Urological Manifestations of the Systemic Vasculitides—A Scoping Review
Abstract
1. Introduction
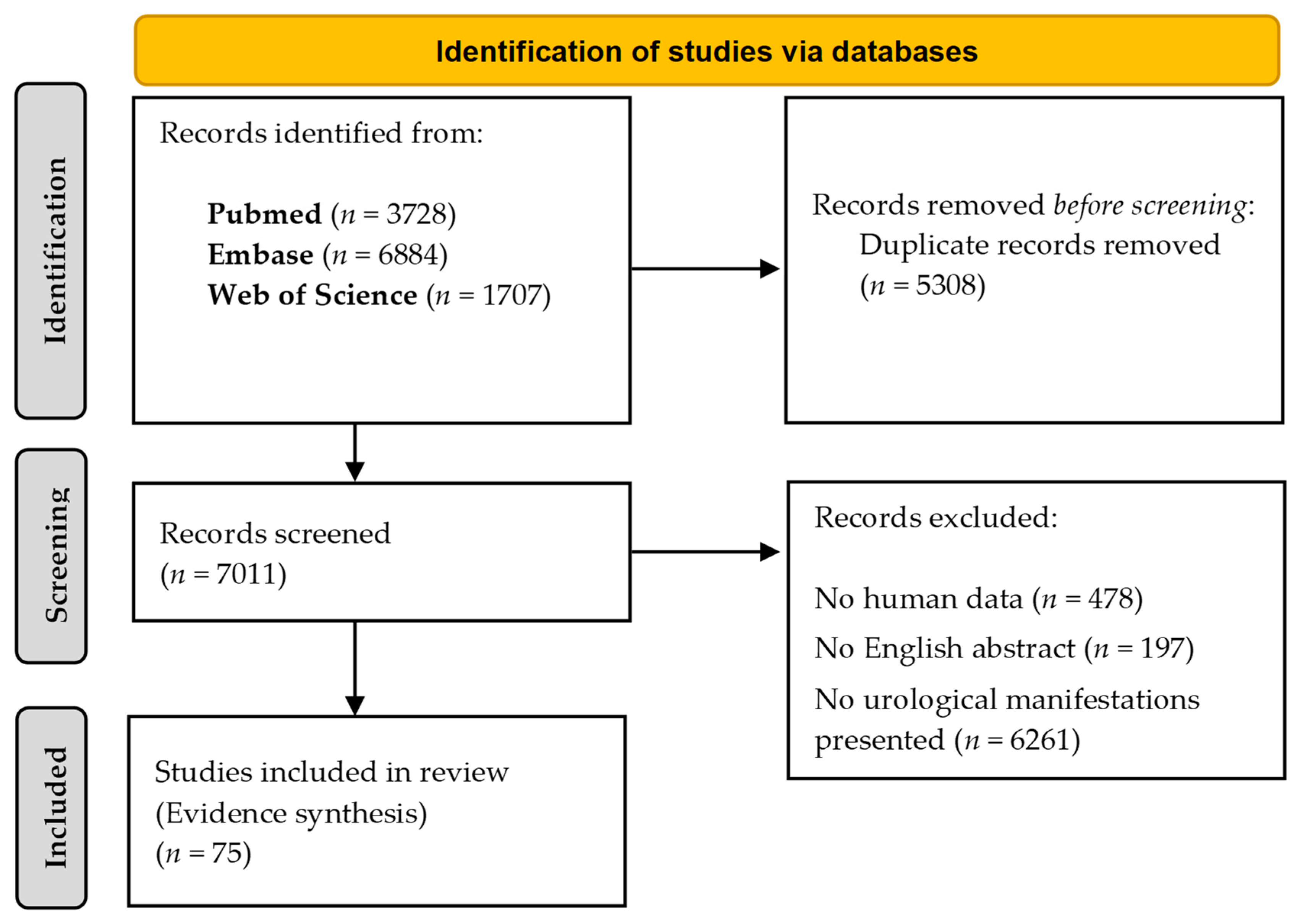
2. Evidence Acquisition
3. Evidence Synthesis
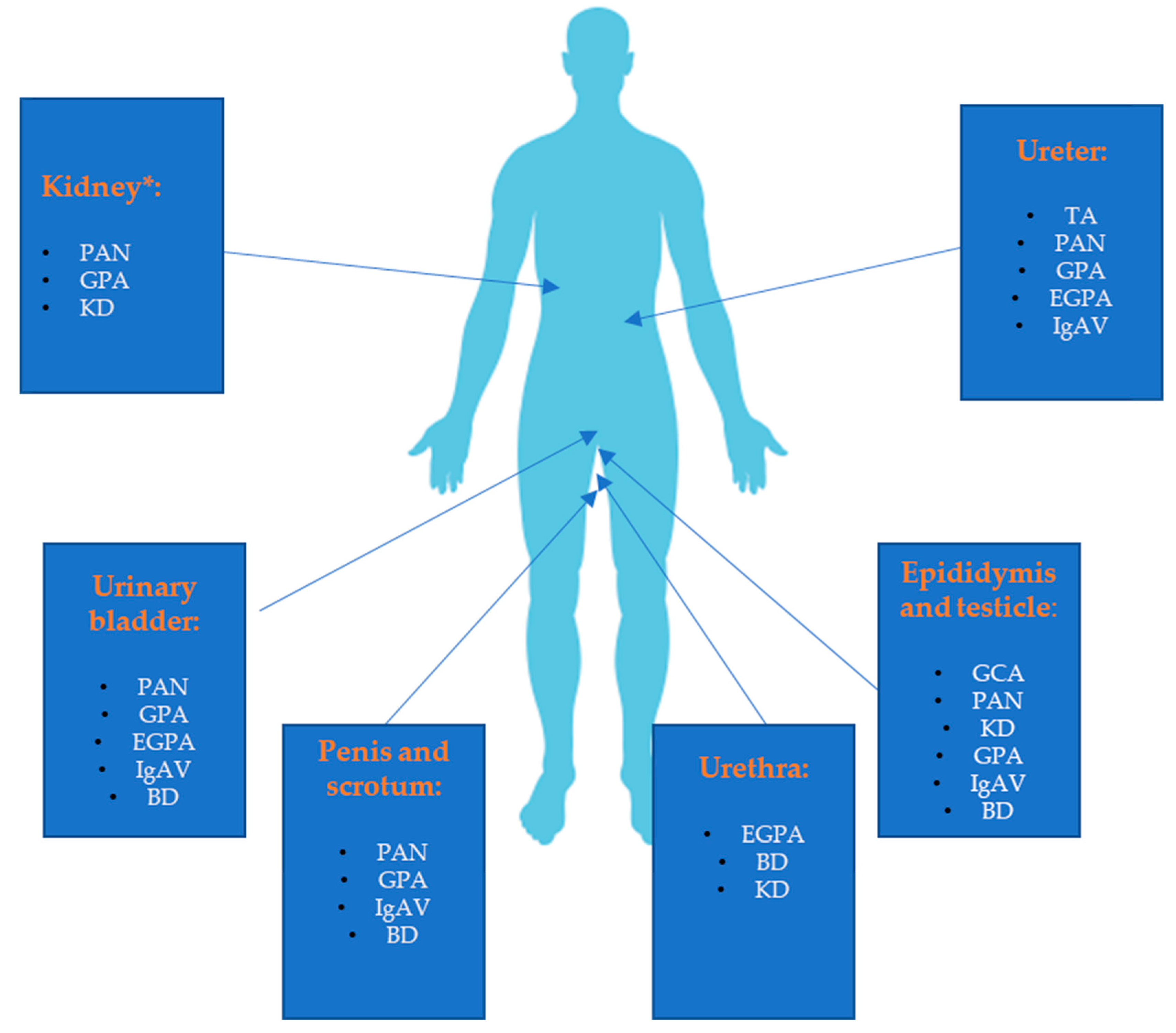
3.1. Large Vessel Vasculitides
3.1.1. Takayasu Arteritis (TA)
3.1.2. Giant Cell Arteritis (GCA)
3.2. Medium Vessel Vasculitides
3.2.1. Polyarteritis Nodosa (PAN)
3.2.2. Kawasaki Disease (KD)
3.3. Small Vessel Vasculitides
3.3.1. ANCA-associated Vasculitides
Granulomatosis with Polyangiitis (GPA)
Microscopic Polyangiitis (MPA)
Eosinophilic Granulomatosis with Polyangiitis (EGPA)
3.3.2. Small Vessels Vasculitides Associated with Immune Complex Deposition
Immunoglobulin A Vasculitis (IgAV)
Other Small Vessels Vasculitides Associated with Immune Complex Deposition
3.4. Variable Vessels Vasculitides
Behçet’s Disease (BD)
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khasnis, A.; Langford, C.A. Update on vasculitis. J. Allergy Clin. Immunol. 2009, 123, 1226–1236. [Google Scholar] [CrossRef] [PubMed]
- Jennette, J.C.; Falk, R.J.; Andrassy, K.; Bacon, P.A.; Churg, J.; Gross, W.L.; Hagen, E.C.; Hoffman, G.S.; Hunder, G.G.; Kallenberg, C.G.; et al. Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994, 37, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Jennette, J.C.; Falk, R.J.; Bacon, P.A.; Basu, N.; Cid, M.C.; Ferrario, F.; Flores-Suarez, L.F.; Gross, W.L.; Guillevin, L.; Hagen, E.C.; et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013, 65, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Elefante, E.; Bond, M.; Monti, S.; Lepri, G.; Cavallaro, E.; Felicetti, M.; Calabresi, E.; Posarelli, C.; Talarico, R.; Quartuccio, L.; et al. One year in review 2018: Systemic vasculitis. Clin. Exp. Rheumatol. 2018, 36 (Suppl. 111), 12–32. [Google Scholar] [PubMed]
- Bateman, H.; Rehman, A.; Valeriano-Marcet, J. Vasculitis-like Syndromes. Curr. Rheumatol. Rep. 2009, 11, 422–429. [Google Scholar] [CrossRef]
- Molloy, E.S.; Langford, C.A. Vasculitis mimics. Curr. Opin. Rheumatol. 2008, 20, 29–34. [Google Scholar] [CrossRef]
- Peracha, J. Urological manifestations and treatment of the primary systemic vasculitides. World J. Clin. Urol. 2015, 4, 5. [Google Scholar] [CrossRef]
- Jghaimi, F.; Kabbaj, A.; Essaadouni, L. Takayasu’s arteritis and retroperitoneal fibrosis: A case report. Rev. Med. Interne 2010, 31, e1–e3. [Google Scholar] [CrossRef]
- Houman, H.; Haouet, S.; Lamloum, M.; Ghorbel, I.B.; Miled, M. Retroperitoneal fibrosis associated with Takayasu arteritis. Ann. Med. Interne 1998, 149, 107–108. [Google Scholar]
- Arnillas, E.; de la Fuente, J.; Nunez, M.; Dominguez, F. Giant cell arteritis with epididymal involvement. Med. Clin. 2009, 132, 485. [Google Scholar] [CrossRef]
- Sundaram, S.; Smith, D.H. Giant cell arteritis mimicking a testicular tumour. Rheumatol. Int. 2001, 20, 215–216. [Google Scholar] [CrossRef]
- Figueiredo, C.; Amaral, M.; Rodrigues, É.; Silva, R.; Vilão, Ó. Paraneoplastic giant cell arteritis and prostate cancer: A case report of a not common association. Clin. Case Rep. 2021, 9, 1405–1407. [Google Scholar] [CrossRef] [PubMed]
- Teichman, J.M.; Mattrey, R.F.; Demby, A.M.; Schmidt, J.D. Polyarteritis nodosa presenting as acute orchitis: A case report and review of the literature. J. Urol. 1993, 149, 1139–1140. [Google Scholar] [CrossRef]
- Bhatia, S.; Herrera Hernandez, L.P.; Kamboj, A.K.; Rieck, K.M. Isolated Polyarteritis Nodosa Presenting as Bilateral Testicular Swelling. Am. J. Med. 2018, 131, e55–e56. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Marcotte, G.; Seidman, M.A.; Dehghan, N. Polyarteritis nodosa isolated to the testis and urinary bladder in the setting of cryptorchidism: A case report and literature review. J. Med. Case Rep. 2019, 13, 236. [Google Scholar] [CrossRef]
- Huisman, T.K.; Collins, W.T., Jr.; Voulgarakis, G.R. Polyarteritis nodosa masquerading as a primary testicular neoplasm: A case report and review of the literature. J. Urol. 1990, 144, 1236–1238. [Google Scholar] [CrossRef]
- Atis, G.; Memis, O.F.; Güngör, H.S.; Arikan, O.; Saglican, Y.; Caskurlu, T. Testicular polyarteritis nodosa mimicking testicular neoplasm. Sci. World J. 2010, 10, 1915–1918. [Google Scholar] [CrossRef]
- Gervaise, A.; Junca-Laplace, C.; Naulet, P.; Pernin, M.; Portron, Y.; Lapierre-Combes, M. Unilateral testicular vasculitis in polyarteritis nodosa mimicking a testicular torsion. Diagn. Interv. Imaging 2014, 95, 615–616. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pagnoux, C.; Seror, R.; Henegar, C.; Mahr, A.; Cohen, P.; Le Guern, V.; Bienvenu, B.; Mouthon, L.; Guillevin, L. Clinical features and outcomes in 348 patients with polyarteritis nodosa: A systematic retrospective study of patients diagnosed between 1963 and 2005 and entered into the French Vasculitis Study Group Database. Arthritis Rheum. 2010, 62, 616–626. [Google Scholar] [CrossRef] [PubMed]
- McKinnon, K.; Baker, K.; Ravi, R. Case of spontaneous bilateral perinephric hematomas. Int. J. Urol. Off. J. Jpn. Urol. Assoc. 2015, 22, 137–138. [Google Scholar] [CrossRef]
- Miyagawa, T.; Iwata, Y.; Oshima, M.; Ogura, H.; Sato, K.; Nakagawa, S.; Yamamura, Y.; Kitajima, S.; Toyama, T.; Hara, A.; et al. Polyarteritis nodosa with perirenal hematoma due to the rupture of a renal artery aneurysm. CEN Case Rep. 2021, 10, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Simsek, E.; Yilmaz, H.; Teke, K.; Uslubas, A.K.; Yuksekkaya, M. Spontaneous Retroperitoneal Haematoma due to Polyarteritis Nodosa: Report of a Case and Literature Review. Case Rep. Urol. 2016, 2016, 7592563. [Google Scholar] [CrossRef] [PubMed]
- Venkatramani, V.; Banerji, J.S. Spontaneous perinephric hemorrhage (Wunderlich syndrome) secondary to polyarteritis nodosa: Computed tomography and angiographic findings. Indian J. Urol. 2014, 30, 452–453. [Google Scholar] [CrossRef] [PubMed]
- Peddi, P.; Kalavakunta, J.K.; Annakula, M.; Armstrong, J.R. An unusual complication of polyarteritis nodosa with massive retroperitoneal hemorrhage: A case report. Int. Arch. Med. 2010, 3, 31. [Google Scholar] [CrossRef]
- Hachulla, E.; Bourdon, F.; Taieb, S.; Robert, Y.; Amrouni, N.; Steckolorom, T.; Jabinet, J.L.; Hatron, P.Y.; Devulder, B. Embolization of two bleeding aneurysms with platinum coils in a patient with polyarteritis nodosa. J. Rheumatol. 1993, 20, 158–161. [Google Scholar]
- Karademir, K.; Senkul, T.; Atasoyu, E.; Yildirim, S.; Nalbant, S. Ulcerative necrosis of the glans penis resulting from polyarteritis nodosa. J. Clin. Rheumatol. 2005, 11, 167–169. [Google Scholar] [CrossRef] [PubMed]
- Bolat, D.; Zumrutbas, A.E.; Baser, A.; Tuncay, L. Spontaneous ureteral rupture in a patient with polyarteritis nodosa. Int. Urol. Nephrol. 2016, 48, 223–224. [Google Scholar] [CrossRef]
- Grinstein, P.; Maximiliano, L.S.; Lucas, Y.; Norberto, B. Polyarteritis nodosa with genital necrosis. Urol. Case Rep. 2020, 33, 101285. [Google Scholar] [CrossRef]
- Wu, C.Y.; Hsieh, K.S.; Chiou, Y.H.; Wang, R.S.; Huang, I.F.; Lee, W.Y.; Chiou, C.C. Prolonged fever and pyuria: A urinary tract infection presentation of incomplete Kawasaki disease. Acta Paediatr. 2005, 94, 375–377. [Google Scholar] [CrossRef]
- Watanabe, T. Kidney and urinary tract involvement in kawasaki disease. Int. J. Pediatr. 2013, 2013, 831834. [Google Scholar] [CrossRef][Green Version]
- Kato, H.; Sugimura, T.; Akagi, T.; Sato, N.; Hashino, K.; Maeno, Y.; Kazue, T.; Eto, G.; Yamakawa, R. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation 1996, 94, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.; DeBartolo, M.; Darras, F.; Ferretti, J.; Wasnick, R. Renal Artery Pseudoaneurysm in Kawasaki Disease. Urology 2016, 98, 165–166. [Google Scholar] [CrossRef] [PubMed]
- Jibiki, T.; Sakai, T.; Saitou, T.; Kanazawa, M.; Ide, T.; Fujita, M.; Iida, Y.; Yamazaki, S.; Ishiwada, F.; Sato, J. Acute scrotum in Kawasaki disease: Two case reports and a literature review. Pediatr. Int. 2013, 55, 771–775. [Google Scholar] [CrossRef] [PubMed]
- Dufour, J.F.; Le Gallou, T.; Cordier, J.F.; Aumaitre, O.; Pinede, L.; Aslangul, E.; Pagnoux, C.; Marie, I.; Puechal, X.; Decaux, O.; et al. Urogenital manifestations in Wegener granulomatosis: A study of 11 cases and review of the literature. Medicine 2012, 91, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Neerhut, T.; Neerhut, G.; Magree, C. Rapidly recurrent prostatic obstruction due to granulomatosis with polyangiitis. Urol. Case Rep. 2021, 39, 101771. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Tang, S.H.; Sun, G.H.; Yu, C.P.; Jin, J.S.; Chang, S.Y. Limited Wegener’s granulomatosis of the epididymis and testis. Asian J. 2006, 8, 737–739. [Google Scholar] [CrossRef]
- Barber, T.D.; Al-Omar, O.; Poulik, J.; McLorie, G.A. Testicular infarction in a 12-year-old boy with Wegener’s granulomatosis. Urology 2006, 67, 846.E9–846.E10. [Google Scholar] [CrossRef]
- Hernandez-Rodriguez, J.; Tan, C.D.; Koening, C.L.; Khasnis, A.; Rodriguez, E.R.; Hoffman, G.S. Testicular vasculitis: Findings differentiating isolated disease from systemic disease in 72 patients. Medicine 2012, 91, 75–85. [Google Scholar] [CrossRef]
- Miller, D.C.; Koss, M.N. Wegener granulomatosis presenting as epididymitis. Urology 2009, 73, 1225–1226. [Google Scholar] [CrossRef]
- Hooda, D.; Parsons, J.; Hooda, S.; Nuss, M.; Layne, R. Isolated bladder vasculitis: A rare presentation of Wegener’s granulomatosis. W Va. Med. J. 2011, 107, 24–25. [Google Scholar]
- Hansen, B.J.; Horby, J.; Hansen, H.J. Wegener’s granulomatosis in the bladder. Br. J. Urol. 1990, 65, 108–109. [Google Scholar] [CrossRef] [PubMed]
- Davenport, A.; Downey, S.E.; Goel, S.; Maciver, A.G. Wegener’s granulomatosis involving the urogenital tract. Br. J. Urol. 1996, 78, 354–357. [Google Scholar] [CrossRef] [PubMed]
- Šoštarič, K.; Krstić, T.L.; Slanič, A.; Caf, P. A Rare Case of Granulomatosis With Polyangiitis Presenting as Retroperitoneal Fibrosis in the Peri-Iliac Region Causing Hydronephrosis. Cureus 2021, 13, e17295. [Google Scholar] [CrossRef]
- Suillot, J.; Bollmann, J.; Rotman, S.; Descombes, E. Bilateral Ureteral Stenosis with Hydronephrosis as First Manifestation of Granulomatosis with Polyangiitis (Wegener’s Granulomatosis): A Case Report and Review of the Literature. Case Rep. Nephrol. 2020, 2020, 7189497. [Google Scholar] [CrossRef] [PubMed]
- Lillaz, J.; Bernardini, S.; Algros, M.P.; Bittard, H.; Kleinclauss, F. Wegener’s granulomatosis: A rare cause of hydronephrosis. Case Rep. Med. 2011, 2011, 814794. [Google Scholar] [CrossRef] [PubMed]
- Sataa, S.; Ben Rhouma, S.; Tanguour, M.; Rebai, S.; Cherif, K.; Kchir, N.; Nouira, Y.; Benrais, N.; Horchani, A. Ureteral stenosis due to Wegener’s granulomatosis. Tunis Med. 2011, 89, 725–726. [Google Scholar] [PubMed]
- Anderson, P.T.; Gottheil, S.; Gabril, M.; Barra, L.; Power, N. Acute urinary retention secondary to urethral involvement of granulomatosis with polyangiitis. Can. Urol. Assoc. J. 2017, 11, E38–E40. [Google Scholar] [CrossRef]
- Al Rajabi, W.; Venturini, M.; Sala, R.; Calzavara-Pinton, P. Wegener’s granulomatosis of the penis: Genital presentation of systemic disease. Dermatology 2006, 212, 370–372. [Google Scholar] [CrossRef]
- Bories, N.; Becuwe, C.; Marcilly, M.C.; Wolf, F.; Balme, B.; Thomas, L. Glans penis ulceration revealing Wegener’s granulomatosis. Dermatology 2007, 214, 187–189. [Google Scholar] [CrossRef]
- Ward, A.; Konya, C.; Mark, E.J.; Rosen, S. Granulomatosis with polyangiitis presenting as a renal tumor. Am. J. Surg. Pathol. 2014, 38, 1444–1448. [Google Scholar] [CrossRef]
- Greco, A.; De Virgilio, A.; Rizzo, M.I.; Gallo, A.; Magliulo, G.; Fusconi, M.; Ruoppolo, G.; Tombolini, M.; Turchetta, R.; de Vincentiis, M. Microscopic polyangiitis: Advances in diagnostic and therapeutic approaches. Autoimmun. Rev. 2015, 14, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Ashikaga, E.; Iyoda, M.; Suzuki, H.; Nagai, H.; Shibata, T.; Akizawa, T. Case of microscopic polyangiitis presenting initially as prostatic vasculitis. Nihon Jinzo Gakkai Shi 2009, 51, 1075–1079. [Google Scholar] [PubMed]
- Lamarche, J.A.; Peguero, A.M.; Rosario, J.O.; Patel, A.; Courville, C. Anti-MPO small-vessel vasculitis causing prostatis and nephritis. Clin. Exp. Nephrol. 2007, 11, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Heers, H.; Ramaswamy, A.; Hofmann, R. A Case of Churg-Strauss Syndrome (Eosinophilic Granulomatosis with Polyangiitis) of the Urinary Bladder. Urology 2017, 108, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Famokunwa, B.; Ockrim, J.; Manson, J.J. Eosinophilic granulomatosis with polyangiitis presenting with a vesicovaginal fistula. Rheumatology 2017, 56, 1080. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kiyokawa, H.; Koyama, M.; Kato, H. Churg-Strauss syndrome presenting with eosinophilic prostatitis. Int. J. Urol. Off. J. Jpn. Urol. Assoc. 2006, 13, 838–840. [Google Scholar] [CrossRef]
- Raza, A.; Ong, E.K.; Palmer, T.; Bramwell, S.P. Churg-Strauss syndrome and eosinophilic prostatitis. BJU Int. 2003, 92 (Suppl. 3), e24–e25. [Google Scholar] [CrossRef]
- Symes, A.; Kalsi, V.; Rickards, D.; Allen, C.; Choong, S.; Philp, T. Dystrophic ureteral calcification associated with Churg-Strauss vasculitis. Urology 2004, 64, 1231. [Google Scholar] [CrossRef]
- Yagihashi, Y.; Toyosato, T.; Shimabukuro, S.; Kato, H. Bilateral calcified ureteral stricure requiring urinary reconstruction in eosinophilic granulomatosis with polyangitis: A case report. Nihon Hinyokika Gakkai Zasshi 2020, 111, 140–144. [Google Scholar] [CrossRef]
- Cortellini, P.; Manganelli, P.; Poletti, F.; Sacchini, P.; Ambanelli, U.; Bezzi, E. Ureteral involvement in the Churg-Strauss syndrome: A case report. J. Urol. 1988, 140, 1016–1018. [Google Scholar] [CrossRef]
- Walsh, I.; Loughridge, W.G.; Keane, P.F. Eosinophilic vasculitis (Churg-Strauss syndrome) involving the urethra. Br. J. Urol. 1994, 74, 255–256. [Google Scholar] [CrossRef]
- Fukui, S.; Iwamoto, N.; Mochizuki, Y.; Nakajima, H.; Abe, K.; Kawakami, A. Eosinophilic granulomatosis with polyangiitis along with funiculitis and myelitis. Int. J. Rheum. Dis. 2017, 20, 2203–2205. [Google Scholar] [CrossRef]
- Ha, T.S.; Lee, J.S. Scrotal involvement in childhood Henoch-Schonlein purpura. Acta Paediatr. 2007, 96, 552–555. [Google Scholar] [CrossRef]
- Gunes, M.; Kaya, C.; Koca, O.; Keles, M.O.; Karaman, M.I. Acute scrotum in Henoch-Schonlein purpura: Fact or fiction? Turk. J. Pediatr. 2012, 54, 194–197. [Google Scholar]
- Diana, A.; Gaze, H.; Laubscher, B.; De Meuron, G.; Tschantz, P. A case of pediatric Henoch-Schonlein purpura and thrombosis of spermatic veins. J. Pediatr. Surg. 2000, 35, 1843. [Google Scholar] [CrossRef]
- Sari, I.; Akar, S.; Secil, M.; Birlik, M.; Kefi, A.; Onen, F.; Celebi, I.; Akkoc, N. Thrombosis and priapism in a patient with Henoch-Schonlein purpura. Rheumatol. Int. 2005, 25, 472–474. [Google Scholar] [CrossRef]
- Bruce, R.G.; Bishof, N.A.; Jackson, E.C.; Skinker, D.M.; McRoberts, J.W. Bilateral ureteral obstruction associated with Henoch-Schoenlein purpura. Pediatr. Nephrol. 1997, 11, 347–349. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.M.; Ware, H.; Williams, G. Recurrent ureteric obstruction in association with Henoch-Schonlein purpura. Postgrad. Med. J. 1987, 63, 699–701. [Google Scholar] [CrossRef]
- Corbett, S.T.; Lennington, J.N.; Chua, A.N.; Gonzales, E.T., Jr. Stenosing ureteritis in a 7-year-old boy with Henoch-Schonlein purpura nephritis: A case report and review of the literature. J. Pediatr. Urol. 2010, 6, 538–542. [Google Scholar] [CrossRef]
- Siomou, E.; Serbis, A.; Salakos, C.; Papadopoulou, F.; Stefanidis, C.J.; Siamopoulou, A. Masked severe stenosing ureteritis: A rare complication of Henoch-Schonlein purpura. Pediatr. Nephrol. 2008, 23, 821–825. [Google Scholar] [CrossRef]
- Hirayama, T.; Matsumoto, K.; Tsuboi, T.; Fujita, T.; Satoh, T.; Iwamura, M.; Ao, T.; Baba, S. Anaphylactoid purpura after intravesical therapy using bacillus Calmette-Guerin for superficial bladder cancer. Hinyokika Kiyo 2008, 54, 127–129. [Google Scholar]
- Ishigaki, H.; Itou, H.; Takeshima, T.; Kawai, M.; Hirai, K.; Shirai, A.; Horita, A.; Saitou, I. Henoch-Schonlein purpura developed after radical cystectomy. Hinyokika Kiyo 2013, 59, 663–667. [Google Scholar] [PubMed]
- Sobieszczanska, M.; Tubek, S.; Poplicha, D.; Grabelus, A.; Pawelczak, J. Henoch-Schonlein purpura (HSP) and high-dose immunoglobulin treatment in patient with familiar prostatic adenocarcinoma. Hum. Vaccines Immunother. 2014, 10, 358–359. [Google Scholar] [CrossRef] [PubMed]
- Braun, G.S.; Horster, S.; Wagner, K.S.; Ihrler, S.; Schmid, H. Cryoglobulinaemic vasculitis: Classification and clinical and therapeutic aspects. Postgrad. Med. J. 2007, 83, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Buck, A.; Christensen, J.; McCarty, M. Hypocomplementemic urticarial vasculitis syndrome: A case report and literature review. J. Clin. Aesthet. Derm. 2012, 5, 36–46. [Google Scholar]
- Turan, Ç.; Karabulut, İ. An unusual localisation of genital ulcer in Behçet’s disease: External urethral meatus. Int. J. Clin. Pract. 2021, 75, e14504. [Google Scholar] [CrossRef]
- Kirkali, Z.; Yigitbasi, O.; Sasmaz, R. Urological aspects of Behcet’s disease. Br. J. Urol. 1991, 67, 638–639. [Google Scholar] [CrossRef]
- Horii, S.; Takada, S.; Kinjo, T.; Nonomura, D.; Yamamoto, Y.; Yoneda, S.; Nomura, H.; Tei, N.; Matsumiya, K.; Shiroyama, Y. Case of Behcet’s disease diagnosed by bilateral epididymitis. Hinyokika Kiyo 2014, 60, 593–596. [Google Scholar]
- Beddouche, A.; Ouaziz, H.; Zougaghi, S.; Alaoui, A.; Dergamoun, H.; El Sayegh, H.; Iken, A.; Benslimane, L.; Nouini, Y. Deep dorsal penile vein thrombosis revealing Behcet’s disease. Pan Afr. Med. J. 2016, 24, 17. [Google Scholar] [CrossRef]
- Akin, Y.; Yucel, S.; Baykara, M. An extremely rare manifestation of Behcet’s disease: Urethrovaginal fistula. Int. Urol. Nephrol. 2014, 46, 359–361. [Google Scholar] [CrossRef]
- Cetinel, B.; Akpinar, H.; Tufek, I.; Uygun, N.; Solok, V.; Yazici, H. Bladder involvement in Behcet’s syndrome. J. Urol. 1999, 161, 52–56. [Google Scholar] [CrossRef]
- Alizadeh, F.; Khorrami, M.H.; Izadpanahi, M.H.; Nouri-Mahdavi, K.; Mohammadi Sichani, M. Bladder involvement in Behcet’s disease. Urol. J. 2012, 9, 347–350. [Google Scholar] [PubMed]

| Type | Main Symptoms | Urological Manifestations |
|---|---|---|
| Large Vessel Vasculitis | ||
| Takayasu arteritis (TA) | Arthralgia, myalgia, carotidynia, absent or weak peripheral pulse, limb claudication, arterial bruit, discrepant blood pressure between arms, hypertension, angina, gastrointestinal symptoms (abdominal pain, diarrhea, gastrointestinal hemorrhage) skin lesions (erythema nodosum, pyoderma gangrenosum), respiratory symptoms (chest pain, dyspnea, hemoptysis, pulmonary hypertension), neurologic symptoms (light headedness, vertigo, syncope, orthostasis, headaches, convulsions, and strokes), visual impairment | Obstructive nephropathy |
| Giant cell arteritis (GCA) | Jaw claudication, ocular symptoms (transient visual loss, permanent vision loss, diplopia, Charles Bonnet syndrome), musculoskeletal symptoms (proximal polyarthralgias and myalgias, peripheral synovitis, distal extremity swelling with pitting edema), large vessel involvement (aneurysms and dissections of the aorta, stenosis, occlusion, and ectasia of large arteries), strokes | Epididymitis, orchitis, testicular masses |
| Medium Vessel Vasculitis | ||
| Polyarteritis nodosa (PAN) | Skin lesions (tender erythematous nodules, purpura, livedo reticularis, ulcers, bullous or vesicular eruption), neurologic symptoms (mononeuropathy multiplexor asymmetric polyneuropathy affecting, e.g., radial, ulnar, peroneal nerves), gastrointestinal symptoms (abdominal pain, nausea, vomiting, melena, bloody or non-bloody diarrhea, life-threatening gastrointestinal bleeding), coronary artery disease (myocardial ischemia, heart failure, cardiomyopathy), myalgia and muscle weakness, ocular symptoms (ischemic retinopathy with hemorrhages, retinal detachment, ischemic optic neuropathy), glomerulonephritis | Orchitis, scrotal necrosis, bladder and testicular masses, ureteric stricture, spontaneous ureteric rupture, renal artery aneurysms, perirenal hematomas, spontaneous retroperitoneal hemorrhage |
| Kawasaki disease (KD) | Conjunctivitis, mucositis, skin lesions (rash, perineal erythema, redness or crust formation at the site of Bacille Calmette–Guérin inoculation), extremity changes (indurated edema of the dorsum of their hands and feet, diffuse erythema of their palms and soles), arthritis, lymphadenopathy (cervical lymphadenopathy), cardiovascular involvement (coronary arteries inflammation, formation of microaneurysms, myocarditis, pericarditis, valvulitis) | Sterile pyuria, hydrocele testis |
| Small Vessel Vasculitis | ||
| Anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis | ||
| Microscopic polyangiitis (MPA) | Elevated purpura, alveolar hemorrhage, glomerulonephritis | Prostatitis |
| Granulomatosis with polyangiitis (GPA) | Upper airways, eye and ear disease (conductive hearing loss, sensorineural hearing loss, strawberry gingivitis, underlying bone destruction with loosening of teeth, non-specific ulcerations throughout the lining of the mouth and nasal septum), renal involvement (rapidly progressive glomerulonephritis), subglottal stenosis, lower respiratory tract involvement (pulmonary nodules, cavitary lesions, bleeding in the lungs, bronchial stenosis), arthritis, skin lesions (subcutaneous nodule on the elbow, purpura), neurologic symptoms: (sensory neuropathy, mononeuritis multiplex) | Prostatitis, epididymitis, orchitis, ureteric stricture, penile ulceration, necrotizing urethritis, large renal and bladder granulomas, vesicovaginal fistula |
| Eosinophilic granulomatosis with polyangiitis (EGPA) | Respiratory symptoms (asthma, allergic rhinitis, nasal polyps, pulmonary bleeding), neurologic symptoms (mononeuropathy multiplex, symmetrical polyneuropathy), renal involvement (glomerulonephritis, hypertension), cardiovascular involvement (myocarditis, pericarditis), skin lesions (elevated purpura, subcutaneous nodules, livedo reticularis), gastrointestinal symptoms (eosinophilic gastroenteritis, diarrhea, gastrointestinal bleeding, colitis) | Prostatitis, cystitis, ureteric stricture, vesicovaginal fistula |
| Immune complex small vessel vasculitides | ||
| IgA vasculitis (IgAV) | Skin lesions (symmetrical erythematosus petechial or purpuric rash that almost exclusively starts on the lower limbs and buttocks), arthritis, gastrointestinal symptoms (nausea, vomiting, colicky abdominal pain, transient paralytic ileus, gastrointestinal hemorrhage, bowel ischemia and necrosis, intussusception, bowel perforation), glomerulonephritis | Epididymitis, orchitis, ureteric stricture, cystitis, priapism, spermatic vein thrombosis |
| Variable Vessel Vasculitis | ||
| Bechet’s disease (BD) | Oral ulcerations, skin lesions (acneiform lesions, papulo-vesiculo-pustular eruptions, pseudofolliculitis, nodules, erythema, palpable purpura), ocular disease (uveitis, secondary cataracta, glaucoma, macular edema), neurologic symptoms, arterial disease (hemorrhage, stenosis, aneurysm formation), venous thrombosis, cardiac disease, gastrointestinal symptoms (abdominal pain, diarrhea, gastrointestinal ulcerations, bleeding) | Genital ulceration, epididymitis, sterile urethritis, bladder wall ulceration, cystitis, vesicovaginal fistula, urethrovaginal fistula, priapism |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowak, Ł.; Krajewski, W.; Krajewska, J.; Chorbińska, J.; Kiełb, P.; Małkiewicz, B.; Szydełko, T. Urological Manifestations of the Systemic Vasculitides—A Scoping Review. Uro 2021, 1, 209-221. https://doi.org/10.3390/uro1040023
Nowak Ł, Krajewski W, Krajewska J, Chorbińska J, Kiełb P, Małkiewicz B, Szydełko T. Urological Manifestations of the Systemic Vasculitides—A Scoping Review. Uro. 2021; 1(4):209-221. https://doi.org/10.3390/uro1040023
Chicago/Turabian StyleNowak, Łukasz, Wojciech Krajewski, Joanna Krajewska, Joanna Chorbińska, Paweł Kiełb, Bartosz Małkiewicz, and Tomasz Szydełko. 2021. "Urological Manifestations of the Systemic Vasculitides—A Scoping Review" Uro 1, no. 4: 209-221. https://doi.org/10.3390/uro1040023
APA StyleNowak, Ł., Krajewski, W., Krajewska, J., Chorbińska, J., Kiełb, P., Małkiewicz, B., & Szydełko, T. (2021). Urological Manifestations of the Systemic Vasculitides—A Scoping Review. Uro, 1(4), 209-221. https://doi.org/10.3390/uro1040023








