Acquiring Wearable Photoplethysmography Data in Daily Life: The PPG Diary Pilot Study †
Abstract
:1. Introduction
2. Methods
2.1. Study Participant
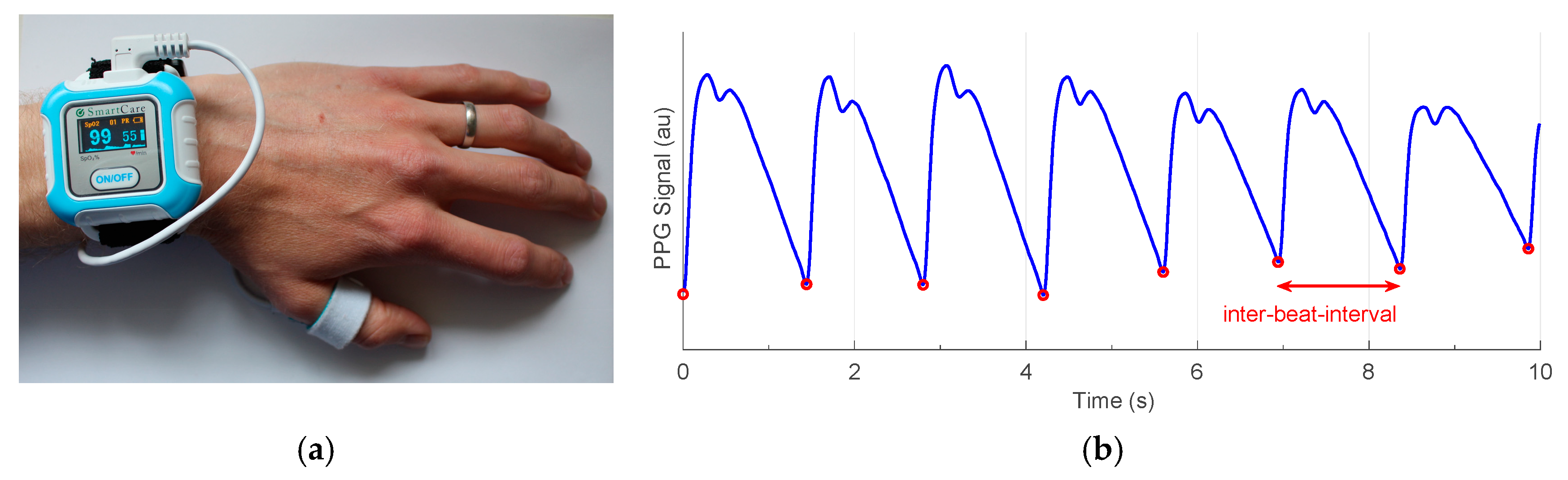
2.2. Data Collection
2.3. Data Curation and Analysis
3. Results and Discussion
3.1. Device Usage
3.2. Data Capture
3.3. Signal Quality
3.4. Potential Utility for Pulse Wave Analysis
3.5. Limitations and Future Work
4. Conclusions
Funding
Conflicts of Interest
References
- Pereira, T.; Tran, N.; Gadhoumi, K.; Pelter, M.M.; Do, D.H.; Lee, R.J.; Colorado, R.; Meisel, K.; Hu, X. Photoplethysmography based atrial fibrillation detection: A review. NPJ Digit. Med. 2020, 3, 3. [Google Scholar] [CrossRef] [PubMed]
- Radin, J.M.; Wineinger, N.E.; Topol, E.J.; Steinhubl, S.R. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: A population-based study. Lancet Digit. Health 2020, 2, e85–e93. [Google Scholar] [CrossRef]
- Elgendi, M.; Fletcher, R.; Liang, Y.; Howard, N.; Lovell, N.H.; Abbott, D.; Lim, K.; Ward, R. The use of photoplethysmography for assessing hypertension. NPJ Digit. Med. 2019, 2, 60. [Google Scholar] [CrossRef] [PubMed]
- Bonnici, T.; Orphanidou, C.; Vallance, D.; Darrell, A.; Tarassenko, L. Testing of wearable monitors in a real-world hospital environment: What lessons can be learnt? In Proceedings of the Conf Proc 9th Wearable and Implantable BSNs, London, UK, 9–12 May 2012; pp. 79–84. [Google Scholar] [CrossRef]
- Charlton, P.H.; Birrenkott, D.A.; Bonnici, T.; Pimentel, M.A.F.; Johnson, A.E.W.; Alastruey, J.; Tarassenko, L.; Watkinson, P.J.; Beale, R.; Clifton, D.A. Breathing rate estimation from the electrocardiogram and photoplethysmogram: A review. IEEE Rev. Biomed. Eng. 2018, 11, 2–20. [Google Scholar] [CrossRef] [PubMed]
- Reiss, A.; Indlekofer, I.; Schmidt, P.; Van Laerhoven, K. Deep PPG: Large-scale heart rate estimation with convolutional neural networks. Sensors 2019, 19, 3079. [Google Scholar] [CrossRef] [PubMed]
- Orphanidou, C.; Bonnici, T.; Charlton, P.; Clifton, D.; Vallance, D.; Tarassenko, L. Signal-quality indices for the electrocardiogram and photoplethysmogram: Derivation and applications to wireless monitoring. IEEE J. Biomed. Health Inform. 2015, 19, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.H.; Mariscal Harana, J.; Vennin, S.; Li, Y.; Chowienczyk, P.; Alastruey, J. Modeling arterial pulse waves in healthy aging: A database for in silico evaluation of hemodynamics and pulse wave indexes. Am. J. Physiol. Circ. Physiol. 2019, 317, H1062–H1085. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.H. PulseAnalyse: A Signal Processing Tool for Cardiovascular Pulse Waves. Available online: https://doi.org/10.5281/zenodo.3272122 (accessed on 19 October 2020).
- Aboy, M.; McNames, J.; Thong, T.; Tsunami, D.; Ellenby, M.S.; Goldstein, B. An automatic beat detection algorithm for pressure signals. IEEE Trans. Biomed. Eng. 2005, 52, 1662–1670. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.V.; Mahaffey, K.W.; Hedlin, H.; Rumsfeld, J.S.; Garcia, A.; Ferris, T.; Balasubramanian, V.; Russo, A.M.; Rajmane, A.; Cheung, L.; et al. Large-scale assessment of a smartwatch to identify atrial fibrillation. N. Engl. J. Med. 2019, 381, 1909–1917. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Pi, Z.; Liu, B. TROIKA: A general framework for heart rate monitoring using wrist-type photoplethysmographic signals during intensive physical exercise. IEEE Trans. Biomed. Eng. 2015, 62, 522–531. [Google Scholar] [CrossRef] [PubMed]
- Charlton, P.H. PPG Diary Pilot Study 1 Data. Available online: https://doi.org/10.5281/zenodo.3268500 (accessed on 19 October 2020).
- Charlton, P.H. PPG Diary Project website. Available online: https://peterhcharlton.github.io/ppg-diary/ (accessed on 19 October 2020).



| Endpoint | Time, Hours (%) |
|---|---|
| Possible wear time: the time for which the participant was asked to wear the device | 576.8 (100.0) |
| Wear time: the time for which the participant noted they wore the device | 432.3 (75.0) |
| Signal time: the time for which a PPG signal was acquired | 349.3 (60.6) |
| High quality signal time: the time for which a high quality signal was acquired | 176.1 (30.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charlton, P.H.; Kyriacou, P.; Mant, J.; Alastruey, J. Acquiring Wearable Photoplethysmography Data in Daily Life: The PPG Diary Pilot Study. Eng. Proc. 2020, 2, 80. https://doi.org/10.3390/ecsa-7-08233
Charlton PH, Kyriacou P, Mant J, Alastruey J. Acquiring Wearable Photoplethysmography Data in Daily Life: The PPG Diary Pilot Study. Engineering Proceedings. 2020; 2(1):80. https://doi.org/10.3390/ecsa-7-08233
Chicago/Turabian StyleCharlton, Peter H., Panicos Kyriacou, Jonathan Mant, and Jordi Alastruey. 2020. "Acquiring Wearable Photoplethysmography Data in Daily Life: The PPG Diary Pilot Study" Engineering Proceedings 2, no. 1: 80. https://doi.org/10.3390/ecsa-7-08233
APA StyleCharlton, P. H., Kyriacou, P., Mant, J., & Alastruey, J. (2020). Acquiring Wearable Photoplethysmography Data in Daily Life: The PPG Diary Pilot Study. Engineering Proceedings, 2(1), 80. https://doi.org/10.3390/ecsa-7-08233






