materials. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2010, 26, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Bacchi, A.; Pfeifer, C.S. Rheological and mechanical properties and interfacial stress development of composite cements modified with thio-urethane oligomers. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2016, 32, 978–986. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Liu, W.; Hao, Z.; Wu, X.; Yin, J.; Panjiyar, A.; Liu, X.; Shen, J.; Wang, H. Characterization of a low shrinkage dental composite containing bismethylene spiroorthocarbonate expanding monomer. Int. J. Mol. Sci. 2014, 15, 2400–2412. [Google Scholar] [CrossRef] [PubMed]
- Halvorson, R.H.; Erickson, R.L.; Davidson, C.L. The effect of filler and silane content on conversion of resin-based composite. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2003, 19, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Beun, S.; Glorieux, T.; Devaux, J.; Vreven, J.; Leloup, G. Characterization of nanofilled compared to universal and microfilled composites. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2007, 23, 51–59. [Google Scholar] [CrossRef]
- Moszner, N.; Salz, U.; Zimmermann, J. Chemical aspects of self-etching enamel-dentin adhesives: A systematic review. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2005, 21, 895–910. [Google Scholar] [CrossRef]
- Price, R.B.; Labrie, D.; Rueggeberg, F.A.; Sullivan, B.; Kostylev, I.; Fahey, J. Correlation between the beam profile from a curing light and the microhardness of four resins. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2014, 30, 1345–1357. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).