1. Introduction
Motor vehicle accidents, including automobile and motorcycle accidents, may cause severe multiple life-threatening injuries. Many of the multiple trauma patients have associated intracranial, thoracic aortic disruption, abdominal and pelvic injuries—including renal and urinary bladder injuries—consequent to these accidents. This patient, on arrival to our emergency room, had examination on the transport gurney which revealed a blood pressure of 60/40, multiple long bone fractures, a weak pulse, and multiple contusions. The emergency department staff obtained an immediate computerized tomography (C-T) of the chest and abdomen, along with an aortogram. Presented is the case report of a severely injured hypotensive individual with thoracic aortic disruption, abdominal (especially splenic and liver lacerations), urinary system injuries (left renal artery total disruption from the aorta and bladder laceration), and fractures of all long bones but one and their corrective approach.
2. Case History
A sixteen year-old young man, while riding a motorcycle, was struck by an automobile driven by an individual under the influence of alcohol. This severely injured young man was brought to our community hospital emergency room in a critical condition. Emergency room evaluation, of the patient on the ambulance gurney, revealed a hypotensive (60/40) poorly responsive individual with multiple injuries and contusions.
The initial physical examination presented a patient with multiple bony deformities of the extremities, a weak pulse, and tender abdomen and chest. Emergency radiographic studies included C-T with IV contrast of the chest, head, and abdomen. The extremity X-rays demonstrated multiple long bone fractures in all extremities except one. The C-T studies showed right upper and lower lung infiltration and multiple pelvic fractures, absence of left renal perfusion, and aortic disruption just below the level of the left subclavian artery origin [
1]. The patient had hematuria which was evaluated by the urologist via a retrograde cystourethrogram which demonstrated a cystourethral disruption, in addition to a bladder disruption. After orthopedic, urology, and cardiothoracic consultation, the patient was prepared for emergency corrective thoracic, abdominal, and pelvic surgery [
2,
3,
4]. This included the thoracic aorta repair, probable splenectomy, possible renal artery and bladder repair, and long bone stabilization.
3. Materials and Method
Due to the multiple extensive injuries, the patient was taken directly from radiology to the surgical operative suite for surgical intervention, including repair of the thoracic aorta, abdominal exploration, urinary (left kidney), and orthopedic stabilization. After multiple intravenous line access, arterial line placement, and splinting of the long bones, the patient was prepared for open thoracic and abdominal surgery. Following endotracheal intubation (which yielded bloody fluid) and administration of blood and blood product transfusion for persistent hypotension (systolic 50–60 mmHg), utilizing a retrograde approach, insertion of a Foley catheter produced bloody fluid.
Table 1 presents the major findings at surgery.
3.1. Thoracoabdominal Repair
The left thoracotomy presented a mediastinal hematoma with a posterior mediastinal tear. A Dacron left subclavian artery to the distal thoracic aorta bypass graft and suture ligation of the transected aortic stump without heparinization (to avoid more bleeding or possible intracranial bleeding) was then completed (
Figure 1). Of note, the mediastinal pleural tamponade had contained the mediastinal hematoma and allowed the patient to have weak femoral pulses preoperatively despite a transected aorta.
Table 2 lists the major procedures utilized to stabilize and treat the patient in the operating room.
After repair of the diaphragm tear and lung laceration, and closure of the chest, we planned a subdiaphragmatic repair of the intra-abdominal injuries depending on the findings and patient condition. The patient was then placed in the supine position for the intra-abdominal surgical intervention which included splenectomy (for multiple ruptures), which had a poorly visualized arterial supply and evacuation of a large volume of free intra-abdominal blood; this was felt to be a contributing cause of the persistent hypotension along with the multiple fractures. Pathologic review of the spleen demonstrated multiple lacerations in the upper, middle, and lower thirds of the spleen, while the microscopic aortic tissue demonstrated only traumatic rupture changes of a normal aorta. Also, both the mesenteric and liver lacerations were repaired.
3.2. Urinary System
The right kidney appeared to be functioning well on review of the angiograms. Palpably, at surgery, there was a left kidney, but angiography demonstrated no evidence nor visualization of the left renal arterial system—nor of the left renal pelvis and collecting system. Also, the left ureter was not visualized in the study, and no evidence of a left aortourinary fistula was present [
5]. The right renal pelvis and collecting system appeared to be normal without visualization of the urinary bladder.
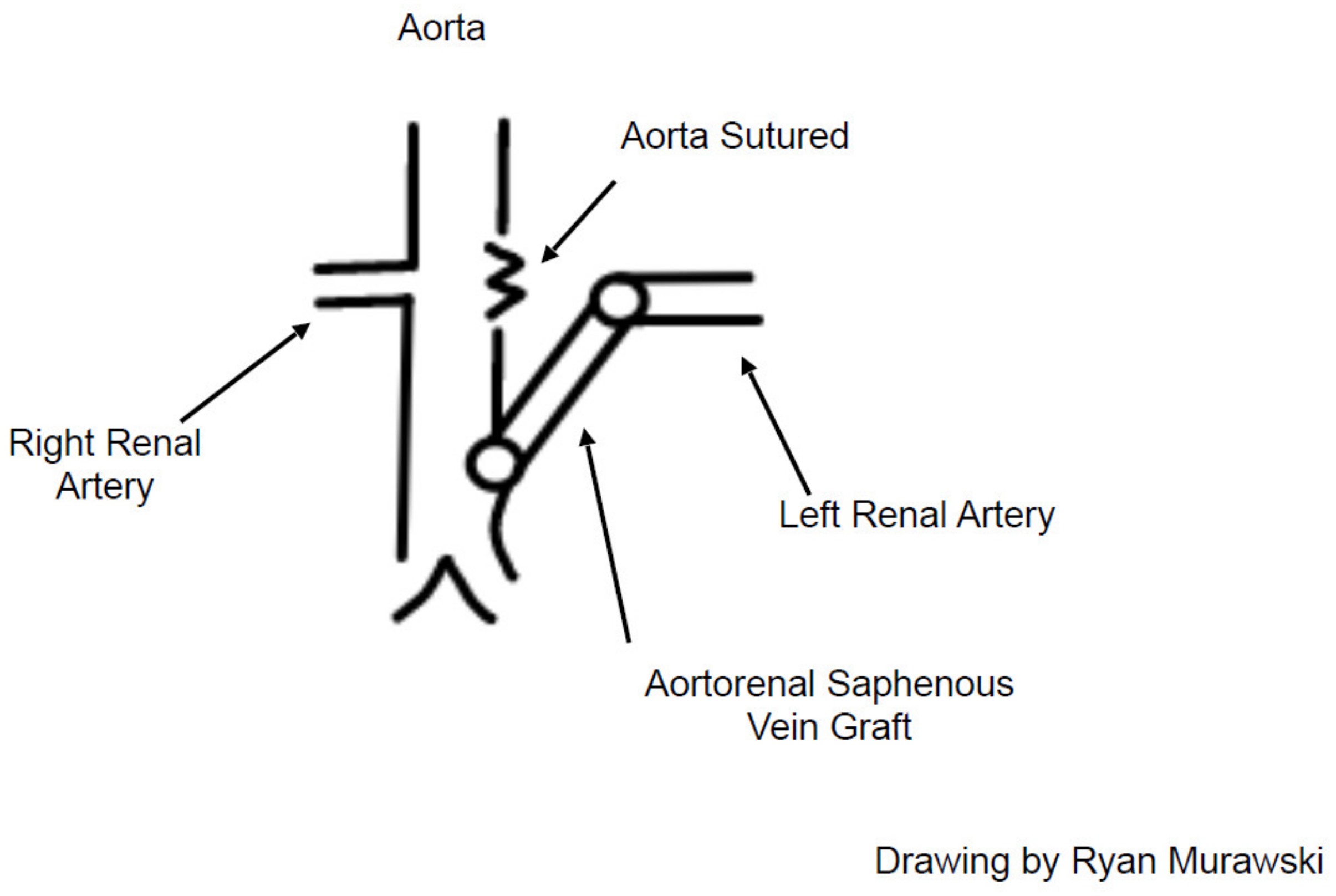
Left periaortic dissection revealed the left renal artery to be completely torn off and separated from the aorta. After discussion, as to the potential for renal salvage, the left groin was prepped, and the proximal six inches of the superficial femoral vein (proximal saphenous vein) were removed. The aortic defect was sutured with prolene and a reversed saphenous vein bypass was constructed between the distal aorta and the distal debrided left renal artery, after removing a half centimeter transection site clot, using 5–0 prolene sutures. This resulted in a good left renal artery pulsation (
Figure 2).
The lacerated bladder and partial cystouretheral disruption at the junction between the bladder and the proximal disrupted urethra was sutured, with interrupted absorbable sutures about the Foley catheter. The bladder was then repaired with running chronic sutures [
6]. Both a suprapubic and Foley catheter were retained in position for complete urinary drainage. Following further orthopedic stabilization in the operating room, the patient was transferred to the intensive care unit after five hours of surgery.
4. Results/Outcome
The treatment (
Table 2) of these multiple injury patients requires timely and appropriate intervention by multiple individuals including those at the accident scene, the emergency room staff, laboratory and X-ray accessibility, surgical facilities (OR room, nursing and physician staff), and the postoperative care units. When the patient is elderly and has serious intracranial injury, the prognosis is guarded. But in young healthy individuals with no or minimal intracranial injury, our goal and expectation is for possible survival with reasonable normal function—our hope and goal for this young man.
The family and all care givers planned for a functional young man. One could not predict such, but our goal would be such. We certainly felt his thoracic injuries were repairable with return to normal function. Would his abdominal surgery lead to a functional left kidney or normal bladder functions was not known, but certainly worth the effort. Dr. Stanley Crawford, an aortic surgeon, repeatedly stated, “Never throw a nephron away”. Could we predict salvage of the left kidney—no? However, if we did a nephrectomy, we knew all those nephrons would be lost.
5. Actual Outcome
Who could predict what the final result would be for this young man? Would he be able to self-care or walk or talk? We could not project. However now, after recovery and discharge from the hospital, the outcome was above all expectations—he could walk, talk, self-care, and have eventual normal functioning of both kidneys, and the urinary bladder—along with strong femoral artery pulsation.
6. Discussion
This patient was maintained for five weeks in the intensive care unit while his status stabilized. His renal function studies demonstrated only a mild elevation of the BUN and creatinine postoperatively (BUN 40 and creatinine 1.8), which returned to normal in a few days. Over the course of the next several weeks his orthopedic issues were aligned, operated, and repaired. His pulmonary infiltrates improved. He was eventually weaned off the respirator. His chest tubes were removed. Tube feedings were initiated during endotracheal intubation until he could take oral sustenance. The patient remained hospitalized for nearly three months while having corrective surgery and treatment of his various traumatic orthopedic injuries. In time, he was able to be up in a wheelchair and later walk with crutches.
After four months, the patient was discharged home from the hospital extended care unit for outpatient treatment with the Foley and percutaneous catheters in place. At the time of hospital discharge, he continued to demonstrate no function of the left renal system on intravenous pyelogram. However, on radioactive renal scan, the left renal system showed radioactive kidney uptake, perfusion to be present. Shortly thereafter, his Foley catheter was removed, and he was able to void his urine normally. The suprapubic catheter was clamped and, then, removed with no residual urinary leakage, nor undo retention. This normal function is not always the case with many other urinary bladder ruptures—such as with tumor or radiotherapy ruptures [
6]. At four months post injury, the patient was mobile and voiding without difficulty. A few weeks later, the patient had normal bilateral renal function demonstrated on IVP (intravenous pyelogram) of the right and left kidney. In addition, repeated blood BUN and creatinine studies were normal.
Renal function after trauma or post major surgery continues to be a concern. Past experience with the young and healthy individual who has received abdominal or retroperitoneal trauma, including to the kidneys, has cautioned us to be slow to perform nephrectomy. Patience and selective intervention has led to salvage of renal function in several of these trauma patients. Of importance, when the kidney has not been dissected, mobilized, or explored, there may be small capsular or other circulation routes that may maintain viability of the renal parenchyma. This patient is an example of such caution and exemplifies the desire to preserve nephrons. We did not, however, have evidence of accessory renal arteries at the aortic angiography in this hypotensive patient.
Renal artery trauma may lead to renal artery dissection, post traumatic renal artery thrombosis with complete renal infarction, renal artery aneurysm formation, or renal artery disruption—partial or complete [
7,
8]. When the renal artery dissection is incomplete, placement of a covered stent may be successful in multiple trauma patients [
9,
10]. However, in this patient, there was total separation of the aorta from the renal artery precluding a stent. Thus, the options were no renal surgery, nephrectomy (for which the urologist advocated), or the attempt of a salvage procedure—which was elected. Fortunately, the patient did not hemorrhage from the aortorenal orifice laceration, presumably due to the hypotension and avoidance of heparin usage for the thoracic aorta repair due to the multiple other injuries which could bleed due to heparin, including possible cerebral injuries [
11,
12]. We do believe that if we had dissected out the kidney, thus possibly eliminating collateral circulation, the chance of kidney salvage would have been less. Additionally, the renal artery outside the kidney was not thrombosed—only the trauma tip-which we felt was a positive finding.
Of importance, we have included a flow-chart outlining our care and treatment for this type of serious injury to further delineate his progress (
Table 3).
7. Conclusions
A 16-year-old male with multiple injuries, due to a vehicular accident, that included the left renal artery being torn off the aorta, a lacerated urinary bladder with a cystourethral injury, and multiple other systemic injuries including long bone fractures, thoracic aortic disruption, and a ruptured spleen, is presented. Following correction of the transected aorta and splenectomy, we directed our attention to the urinary system. Concern about his urinary system injuries, both short and long term function, required initial renal artery bypass, urinary bladder repair, and cystourethral catheters. The multiple surgical repairs provided the patient with the opportunity for eventual survival with normal urinary system function, along with a functional aortorenal and thoracic aortic bypass, and near normal ambulation.
Author Contributions
R.A.D.J. and G.B.K. were directly involved with the care and treatment of the patient, as well as the development and preparation of the manuscript, writing and completion. R.S.D. and R.A.D.III were involved in the concept, research, preparation and finalization of the manuscript—including the obtainment of references. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Patient consent was waived due to loss of patient contact.
Data Availability Statement
See reference libraries and computer sites for the topics.
Acknowledgments
We wish to acknowledge the efforts of the police, paramedics, emergency room staff, orthopedists, urologists, intensive care units and operating room staff, lab and X-ray staff, and all the others involved. Thank you!
Conflicts of Interest
There are no conflict of interest. No conflict of interest were present in his care or in the case preparation.
References
- Perumean, J.C.; Minei, J.P. Trauma of the aorta. In Diseases of the Aorta; Dieter, R.S., Dieter, R.A., Jr., Dieter, R.A., III, Eds.; Springer: Cham, Switzerland, 2019; Volume 29, pp. 397–414. [Google Scholar]
- Ahn, J.H.; Mores, A.F.; McAninch, J.W. Workup and management of traumatic hematuria. Emerg. Med. Clin. N. Am. 1998, 16, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Rehm, C.G.; Mure, A.J.; O’Malley, K.F.; Ross, S.E. Blunt traumatic bladder rupture: The role of retrograde cystogram. Ann. Emerg. Med. 1991, 20, 845–847. [Google Scholar] [CrossRef] [PubMed]
- Neil, J.A.; Laurent, D.; Das, K.; Mehta, H. Retrograde cysto-myelogram: Case report. Surg. Neurol. Int. 2015, 6 (Suppl. 3), S124. [Google Scholar] [CrossRef]
- Dieter, R.A., Jr.; Kuzycz, G.K.; Dieter, R.A., III; Leehey, D.J.; Walter, J.B.; Rahman, M.A. Aortourinary Fistula: Ureter/renal. In Diseases of the Aorta; Dieter, R.S., Dieter, R.A., Jr., Dieter, R.A., III, Eds.; Springer: Cham, Switzerland, 2019; Volume 23, pp. 349–353. [Google Scholar]
- Barnard, J.; Overholt, T.; Hajiran, A.; Crigger, C.; Jessop, M.; Knight, J.; Morley, C. Traumatic bladder ruptures: A ten-year review at a level 1 trauma center. Adv. Urol. 2019, 2019, 2614586. [Google Scholar] [CrossRef] [PubMed]
- Rozzanigo, U.; Luppi, G.; Gatti, F.; Donner, D.; Centonze, M.; Luciani, L. Traumatic renal artery dissection: From imaging to management. Clin. Radiol. 2021, 76, 153.e17–153.e24. [Google Scholar] [CrossRef] [PubMed]
- Bryniak, S.R.; Morales, A. Blunt trauma to renal artery. Urology 1976, 8, 379–381. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.T.; White, R.A. Endovascular management of blunt traumatic renal artery dissection. J. Endovasc. Ther. 2002, 9, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Best, I.M. Percutaneous repair of a disrupted left renal artery after rapid stabilization. Clin. Pract. 2011, 1, e116. [Google Scholar] [CrossRef] [PubMed]
- Clements, W.; Moriarty, H.K. Blunt renal vascular trauma resulting in arterial avulsion injury with a nephron-sparing outcome. J. Med. Imagin. Radial. Oncol. 2019, 63, 795–798. [Google Scholar] [CrossRef] [PubMed]
- Blecha, M.; Bunn, C.; Soult, M.; Gahtan, V. Thoracic aortic trauma: Who gets endovascular intervention and how to optimize outcomes. Endovasc. Today 2020, 19, 65–70. [Google Scholar]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).