Contrast Agent Mimicking Calculi in Entrapped Calyx. A Report of a Case
Abstract
:1. Introduction
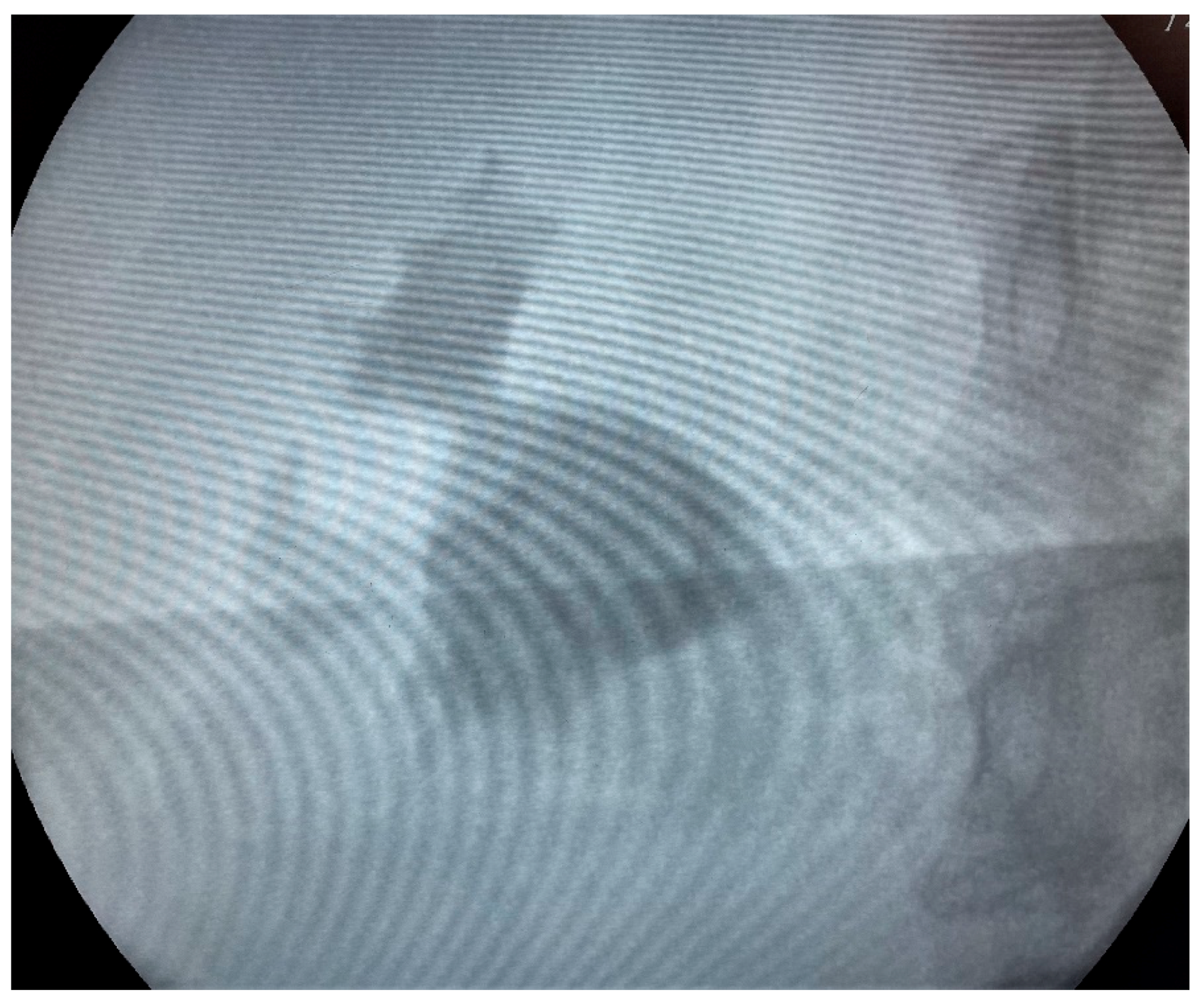
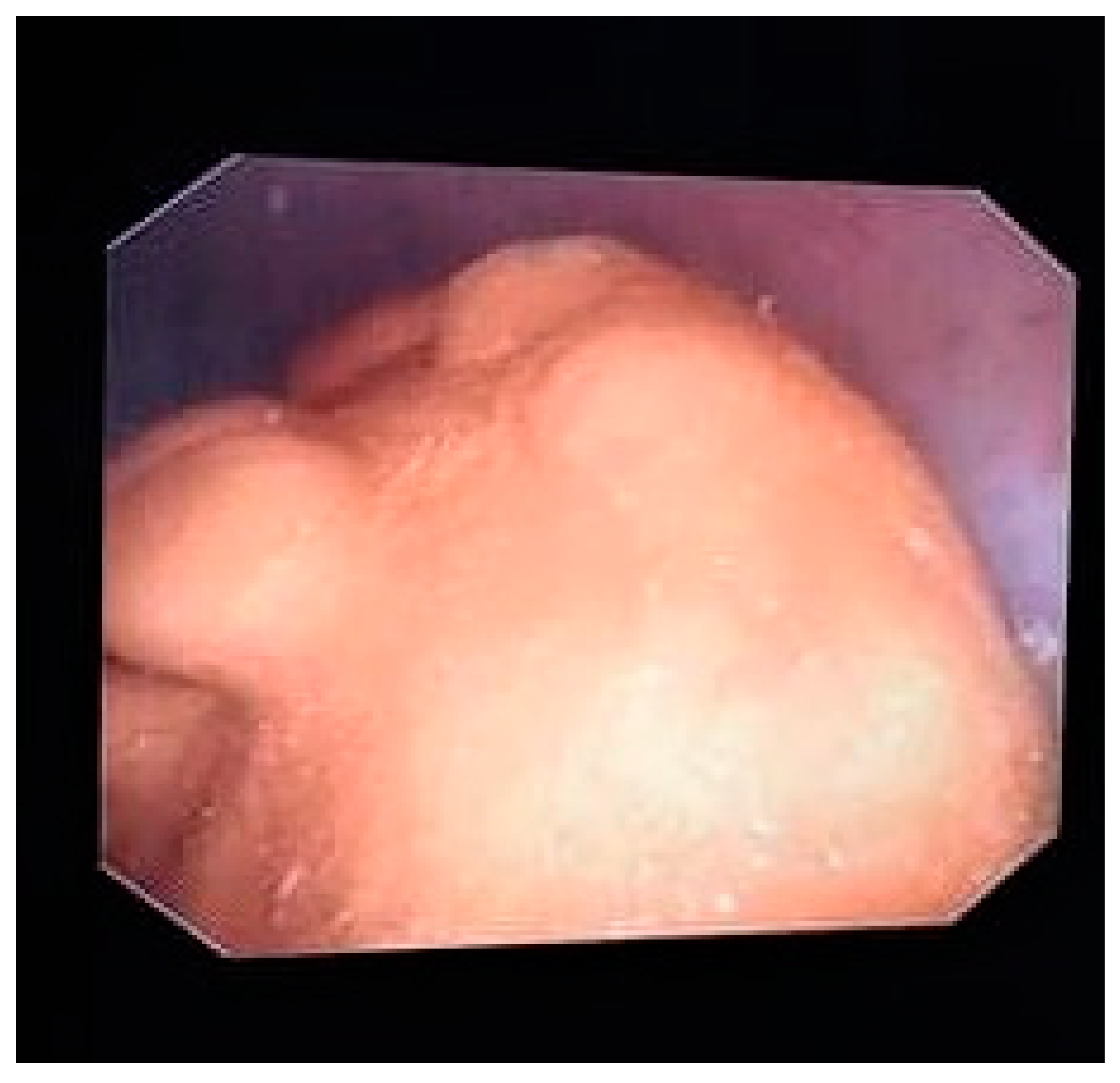
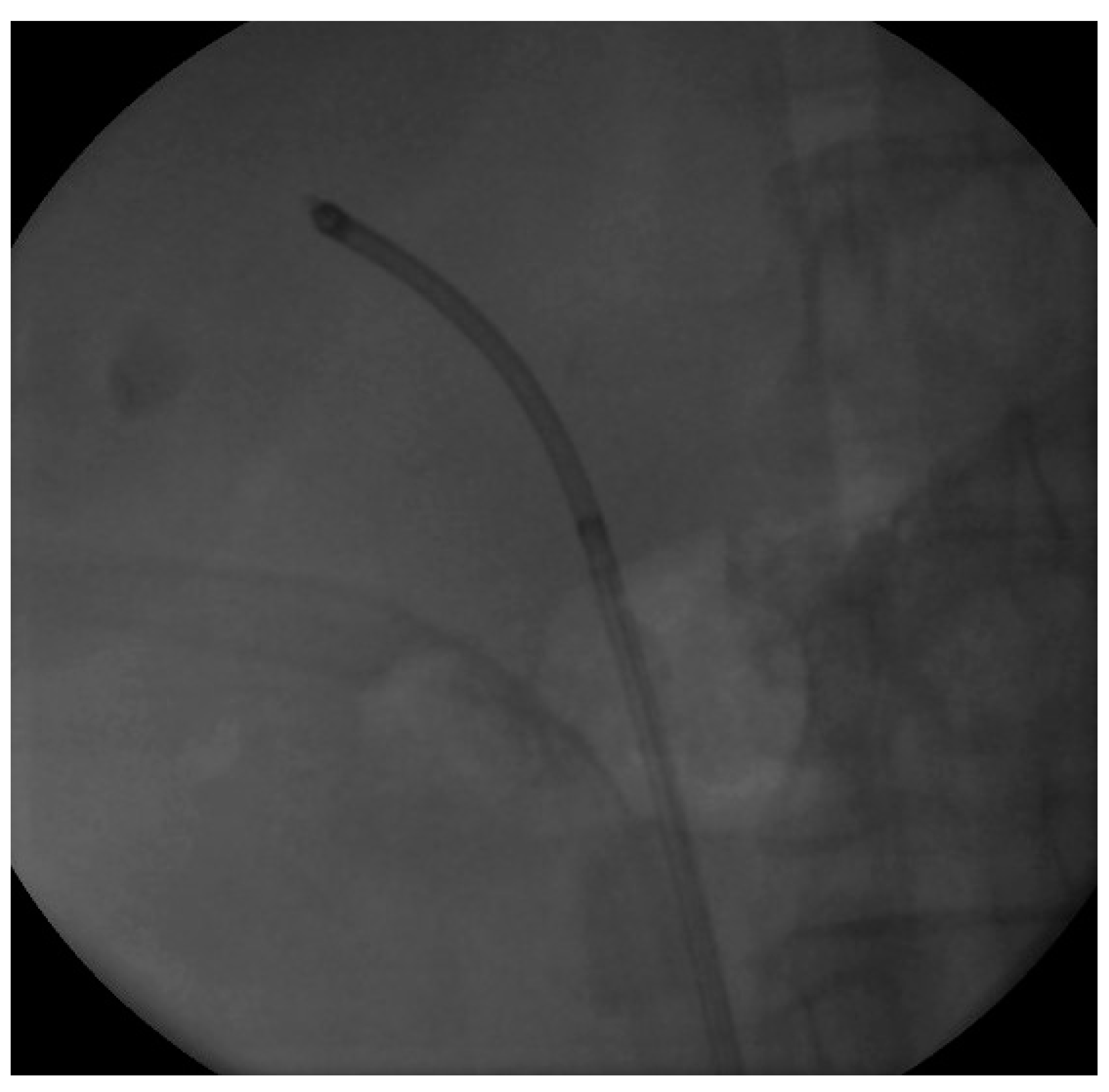
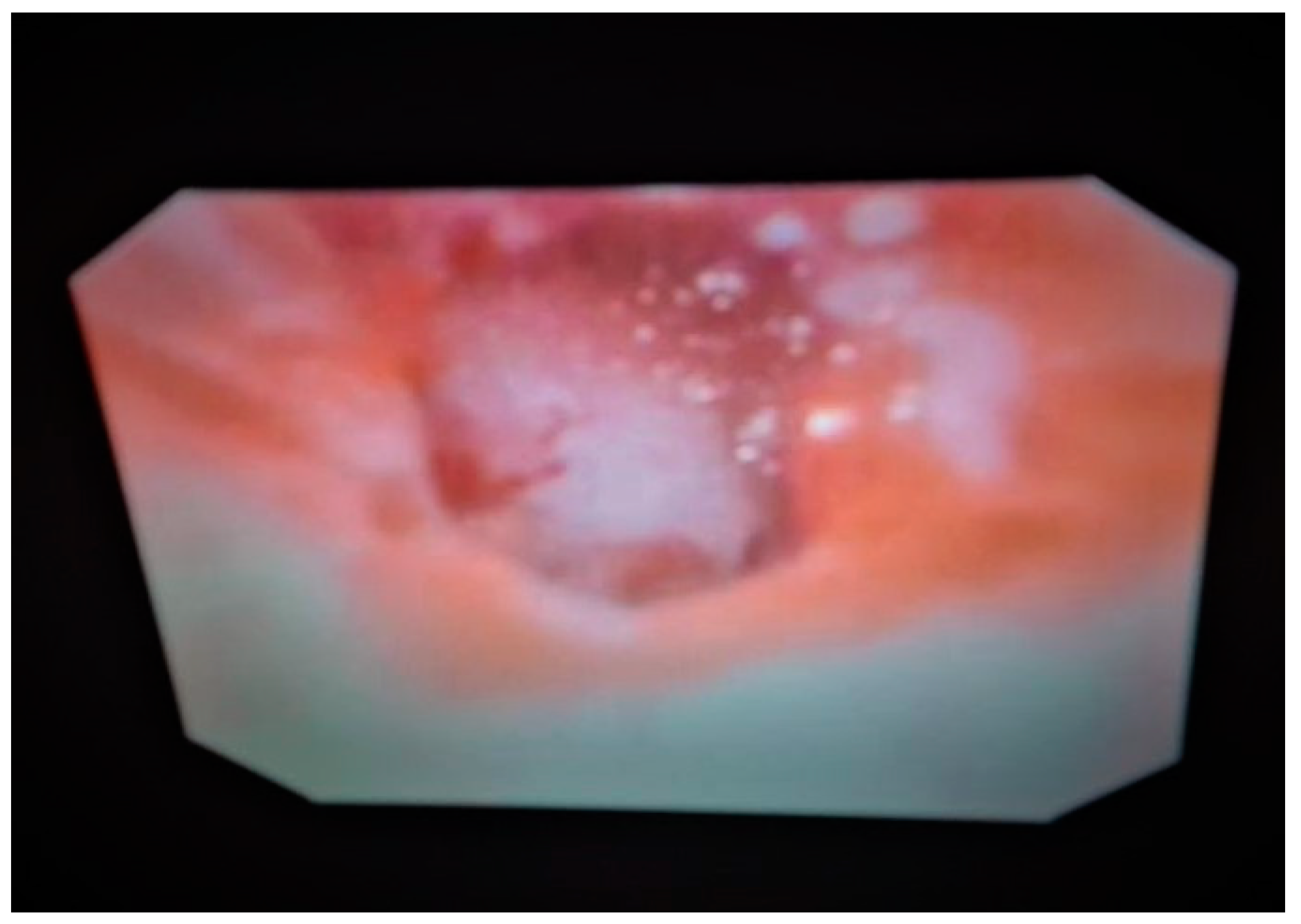
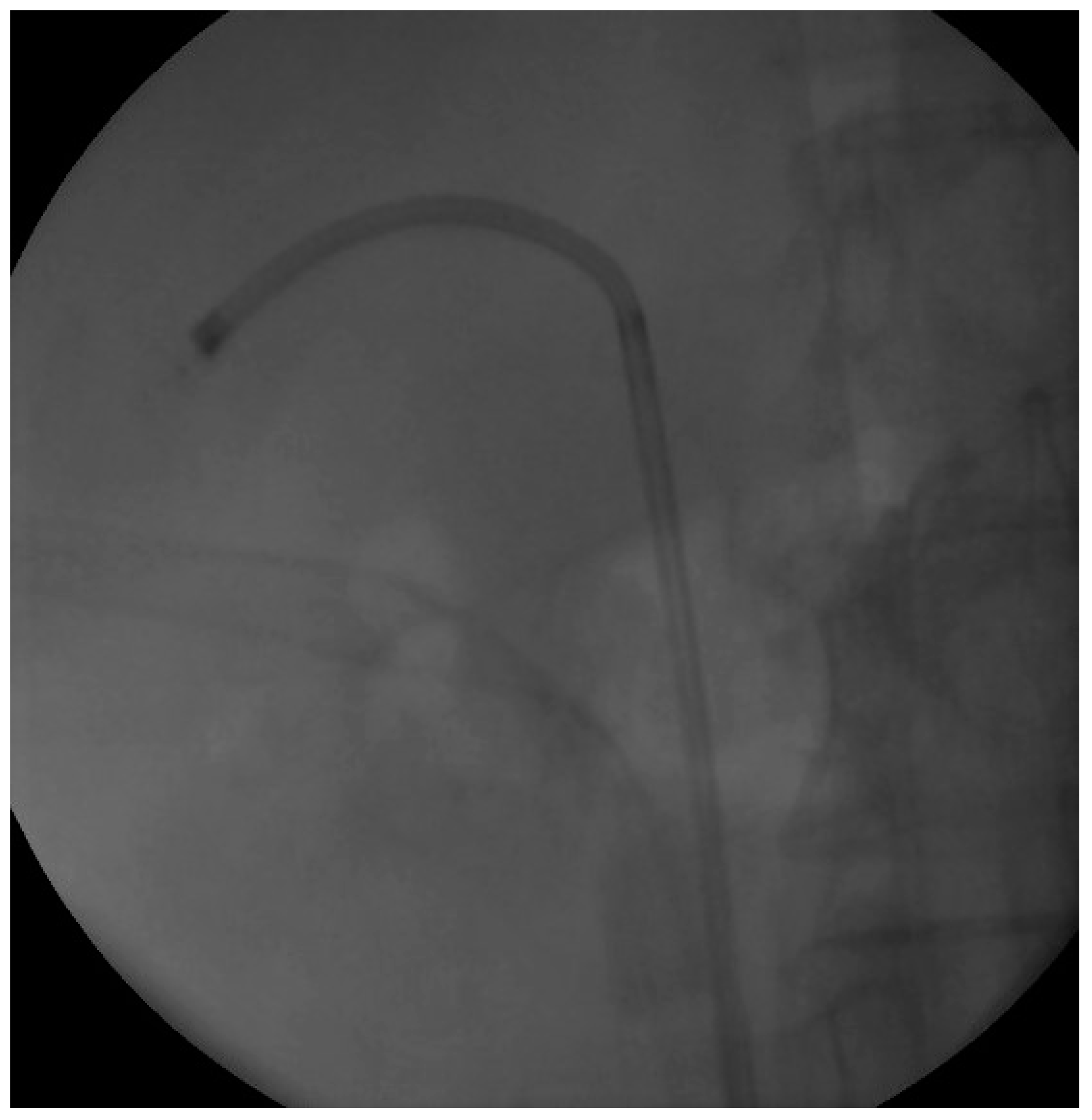
2. Case Presentation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Trinchieri, A. Epidemiology, in Stone Disease; Segura, C.P., Pak, C.Y., Preminger, G.M., Tolley, D., Eds.; Health Publications: Paris, France, 2003. [Google Scholar]
- Kılıç, Ö.; Akand, M.; Van Cleynenbreugel, B. Retrograde intrarenal surgery for renal stones—Part 2. Turk. J. Urol. 2017, 43, 252–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chung, M.J. Urolithiasis and nephrolithiasis. JAAPA 2017, 30, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Worster, A.; Preyra, I.; Weaver, B.; Haines, T. The accuracy of noncontrast helical computed tomography versus intravenous pyelography in the diagnosis of suspected acute urolithiasis: A meta-analysis. Ann. Emerg. Med. 2002, 40, 280. [Google Scholar] [CrossRef] [PubMed]
- Wendt-Nordahl, G.; Mut, T.; Krombach, P.; Michel, M.S.; Knoll, T. Do new generation flexible ureterorenoscopes offer a higher treatment success than their predecessors? Urol. Res. 2011, 39, 185. [Google Scholar] [CrossRef] [PubMed]
- Binbay, M.; Yuruk, E.; Akman, T.; Ozgor, F.; Seyrek, M.; Ozkuvanci, U.; Berberoglu, Y.; Muslumanoglu, A.Y. Is there a difference in outcomes between digital and fiberoptic flexible ureterorenoscopy procedures? J. Endourol. 2010, 24, 1929. [Google Scholar] [CrossRef] [PubMed]
- Geraghty, R.; Abourmarzouk, O.; Rai, B.; Biyani, C.S.; Rukin, N.J.; Somani, B. Evidence for Ureterorenoscopy and Laser Fragmentation (URSL) for Large Renal Stones in the Modern Era. Curr. Urol. Rep. 2015, 16, 54. [Google Scholar] [CrossRef] [PubMed]
- Uhlenhuth, E.; Amin, M.; Harty, J.I.; Howerton, L.W. Infundibulopelvic dysgenesis: A spectrum of obstructive renal disease. Urology 1990, 35, 334–337. [Google Scholar] [CrossRef]
- Dally, E.A.; Raman, A.; Webb, N.R.; Farnsworth, R.H. Unilateral multicystic dysplastic kidney with progressive infundibular stenosis in the contralateral kidney: Experience at 1 center and review of literature. J. Urol. 2011, 186, 1053–1058. [Google Scholar] [CrossRef] [PubMed]
- Nurzia, M.J.; Costantinescu, A.R.; Barone, J.G. Childhood infundibular stenosis. Urology 2002, 60, 344. [Google Scholar] [CrossRef]
- Wein, A.J.; Kavoussi, L.R.; Novick, A.C.; Partin, A.W.; Peters, C.A. Campbell-Walsh urology. In Normal Development of the Genitourinary Tract; Elsevier: New York, NY, USA, 2012; pp. 2975–3001. [Google Scholar]
- Koopman, S.G.; Fuchs, G. Management of stones associated with intrarenal stenosis: Infundibular stenosis and caliceal diverticulum. J. Endourol. 2013, 27, 1546–1550. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zervopoulos, G.; Venetsanos, F. Contrast Agent Mimicking Calculi in Entrapped Calyx. A Report of a Case. Uro 2021, 1, 238-244. https://doi.org/10.3390/uro1040026
Zervopoulos G, Venetsanos F. Contrast Agent Mimicking Calculi in Entrapped Calyx. A Report of a Case. Uro. 2021; 1(4):238-244. https://doi.org/10.3390/uro1040026
Chicago/Turabian StyleZervopoulos, Georgios, and Filippos Venetsanos. 2021. "Contrast Agent Mimicking Calculi in Entrapped Calyx. A Report of a Case" Uro 1, no. 4: 238-244. https://doi.org/10.3390/uro1040026
APA StyleZervopoulos, G., & Venetsanos, F. (2021). Contrast Agent Mimicking Calculi in Entrapped Calyx. A Report of a Case. Uro, 1(4), 238-244. https://doi.org/10.3390/uro1040026






