Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease: From “One Size Fits All” to a Multidisciplinary-Tailored Approach
Abstract
1. Background
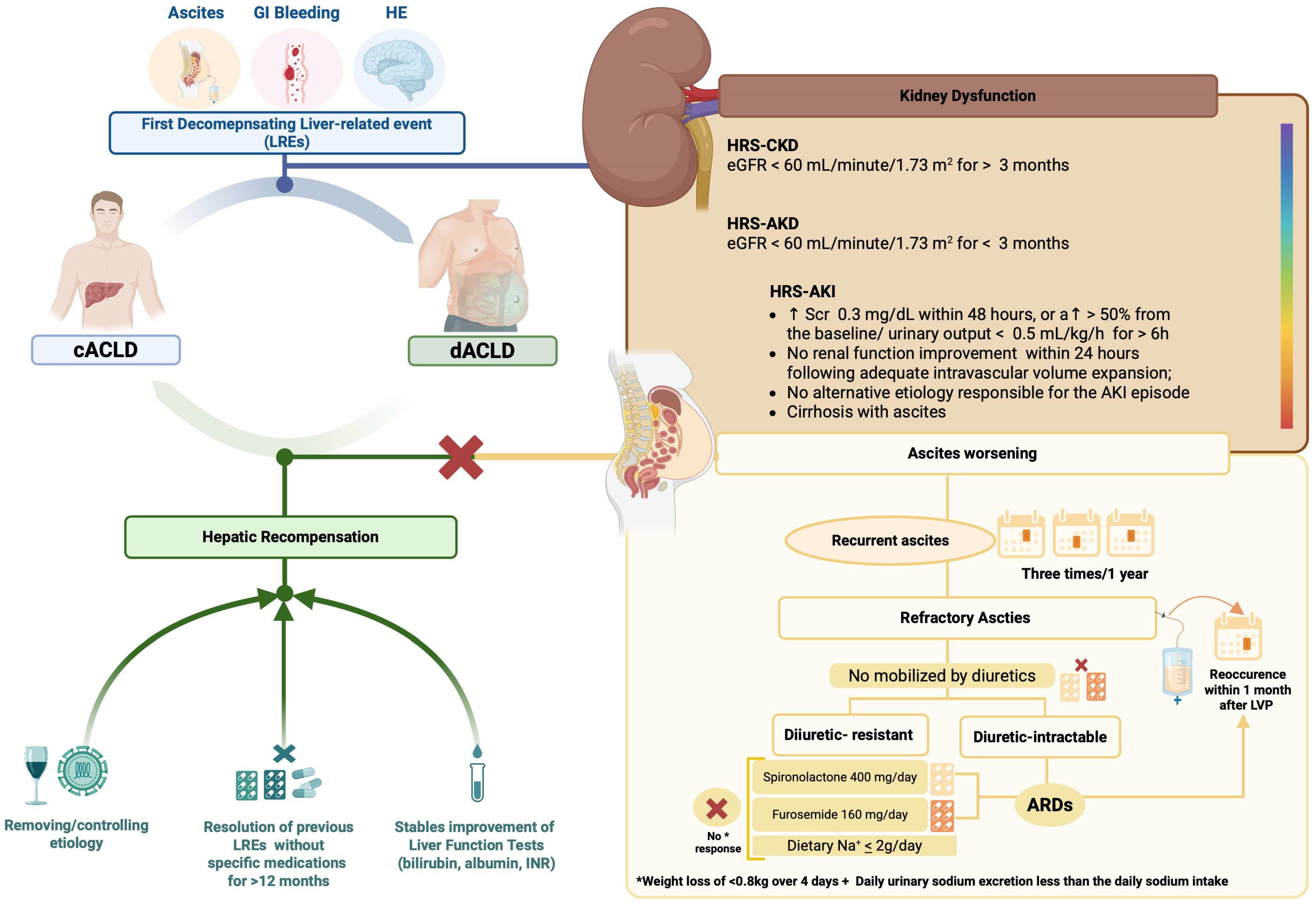
1.1. Hepatic Recompensation: Revolutionizing the “Irreversibility” in Advanced Chronic Liver Disease
1.2. Exploring Refractory Ascites: When Hepatic Recompensation Remains Utopian
1.3. Kidney Dysfunction and Ascites in Decompensated Advanced Chronic Liver Disease
1.4. Kidney Dysfunction and Ascites in Acute-on-Chronic Liver Failure (ACLF)
1.5. Aim of the Present Research
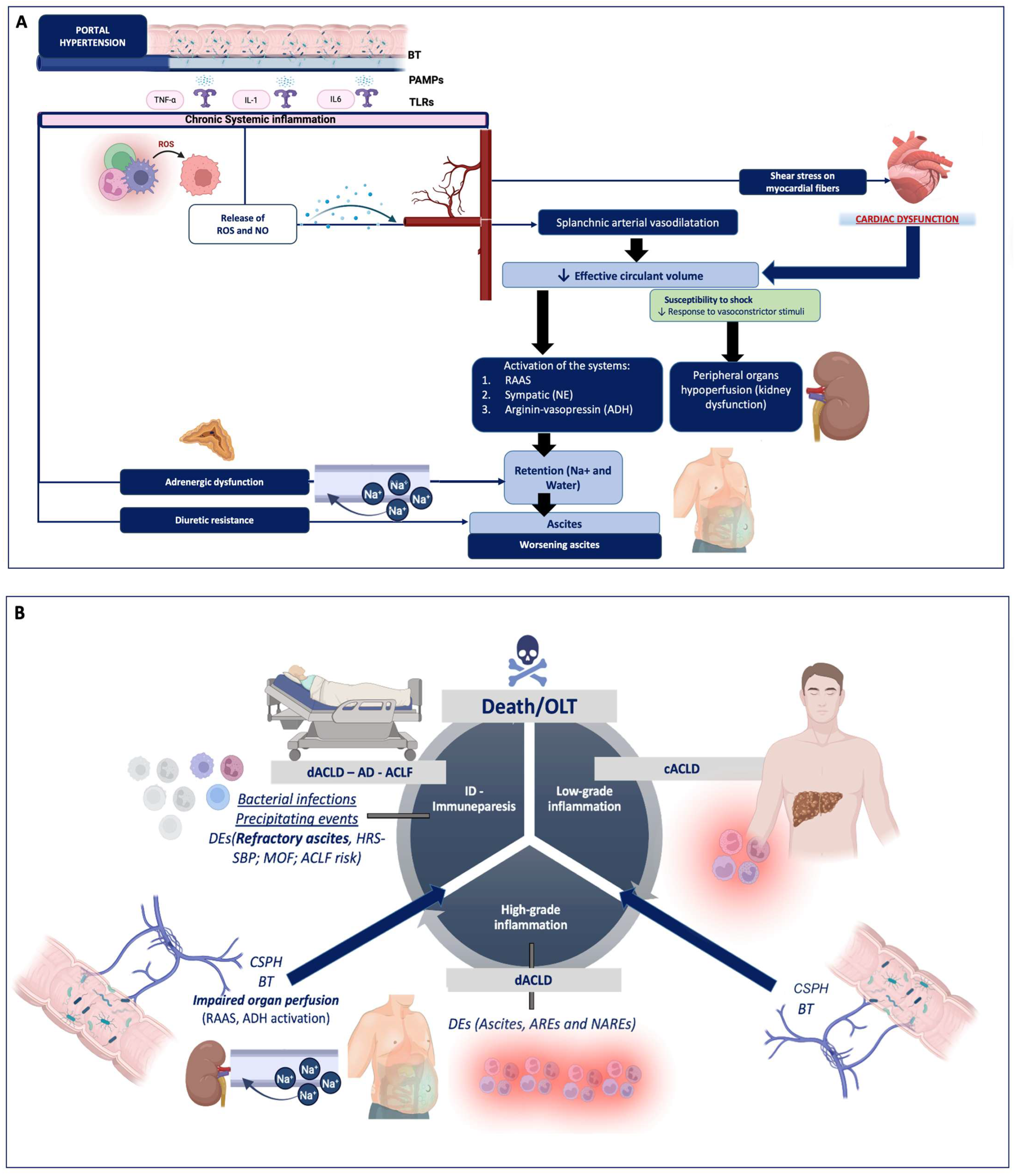
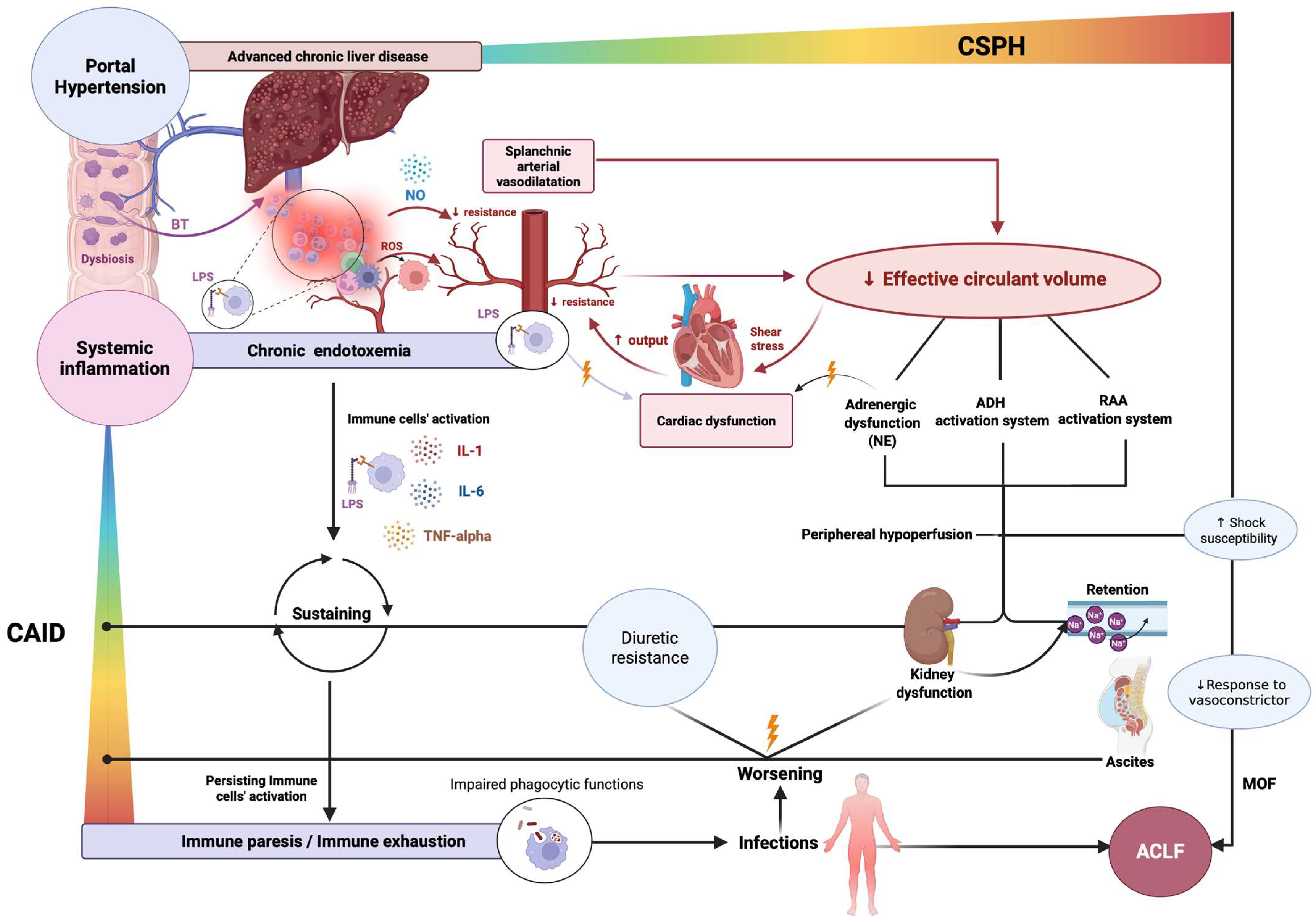
2. Overweening Physiopathology of Ascites and Kidney Dysfunction
2.1. From “Classic” Peripheral Arterial Dilatation to the Novel “Cirrhosis-Associated Immune Dysfunction (CAID)” Theory
2.2. Systemic Inflammation: One Shared Pathogenetic Driver for Two Divergent Clinical Trajectories: Elucidating the Paradox of “Ascites Worsening and Variceal Regression”
3. Therapeutic Options in Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease
3.1. Role of Human Albumin Administration: State of the Art
3.1.1. The Pleiotropic Effects of Human Albumin: More than a Plasma Volume Expander
3.1.2. Re-Evaluating the Best Timeframe for Human Albumin Administration in HRS-AKI
3.2. Role of Terlipressin Administration in dACLD and Ascites: Beyond Hepatorenal Syndrome
3.3. Role of the Transjugular Intrahepatic Portosystemic Shunt (TIPS): State of the Art
3.4. Role of Alphapump®: State of the Art
3.5. Managing Infections Properly: Crucial Impact on Ascites and Kidney Dysfunction Worsening
3.6. Managing Kidney Dysfunction in Acute-on-Chronic Liver Failure: A Hard Clinical Challenge
3.7. The Emerging Role of Palliative Care (PC)
4. Future Perspectives
4.1. Fecal Microbiota Transplantation (FMT): Rationale of a Nascent Approach
4.2. Peritoneal Dialysis (PD): Rationale and Potential Clinical Applications
4.3. Punctual Risk Stratification and Accurate Prediction of Outcomes: Is It Time to Go Beyond “General” Phenotype Classification and Consider “Tailored” Approaches?
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACLD | Advanced Chronic Liver Disease |
| ADH | Antidiuretic Hormone |
| ADQI | Acute Disease Quality Initiative |
| AKD | Acute Kidney Disease |
| AKI | Acute Kidney Injury |
| ALD | Alcoholic Liver Disease |
| APD | Automated Peritoneal Dialysis |
| AREs | Ascites-Related Events |
| ASC | Ascites |
| ATN | Acute Tubular Necrosis |
| CAID | Cirrhosis-Associated Immune Dysfunction |
| CAPD | Continuous Ambulatory Peritoneal Dialysis |
| CPGs | Clinical Practice Guidelines |
| CRP | C-Reactive Protein |
| CKD | Chronic Kidney Disease |
| dACLD | Decompensated Advanced Chronic Liver Disease |
| EASL | European Association for the Study of the Liver |
| EMA | European Medicines Agency |
| eGFR | Estimated Glomerular Filtration Rate |
| FIB-4 | Fibrosis-4 Score |
| FMT | Fecal Microbiota Transplantation |
| HA | Human Albumin |
| HE | Hepatic Encephalopathy |
| HPA | Hypothalamic–Pituitary–Adrenal |
| HRS | Hepatorenal Syndrome |
| HRS-AKI | Hepatorenal Syndrome–Acute Kidney Injury |
| HRS-AKD | Hepatorenal Syndrome–Acute Kidney Disease |
| HRS-CKD | Hepatorenal Syndrome–Chronic Kidney Disease |
| HRS-NAKI | Hepatorenal Syndrome–Non-Acute Kidney Injury |
| HD | Hemodialysis |
| IL | Interleukin |
| ICA | International Club of Ascites |
| LPS | Lipopolysaccharide |
| LRE | Liver-Related Event |
| LT | Liver transplant/Liver transplantation |
| LVP | Large-Volume Paracentesis |
| MELD | Model for End-Stage Liver Disease |
| MDROs | Multidrug-resistant organisms |
| ML | Machine Learning |
| NAKI | Non-Acute Kidney Injury |
| NAREs | Non-Ascites-Related Events |
| NITs | Non-Invasive Tools |
| NSBBs | Non-Selective Beta-Blockers |
| PAMPs | Pathogen-Associated Molecular Patterns |
| PD | Peritoneal Dialysis |
| PRRs | Pattern Recognition Receptors |
| RA | Refractory Ascites |
| RAAS | Renin-Angiotensin-Aldosterone System |
| RecA | Recurrent Ascites |
| RRT | Renal Replacement Therapy |
| SBP | Spontaneous Bacterial Peritonitis |
| SCFAs | Short-Chain Fatty Acids |
| SNS | Sympathetic Nervous System |
| TIPS | Transjugular Intrahepatic Portosystemic Shunt |
| TNF-α | Tumor Necrosis Factor-alpha |
| TLRs | Toll-Like Receptors |
References
- Baumgartner, K.; Cooper, J.; Smith, A.; St Louis, J. Liver Disease: Cirrhosis. FP Essent 2021, 511, 36–43. [Google Scholar]
- Tapper, E.B.; Goldberg, D.; Parikh, N.D.; Terrault, N.A.; Welch, N.; Sharpton, S.; Hameed, B.; Khalili, M.; Stolz, A.; Verna, E.C.; et al. The Liver Cirrhosis Network Cohort Study: Cirrhosis Definition, Study Population, and Endpoints. Am. J. Gastroenterol. 2025, 120, 570–575. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the Management of Patients with Decompensated Cirrhosis. J. Hepatol. 2018, 69, 406–460. [Google Scholar] [CrossRef]
- de Franchis, R.; Bosch, J.; Garcia-Tsao, G.; Reiberger, T.; Ripoll, C.; Baveno VII Faculty. Baveno VII—Renewing Consensus in Portal Hypertension. J. Hepatol. 2022, 76, 959–974. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, G.; Bernardi, M.; Angeli, P. Towards a New Definition of Decompensated Cirrhosis. J. Hepatol. 2022, 76, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Balcar, L.; Tonon, M.; Semmler, G.; Calvino, V.; Hartl, L.; Incicco, S.; Jachs, M.; Bauer, D.; Hofer, B.S.; Gambino, C.G.; et al. Risk of Further Decompensation/Mortality in Patients with Cirrhosis and Ascites as the First Single Decompensation Event. JHEP Rep. 2022, 4, 100513. [Google Scholar] [CrossRef] [PubMed]
- Tonon, M.; Piano, S.; Gambino, C.G.; Romano, A.; Pilutti, C.; Incicco, S.; Brocca, A.; Sticca, A.; Bolognesi, M.; Angeli, P. Outcomes and Mortality of Grade 1 Ascites and Recurrent Ascites in Patients With Cirrhosis. Clin. Gastroenterol. Hepatol. 2021, 19, 358–366.e8. [Google Scholar] [CrossRef]
- Tonon, M.; Gagliardi, R.; Pompili, E.; Barone, A.; Zaccherini, G.; Zilio, G.; Baldassarre, M.; Accetta, A.; Carrello, D.; Calvino, V.; et al. Validation and Expansion of Baveno VII Recompensation Criteria in Patients with Cirrhosis and Curable Liver Disease. J. Hepatol. 2025, 83, 888–898. [Google Scholar] [CrossRef]
- Piano, S.; Reiberger, T.; Bosch, J. Mechanisms and Implications of Recompensation in Cirrhosis. JHEP Rep. 2024, 6, 101233. [Google Scholar] [CrossRef]
- Reiberger, T.; Hofer, B.S. The Baveno VII Concept of Cirrhosis Recompensation. Dig. Liver Dis. 2023, 55, 431–441. [Google Scholar] [CrossRef]
- Wong, F. Management of Refractory Ascites. Clin. Mol. Hepatol. 2023, 29, 16–32. [Google Scholar] [CrossRef] [PubMed]
- Moreau, R.; Delègue, P.; Pessione, F.; Hillaire, S.; Durand, F.; Lebrec, D.; Valla, D.-C. Clinical Characteristics and Outcome of Patients with Cirrhosis and Refractory Ascites. Liver Int. 2004, 24, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Olteanu, D.; Lupu, D. The Kidney in Cirrhosis with Portal Hypertension. J. Med. Life 2010, 3, 175–177. [Google Scholar] [PubMed]
- Sargent, S.; Martin, W. Renal Dysfunction in Liver Cirrhosis. Br. J. Nurs. 2006, 15, 12–16. [Google Scholar] [CrossRef]
- Adebayo, D.; Neong, S.F.; Wong, F. Ascites and Hepatorenal Syndrome. Clin. Liver Dis. 2019, 23, 659–682. [Google Scholar] [CrossRef]
- Villanueva, C.; Tripathi, D.; Bosch, J. Preventing the Progression of Cirrhosis to Decompensation and Death. Nat. Rev. Gastroenterol. Hepatol. 2025, 22, 265–280. [Google Scholar] [CrossRef]
- Angeli, P.; Garcia-Tsao, G.; Nadim, M.K.; Parikh, C.R. News in Pathophysiology, Definition and Classification of Hepatorenal Syndrome: A Step beyond the International Club of Ascites (ICA) Consensus Document. J. Hepatol. 2019, 71, 811–822. [Google Scholar] [CrossRef]
- Cullaro, G.; Asrani, S.K. Not All Episodes of Acute Kidney Injury Are Equal in Patients With Cirrhosis, Based on Patterns of Renal Dysfunction. Clin. Gastroenterol. Hepatol. 2020, 18, 1694–1695. [Google Scholar] [CrossRef]
- Allegretti, A.S.; Patidar, K.R.; Ma, A.T.; Cullaro, G. From Past to Present to Future: Terlipressin and Hepatorenal Syndrome-Acute Kidney Injury. Hepatology 2025, 81, 1878–1897. [Google Scholar] [CrossRef]
- Angeli, P.; Morando, F.; Cavallin, M.; Piano, S. Hepatorenal Syndrome. Contrib. Nephrol. 2011, 174, 46–55. [Google Scholar] [CrossRef]
- Pose, E.; Piano, S.; Juanola, A.; Ginès, P. Hepatorenal Syndrome in Cirrhosis. Gastroenterology 2024, 166, 588–604.e1. [Google Scholar] [CrossRef] [PubMed]
- Ginès, P.; Solà, E.; Angeli, P.; Wong, F.; Nadim, M.K.; Kamath, P.S. Hepatorenal Syndrome. Nat. Rev. Dis. Primers 2018, 4, 23. [Google Scholar] [CrossRef] [PubMed]
- Simonetto, D.A.; Gines, P.; Kamath, P.S. Hepatorenal Syndrome: Pathophysiology, Diagnosis, and Management. BMJ 2020, 370, m2687. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.; Bhurwal, A.; Law, C.; Ventre, S.; Minacapelli, C.D.; Kabaria, S.; Li, Y.; Tait, C.; Catalano, C.; Rustgi, V.K. Acute Kidney Injury and Hepatorenal Syndrome in Cirrhosis. World J. Gastroenterol. 2021, 27, 3984–4003. [Google Scholar] [CrossRef]
- Arnold, J.; Avila, E.; Idalsoaga, F.; Diaz, L.A.; Ayala Valverde, M.; Ayares, G.; Arrese, M.; Roessler, E.; Huidobro, J.P.; Hudson, D.; et al. Advances in the Diagnosis and Management of Hepatorenal Syndrome: Insights into HRS-AKI and Liver Transplantation. eGastroenterology 2023, 1, e100009. [Google Scholar] [CrossRef]
- Nadim, M.K.; Kellum, J.A.; Forni, L.; Francoz, C.; Asrani, S.K.; Ostermann, M.; Allegretti, A.S.; Neyra, J.A.; Olson, J.C.; Piano, S.; et al. Acute Kidney Injury in Patients with Cirrhosis: Acute Disease Quality Initiative (ADQI) and International Club of Ascites (ICA) Joint Multidisciplinary Consensus Meeting. J. Hepatol. 2024, 81, 163–183. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines on TIPS. J. Hepatol. 2025, 83, 177–210. [Google Scholar] [CrossRef]
- Moreau, R.; Jalan, R.; Gines, P.; Pavesi, M.; Angeli, P.; Cordoba, J.; Durand, F.; Gustot, T.; Saliba, F.; Domenicali, M.; et al. Acute-on-Chronic Liver Failure Is a Distinct Syndrome That Develops in Patients with Acute Decompensation of Cirrhosis. Gastroenterology 2013, 144, 1426–1437.e9. [Google Scholar] [CrossRef]
- Arroyo, V.; Moreau, R.; Jalan, R.; Ginès, P.; EASL-CLIF Consortium CANONIC Study. Acute-on-Chronic Liver Failure: A New Syndrome That Will Re-Classify Cirrhosis. J. Hepatol. 2015, 62, S131–S143. [Google Scholar] [CrossRef]
- Jalan, R.; Saliba, F.; Pavesi, M.; Amoros, A.; Moreau, R.; Ginès, P.; Levesque, E.; Durand, F.; Angeli, P.; Caraceni, P.; et al. Development and Validation of a Prognostic Score to Predict Mortality in Patients with Acute-on-Chronic Liver Failure. J. Hepatol. 2014, 61, 1038–1047. [Google Scholar] [CrossRef]
- Jalan, R.; Pavesi, M.; Saliba, F.; Amorós, A.; Fernandez, J.; Holland-Fischer, P.; Sawhney, R.; Mookerjee, R.; Caraceni, P.; Moreau, R.; et al. The CLIF Consortium Acute Decompensation Score (CLIF-C ADs) for Prognosis of Hospitalised Cirrhotic Patients without Acute-on-Chronic Liver Failure. J. Hepatol. 2015, 62, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Roth, D.; Bloom, R.D.; Molnar, M.Z.; Reese, P.P.; Sawinski, D.; Sise, M.E.; Terrault, N.A. KDOQI US Commentary on the 2018 KDIGO Clinical Practice Guideline for the Prevention, Diagnosis, Evaluation, and Treatment of Hepatitis C. Am. J. Kidney Dis. 2020, 75, 665–683. [Google Scholar] [CrossRef] [PubMed]
- Rashed, E.; Soldera, J. CLIF-SOFA and CLIF-C Scores for the Prognostication of Acute-on-Chronic Liver Failure and Acute Decompensation of Cirrhosis: A Systematic Review. World J. Hepatol. 2022, 14, 2025–2043. [Google Scholar] [CrossRef] [PubMed]
- Piano, S.; Rosi, S.; Maresio, G.; Fasolato, S.; Cavallin, M.; Romano, A.; Morando, F.; Gola, E.; Frigo, A.C.; Gatta, A.; et al. Evaluation of the Acute Kidney Injury Network Criteria in Hospitalized Patients with Cirrhosis and Ascites. J. Hepatol. 2013, 59, 482–489. [Google Scholar] [CrossRef]
- Engelmann, C.; Clària, J.; Szabo, G.; Bosch, J.; Bernardi, M. Pathophysiology of Decompensated Cirrhosis: Portal Hypertension, Circulatory Dysfunction, Inflammation, Metabolism and Mitochondrial Dysfunction. J. Hepatol. 2021, 75 (Suppl. S1), S49–S66. [Google Scholar] [CrossRef]
- Ginès, P.; Krag, A.; Abraldes, J.G.; Solà, E.; Fabrellas, N.; Kamath, P.S. Liver Cirrhosis. Lancet 2021, 398, 1359–1376. [Google Scholar] [CrossRef]
- Simões E Silva, A.C.; Miranda, A.S.; Rocha, N.P.; Teixeira, A.L. Renin Angiotensin System in Liver Diseases: Friend or Foe? World J. Gastroenterol. 2017, 23, 3396–3406. [Google Scholar] [CrossRef]
- Alukal, J.J.; John, S.; Thuluvath, P.J. Hyponatremia in Cirrhosis: An Update. Am. J. Gastroenterol. 2020, 115, 1775–1785. [Google Scholar] [CrossRef]
- Fortune, B.; Cardenas, A. Ascites, Refractory Ascites and Hyponatremia in Cirrhosis. Gastroenterol. Rep. 2017, 5, 104–112. [Google Scholar] [CrossRef]
- Møller, S.; Bendtsen, F.; Henriksen, J.H. Splanchnic and Systemic Hemodynamic Derangement in Decompensated Cirrhosis. Can. J. Gastroenterol. 2001, 15, 94–106. [Google Scholar] [CrossRef]
- Bernardi, M.; Moreau, R.; Angeli, P.; Schnabl, B.; Arroyo, V. Mechanisms of Decompensation and Organ Failure in Cirrhosis: From Peripheral Arterial Vasodilation to Systemic Inflammation Hypothesis. J. Hepatol. 2015, 63, 1272–1284. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, V.; Angeli, P.; Moreau, R.; Jalan, R.; Clària, J.; Trebicka, J.; Fernández, J.; Gustot, T.; Caraceni, P.; Bernardi, M.; et al. The Systemic Inflammation Hypothesis: Towards a New Paradigm of Acute Decompensation and Multiorgan Failure in Cirrhosis. J. Hepatol. 2021, 74, 670–685. [Google Scholar] [CrossRef] [PubMed]
- Dirchwolf, M.; Podhorzer, A.; Marino, M.; Shulman, C.; Cartier, M.; Zunino, M.; Paz, S.; Muñoz, A.; Bocassi, A.; Gimenez, J.; et al. Immune Dysfunction in Cirrhosis: Distinct Cytokines Phenotypes According to Cirrhosis Severity. Cytokine 2016, 77, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Pascual, S.; Such, J.; Esteban, A.; Zapater, P.; Casellas, J.A.; Aparicio, J.R.; Girona, E.; Gutiérrez, A.; Carnices, F.; Palazón, J.M.; et al. Intestinal Permeability Is Increased in Patients with Advanced Cirrhosis. Hepatogastroenterology 2003, 50, 1482–1486. [Google Scholar]
- Bajaj, J.S.; Heuman, D.M.; Hylemon, P.B.; Sanyal, A.J.; White, M.B.; Monteith, P.; Noble, N.A.; Unser, A.B.; Daita, K.; Fisher, A.R.; et al. Altered Profile of Human Gut Microbiome Is Associated with Cirrhosis and Its Complications. J. Hepatol. 2014, 60, 940–947. [Google Scholar] [CrossRef]
- Bauer, T.M.; Schwacha, H.; Steinbrückner, B.; Brinkmann, F.E.; Ditzen, A.K.; Aponte, J.J.; Pelz, K.; Berger, D.; Kist, M.; Blum, H.E. Small Intestinal Bacterial Overgrowth in Human Cirrhosis Is Associated with Systemic Endotoxemia. Am. J. Gastroenterol. 2002, 97, 2364–2370. [Google Scholar] [CrossRef]
- Wiest, R.; Lawson, M.; Geuking, M. Pathological Bacterial Translocation in Liver Cirrhosis. J. Hepatol. 2014, 60, 197–209. [Google Scholar] [CrossRef]
- Peng, J.L.; Techasatian, W.; Hato, T.; Liangpunsakul, S. Role of Endotoxemia in Causing Renal Dysfunction in Cirrhosis. J. Investig. Med. 2020, 68, 26–29. [Google Scholar] [CrossRef]
- Trebicka, J.; Fernandez, J.; Papp, M.; Caraceni, P.; Laleman, W.; Gambino, C.; Giovo, I.; Uschner, F.E.; Jimenez, C.; Mookerjee, R.; et al. The PREDICT Study Uncovers Three Clinical Courses of Acutely Decompensated Cirrhosis That Have Distinct Pathophysiology. J. Hepatol. 2020, 73, 842–854. [Google Scholar] [CrossRef]
- Jachs, M.; Hartl, L.; Schaufler, D.; Desbalmes, C.; Simbrunner, B.; Eigenbauer, E.; Bauer, D.J.M.; Paternostro, R.; Schwabl, P.; Scheiner, B.; et al. Amelioration of Systemic Inflammation in Advanced Chronic Liver Disease upon Beta-Blocker Therapy Translates into Improved Clinical Outcomes. Gut 2021, 70, 1758–1767. [Google Scholar] [CrossRef]
- Sansoè, G.; Aragno, M.; Mastrocola, R.; Mengozzi, G.; Parola, M. Alpha-2A Adrenoceptor Agonist Guanfacine Restores Diuretic Efficiency in Experimental Cirrhotic Ascites: Comparison with Clonidine. PLoS ONE 2016, 11, e0158486. [Google Scholar] [CrossRef]
- Wong, F. The Cardiorenal Connection: Is Cardiac Output the Sole Determinant of Renal Dysfunction in Cirrhosis? Am. J. Gastroenterol. 2022, 117, 1242–1243. [Google Scholar] [CrossRef]
- Krag, A.; Bendtsen, F.; Burroughs, A.K.; Møller, S. The Cardiorenal Link in Advanced Cirrhosis. Med. Hypotheses 2012, 79, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Violi, F.; Castellani, V.; Menichelli, D.; Pignatelli, P.; Pastori, D. Gut Barrier Dysfunction and Endotoxemia in Heart Failure: A Dangerous Connubium? Am. Heart J. 2023, 264, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Li, J.; Guo, J.; Geng, B.; Ji, W.; Zhao, Q.; Li, J.; Liu, X.; Liu, J.; Guo, Z.; et al. Gut-Dependent Microbial Translocation Induces Inflammation and Cardiovascular Events after ST-Elevation Myocardial Infarction. Microbiome 2018, 6, 66. [Google Scholar] [CrossRef] [PubMed]
- Noor, M.T.; Manoria, P. Immune Dysfunction in Cirrhosis. J. Clin. Transl. Hepatol. 2017, 5, 50–58. [Google Scholar] [CrossRef]
- Albillos, A.; Martin-Mateos, R.; Van der Merwe, S.; Wiest, R.; Jalan, R.; Álvarez-Mon, M. Cirrhosis-Associated Immune Dysfunction. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 112–134. [Google Scholar] [CrossRef]
- Irvine, K.M.; Ratnasekera, I.; Powell, E.E.; Hume, D.A. Causes and Consequences of Innate Immune Dysfunction in Cirrhosis. Front. Immunol. 2019, 10, 293. [Google Scholar] [CrossRef]
- Romeo, M.; Silvestrin, A.; Senese, G.; Di Nardo, F.; Napolitano, C.; Vaia, P.; Coppola, A.; Federico, P.; Dallio, M.; Federico, A. From “Traditional” to “Trained” Immunity: Exploring the Novel Frontiers of Immunopathogenesis in the Progression of Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD). Biomedicines 2025, 13, 2004. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Tsai, I.-F.; Ho, Y.-P.; Huang, C.-T.; Lin, Y.-C.; Lin, C.-J.; Tseng, S.-C.; Lin, W.-P.; Chen, W.-T.; Sheen, I.-S. Endotoxemia Contributes to the Immune Paralysis in Patients with Cirrhosis. J. Hepatol. 2007, 46, 816–826. [Google Scholar] [CrossRef]
- Rodríguez-Negrete, E.V.; Gálvez-Martínez, M.; Sánchez-Reyes, K.; Fajardo-Felix, C.F.; Pérez-Reséndiz, K.E.; Madrigal-Santillán, E.O.; Morales-González, Á.; Morales-González, J.A. Liver Cirrhosis: The Immunocompromised State. J. Clin. Med. 2024, 13, 5582. [Google Scholar] [CrossRef] [PubMed]
- Martin-Mateos, R.; Alvarez-Mon, M.; Albillos, A. Dysfunctional Immune Response in Acute-on-Chronic Liver Failure: It Takes Two to Tango. Front. Immunol. 2019, 10, 973. [Google Scholar] [CrossRef] [PubMed]
- McGettigan, B.; Hernandez-Tejero, M.; Malhi, H.; Shah, V. Immune Dysfunction and Infection Risk in Advanced Liver Disease. Gastroenterology 2025, 168, 1085–1100. [Google Scholar] [CrossRef] [PubMed]
- Kronsten, V.T.; Shawcross, D.L. Clinical Implications of Inflammation in Patients With Cirrhosis. Am. J. Gastroenterol. 2025, 120, 65–74. [Google Scholar] [CrossRef]
- Jothimani, D.; Rela, M.; Kamath, P.S. Liver Cirrhosis and Portal Hypertension: How to Deal with Esophageal Varices? Med. Clin. N. Am. 2023, 107, 491–504. [Google Scholar] [CrossRef]
- Alvarez-Silva, C.; Schierwagen, R.; Pohlmann, A.; Magdaleno, F.; Uschner, F.E.; Ryan, P.; Vehreschild, M.J.G.T.; Claria, J.; Latz, E.; Lelouvier, B.; et al. Compartmentalization of Immune Response and Microbial Translocation in Decompensated Cirrhosis. Front. Immunol. 2019, 10, 69. [Google Scholar] [CrossRef]
- Morales-Ruiz, M.; Cejudo-Martín, P.; Jiménez, W. Ascites and vascular dysfunction in human liver cirrhosis: New pathophysiologic concepts for a severe complication. Nefrologia 2003, 23 (Suppl. S3), 58–61. [Google Scholar]
- Zheng, X.; Bai, Z.; Wang, T.; Romeiro, F.G.; Mancuso, A.; Philips, C.A.; Wong, Y.J.; Nery, F.G.; Qi, X. Human Albumin Infusion for the Management of Liver Cirrhosis and Its Complications: An Overview of Major Findings from Meta-Analyses. Adv. Ther. 2023, 40, 1494–1529. [Google Scholar] [CrossRef]
- Naldi, M.; Baldassarre, M.; Domenicali, M.; Bartolini, M.; Caraceni, P. Structural and Functional Integrity of Human Serum Albumin: Analytical Approaches and Clinical Relevance in Patients with Liver Cirrhosis. J. Pharm. Biomed. Anal. 2017, 144, 138–153. [Google Scholar] [CrossRef]
- Arroyo, V.; García-Martinez, R.; Salvatella, X. Human Serum Albumin, Systemic Inflammation, and Cirrhosis. J. Hepatol. 2014, 61, 396–407. [Google Scholar] [CrossRef]
- Caraceni, P.; Riggio, O.; Angeli, P.; Alessandria, C.; Neri, S.; Foschi, F.G.; Levantesi, F.; Airoldi, A.; Boccia, S.; Svegliati-Baroni, G.; et al. Long-Term Albumin Administration in Decompensated Cirrhosis (ANSWER): An Open-Label Randomised Trial. Lancet 2018, 391, 2417–2429. [Google Scholar] [CrossRef]
- Caraceni, P.; O’Brien, A.; Gines, P. Long-Term Albumin Treatment in Patients with Cirrhosis and Ascites. J. Hepatol. 2022, 76, 1306–1317. [Google Scholar] [CrossRef]
- Philips, C.A.; Maiwall, R.; Sharma, M.K.; Jindal, A.; Choudhury, A.K.; Kumar, G.; Bhardwaj, A.; Mitra, L.G.; Agarwal, P.M.; Sarin, S.K. Comparison of 5% Human Albumin and Normal Saline for Fluid Resuscitation in Sepsis Induced Hypotension among Patients with Cirrhosis (FRISC Study): A Randomized Controlled Trial. Hepatol. Int. 2021, 15, 983–994. [Google Scholar] [CrossRef]
- Sort, P.; Navasa, M.; Arroyo, V.; Aldeguer, X.; Planas, R.; Ruiz-del-Arbol, L.; Castells, L.; Vargas, V.; Soriano, G.; Guevara, M.; et al. Effect of Intravenous Albumin on Renal Impairment and Mortality in Patients with Cirrhosis and Spontaneous Bacterial Peritonitis. N. Engl. J. Med. 1999, 341, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Pompili, E.; Zaccherini, G.; Piano, S.; Toniutto, P.; Lombardo, A.; Gioia, S.; Iannone, G.; De Venuto, C.; Tonon, M.; Gagliardi, R.; et al. Real-World Experience with Long-Term Albumin in Patients with Cirrhosis and Ascites. JHEP Rep. 2024, 6, 101221. [Google Scholar] [CrossRef] [PubMed]
- China, L.; Freemantle, N.; Forrest, E.; Kallis, Y.; Ryder, S.D.; Wright, G.; Portal, A.J.; Becares Salles, N.; Gilroy, D.W.; O’Brien, A.; et al. A Randomized Trial of Albumin Infusions in Hospitalized Patients with Cirrhosis. N. Engl. J. Med. 2021, 384, 808–817. [Google Scholar] [CrossRef] [PubMed]
- China, L.; Tittanegro, T.; Crocombe, D.; Forrest, E.; Kallis, Y.; Ryder, S.D.; Wright, G.; Freemantle, N.; O’Brien, A. Investigating Potential Confounding by Indication When Considering the Association between Proton Pump Inhibitor Use, Infection, Hepatic Encephalopathy and Mortality in Hospitalised Decompensated Cirrhosis: A Post-Hoc Analysis of the ATTIRE Trial. EClinicalMedicine 2023, 58, 101924. [Google Scholar] [CrossRef]
- Solà, E.; Solé, C.; Simón-Talero, M.; Martín-Llahí, M.; Castellote, J.; Garcia-Martínez, R.; Moreira, R.; Torrens, M.; Márquez, F.; Fabrellas, N.; et al. Midodrine and Albumin for Prevention of Complications in Patients with Cirrhosis Awaiting Liver Transplantation. A Randomized Placebo-Controlled Trial. J. Hepatol. 2018, 69, 1250–1259. [Google Scholar] [CrossRef]
- Trebicka, J.; Garcia-Tsao, G. Controversies Regarding Albumin Therapy in Cirrhosis. Hepatology 2025, 81, 288–303. [Google Scholar] [CrossRef]
- Bai, Z.; Méndez-Sánchez, N.; Romeiro, F.G.; Mancuso, A.; Philips, C.A.; Tacke, F.; Basaranoglu, M.; Primignani, M.; Ibrahim, M.; Wong, Y.J.; et al. Use of Albumin Infusion for Cirrhosis-Related Complications: An International Position Statement. JHEP Rep. 2023, 5, 100785. [Google Scholar] [CrossRef]
- Karki, N.; Kc, S.; Sharma, D.; Jaisi, B.; Khadka, S. Cardiac Dysfunction in Patients with Liver Cirrhosis. J. Nepal Health Res. Counc. 2019, 17, 357–361. [Google Scholar] [CrossRef]
- Schleicher, E.M.; Karbannek, H.; Weinmann-Menke, J.; Galle, P.R.; Stallmach, A.; Gairing, S.J.; Zipprich, A.; Ripoll, C.; Labenz, C. Effect of Albumin Treatment Duration on Response Rates and Outcomes in Patients with Cirrhosis and Acute Kidney Injury. J. Hepatol. 2025, 83, 682–691. [Google Scholar] [CrossRef]
- Ma, A.T.; Juanola, A.; Solé, C.; Ginès, P. Shortening the Albumin Challenge from 48 to 24 Hours May Lead to Overdiagnosis of Hepatorenal Syndrome-Acute Kidney Injury and Overtreatment with Terlipressin. J. Hepatol. 2025, 82, e98–e99. [Google Scholar] [CrossRef]
- Angeli, P.; Labenz, C.; Piano, S.; Juanola, A.; Krag, A.; Caraceni, P.; Trebicka, J.; Maiwall, R.; Singh, V.; Pose, E.; et al. Albumin Infusion in Hepatorenal Syndrome-Acute Kidney Injury: New Evidence Challenges Recent Consensus. J. Hepatol. 2025, 83, 800–802. [Google Scholar] [CrossRef]
- Scheinberg, A.R.; Martin, P.; Turkeltaub, J.A. Terlipressin in the Management of Liver Disease. Expert Opin. Pharmacother. 2023, 24, 1665–1671. [Google Scholar] [CrossRef] [PubMed]
- Wong, F. Terlipressin for Hepatorenal Syndrome. Curr. Opin. Gastroenterol. 2024, 40, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Terbah, R.; Hoermann, R.; Grace, J.A.; Burrell, L.M.; Patel, S.K.; Testro, A.; Majumdar, A.; Sinclair, M. Impact of Long-Term Continuous Terlipressin Infusion on the Renin-Angiotensin-Aldosterone System in Patients with Decompensated Cirrhosis. Frontline Gastroenterol. 2025. [Google Scholar] [CrossRef]
- Terbah, R.; Testro, A.G.; Hoermann, R.; Majumdar, A.; Chapman, B.; Gow, P.J.; Sinclair, M. Continuous Home Terlipressin Infusion Increases Handgrip Strength and Reduces Ascites-A Prospective Randomized Crossover Study. Hepatology 2024, 80, 605–620. [Google Scholar] [CrossRef]
- Bai, Z.; An, Y.; Guo, X.; Teschke, R.; Méndez-Sánchez, N.; Li, H.; Qi, X. Role of Terlipressin in Cirrhotic Patients with Ascites and without Hepatorenal Syndrome: A Systematic Review of Current Evidence. Can. J. Gastroenterol. Hepatol. 2020, 2020, 5106958. [Google Scholar] [CrossRef]
- Shen, L.; Ying, J.; Zhao, J. The Application of Terlipressin in the Management of Ascites in Liver Cirrhosis: Current Status and Prospects. Br. J. Hosp. Med. 2024, 85, 1–13. [Google Scholar] [CrossRef]
- Larrue, H.; D’Amico, G.; Olivas, P.; Lv, Y.; Bucsics, T.; Rudler, M.; Sauerbruch, T.; Hernandez-Gea, V.; Han, G.; Reiberger, T.; et al. TIPS Prevents Further Decompensation and Improves Survival in Patients with Cirrhosis and Portal Hypertension in an Individual Patient Data Meta-Analysis. J. Hepatol. 2023, 79, 692–703. [Google Scholar] [CrossRef]
- Rajesh, S.; George, T.; Philips, C.A.; Ahamed, R.; Kumbar, S.; Mohan, N.; Mohanan, M.; Augustine, P. Transjugular Intrahepatic Portosystemic Shunt in Cirrhosis: An Exhaustive Critical Update. World J. Gastroenterol. 2020, 26, 5561–5596. [Google Scholar] [CrossRef] [PubMed]
- Allaire, M.; Walter, A.; Sutter, O.; Nahon, P.; Ganne-Carrié, N.; Amathieu, R.; Nault, J.-C. TIPS for Management of Portal-Hypertension-Related Complications in Patients with Cirrhosis. Clin. Res. Hepatol. Gastroenterol. 2020, 44, 249–263. [Google Scholar] [CrossRef] [PubMed]
- Colombato, L. The Role of Transjugular Intrahepatic Portosystemic Shunt (TIPS) in the Management of Portal Hypertension. J. Clin. Gastroenterol. 2007, 41 (Suppl. S3), S344–S351. [Google Scholar] [CrossRef] [PubMed]
- Rössle, M.; Ochs, A.; Gülberg, V.; Siegerstetter, V.; Holl, J.; Deibert, P.; Olschewski, M.; Reiser, M.; Gerbes, A.L. A Comparison of Paracentesis and Transjugular Intrahepatic Portosystemic Shunting in Patients with Ascites. N. Engl. J. Med. 2000, 342, 1701–1707. [Google Scholar] [CrossRef]
- Bureau, C.; Thabut, D.; Oberti, F.; Dharancy, S.; Carbonell, N.; Bouvier, A.; Mathurin, P.; Otal, P.; Cabarrou, P.; Péron, J.M.; et al. Transjugular Intrahepatic Portosystemic Shunts with Covered Stents Increase Transplant-Free Survival of Patients With Cirrhosis and Recurrent Ascites. Gastroenterology 2017, 152, 157–163. [Google Scholar] [CrossRef]
- Ginès, P.; Uriz, J.; Calahorra, B.; Garcia-Tsao, G.; Kamath, P.S.; Del Arbol, L.R.; Planas, R.; Bosch, J.; Arroyo, V.; Rodés, J. Transjugular Intrahepatic Portosystemic Shunting versus Paracentesis plus Albumin for Refractory Ascites in Cirrhosis. Gastroenterology 2002, 123, 1839–1847. [Google Scholar] [CrossRef]
- Salerno, F.; Merli, M.; Riggio, O.; Cazzaniga, M.; Valeriano, V.; Pozzi, M.; Nicolini, A.; Salvatori, F. Randomized Controlled Study of TIPS versus Paracentesis plus Albumin in Cirrhosis with Severe Ascites. Hepatology 2004, 40, 629–635. [Google Scholar] [CrossRef]
- Lebrec, D.; Giuily, N.; Hadengue, A.; Vilgrain, V.; Moreau, R.; Poynard, T.; Gadano, A.; Lassen, C.; Benhamou, J.P.; Erlinger, S. Transjugular Intrahepatic Portosystemic Shunts: Comparison with Paracentesis in Patients with Cirrhosis and Refractory Ascites: A Randomized Trial. French Group of Clinicians and a Group of Biologists. J. Hepatol. 1996, 25, 135–144. [Google Scholar] [CrossRef]
- Narahara, Y.; Kanazawa, H.; Fukuda, T.; Matsushita, Y.; Harimoto, H.; Kidokoro, H.; Katakura, T.; Atsukawa, M.; Taki, Y.; Kimura, Y.; et al. Transjugular Intrahepatic Portosystemic Shunt versus Paracentesis plus Albumin in Patients with Refractory Ascites Who Have Good Hepatic and Renal Function: A Prospective Randomized Trial. J. Gastroenterol. 2011, 46, 78–85. [Google Scholar] [CrossRef]
- Song, T.; Rössle, M.; He, F.; Liu, F.; Guo, X.; Qi, X. Transjugular Intrahepatic Portosystemic Shunt for Hepatorenal Syndrome: A Systematic Review and Meta-Analysis. Dig. Liver Dis. 2018, 50, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.L.; Saad, W.E.A.; Kalagher, S.D.; Caldwell, S.; Sabri, S.; Turba, U.C.; Matsumoto, A.H.; Angle, J.F. Effect of Transjugular Intrahepatic Portosystemic Shunt Placement on Renal Function: A 7-Year, Single-Center Experience. J. Vasc. Interv. Radiol. 2010, 21, 1370–1376. [Google Scholar] [CrossRef] [PubMed]
- Allegretti, A.S.; Ortiz, G.; Cui, J.; Wenger, J.; Bhan, I.; Chung, R.T.; Thadhani, R.I.; Irani, Z. Changes in Kidney Function After Transjugular Intrahepatic Portosystemic Shunts Versus Large-Volume Paracentesis in Cirrhosis: A Matched Cohort Analysis. Am. J. Kidney Dis. 2016, 68, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, A.J.; Genning, C.; Reddy, K.R.; Wong, F.; Kowdley, K.V.; Benner, K.; McCashland, T.; North American Study for the Treatment of Refractory Ascites Group. The North American Study for the Treatment of Refractory Ascites. Gastroenterology 2003, 124, 634–641. [Google Scholar] [CrossRef]
- Haskal, Z.J.; Radhakrishnan, J. Transjugular Intrahepatic Portosystemic Shunts in Hemodialysis-Dependent Patients and Patients with Advanced Renal Insufficiency: Safety, Caution, and Encephalopathy. J. Vasc. Interv. Radiol. 2008, 19, 516–520. [Google Scholar] [CrossRef]
- Bekaert, J.; Aerts, M.; François, S.; Raevens, S.; Degroote, H.; Geerts, A.; Verhelst, X.; Van Vlierberghe, H.; Reynaert, H. The Burden of Ascites in Cirrhosis. Acta Clin. Belg. 2025, 80, 8–16. [Google Scholar] [CrossRef]
- Lauerer, M.; Kaiser, K.; Nagel, E. Organ Transplantation in the Face of Donor Shortage—Ethical Implications with a Focus on Liver Allocation. Visc. Med. 2016, 32, 278–285. [Google Scholar] [CrossRef]
- Wong, F. Innovative Approaches to the Management of Ascites in Cirrhosis. JHEP Rep. 2023, 5, 100749. [Google Scholar] [CrossRef]
- Weil-Verhoeven, D.; Di Martino, V.; Stirnimann, G.; Cervoni, J.P.; Nguyen-Khac, E.; Thévenot, T. Alfapump® Implantable Device in Management of Refractory Ascites: An Update. World J. Hepatol. 2022, 14, 1344–1356. [Google Scholar] [CrossRef]
- Bellot, P.; Welker, M.-W.; Soriano, G.; von Schaewen, M.; Appenrodt, B.; Wiest, R.; Whittaker, S.; Tzonev, R.; Handshiev, S.; Verslype, C.; et al. Automated Low Flow Pump System for the Treatment of Refractory Ascites: A Multi-Center Safety and Efficacy Study. J. Hepatol. 2013, 58, 922–927. [Google Scholar] [CrossRef]
- Bureau, C.; Adebayo, D.; Chalret de Rieu, M.; Elkrief, L.; Valla, D.; Peck-Radosavljevic, M.; McCune, A.; Vargas, V.; Simon-Talero, M.; Cordoba, J.; et al. Alfapump® System vs. Large Volume Paracentesis for Refractory Ascites: A Multicenter Randomized Controlled Study. J. Hepatol. 2017, 67, 940–949. [Google Scholar] [CrossRef]
- Solà, E.; Sanchez-Cabús, S.; Rodriguez, E.; Elia, C.; Cela, R.; Moreira, R.; Pose, E.; Sánchez-Delgado, J.; Cañete, N.; Morales-Ruiz, M.; et al. Effects of AlfapumpTM System on Kidney and Circulatory Function in Patients with Cirrhosis and Refractory Ascites. Liver Transpl. 2017, 23, 583–593. [Google Scholar] [CrossRef]
- Macdonald, S.; Jalan, R. Editorial: Alfapump-an Alternative to Large-Volume Paracentesis for Patients with Refractory Ascites? Aliment. Pharmacol. Ther. 2018, 47, 139–140. [Google Scholar] [CrossRef]
- Piano, S.; Singh, V.; Caraceni, P.; Maiwall, R.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; Marino, M.; et al. Epidemiology and Effects of Bacterial Infections in Patients with Cirrhosis Worldwide. Gastroenterology 2019, 156, 1368–1380.e10. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Acevedo, J.; Wiest, R.; Gustot, T.; Amoros, A.; Deulofeu, C.; Reverter, E.; Martínez, J.; Saliba, F.; Jalan, R.; et al. Bacterial and Fungal Infections in Acute-on-Chronic Liver Failure: Prevalence, Characteristics and Impact on Prognosis. Gut 2018, 67, 1870–1880. [Google Scholar] [CrossRef] [PubMed]
- Fasolato, S.; Angeli, P.; Dallagnese, L.; Maresio, G.; Zola, E.; Mazza, E.; Salinas, F.; Donà, S.; Fagiuoli, S.; Sticca, A.; et al. Renal Failure and Bacterial Infections in Patients with Cirrhosis: Epidemiology and Clinical Features. Hepatology 2007, 45, 223–229. [Google Scholar] [CrossRef]
- Arvaniti, V.; D’Amico, G.; Fede, G.; Manousou, P.; Tsochatzis, E.; Pleguezuelo, M.; Burroughs, A.K. Infections in Patients with Cirrhosis Increase Mortality Four-Fold and Should Be Used in Determining Prognosis. Gastroenterology 2010, 139, 1246–1256, 1256.e1-5. [Google Scholar] [CrossRef] [PubMed]
- Fernández, J.; Bert, F.; Nicolas-Chanoine, M.-H. The Challenges of Multi-Drug-Resistance in Hepatology. J. Hepatol. 2016, 65, 1043–1054. [Google Scholar] [CrossRef]
- Park, H. Appropriate Empirical Antibiotic Use and 30-d Mortality in Cirrhotic Patients with Bacteremia. WJG 2015, 21, 3587. [Google Scholar] [CrossRef]
- Maiwall, R.; Piano, S.; Singh, V.; Caraceni, P.; Alessandria, C.; Fernandez, J.; Soares, E.C.; Kim, D.J.; Kim, S.E.; Marino, M.; et al. Determinants of Clinical Response to Empirical Antibiotic Treatment in Patients with Cirrhosis and Bacterial and Fungal Infections-Results from the ICA “Global Study” (EABCIR-Global Study). Hepatology 2024, 79, 1019–1032. [Google Scholar] [CrossRef]
- Wong, F.; Pappas, S.C.; Curry, M.P.; Reddy, K.R.; Rubin, R.A.; Porayko, M.K.; Gonzalez, S.A.; Mumtaz, K.; Lim, N.; Simonetto, D.A.; et al. Terlipressin plus Albumin for the Treatment of Type 1 Hepatorenal Syndrome. N. Engl. J. Med. 2021, 384, 818–828. [Google Scholar] [CrossRef]
- Nazar, A.; Pereira, G.H.; Guevara, M.; Martín-Llahi, M.; Pepin, M.-N.; Marinelli, M.; Solá, E.; Baccaro, M.E.; Terra, C.; Arroyo, V.; et al. Predictors of Response to Therapy with Terlipressin and Albumin in Patients with Cirrhosis and Type 1 Hepatorenal Syndrome. Hepatology 2010, 51, 219–226. [Google Scholar] [CrossRef]
- Jordan, R.I.; Tandon, P. Emerging Role of Palliative Care in Patients with Advanced Liver Disease. Semin. Liver Dis. 2020, 40, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Trotter, J.F. Liver Transplantation around the World. Curr. Opin. Organ Transplant. 2017, 22, 123–127. [Google Scholar] [CrossRef]
- Collins, K.M.; Chapman, W.C. High-Risk Liver Transplant Candidates: An Ethical Proposal on Where to Draw the Line. Liver Transpl. 2015, 21, 567–569. [Google Scholar] [CrossRef] [PubMed]
- Mafi, V.I.P.; Soldera, J. Palliative Care for End-Stage Liver Disease and Acute on Chronic Liver Failure: A Systematic Review. World J. Methodol. 2024, 14, 95904. [Google Scholar] [CrossRef] [PubMed]
- Dallio, M.; Romeo, M.; Di Nardo, F.; Napolitano, C.; Vaia, P.; Iadanza, G.; Olivieri, S.; Coppola, A.; Niosi, M.; Federico, A. Dysgeusia in MASLD-Related Advanced Chronic Liver Disease (ACLD): A Silent Driver towards the “Bermuda” Triangle of Malnutrition-Sarcopenia-Frailty Severely Affecting Prognosis. Nutr. J. 2025, 24, 10. [Google Scholar] [CrossRef]
- Albillos, A.; de Gottardi, A.; Rescigno, M. The Gut-Liver Axis in Liver Disease: Pathophysiological Basis for Therapy. J. Hepatol. 2020, 72, 558–577. [Google Scholar] [CrossRef]
- Romeo, M.; Dallio, M.; Di Nardo, F.; Napolitano, C.; Vaia, P.; Martinelli, G.; Federico, P.; Olivieri, S.; Iodice, P.; Federico, A. The Role of the Gut-Biliary-Liver Axis in Primary Hepatobiliary Liver Cancers: From Molecular Insights to Clinical Applications. J. Pers. Med. 2025, 15, 124. [Google Scholar] [CrossRef]
- Boicean, A.; Birlutiu, V.; Ichim, C.; Brusnic, O.; Onișor, D.M. Fecal Microbiota Transplantation in Liver Cirrhosis. Biomedicines 2023, 11, 2930. [Google Scholar] [CrossRef]
- Boicean, A.; Birlutiu, V.; Ichim, C.; Anderco, P.; Birsan, S. Fecal Microbiota Transplantation in Inflammatory Bowel Disease. Biomedicines 2023, 11, 1016. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Lu, Q.; Zhang, C.; Tang, Z.; Chu, L. Clinical Application and Progress of Fecal Microbiota Transplantation in Liver Diseases: A Review. Semin. Liver Dis. 2021, 41, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Bastos, R.M.C.; Simplício-Filho, A.; Sávio-Silva, C.; Oliveira, L.F.V.; Cruz, G.N.F.; Sousa, E.H.; Noronha, I.L.; Mangueira, C.L.P.; Quaglierini-Ribeiro, H.; Josefi-Rocha, G.R.; et al. Fecal Microbiota Transplant in a Pre-Clinical Model of Type 2 Diabetes Mellitus, Obesity and Diabetic Kidney Disease. Int. J. Mol. Sci. 2022, 23, 3842. [Google Scholar] [CrossRef]
- Rajora, N.; De Gregorio, L.; Saxena, R. Peritoneal Dialysis Use in Patients With Ascites: A Review. Am. J. Kidney Dis. 2021, 78, 728–735. [Google Scholar] [CrossRef]
- Mekraksakit, P.; Suppadungsuk, S.; Thongprayoon, C.; Miao, J.; Leelaviwat, N.; Thongpiya, J.; Qureshi, F.; Craici, I.M.; Cheungpasitporn, W. Outcomes of Peritoneal Dialysis in Cirrhosis: A Systematic Review and Meta-Analysis. Perit. Dial. Int. 2025, 45, 93–105. [Google Scholar] [CrossRef]
- Carrier, P.; Loustaud-Ratti, V.; Debette-Gratien, M.; Elkrief, L. Ascites in Cirrhotic Patients: A Comprehensive Review. Explor. Dig. Dis. 2024, 3, 362–381. [Google Scholar] [CrossRef]
- Angeli, P.; Gines, P.; Wong, F.; Bernardi, M.; Boyer, T.D.; Gerbes, A.; Moreau, R.; Jalan, R.; Sarin, S.K.; Piano, S.; et al. Diagnosis and Management of Acute Kidney Injury in Patients with Cirrhosis: Revised Consensus Recommendations of the International Club of Ascites. Gut 2015, 64, 531–537. [Google Scholar] [CrossRef]
- Msilanga, D.P.; Kwong, Y.D. Classifying Severe Acute Kidney Injury in Cirrhosis: Implications for Mortality? Kidney360 2025, 6, 182–184. [Google Scholar] [CrossRef]
- Cama-Olivares, A.; Ouyang, T.; Takeuchi, T.; St Hillien, S.A.; Robinson, J.E.; Chung, R.T.; Cullaro, G.; Karvellas, C.J.; Levitsky, J.; Orman, E.S.; et al. Association of Hepatorenal Syndrome-Acute Kidney Injury with Mortality in Patients with Cirrhosis Requiring Renal Replacement Therapy: Results from the HRS-HARMONY Consortium. Kidney360 2025, 6, 247–256. [Google Scholar] [CrossRef]
- Villa, G.; Ricci, Z.; Ronco, C. Renal Replacement Therapy. Crit. Care. Clin. 2015, 31, 839–848. [Google Scholar] [CrossRef]
- Tapper, E.B.; Parikh, N.D. Diagnosis and Management of Cirrhosis and Its Complications: A Review. JAMA 2023, 329, 1589–1602. [Google Scholar] [CrossRef]
- Dallio, M.; Romeo, M.; Di Nardo, F.; Napolitano, C.; Vaia, P.; Olivieri, S.; Niosi, M.; Federico, A. Spleen Area Affects the Performance of the Platelet Count-Based Non-Invasive Tools in Predicting First Hepatic Decompensation in Metabolic Dysfunction-Associated Steatotic Liver Disease Cirrhosis. J. Clin. Exp. Hepatol. 2025, 15, 102596. [Google Scholar] [CrossRef]
- Dallio, M.; Romeo, M.; Vaia, P.; Auletta, S.; Mammone, S.; Cipullo, M.; Sapio, L.; Ragone, A.; Niosi, M.; Naviglio, S.; et al. Red Cell Distribution Width/Platelet Ratio Estimates the 3-Year Risk of Decompensation in Metabolic Dysfunction-Associated Steatotic Liver Disease-Induced Cirrhosis. World J. Gastroenterol. 2024, 30, 685–704. [Google Scholar] [CrossRef] [PubMed]
- Schepke, M.; Appenrodt, B.; Heller, J.; Zielinski, J.; Sauerbruch, T. Prognostic Factors for Patients with Cirrhosis and Kidney Dysfunction in the Era of MELD: Results of a Prospective Study. Liver Int. 2006, 26, 834–839. [Google Scholar] [CrossRef] [PubMed]
- Hasan, I.; Nababan, S.H.H.; Handayu, A.D.; Aprilicia, G.; Gani, R.A. Scoring System for Predicting 90-Day Mortality of in-Hospital Liver Cirrhosis Patients at Cipto Mangunkusumo Hospital. BMC Gastroenterol. 2023, 23, 190. [Google Scholar] [CrossRef] [PubMed]
- Malik, S.; Frey, L.J.; Qureshi, K. Evaluating the Predictive Power of Machine Learning in Cirrhosis Mortality: A Systematic Review. J. Med. Artif. Intell. 2025, 8, 15. [Google Scholar] [CrossRef]
- Tantai, X.; Liu, Y.; Yeo, Y.H.; Praktiknjo, M.; Mauro, E.; Hamaguchi, Y.; Engelmann, C.; Zhang, P.; Jeong, J.Y.; van Vugt, J.L.A.; et al. Effect of Sarcopenia on Survival in Patients with Cirrhosis: A Meta-Analysis. J. Hepatol. 2022, 76, 588–599. [Google Scholar] [CrossRef]
- Grattagliano, I.; Ubaldi, E.; Bonfrate, L.; Portincasa, P. Management of Liver Cirrhosis between Primary Care and Specialists. World J. Gastroenterol. 2011, 17, 2273–2282. [Google Scholar] [CrossRef]
- Kjaergaard, M.; Lindvig, K.P.; Thorhauge, K.H.; Andersen, P.; Hansen, J.K.; Kastrup, N.; Jensen, J.M.; Hansen, C.D.; Johansen, S.; Israelsen, M.; et al. Using the ELF Test, FIB-4 and NAFLD Fibrosis Score to Screen the Population for Liver Disease. J. Hepatol. 2023, 79, 277–286. [Google Scholar] [CrossRef]
- Yeo, Y.H.; Samaan, J.S.; Ng, W.H.; Ting, P.-S.; Trivedi, H.; Vipani, A.; Ayoub, W.; Yang, J.D.; Liran, O.; Spiegel, B.; et al. Assessing the Performance of ChatGPT in Answering Questions Regarding Cirrhosis and Hepatocellular Carcinoma. Clin. Mol. Hepatol. 2023, 29, 721–732. [Google Scholar] [CrossRef]
- Wong, G.L.-H.; Espinosa, W.Z.; Wong, V.W.-S. Personalized Management of Cirrhosis by Non-Invasive Tests of Liver Fibrosis. Clin. Mol. Hepatol. 2015, 21, 200–211. [Google Scholar] [CrossRef]
- Cullaro, G.; Rubin, J.B.; Fortune, B.E.; Crawford, C.V.; Verna, E.C.; Hsu, C.-Y.; Liu, K.D.; Brown, R.S.; Lai, J.C.; Rosenblatt, R. Association Between Kidney Dysfunction Types and Mortality Among Hospitalized Patients with Cirrhosis. Dig. Dis. Sci. 2022, 67, 3426–3435. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romeo, M.; Napolitano, C.; Vaia, P.; Di Nardo, F.; Borrelli, S.; Garofalo, C.; De Nicola, L.; Federico, A.; Dallio, M. Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease: From “One Size Fits All” to a Multidisciplinary-Tailored Approach. Livers 2025, 5, 46. https://doi.org/10.3390/livers5030046
Romeo M, Napolitano C, Vaia P, Di Nardo F, Borrelli S, Garofalo C, De Nicola L, Federico A, Dallio M. Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease: From “One Size Fits All” to a Multidisciplinary-Tailored Approach. Livers. 2025; 5(3):46. https://doi.org/10.3390/livers5030046
Chicago/Turabian StyleRomeo, Mario, Carmine Napolitano, Paolo Vaia, Fiammetta Di Nardo, Silvio Borrelli, Carlo Garofalo, Luca De Nicola, Alessandro Federico, and Marcello Dallio. 2025. "Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease: From “One Size Fits All” to a Multidisciplinary-Tailored Approach" Livers 5, no. 3: 46. https://doi.org/10.3390/livers5030046
APA StyleRomeo, M., Napolitano, C., Vaia, P., Di Nardo, F., Borrelli, S., Garofalo, C., De Nicola, L., Federico, A., & Dallio, M. (2025). Managing Ascites and Kidney Dysfunction in Decompensated Advanced Chronic Liver Disease: From “One Size Fits All” to a Multidisciplinary-Tailored Approach. Livers, 5(3), 46. https://doi.org/10.3390/livers5030046








