Association Between Severity of COVID-19 and Social Determinants of Health with Adverse Pregnancy Outcomes in a Study of Mother–Infant Pairs in Los Angeles, California
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Operational Definitions
2.4. Statistical Analysis
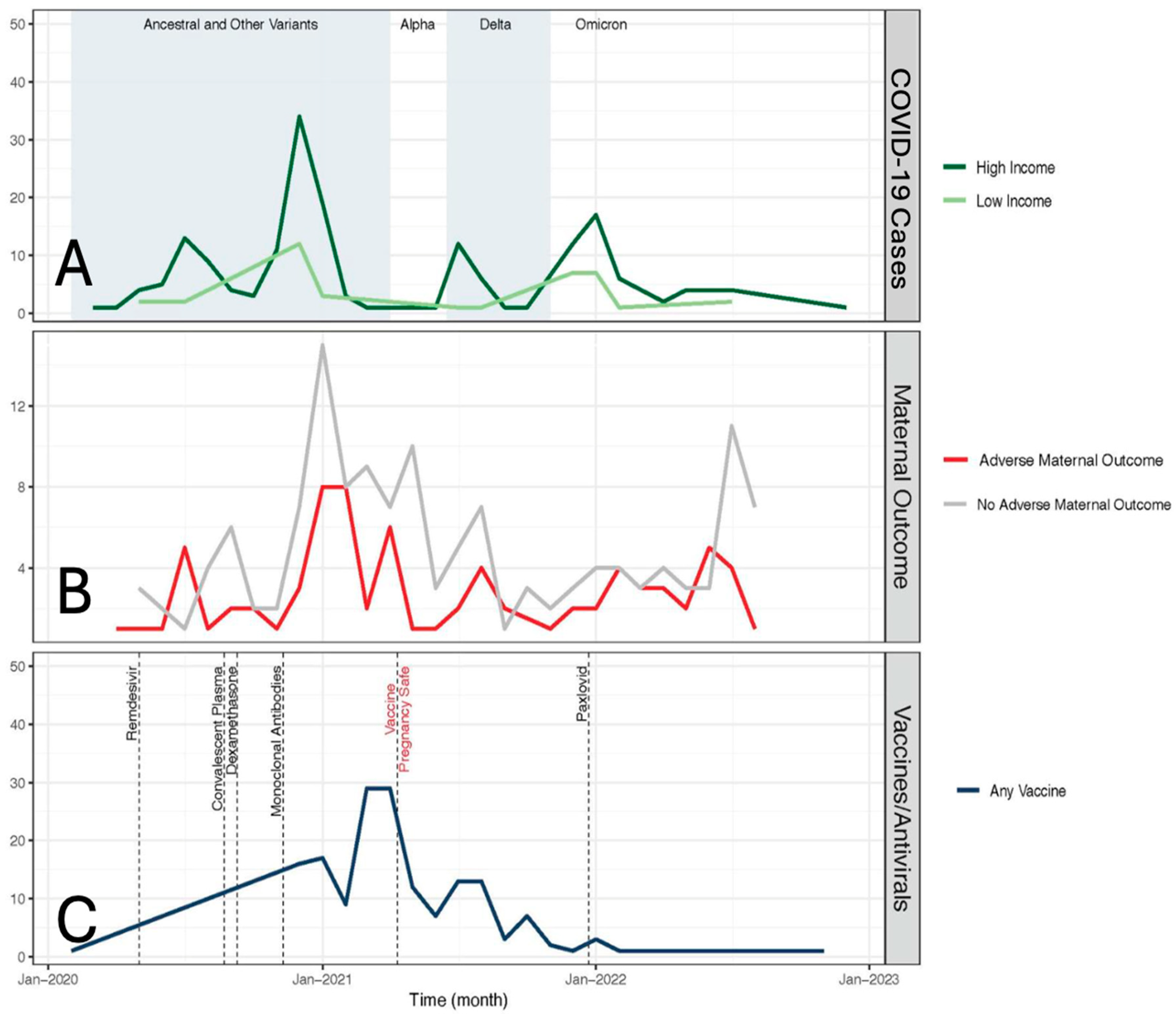
3. Results
3.1. Demographics
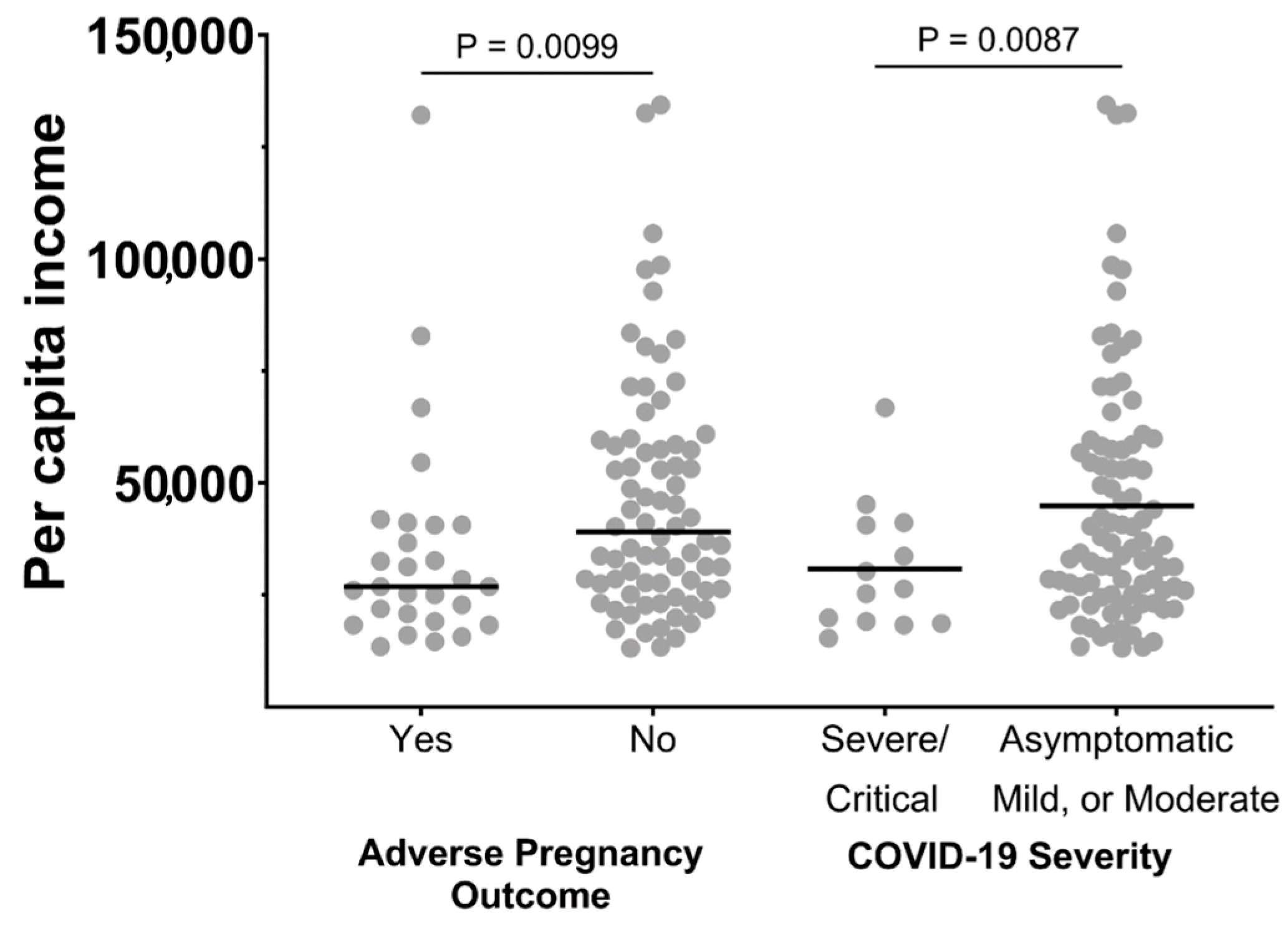
3.2. Association of APOs and COVID-19 Severity: Influence of SODHs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Villar, J.; Soto Conti, C.P.; Gunier, R.B.; Ariff, S.; Craik, R.; Cavoretto, P.I.; Rauch, S.; Gandino, S.; Nieto, R.; Winsey, A.; et al. Pregnancy outcomes and vaccine effectiveness during the period of omicron as the variant of concern, INTERCOVID-2022: A multinational, observational study. Lancet 2023, 401, 447–457. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cambou, M.C.; Liu, C.M.; Mok, T.; Fajardo-Martinez, V.; Paiola, S.G.; Ibarrondo, F.J.; Kerin, T.; Fuller, T.; Tobin, N.H.; Garcia, G.; et al. Longitudinal Evaluation of Antibody Persistence in Mother-Infant Dyads After Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Pregnancy. J. Infect. Dis. 2023, 227, 236–245. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fajardo Martinez, V.; Zhang, D.; Paiola, S.; Mok, T.; Cambou, M.C.; Kerin, T.; Rao, R.; Brasil, P.; Ferreira, F.; Fuller, T.; et al. Neuromotor repertoires in infants exposed to maternal COVID-19 during pregnancy: A cohort study. BMJ Open 2023, 13, e069194. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Foo, S.S.; Cambou, M.C.; Mok, T.; Fajardo, V.M.; Jung, K.L.; Fuller, T.; Chen, W.; Kerin, T.; Mei, J.; Bhattacharya, D.; et al. The systemic inflammatory landscape of COVID-19 in pregnancy: Extensive serum proteomic profiling of mother-infant dyads with. Cell Rep. Med. 2021, 2, 100453. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jamieson, D.J.; Rasmussen, S.A. An update on COVID-19 and pregnancy. Am. J. Obstet. Gynecol. 2022, 226, 177–186. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wei, S.Q.; Bilodeau-Bertrand, M.; Liu, S.; Auger, N. The impact of COVID-19 on pregnancy outcomes: A systematic review and meta-analysis. CMAJ 2021, 193, E540–E548. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chen, M.; Zeng, J.; Liu, X.; Sun, G.; Gao, Y.; Liao, J.; Yu, J.; Luo, X.; Qi, H. Changes in physiology and immune system during pregnancy and coronavirus infection: A review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 255, 124–128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- World Health Organization. Social Determinants of Health. 2024. Available online: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (accessed on 20 January 2025).
- U.S. Department of Health and Human Services OoDPaH. Healthy People 2030. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 20 January 2025).
- Prasannan, L.; Rochelson, B.; Shan, W.; Nicholson, K.; Solmonovich, R.; Kulkarni, A.; Lewis, D.; Greenberg, M.; Nimaroff, M.; Blitz, M.J. Social determinants of health and coronavirus disease 2019 in pregnancy. Am. J. Obs. Gynecol MFM 2021, 3, 100349. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsai, J.; Wilson, M. COVID-19: A potential public health problem for homeless populations. Lancet Public Health 2020, 5, e186–e187. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Backer, S.; Rezene, A.; Kahar, P.; Khanna, D. Socioeconomic Determinants of COVID-19 Incidence and Mortality in Florida. Cureus 2022, 14, e22491. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yancy, C.W. COVID-19 and African Americans. JAMA 2020, 323, 1891–1892. [Google Scholar] [CrossRef] [PubMed]
- Girardi, G.; Longo, M.; Bremer, A.A. Social determinants of health in pregnant individuals from underrepresented, understudied, and underreported populations in the United States. Int. J. Equity Health 2023, 22, 186. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hirshberg, A.; Srinivas, S.K. Epidemiology of maternal morbidity and mortality. Semin. Perinatol. 2017, 41, 332–337. [Google Scholar] [CrossRef] [PubMed]
- MacDorman, M.F.; Thoma, M.; Declcerq, E.; Howell, E.A. Racial and Ethnic Disparities in Maternal Mortality in the United States Using Enhanced Vital Records, 2016–2017. Am. J. Public Health 2021, 111, 1673–1681. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Glazer, K.B.; Zeitlin, J.; Howell, E.A. Intertwined disparities: Applying the maternal-infant dyad lens to advance perinatal health equity. Semin. Perinatol. 2021, 45, 151410. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dyer, L.; Chambers, B.D.; Crear-Perry, J.; Theall, K.P.; Wallace, M. The Index of Concentration at the Extremes (ICE) and Pregnancy-Associated Mortality in Louisiana, 2016–2017. Matern. Child Health J. 2022, 26, 814–822. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mack, J.A.; Voss, E.A.; Rusu, R.; Hernandez, M.C.; Hernandez-Diaz, S.; Wyszynski, D.F.; Sylvester, S.; DiSantostefano, R.L. Social determinants of health associated with COVID-19 severity during pregnancy: A multinational cohort study (in the International Registry of Coronavirus Exposure in Pregnancy). BMC Public Health 2022, 22, 2256. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dongarwar, D.; Ajewole, V.B.; Oduguwa, E.; Ngujede, A.; Harris, K.; Ofili, T.U.; Olaleye, O.A.; Salihu, H.M. Role of Social Determinants of Health in Widening Maternal and Child Health Disparities in the Era of COVID-19 Pandemic. Int. J. MCH AIDS 2020, 9, 316–319. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- DiBari, J.N.; Yu, S.M.; Chao, S.M.; Lu, M.C. Use of postpartum care: Predictors and barriers. J. Pregnancy 2014, 2014, 530769. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Fajardo-Martinez, V.; Ferreira, F.; Fuller, T.; Cambou, M.C.; Kerin, T.; Paiola, S.; Mok, T.; Rao, R.; Mohole, J.; Paravastu, R.; et al. Neurodevelopmental delay in children exposed to maternal SARS-CoV-2 in-utero. Sci. Rep. 2024, 14, 11851. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Man, O.M.; Azamor, T.; Cambou, M.C.; Fuller, T.L.; Kerin, T.; Paiola, S.G.; Cranston, J.S.; Mok, T.; Rao, R.; Chen, W.; et al. Respiratory distress in SARS-CoV-2 exposed uninfected neonates followed in the COVID Outcomes in Mother-Infant Pairs (COMP) Study. Nat. Commun. 2024, 15, 399. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
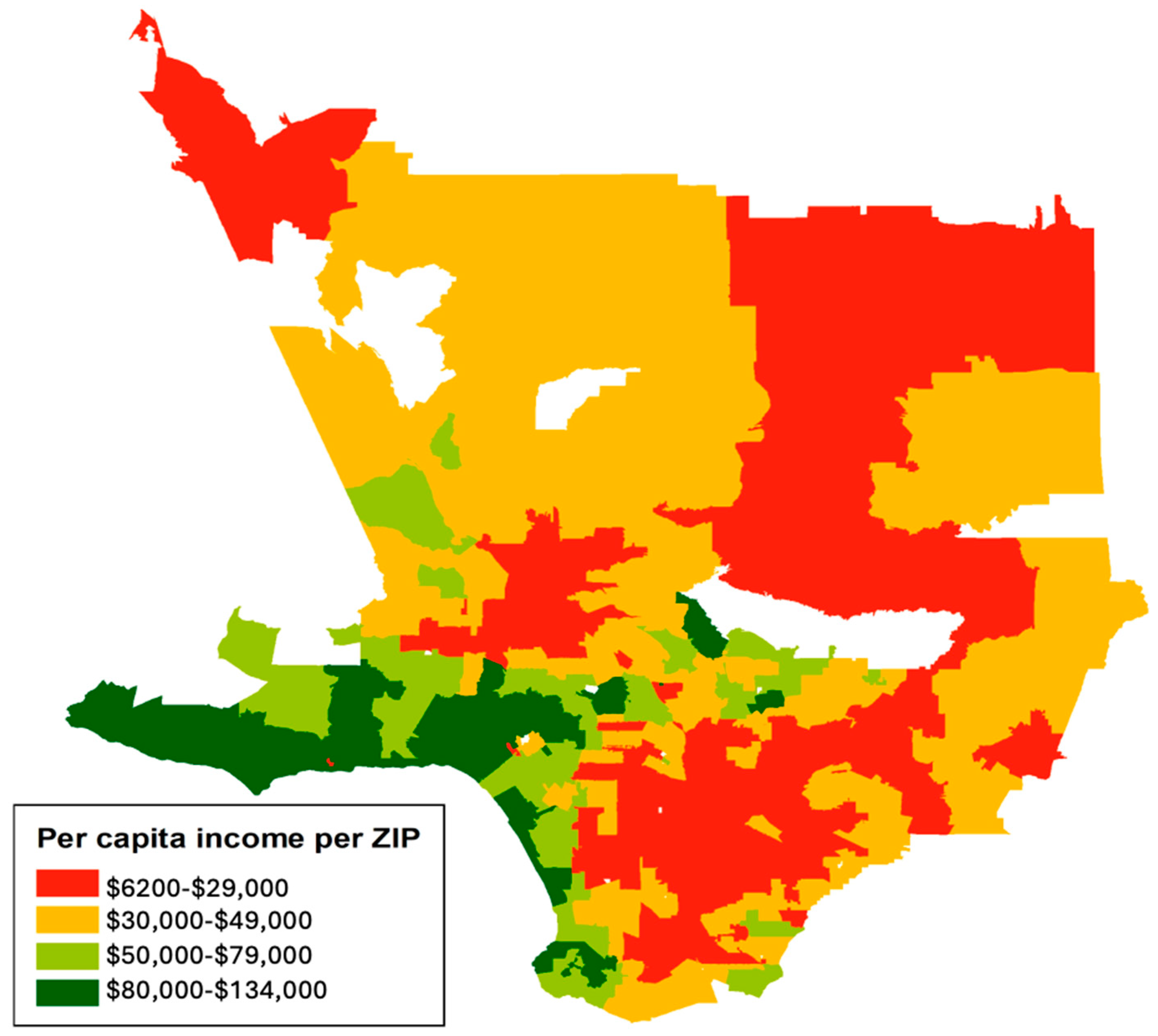
- SimplyAnalytics. Map with 2021 Median Household Income. SimplyAnalytics Database. 2023. Available online: https://www.simplyanalytics.com/ (accessed on 4 June 2023).
- ArcGIS. Available online: https://egis-lacounty.hub.arcgis.com/search?categories=%252Fcategories%252Fproperty%2520and%2520planning (accessed on 20 January 2025).
- OpenStreetMap. Copyright and License [10 June 2021]. Available online: https://www.openstreetmap.org/copyright (accessed on 20 January 2025).
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- COVID-19 Treatment Guidelines Panel. Coronavirus 2019 Disease (COVID-19) Treatment Guidelines; National Institutes of Health: Bethesda, MD, USA, 2023. Available online: https://web.archive.org/web/20240816204014/https://www.covid19treatmentguidelines.nih.gov/ (accessed on 1 April 2025).
- Braveman, P. Health disparities and health equity: Concepts and measurement. Annu. Rev. Public Health 2006, 27, 167–194. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P. Defining Health Equity. J. Natl. Med. Assoc. 2022, 114, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. S2), 19–31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morelli, V. Social Determinants of Health: An Overview for the Primary Care Provider. Prim. Care 2023, 50, 507–525. [Google Scholar] [CrossRef] [PubMed]
- California Department of Housing and Community Development. Available online: https://www.hcd.ca.gov/planning-and-community-development/housing-elements/building-blocks/overpayment-payment-and-overcrowding (accessed on 1 April 2025).
- WHO. 3 Household Crowding. In WHO Housing and Health Guidelines; World Health Organization: Geneva, Switzerland, 2018; Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- Virk, S.; Gangu, K.; Nasrullah, A.; Shah, A.; Faiz, Z.; Khan, U.; Jackson, D.B.; Javed, A.; Farooq, A.; DiSilvio, B.; et al. Impact of COVID-19 on Pregnancy Outcomes across Trimesters in the United States. Biomedicines 2023, 11, 2886. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Macias Gil, R.; Marcelin, J.R.; Zuniga-Blanco, B.; Marquez, C.; Mathew, T.; Piggott, D.A. COVID-19 Pandemic: Disparate Health Impact on the Hispanic/Latinx Population in the United States. J. Infect. Dis. 2020, 222, 1592–1595. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Clark, E.; Fredricks, K.; Woc-Colburn, L.; Bottazzi, M.E.; Weatherhead, J. Disproportionate impact of the COVID-19 pandemic on immigrant communities in the United States. PLoS Negl. Trop. Dis. 2020, 14, e0008484. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Simon, P.; Ho, A.; Shah, M.D.; Shetgiri, R. Trends in Mortality From COVID-19 and Other Leading Causes of Death Among Latino vs White Individuals in Los Angeles County, 2011–2020. JAMA 2021, 326, 973–974. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Metz, T.D.; Clifton, R.G.; Hughes, B.L.; Sandoval, G.J.; Grobman, W.A.; Saade, G.R.; Manuck, T.A.; Longo, M.; Sowles, A.; Clark, K.; et al. Association of SARS-CoV-2 Infection with Serious Maternal Morbidity and Mortality from Obstetric Complications. JAMA 2022, 327, 748–759. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Abbasi, J. The COVID Heart-One Year After SARS-CoV-2 Infection, Patients Have an Array of Increased Cardiovascular Risks. JAMA 2022, 327, 1113–1114. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.; Marks, R.; Ramirez, R.; Ríos-Vargas, M. 2020 Census Illuminates Racial and Ethnic Composition of the Country. 2021. Available online: https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html (accessed on 20 January 2025).
- Wadhera, R.K.; Wadhera, P.; Gaba, P.; Figueroa, J.F.; Joynt Maddox, K.E.; Yeh, R.W.; Shen, C. Variation in COVID-19 Hospitalizations and Deaths Across New York City Boroughs. JAMA 2020, 323, 2192–2195. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mayorquin, J. In This LA Neighborhood, Nicknamed “Black Beverly Hills”, Success Is Common for African Americans: ABC7. 2020. Available online: https://abc7.com/black-beverly-hills-baldwin-ladera-heights-real-estate/7222331/ (accessed on 12 September 2024).
- Piekos, S.N.; Hwang, Y.M.; Roper, R.T.; Sorensen, T.; Price, N.D.; Hood, L.; Hadlock, J.J. Effect of COVID-19 vaccination and booster on maternal-fetal outcomes: A retrospective cohort study. Lancet Digit. Health 2023, 5, e594–e606. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Beck, A.N.; Thomas, K.; Finch, B.K.; Gibbons, J. Determining Gentrification’s Relationship to Birth Outcomes in Metropolitan California. Hous. Policy Debate 2023, 33, 107–128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Keisler-Starkey, K.; Bunch, L.N.; Lindstrom, R.A. Health Insurance Coverage in the United States: 2022. 2023. Available online: https://www.census.gov/library/publications/2023/demo/p60-281.html (accessed on 20 January 2025).
- Khalifeh, Z.; Saluja, S.; Lam, C.N.; Kaplan, C. Disparities in access to COVID-19 testing in Los Angeles County. Prev. Med. Rep. 2024, 37, 102567. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Pregnant Participants | All Participants | Asymptomatic/Mild/ Moderate COVID-19 N = 192 | Severe/Critical COVID-19 N = 29 | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Mean maternal age (std) | 32.7 | 6.52 | 32.8 | 6 | 32.1 | 5.54 | 0.58 | |
| Maternal ethnicity | ||||||||
| Asian | 28 | 12.7 | 26 | 13.5 | 2 | 6.9 | 0.27 | |
| Black/African American | 14 | 6.3 | 11 | 5.7 | 3 | 10.3 | ||
| Hispanic/Latinx | 96 | 43.4 | 79 | 41.1 | 17 | 58.6 | ||
| White | 55 | 24.9 | 50 | 26.0 | 5 | 17.2 | ||
| Other/unknown | 28 | 12.7 | 26 | 13.5 | 2 | 6.9 | ||
| COVID-19 immunization | ||||||||
| No dose before delivery | 145 | 65.6 | 119 | 62.0 | 26 | 89.7 | 0.01 | |
| At least one dose before infection | 68 | 30.8 | 66 | 34.4 | 2 | 6.9 | ||
| At least one dose before delivery | 76 | 34.3 | 73 | 38.0 | 3 | 10.3 | ||
| Insurance | ||||||||
| Private insurance | 133 | 60.2 | 118 | 61.5 | 15 | 51.7 | 0.01 | |
| Government insurance | 54 | 24.4 | 41 | 21.4 | 13 | 44.8 | ||
| Uninsured/unknown | 34 | 15.4 | 33 | 17.2 | 1 | 3.4 | ||
| Selected maternal comorbidities | ||||||||
| Asthma | 30 | 13.6 | 23 | 12.0 | 7 | 24.1 | 0.07 | |
| Autoimmune disorders | 18 | 8.1 | 16 | 8.3 | 2 | 6.9 | 0.79 | |
| Congenital heart disease | 10 | 4.5 | 9 | 4.7 | 1 | 3.4 | 0.76 | |
| Diabetes | 44 | 19.9 | 39 | 20.3 | 5 | 17.2 | 0.69 | |
| Obesity | 62 | 28.1 | 45 | 23.4 | 12 | 41.4 | <0.001 | |
| Substance abuse disorder | 8 | 3.6 | 8 | 4.2 | 0 | 0.0 | 0.11 | |
| Adverse pregnancy outcomes (N = 207) | ||||||||
| Hypertensive Disorder of pregnancy (preeclampsia, HELLP *, gestational HTN and chronic HTN) | 75 | 33.9 | 61 | 31.8 | 14 | 48.3 | 0.08 | |
| Prolonged rupture of membranes | 15 | 6.8 | 14 | 7.3 | 1 | 3.4 | 0.44 | |
| Fetal loss or demise | 6 | 2.7 | 5 | 2.6 | 1 | 3.4 | ||
| Maternal death | 1 | 0.5 | 0 | 0.0 | 1 | 3.4 | ||
| Any adverse outcome | 91 | 41.2 | 75 | 39.1 | 16 | 55.2 | 0.1 | |
| Variable | Crude | Adjusted * | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |||
| Ethnicity/race | ||||||||
| White | REF | REF | ||||||
| Asian | 0.71 | 0.26 | 1.83 | 0.49 | 0.70 | 0.26 | 1.85 | 0.48 |
| Black/African American | 2.70 | 0.82 | 9.81 | 0.11 | 2.62 | 0.75 | 10.16 | 0.14 |
| Hispanic/Latinx | 1.07 | 0.55 | 2.12 | 0.84 | 0.93 | 0.46 | 1.91 | 0.85 |
| Unknown/other | 0.97 | 0.38 | 2.45 | 0.95 | 1.06 | 0.39 | 2.83 | 0.91 |
| COVID-19 immunization No dose before delivery | REF | REF | ||||||
| ≥1 dose before infection | 0.98 | 0.52 | 1.68 | 0.83 | 1.09 | 0.58 | 2.06 | 0.78 |
| ≥1 dose before delivery | 0.74 | 0.01 | 1.11 | 0.13 | 0.18 | 0.01 | 1.18 | 0.13 |
| Insurance | ||||||||
| Private insurance | REF | REF | ||||||
| Government insurance | 1.51 | 0.80 | 2.86 | 0.20 | 1.27 | 0.63 | 2.57 | 0.51 |
| Uninsured/unknown | 0.72 | 0.32 | 1.57 | 0.42 | 0.73 | 0.30 | 1.69 | 0.47 |
| Selected maternal comorbidities ** | ||||||||
| Any | 1.18 | 0.69 | 2.03 | 0.54 | 0.96 | 0.54 | 1.71 | 0.90 |
| CHD | 1.45 | 0.39 | 5.37 | 0.56 | 1.30 | 0.32 | 5.19 | 0.71 |
| DM | 1.38 | 0.70 | 2.72 | 0.35 | 1.41 | 0.68 | 2.92 | 0.36 |
| Obesity | 1.15 | 0.63 | 2.07 | 0.66 | 0.88 | 0.44 | 1.73 | 0.71 |
| Disease Severity | ||||||||
| Asymp/mild/moderate | REF | REF | ||||||
| Severe | 1.92 | 0.88 | 4.28 | 0.10 | 1.75 | 0.75 | 4.15 | 0.20 |
| Variable | Crude | Adjusted * | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |||
| Ethnicity | ||||||||
| White (Ref) | REF | REF | ||||||
| Asian | 0.77 | 0.11 | 3.84 | 0.76 | 0.83 | 0.11 | 4.46 | 0.83 |
| Black/African American | 2.73 | 0.50 | 12.93 | 0.21 | 1.78 | 0.28 | 10.19 | 0.52 |
| Hispanic/Latina | 2.15 | 0.79 | 6.88 | 0.16 | 1.78 | 0.57 | 6.44 | 0.35 |
| Unknown/other | 0.77 | 0.11 | 3.84 | 0.76 | 0.51 | 0.07 | 2.74 | 0.45 |
| COVID-19 immunization | ||||||||
| No dose before delivery | REF | REF | ||||||
| ≥1 dose before infection | 0.14 | 0.02 | 0.48 | 0.01 | 0.14 | 0.02 | 0.53 | 0.01 |
| ≥1 dose before delivery | 0.65 | 0.03 | 3.90 | 0.70 | 1.21 | 0.06 | 9.57 | 0.87 |
| Insurance | ||||||||
| Private insurance | REF | REF | ||||||
| Government insurance | 2.49 | 1.08 | 5.70 | 0.30 | 1.52 | 0.58 | 3.98 | 0.39 |
| Uninsured/unknown | 0.24 | 0.01 | 1.24 | 0.17 | 0.16 | 0.01 | 0.94 | 0.10 |
| Selected maternal comorbidities ** | ||||||||
| Any | 2.22 | 0.99 | 5.36 | 0.06 | 2.05 | 0.84 | 5.28 | 0.12 |
| CHD | 0.73 | 0.04 | 4.09 | 0.77 | 0.32 | 0.02 | 2.23 | 0.32 |
| DM | 0.87 | 0.28 | 2.28 | 0.80 | 0.96 | 0.28 | 2.82 | 0.94 |
| Obesity | 4.63 | 2.07 | 10.64 | 0.001 | 3.61 | 1.44 | 9.46 | 0.01 |
| Variable | Crude | Adjusted * | ||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |||
| Ethnicity | ||||||||
| White (Ref) | REF | REF | ||||||
| Asian | 0.86 | 0.31 | 2.30 | 0.77 | 0.86 | 0.30 | 2.33 | 0.77 |
| Black/African American | 4.35 | 1.11 | 21.78 | 0.05 | 4.14 | 1.02 | 21.22 | 0.05 |
| Hispanic/Latina | 0.95 | 0.47 | 1.98 | 0.88 | 0.89 | 0.41 | 1.92 | 0.77 |
| Unknown/other | 1.02 | 0.38 | 2.69 | 0.97 | 1.12 | 0.40 | 3.11 | 0.83 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daouk, S.; Kerin, T.; Fuller, T.; Man, O.; Cambou, M.C.; Fajardo-Martinez, V.; Paiola, S.; Mok, T.; Rao, R.; Nielsen-Saines, K. Association Between Severity of COVID-19 and Social Determinants of Health with Adverse Pregnancy Outcomes in a Study of Mother–Infant Pairs in Los Angeles, California. Women 2025, 5, 12. https://doi.org/10.3390/women5020012
Daouk S, Kerin T, Fuller T, Man O, Cambou MC, Fajardo-Martinez V, Paiola S, Mok T, Rao R, Nielsen-Saines K. Association Between Severity of COVID-19 and Social Determinants of Health with Adverse Pregnancy Outcomes in a Study of Mother–Infant Pairs in Los Angeles, California. Women. 2025; 5(2):12. https://doi.org/10.3390/women5020012
Chicago/Turabian StyleDaouk, Sarah, Tara Kerin, Trevon Fuller, Olivia Man, Mary C. Cambou, Viviana Fajardo-Martinez, Sophia Paiola, Thalia Mok, Rashmi Rao, and Karin Nielsen-Saines. 2025. "Association Between Severity of COVID-19 and Social Determinants of Health with Adverse Pregnancy Outcomes in a Study of Mother–Infant Pairs in Los Angeles, California" Women 5, no. 2: 12. https://doi.org/10.3390/women5020012
APA StyleDaouk, S., Kerin, T., Fuller, T., Man, O., Cambou, M. C., Fajardo-Martinez, V., Paiola, S., Mok, T., Rao, R., & Nielsen-Saines, K. (2025). Association Between Severity of COVID-19 and Social Determinants of Health with Adverse Pregnancy Outcomes in a Study of Mother–Infant Pairs in Los Angeles, California. Women, 5(2), 12. https://doi.org/10.3390/women5020012






