Abstract
(1) Background: The Adjustable Transobturator Male System (ATOMS) device is increasingly used to treat post-prostatectomy incontinence as it enhances residual urinary sphincteric function and allows continence recovery or improvement by dorsal compression of the bulbar urethra through a fixed transobturator mesh passage. The mode of action and the profile of the patients with best results are not totally understood. (2) Methods: Intraoperative urethral pressure measurements at different filling levels of the ATOMS device show increased urethral resistance and enhanced residual sphincteric activity. We evaluated whether the pattern of urethral pressure change secondary to serial progressive intraoperative filling of the cushion can predict postoperative results after ATOMS placement. (3) Results: The regression analysis showed a significant direct relationship between cushion volume and intraurethral pressure (p = 0.000). The median intraurethral pressure at atmospheric pressure was 51 ± 22.7 cm H2O, and at atmospheric pressure plus 4 mL was 80 ± 23.1 cm H2O). Cluster analyses defined a group of patients (n = 6) formed by patients with a distensible urethra and 100% continence after adjustment in contrast to another group (n = 3) with rigid urethras and 33% continence after adjustment. (4) Conclusions: As a part of its continence mechanism, the ATOMS device leads to continence by increasing intraurethral pressure owing to the stretching effect on the urethral wall caused by cushion filling that increases urethral resistance.
1. Introduction
Male stress urinary incontinence (SUI) is a distressful complication after prostatic surgery for either prostate cancer or benign prostatic hyperplasia. The Adjustable Transobturator Male System (ATOMS) is increasingly used for the surgical treatment of moderate to severe male SUI. This system is based on the ventral compression of the bulbar urethra exerted by a silicone cushion that can be filled both intraoperatively and postoperatively [1]. Compared to the artificial urinary sphincter (AUS), the ATOMS does not need patient manipulation. Other advantages of this system are its simplicity, the much lower risk of urethral atrophy or erosion, and the capability of postoperative adjustment [1,2,3]. There is accumulated evidence regarding both efficacy and safety of this incontinence device, without contraindication for the elderly and/or radiated population [4]. Currently, not only AUS, but also male slings and adjustable systems like ATOMS, are well-accepted therapies for male SUI [5].
The ATOMS device is also advantageous over other adjustable systems, both for a diminished rate of complications compared to the male REEMEX system [6] and also for increased effectiveness and durability compared to ProACT [7]. However, its mode of action is not well understood and analyses using urodynamic studies are scarce [8]. Our hypothesis is that the compression produced by the cushion filling produces a stretching effect on the bulbar urethra that increases urethral resistance and enhances the residual sphincteric activity, and also that the different responses to serial filling of the cushion intraoperatively after ATOMS placement could help to define the patients with the best postoperative results. Therefore, the objective of our study was to analyze the relationship between cushion volume and intraurethral pressure at the place of ATOMS contact. Our secondary objective was to evaluate whether a “stress test” performed intraoperatively could help us delineate the profile of a patient that would have the best chance of objective continence results after ATOMS implantation and postoperative adjustment.
2. Materials and Methods
We carried out a cross sectional study in nine consecutive male patients submitted to ATOMS placement for moderate and severe SUI. There were no exclusion criteria regarding leakage severity, concomitant radiotherapy, history of urethral stricture, or previous SUI surgery. Surgical technique and perioperative care followed the original description [1,3]. Sample size was calculated based on data published by Ito et al. [9]. Assuming that the standard deviation of maximum urethral pressure in adult men is 7.75 cm H2O with a precision of ±4 cm H2O and a confidence interval of 95%, the minimum sample size should be 7 patients. The study was IRB approved and all patients signed informed consent for inclusion in the study.
Perioperative intraurethral pressure measurement was carried out before and after ATOMS placement but before closing the incision, so that we could be sure the measurement was performed at the level at which the ATOMS device compresses the urethra (Figure 1). We measured this pressure by a T-DOC® air charged catheter inside the urethra at the point of contact between the ATOMS cushion and the urethra (Laborie, Mississaugua, ON, Canada), connected to Solar® urodynamic equipment (MMS, Enschede, the Netherlands). The system was calibrated before each measurement. The initial pressure was measured with an empty cushion, followed by 5 mL serial fillings until 30 mL was reached (Figure 2).
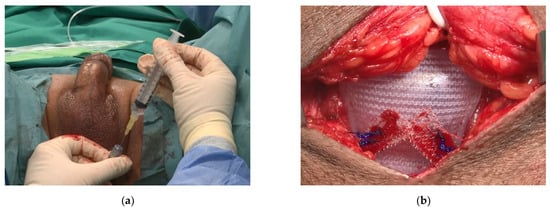
Figure 1.
Operative view at the time of the ATOMS implant with a T-DOC air charged urethral catheter to perform intraoperative urodynamics. (a) Controlled system filling of the port through a perineal incision; (b) the ATOMS cushion inflated with variable volumes caused a change in intraurethral pressures that were registered by urodynamic equipment.
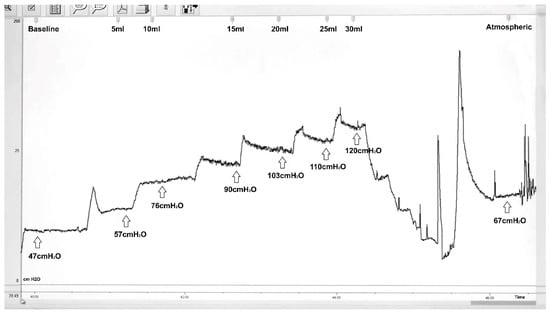
Figure 2.
Example of continuous intraoperative registry that corresponds to patient ID 281568. ATOMS progressive filling with 5 mL serial increment from baseline to 30 mL is followed by total deflation and refill up to atmospheric pressure (Atmospheric). Intraurethral pressure in cm H2O (Y-axis) and filling volume in ml (X axis) are specified at each time point in the graph. In this patient, ATOMS cushion at atmospheric pressure with 8 mL increased urethral pressure to 67 cm H2O.
Afterwards, the cushion was completely emptied, and filled again up to atmospheric pressure (slightly different in every case), determined by the anatomic position and the degree of pressing when the mesh arms were tied to the cushion. Finally, we measured the pressure by filling to atmospheric pressure plus an additional 4 mL. With each measurement, we observed that filling causes a peak of pressure followed by accommodation. All pressure data for each patient were tabulated. We blinded the clinical information of each patient regarding baseline characteristics including stress incontinence severity (daily pad test), former radiotherapy, and patient age during the registration of intraoperative measurements.
We carried out a regression analysis of filling cushion values on intraurethral pressures, and calculated the Pearson correlation coefficient between preoperative pad test, cushion volume, and intraurethral pressure. We also performed a multivariate cluster analysis to search for different filling and pressure patterns. Several months after surgery, once postoperative ATOMS adjustment was completed, we registered whether continence was achieved and the results of a postoperative pad test. Continence after adjustment, variables regarding incontinence severity baseline (pad count, pad test, ICIQ-SF with Q1-Q3 questions), and other clinical and preoperative urodynamic variables were evaluated. Their distribution according to the clusters identified was evaluated using Wilcoxon and chi2 tests.
3. Results
Table 1 shows each value of intraurethral pressure registered for every patient following the dynamic changes for each ATOMS cushion volume tested. We found that each patient followed a different pattern of pressure change and also that a great variation of pressure is exerted when the ATOMS filling exceeds 10 mL. Characteristically, 10 mL filling always increased urethral pressure beyond 60 cm H2O. Atmospheric pressure filling of the system led to intraurethral pressures in a range of 26–95 cm H2O (median 51 ± 22.7 cm H2O) and an additional 4 mL filling brought pressures to 45–110 cm H2O (median 80 ± 23.1 cm H2O). This is in agreement with the effects expected for ATOMS with a percentage of patients achieving continence after surgery and an additional population reaching continence after postoperative adjustment (i.e., adding some extra volume).

Table 1.
Intraurethral pressure in cm H2O at different filling volumes of ATOMS for each patient. Medians in last row in bold.
The regression analyses showed significant direct relationships between cushion volumes and intraurethral pressure (beta coefficient = 0.072 cm H2O/mL, p = 0.000). Intraurethral pressures increased mildly to moderately with filling under 15 mL (73 ± 22.7 cm H2O) but above 20 mL, there was a wide variability in the pressure increment (233 ± 108.9 cm H2O) (Figure 3).
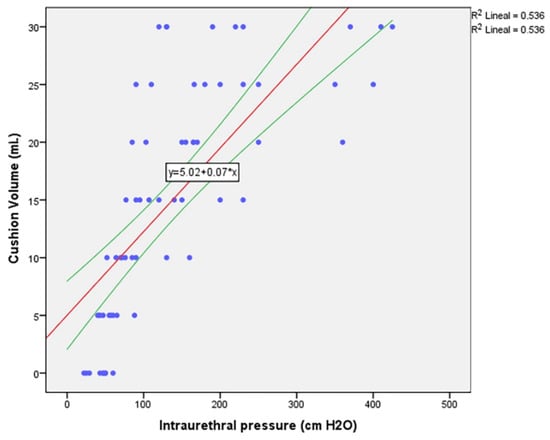
Figure 3.
Correlation between urethral pressure and ATOMS cushion volume.
There is a correlation between intraurethral pressure baseline with ATOMS placed unfilled and filled at atmospheric pressure (p = 0.038), and also between intraurethral pressure before ATOMS placement and with ATOMS placed and filled at atmospheric pressure plus 4 mL (p = 0.047). Additionally, a correlation was found between ATOMS filling to a medium-range volume (10 mL and 15 mL, p = 0.000; 15 mL and 20 mL, p = 0.004; 10 mL and 20 mL, p = 0.019) and also to a high-range volume (20 mL and 25 mL, p = 0.007; 25 mL and 30 mL, p = 0.003). These figures evidence that, although the pressure variation appears very variable, it can be determined by two ranges of volumes (i.e., 10–20 and 20–25 mL or beyond).
Cluster analysis distributed the nine patients in two different patterns (cluster 1 and 2). Cluster 1 is formed by six patients with distensible urethras, while cluster 2 is formed by three patients with more rigid urethras (Figure 4). Patients in cluster 2 reach higher pressure than the rest at 25–30 mL filling volume.
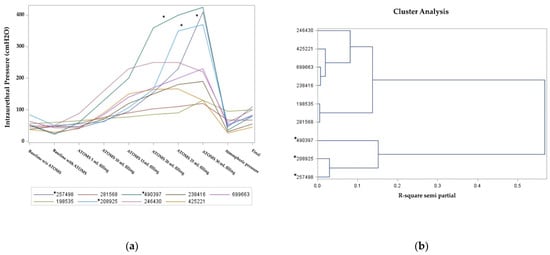
Figure 4.
Intraurethral pressure for different cushion volume: (a) Stress test performed for each patient, expressed as ID number; (b) cluster analysis distinguishes two different patterns of intraurethral pressure. Patients in cluster 2 are marked with asterisks.
The clinical characteristics that define each cluster, based on clinical and urodynamic characteristics, are evaluated in Table 2. All six patients in cluster 1 (100%) achieved continence, but only one patient in cluster 2 (33%) did so. Despite the small numbers, preoperative severity of incontinence was higher in patients in cluster 2, as revealed by a pad test, pad count, and also ICIQ-SF Question 1 (each p < 0.05).

Table 2.
Cluster characterization according to features expressed; significant values in bold.
Additionally, ultrasound images performed after ATOMS adjustment at different times for serial postoperative filling in a case needing progressive filling up to 25 mL show that ATOMS filling elongates the transversal urethral diameter whereas it reduces the antero-posterior diameter (Figure 5).
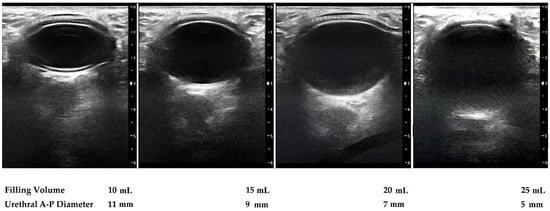
Figure 5.
Sonographic perineal evaluation with lineal probe shows urethral diameter (antero-posterior) diminishes with the increase in ATOMS filling volume.
4. Discussion
From a physiological point of view, intraurethral resting pressure must be adequate to maintain continence. Urethral pressure measurements have indicated that normal urethral resting pressure is 70 ± 7.75 cm H2O [9]. According to Laplace’s law, intraurethral pressure is proportional to the tension of its wall. This tension increases in direct proportion to the degree to which the wall is stretched [10]. This may be the mechanism by which ATOMS increases intraurethral pressure.
Tissue biomechanics inform us that the relationship between tension and stretch depends on the histologic composition of tissues. Elastin fibers and muscle tissues allow great deformations without a proportional boost of tension. These fibers have a high compliance. Other fibers like collagen allow initial deformation without a high tension. However, once they reach their working length, they strongly resist further stretching by sharply increasing their tension. Our cluster analysis confirms the existence of two patterns. We assume that the pattern in cluster 1 fits with normal urethras where elastin and muscle fibers are predominant and whose maximum intraoperative intraurethral pressure was 250 cm H2O; while the pattern in cluster 2 is formed by rigid urethras where collagen is predominant and maximum intraurethral pressure reached values of 425 cm H2O. In these urethras, overfilling does not guarantee continence status. This explains the finding previously reported that mean cushion filling in patients with ATOMS is higher in those who do not achieve continence than in continent patients [11]. The patients in cluster 2 are those with higher baseline SUI severity and also those with worst postoperative results (Table 2). In fact, clinical evidence with ATOMS implantation also confirmed that patients with higher SUI severity at baseline and patients who received prior radiation therapy are those with a lower possibility to achieve continence [2,4,11].
However, direct compression is most probably not the only factor through which ATOMS exerts its mode of action. In fact, an elastic urethra and corpus spongiosum allows the distribution of pressure to the membranous urethra, an explanation that is perfectly in line with our results.
Meta-analysis of outcomes reported for ATOMS reveals that 67% of the patients achieve continence after implantation and adjustment, and also that 90% improve their continence status [4]. Despite complications that may occur and possible pain after the implantation, which can hamper results in terms of patient satisfaction, overall satisfaction with the device remains very high [3,12,13]. Long-term outcomes appear reassuring as well [14], though a proportion of patients undergo device explantation for several reasons that include ineffectiveness, port erosion, and device infection [15,16].
The main cornerstone of male SUI therapy using prosthetic surgery is the identification of the best candidate for each device. In this sense, the study we present gives an idea of the mode of action of ATOMS as a sphincteric-reinforcing mechanism that produces ventral compression of the bulbar urethra to stretch its walls, thereby increasing intraurethral pressure. We have no clinical evidence that the effect exerted by ATOMS causes bladder outlet obstruction, at least from a clinical point of view. More studies assessing urodynamics after ATOMS placement are needed. Meanwhile, dynamic urethral pressure profiling can help distinguish the population of patients more likely to achieve the best postoperative results.
One of the main limitations of the study is the small number of cases evaluated. Another limitation is that repeat urethral pressure measurements were not performed after surgery, once postoperative adjustment was complete, to evaluate the pressure transmitted to the bulbar urethra once the fibrous capsule was formed around the ATOMS cushion. Additionally, future investigations should be conducted in larger series to better evaluate urodynamic changes caused by ATOMS in both the voiding and the filling phase in these patients.
5. Conclusions
We confirm the hypothesis that ATOMS leads to continence by increasing intraurethral pressure owing to the stretching effect on the urethral wall caused by ATOMS cushion filling, thus increasing urethral resistance. We have demonstrated that the response to serial filling performed intraoperatively depends on urethral rigidity, reflects baseline SUI severity, and predicts postoperative results.
6. Patents
The nine patients in this report signed an informed consent to participate in the study. All nine suffered incontinence after radical prostatectomy for prostate cancer. Three also received adjuvant radiotherapy. They were consecutive patients undergoing ATOMS placement in a university hospital between October 2019 and January 2020. The surgical team has intervened in more than 150 cases with ATOMS. Cystoscopy and urodynamic study were performed before ATOMS surgery. In one case, bladder outlet obstruction was confirmed despite previous endoscopic treatment of urethral stricture, but allowed urethral catheterization. Incontinence severity was evaluated by daily pad count, daily pad test (based on 3 consecutive days), and also a self-performed ICIQ-SF questionnaire, with three individual questions (Q1 dealing with urine leakage frequency from 0 to 5, Q2 dealing with incontinence severity from 0 to 6, and Q3 dealing with quality of life and patient discomfort).
The urethral pressure study was performed intraoperatively as described in the Materials and Methods section. Perioperative and postoperative care followed standards. ATOMS adjustment was performed by postoperative filling of the system through a silicone-covered scrotal port in five cases, with multiple filling needed in three of them. Seven achieved continence, defined by use of no pads or one security pad per day. No intraoperative or postoperative complications occurred.
Table 3 shows the most relevant clinical information for each patient included in the study regarding baseline SUI severity and other features like radiation and urethral stricture, operative data, and continence outcomes.

Table 3.
Clinical data of patients included in the study, including baseline, operative, and postoperative information.
All patients were followed for a year. Three patients suffered late complications. One patient had a device-related infection and it was explanted; another died of pneumonia related to COVID-19; and the third patient was diagnosed with superficial bladder cancer.
Author Contributions
Conceptualization, J.C.A. and M.V.-C.; methodology, M.V.-C.; validation, S.R., M.V.-C. and J.C.A.; formal analysis, J.C.A. and M.V.-C.; investigation, S.R., M.V.-C., F.Q., A.L., I.A. and J.C.A.; data curation, S.R. and A.L.; writing—original draft preparation, J.C.A. and M.V.-C.; writing—review and editing, S.R., F.Q., A.L. and I.A.; supervision, J.C.A.; project administration, J.C.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Hospital Universitario de Getafe, Madrid, Spain (protocol A02/20, finally approved 26 March 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent was obtained from the patients to allow publication of figures.
Data Availability Statement
Data supporting reported results will be provided by the corresponding author upon reasonable request.
Acknowledgments
We thank the patients participating in this study. We also thank Juan Dorado (PeRTICA statistical solutions) for statistical analysis; Xavier Genieser and Cristina Molina (Medicina y Mercado, MMS Laborie) for technical and instrumental support to perform the studies; and José Domínguez Pallas (Fotografía y Documentación Clínica, Hospital Universitario de Getafe, Madrid, Spain) for the iconographic support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Seweryn, J.; Bauer, W.; Ponholzer, A.; Schramek, P. Initial experience and results with a new adjustable transobturator male system for the treatment of stress urinary incontinence. J. Urol. 2012, 187, 956–961. [Google Scholar] [CrossRef] [PubMed]
- Friedl, A.; Mühlstädt, S.; Zachoval, R.; Giammò, A.; Kivaranovic, D.; Rom, M.; Fornara, P.; Brössner, C. Long-term outcome of the adjustable transobturator male system (ATOMS): Results of a European multicentre study. BJU Int. 2017, 119, 785–792. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Arance, I.; Esquinas, C.; Dorado, J.F.; Marcelino, J.P.; Martins, F.E. Outcome measures of Adjustable Transobturator Male System with pre-attached scrotal port for male stress urinary incontinence after radical prostatectomy: A prospective study. Adv. Ther. 2017, 34, 1173–1183. [Google Scholar] [CrossRef] [PubMed]
- Esquinas, C.; Angulo, J.C. Effectiveness of Adjustable Transobturator Male System (ATOMS) to treat male stress incontinence: A systematic review and meta-analysis. Adv. Ther. 2019, 36, 426–441. [Google Scholar] [CrossRef] [PubMed]
- Esquinas, C.; Ruiz, S.; de Sancha, E.; Vazquez, M.; Dorado, J.F.; Virseda, M.; Arance, I.; Angulo, J.C. Outcomes of a series of patients with post-prostatectomy incontinence treated with an adjustable transobturator male system or artificial urinary sphincter. Adv. Ther. 2021, 38, 678–690. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Ruiz, S.; Lozano, M.; Arance, I.; Virseda, M.; Lora, D. Systematic review and meta-analysis comparing Adjustable Transobturator Male System (ATOMS) and male Readjustment Mechanical External (REMEEX) system for post-prostatectomy incontinence. World J. Urol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Schönburg, S.; Giammò, A.; Abellán, F.J.; Arance, I.; Lora, D. Systematic review and meta-analysis comparing Adjustable Transobturator Male System (ATOMS) and Adjustable Continence Therapy (ProACT) for male stress incontinence. PLoS ONE 2019, 14, e0225762. [Google Scholar] [CrossRef] [PubMed]
- Virseda-Chamorro, M.; Ruiz, S.; García, G.; Queissert, F.; Salinas, J.; Arance, I.; Angulo, J.C. Do voiding urodynamic parameters predict the success of adjustable transobturator male system (ATOMS) to treat postprostatectomy urinary incontinence? Neurourol. Urodyn. 2020, 39, 1746–1752. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Sakakibara, R.; Uchiyama, T.; Zhi, L.; Yamamoto, T.; Hattori, T. Videomanometry of the pelvic organs: A comparison of the normal lower urinary and gastrointestinal tracts. Int. J. Urol. 2006, 13, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Zinner, N.R.; Ritter, R.C.; Sterling, A.M.; Donker, P.J. The physical basis of some urodynamic measurements. J. Urol. 1977, 117, 682–689. [Google Scholar] [CrossRef]
- Angulo, J.C.; Cruz, F.; Esquinas, C.; Arance, I.; Manso, M.; Rodríguez, A.; Pereira, J.; Ojea, A.; Carballo, M.; Rabassa, M.; et al. Treatment of male stress urinary incontinence with the adjustable transobturator male system: Outcomes of a multi-center Iberian study. Neurourol. Urodyn. 2018, 37, 1458–1466. [Google Scholar] [CrossRef] [PubMed]
- Mühlstädt, S.; Angulo, J.C.; Mohammed, N.; Schumann, A.; Fornara, P. Complications of the urinary incontinence system ATOMS: Description of risk factors and how to prevent these pitfalls. World J. Urol. 2020, 38, 1795–1803. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Arance, I.; Ojea, A.; Carballo, M.; Rodríguez, A.; Pereira, J.; Rebassa, M.; Teyrouz, A.; Escribano, G.; Teba, F.; et al. Patient satisfaction with adjustable transobturator male system in the Iberian multicenter study. World J. Urol. 2019, 37, 2189–2197. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Virseda-Chamorro, M.; Arance, I.; Ruiz, S.; Ojea, A.; Carballo, M.; Rodríguez, A.; Pereira, J.; Teyrouz, A.; Rebassa, M.; et al. Long-term outcome of adjustable transobturator male system for stress urinary incontinence in the Iberian multicentre study. Neurourol. Urodyn. 2020, 39, 1737–1745. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Schönburg, S.; Giammò, A.; Queissert, F.; Gonsior, A.; González-Enguita, C.; Martins, F.E.; Rourke, K.; Cruz, F. Artificial urinary sphincter or a second adjustable transobturator male system offer equivalent outcomes in patients whom required revision on the initial ATOMS device: An international multi-institutional experience. Neurourol. Urodyn. 2021, 40, 897–909. [Google Scholar] [CrossRef] [PubMed]
- Angulo, J.C.; Rourke, K.; Queissert, F.; Giammò, A.; Schönburg, S.; Cruz, F.; Martins, F.E.; Gonsior, A.; González-Enguita, C. Adjustable transobturator male system (ATOMS) infection: Causative organisms and clinical profile. Urology 2021, in press. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).