1. Introduction
As the global pandemic caused by SARS-CoV-2 (the novel coronavirus responsible for the disease COVID-19) enters its third year, it has become apparent that some individuals who contract the virus experience persisting illness. This is consistent with the two prior 21st century coronavirus epidemics (SARS and MERS), where some endured physical and mental sequelae for months or years after illness onset [
1]. In May 2020, the first anecdotal report of prolonged COVID-19 was published, and by June, online communities of people experiencing this were forming [
2]. These groups suggested that focusing on case numbers and deaths was creating an incomplete picture of COVID-19; it omitted this chronic condition, which these groups named long COVID [
3].
International definitions for long COVID have only recently been developed. The World Health Organization conducted a Delphi consensus study to establish a clinical case definition:
“Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others which generally have an impact on everyday functioning. Symptoms may be new onset, following initial recovery from an acute COVID19 episode, or persist from the initial illness. Symptoms may also fluctuate or relapse over time. A separate definition may be applicable for children” [
4] (p. 1). An international core outcome set was published following a further consensus study [
5] listing recovery from: “fatigue or exhaustion; pain; post-exertion symptoms; work/occupational and study changes; survival; and “functioning, symptoms and conditions” for each of the following outcomes: cardiovascular, respiratory, nervous system, cognition, mental and physical”.
There is currently an incomplete understanding of long COVID epidemiology and pathology [
6]. At the time of writing, the most recent Office for National Statistics [
7] report estimates that 1.3 million people in the UK, 2.1% of the population, have symptoms of their infection lasting beyond four weeks, based on self-reporting. Almost two thirds of those people felt their symptoms negatively impacted their daily life; almost a fifth felt their day-to-day activities were ‘limited a lot’. People who were aged 35–39, female, working in certain occupations or living in less affluent areas, and with another health condition were most likely to be affected. Therefore, long COVID has the potential to pose a significant burden to both individuals and healthcare systems.
It is currently unknown why some individuals experience symptoms past the acute phase, with persisting illness occurring regardless of acute disease severity [
3]. Some researchers theorize that women between 35–59 have a greater risk due to higher mortality rates in men and people of older ages [
8], while people of younger ages have greater immunity. There is evidence that women are likely to have greater impacts on their ability to fulfil family responsibilities [
9]; at this age it is possible that women are caring for people who are older and younger than themselves. Despite likely differences in women’s illness experiences, research has a tendency to include more men [
8,
9,
10,
11,
12]. Gaps in understanding remain and further research is needed [
13].
As long-COVID pathology and epidemiology are investigated, it is equally important to explore this condition through those that live it. This is in line with Scotland’s COVID-19 Rehabilitation and Recovery Framework [
14], which calls for the involvement of service users throughout each phase of the COVID-19 recovery process. Patient involvement in healthcare research, design, and provision are an increasingly valued perspective [
15]. Qualitative studies, an avenue of patient involvement, can expose the social and emotional impacts of an illness as well as how individuals understand and make sense of their condition [
16,
17]. This methodology encompasses multiple types, one being phenomenology. Phenomenology offers a deeper understanding of a phenomenon (long COVID) through exploring an individual’s perceptions and experiences [
18]. This allows studies to move beyond general descriptions to investigate how individuals attach meaning to a phenomenon and how this influences their reality [
19]. As the pandemic timeline continues, studying the holistic implications of long COVID will provide insight into the complexity of the illness experience, which can help inform the development of appropriate medical and social supports. It is important to understand the experience of women who have been identified as being at a greater risk of long COVID and who frequently have different influences on their illness experience when compared with men.
Therefore, the aim of this qualitative study is to explore the experiences and perceptions of women with confirmed or suspected COVID-19 who were living with persisting symptoms.
2. Materials and Methods
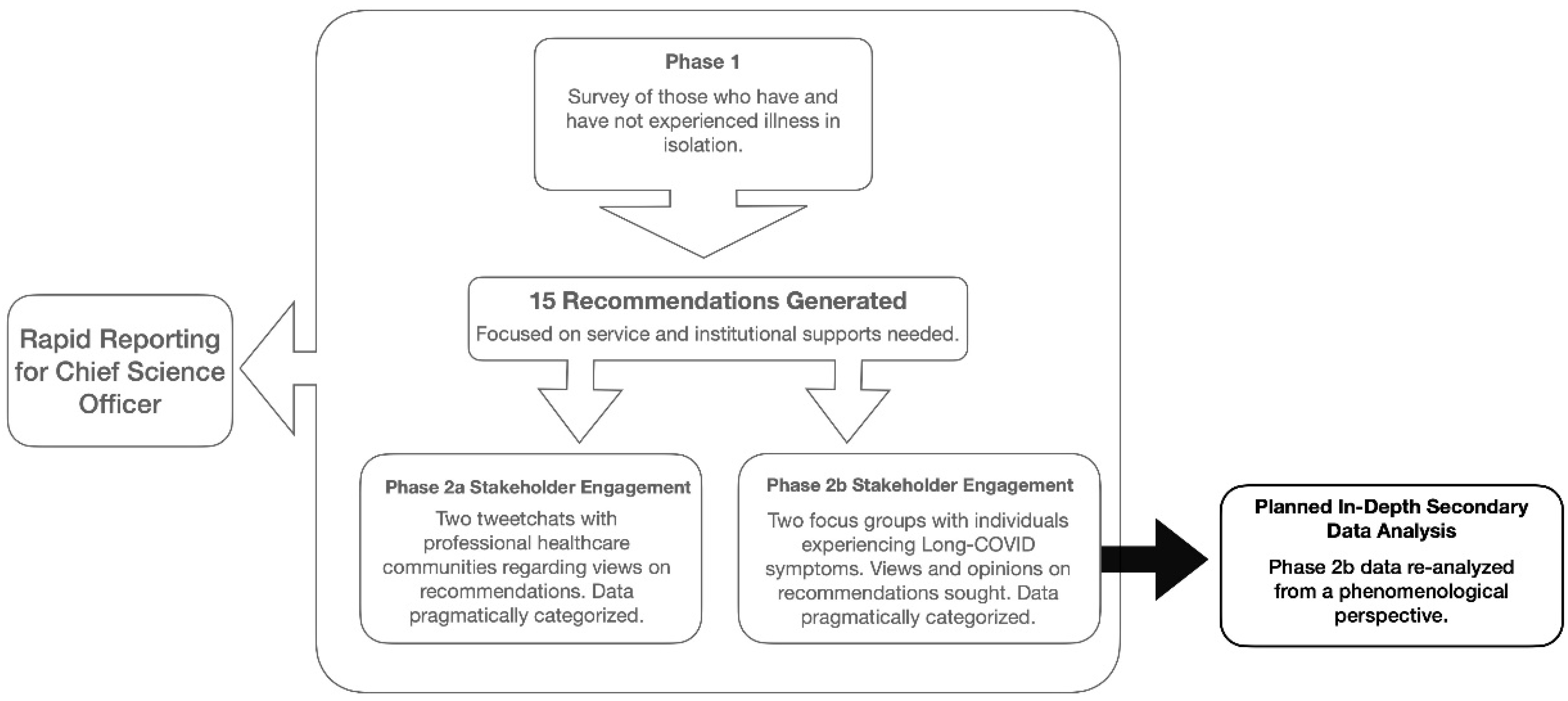
This study undertakes a planned in-depth secondary qualitative data analysis (SQDA) of data collected during a larger research project (see
Figure 1 below). This secondary analysis was intended to provide a deeper understanding of participants’ experiences through applying a phenomenological perspective. The secondary analysis was undertaken by research assistants that were present during data collection but were uninvolved in the primary analysis.
In order to explore and describe the experiences of individuals who identified as having long COVID, a qualitative approach was used [
20]. As much of the long-COVID community emerged through support groups, data were collected through focus groups in order to study this phenomenon from multiple perspectives [
21]. These were conducted remotely due to the ongoing COVID-19 pandemic using the online platform Blackboard Collaborate. This platform includes integrated audio–video tools, a chat function, and screen-sharing features. Ethical approval was gained from the appropriate higher education institution.
2.1. Sample and Recruiting
Participants were recruited in September and October 2020 through the Twitter account @LongCovidScot, a Scottish long-COVID peer support group. As peer groups played an important role in publicizing long COVID [
2], it was viewed as an appropriate participant pool. The research team contacted the peer group, and a digital meeting was held between two founding members and an individual from the research team. The peer support group privately promoted this study to their members and provided the research team’s contact details to interested individuals. Potential participants emailed the study team. In response, they received the recommendations generated in phase 1 (see
Figure 1 above) and a general overview, which included the study history, research aims, data management strategy, and what individuals could expect to occur during the focus groups. These were provided to facilitate informed consent.
The participation criteria included residency in Scotland, experiencing illness during the pandemic (which participants associated with a COVID-19 infection), and holding a conversational level of English. The criteria were implicitly met through the advocacy group membership. A formal diagnosis of COVID-19 was not required to participate in this study. There were two reasons for this decision. First, our study included individuals who became ill during the first several months of the COVID-19 pandemic. During this period, testing was either unavailable, challenging to access, or inaccurate [
22], and many individuals who fell ill in this period never received a COVID-19 diagnosis. Second, at the time of study conduction, there was no clinical definition nor diagnostic criteria for long COVID; this was an emerging condition that received minimal attention compared to acute COVID-19 illness. Due to the reality of the on-going pandemic, it was determined that self-identification with this condition met the inclusion criteria.
Eight individuals participated in this study. Though 18 people expressed interest and received the study information, 9 chose not to enroll, while 1 individual enrolled but did not attend the session. Eight participants was deemed an appropriate sample size for the phenomenological analysis [
23] while mitigating the consequences of remote focus groups, such as less data production [
24]. Acknowledging that individuals may be in a state of illness, participants self-selected session attendance to aid accessibility. Seven sessions were proposed; based on enrolment, two were held, and each contained four participants.
2.2. Protocol
Hour-long semi-structured focus groups occurred in October 2020. A topic guide, which included experiences with COVID-19, perspectives on the 15 recommendations, and identifying key messages for decision makers, steered the conversation. This directed discussion around research aims but provided participants the freedom to engage with elements central to their experience.
Before beginning the session, a consent statement was read, and participants consented to participate verbally or through the chat feature. The participants were reminded that audio, video, and chat data would be captured, ensuring informed consent, which is outlined in our ethics. Due to the ongoing nature of the pandemic, verbal consent was deemed appropriate to aid accessibility. Individuals were informed they had two weeks to withdraw from the study or alter contributions; this could be performed by emailing the research team stating their decision. The participants were reminded their identities would not be disclosed, and it was requested to respect the anonymity and privacy of fellow attendees and their contributions. Finally, though the discussion was not designed to elicit harm, individuals were reminded they could leave the conversation at any time without explanation. If, due to participation, someone experienced distress, mental health resources relevant to their geographical area would be provided.
A member of the research team (EC) with facilitation experience led both focus groups. Two research assistants (AJ and MM) were also in attendance. Introductions were followed by displaying the 15 recommendations on participants’ screens. Individuals shared their experiences with COVID-19 in the acute and long stages.
Research assistants were involved in two ways. One (AJ) used the chat function to encourage participation. This was performed by posing questions such as “[name] it appears that you agree with what’s being said, do you have anything else you’d like to add?”. This was used if individuals had not contributed recently and displayed a non-verbal communication cue (such as a head nod) in response to the discussion. The other (MM) asked clarifying questions in the chat, these were answered through text or audio. Both approaches aided in additional data generation and exploring everyone’s experiences.
2.3. Data Management, Processing, and Analysis
Focus groups produced audio–video recordings that included chat content. These were transcribed verbatim with identifiable information redacted and pseudonyms assigned. Though visual data was captured, the image predominantly displayed the 15 recommendations, not participants’ faces. Therefore, only the audio and chat were included in the transcriptions. A thematic analysis from a phenomenological perspective was then undertaken.
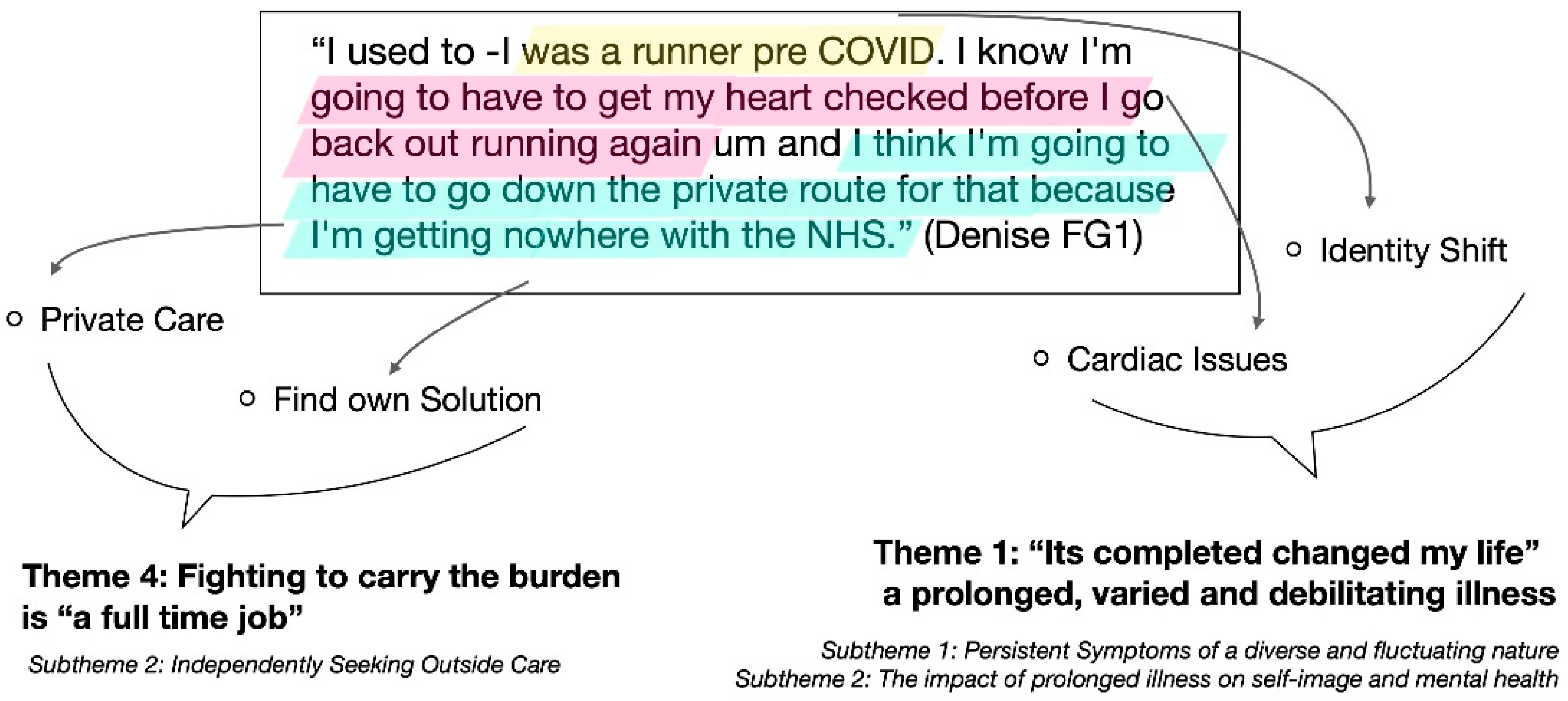
The complete thematic analysis technique is illustrated in
Figure 2 and is adopted from Vaismoradi et al. [
25]. Transcripts were analyzed in text blocks, which were one or two sentences long. A label was generated for each text block; this is a reductive process which aims to turn the meaning of each block into a single word or phrase [
25]. A common label was used for similar blocks, with new labels generated as necessary. Once both texts had been labelled, each transcript was reanalyzed; this ensured labels developed later in the analysis could be fully explored in both transcripts. At the end of this process, labeling was complete, with 87 distinct labels produced. Two research assistants (AJ and MM) agreed on labels to aid the rigor.
Labels expressing similar concepts were then grouped to generate themes. Themes represented an increasing level of abstraction, depicting ideas central to participants’ experiences [
25]. When the two research assistants could not agree on a label’s placement, a third researcher (EC) was sought to mediate.
Subthemes were generated by analyzing each theme. It was considered whether themes were a single unified experience or reflected several elements sharing a common nature; if the latter occurred, subthemes were developed. Quotes represented by the original labels were then selected for each theme and subtheme. This allowed for the illustration and explanation of experiences using participants’ own words. The development of an overarching explanatory theory was then undertaken.
Theories logically and meaningfully explain a phenomenon and are influenced by methodological choices [
26]. As a phenomenological perspective was used, our theory aimed to capture the essential nature and meaning of participants’ experiences [
19]. To undertake this, the relationships between themes were explored. Specifically, cause-and-effect and temporal connections were considered. This data analysis process was captured in tables (labeling) and a word cloud (themes). Additionally, tables with further supporting quotes for each theme were included as
Supplementary Materials for further audibility.
3. Results
Eight adults who identified as having long COVID participated in this study. Two focus groups (FG) were held (FG1 and FG2), and four participants attended each group. All presented as women and Caucasian. All were employed at the beginning of the pandemic, resided in Scotland, and experienced their illness onset between March and April 2020.
The thematic analysis produced five central themes. These include:
“It’s completely changed my life”: A prolonged, varied, and debilitating illness;
Barriers to care, “there’s definitely a gap”;
“Stay away, stay home”: Predominantly negative experiences of care;
Fighting to carry the burden is “a full-time job”;
Looking to the future and “those who come after”.
Each central theme, and their subthemes, are explained in turn. In-text quotations are used to provide evidence and illustrate experiences in participants’ own words. Additional supportive quotes are included in
Supplementary Materials Tables S1–S5. Once central themes are described, thematic relationships are explored, and an overarching theory is developed.
3.1. Central Theme 1: “It’s Completely Changed My Life”: A Prolonged, Varied, and Debilitating Illness
3.1.1. Persistent Symptoms of a Diverse and Fluctuating Nature
Both focus groups discussed the timing of illness onset and the persistent nature of symptoms. One participant noted, “I’m definitely still trying to get well from COVID in March and that’s nearly 7 months” (Denise FG1), while in FG1, Jill stated, “I took not well on the 22nd of April. It’s amazing how we all remember the date”.
Several individuals commented on the fluctuating nature of long COVID. This was described as both illness progression and symptom presentation. Kate from FG1 stated, “I started to feel better day 12 and [by] about day 17 the shortness of breath returned and I again was bedridden. About week four or so I started to get really intense GERD, um indigestion, I’ve never experienced before and then um week 5 I had some heart complications as well”. Similarly, Mary from FG1 noted, “Thankfully it’s never all the symptoms at once but they will rotate …, there’s something all the time”. Though personal experiences varied (see
Table 1), cardiorespiratory effects and fatigue were the most frequently described. Additionally, several participants stated the absence of commonly cited COVID-19 symptoms, such as a cough or fever, further individualizing the illness.
3.1.2. The Impact of Prolonged Illness on Self-Image and Mental Health
The participants’ descriptions of long COVID encompassed elements beyond physical symptoms. For some, as the illness persisted, mental health deteriorated. One individual noted, “… [the] effects of being sick for this long is causing depression in people and anxiety” (Paula FG2). This created an increasingly complex experience for participants managing physical and mental symptoms.
Several individuals noted how long COVID impacted their self-image, with a specific reference to aging occurring. One participated noted, “I need to have a nap every afternoon um, it’s like I’m 90. I feel like I look 90 as well” (Mary FG1), while another focus group participant described how, “There was a person before COVID and it’s not the same person [now]” (Lisa FG2), demonstrating the substantial way illness affected her self-image.
3.2. Central Theme 2: Barriers to Care, “There’s Definitely a Gap”
3.2.1. Ill but Not Enough for Admission
None of the individuals included in this study reported hospital admission for acute illness management. Though several attended accidents and emergency (A&E), their illness was deemed too mild for admission. One participant commented, “It’s almost better to have been so ill that you were in intensive care, because then you get the care” (Amy FG2). Though many acknowledged that healthcare resources were stretched, this lack of treatment was viewed by many a barrier. This additionally created uncertainty regarding how this lack of hospitalization influenced ongoing illness.
3.2.2. Struggling to Navigate Pathways of Care
Multiple elements of the care pathway were identified as barriers to receiving timely treatment and support. Several individuals noted the absence of general practitioner (GP) involvement in their COVID care. This created challenges when GP referrals were required for testing but GP surgeries directed COVID patients to the national COVID hotline. As one participant noted, “As soon as I mention anything about COVID to my GP’s receptionist she immediately says you’re phoning the wrong number” (Florence FG1). Additionally, several participants stated that care was only accessible to them through A&E. One noted, “that shouldn’t have been the pathway, I shouldn’t have had to go to A&E to get things” (Kate FG1).
Several participants also relayed how the lack of a clinical code for COVID prevented healthcare providers from collecting information about their condition. One had been told, “General practitioners are not in a position to collect data on COVID-19 at the moment, because they don’t have a clinical code” (Florence FG1). This barrier prevented GPs from understanding the magnitude of the problem or acknowledging participants’ conditions. These combined factors left participants feeling that the system was neither set up to support them nor to guide them through illness.
3.2.3. Negative Test Results and Unsatisfactory Answers
Participants undertook broad testing to investigate ongoing symptoms. In FG2, Jill stated, “I’ve had two chest X-rays, two ECGs, my bloods have been checked and I’ve had a CT scan. And every single one of them’s normal. So according to all the tests there’s nothing wrong with me”. In FG1, a similar sentiment was expressed by Mary, who recalled, “I’ve been tested for everything, I think, um but that all came back fine, so they discharged me”. However, these results did not match up to participants realities, with one noting, “a lot of people are saying everything is “normal”. When clearly, it’s not normal…”
For all participants, test results have not explained persistent illness, leading some healthcare professionals to propose unsatisfactory explanations. Several participants described how anxiety was proposed to be the root of their symptoms, while others were suggested menopause, “It’s interpreted as anxiety, and especially I think females of a certain age, menopause, anxiety, it’s an easy route to go down” (Denise FG1).
3.3. Central Theme 3: “Stay Away, Stay Home”: Predominantly Negative Experiences of Care
Most participants described feeling unsupported and abandoned by the public healthcare system throughout their illness. One participant recalled her experience as a “[struggle] to get support, struggled to get anyone to basically see me. Um just rest and stay in bed basically I was told, um even though I couldn’t breathe”. (Denise FG1). Several individuals noted the absence of their GPs, with one stating that due to a pre-existing condition she “was in contact with the GP monthly and having lots of support and this support all of sudden stopped um sort of March April time” (Mary FG1). Another participant echoed this sentiment, noting there’s a “chorus of all of us [long COVID patients] saying where have our GPs gone” (Kate FG1).
Participants additionally described incidents of poor communication where they felt their concerns were unheard and their illness was dismissed. One individual stated, “I’ve actually stopped ringing my GP now because the last time, the last words were, it takes a long time to get over a virus” (Denise FG1). A GP who would take ongoing concerns seriously was found by some participants but not all. Ultimately, most participants felt the public healthcare system had no further answer for their ongoing illness.
3.4. Central Theme 4: Fighting to Carry the Burden Is “A Full-Time Job”
3.4.1. Balancing Illness While Striving for Normalcy
Several participants described the burden of living with a new condition that was not widely understood. One individual depicted interactions with the world as a constant fight, noting, “You’re fighting for treatment and fighting to be recognized, and fighting … with family and friends to be understood. Everything’s a fight when it shouldn’t be” (Amy FG2). Ultimately, many felt that the lack of understanding regarding their ongoing experiences imposed an additional burden in returning to their pre-illness state.
Returning to work was discussed by most participants. One noted, “I’m having issues with my employer. I haven’t been able to get back to work” (Paula FG2). Another individual noted how she returned to work too early, stating, “I thought that I should be at work because I wasn’t dying. Not realizing, you know, that [long COVID] was a thing” (Jill FG2). Finally, one participant recalled her experiences as “I’m trying to work from home um at the moment, um but the exhaustion and the concentration levels and the brain fog by lunch time are just ridiculous” (Mary FG1). Returning to their prior activities was important, but many felt the support and understanding to complete this transition were lacking.
3.4.2. Independently Seeking Outside Care
All participants described undertaking extensive efforts to address their illness, which extended beyond public healthcare system engagement. Many individuals had already accessed private medical care to address ongoing symptoms, and others were contemplating paying for this service. One participant stated, “I’ve had to basically pay for support and care” (Denise FG1). Accessing testing, GPs, and treatment through the private sector were commonly shared experiences.
Participants additionally used online communities to identify potential treatments and diagnostic tools. Two participants noted a research tool in Oxford, England, used to diagnose organ damage. One woman noted she “Did get the chance to go down [to the scan]. But I think that says so much, that we would have to travel … to Oxford in order to get seen” (Kate FG1).
3.5. Central Theme 5: Looking to the Future and “Those Who Come After”
Throughout the focus groups, many participants expressed a clear vision for ideal long-COVID care provision. One participant commented if “one or two GPs that want to specialize and maybe they deal with the long haulers and hopefully they can cascade that information…” (Kate FG1). Most expressed the need for a specialized service, with many advocating for a centralized location. This “one-stop shop” model was viewed by many as an appropriate solution to overcome the challenges faced during their illness journey. One individual stated, “There should be a joined-up approach with all of these [services] together because people are suffering from multiple things” (Paula FG2). Several participants felt this solution would overcome challenges regarding diagnostics, treatment, and research dissemination, with one individual noting, “There needs to also be a clear protocol for identifying long-haul patients and approaching treatment” (Kate FG1).
Several individuals also highlighted their wishes for long COVID to be discussed more within society. When referring to the first minister’s COVID briefings, one participant felt, “I think they should be saying how many people have long COVID. Not every day but at least weekly because it’s just being overlooked” (Paula FG2). Many participants expressed their desire to improve services for future individuals. One participant questioned, “Even though they do know about long COVID are they treating people differently?” (Amy FG2).
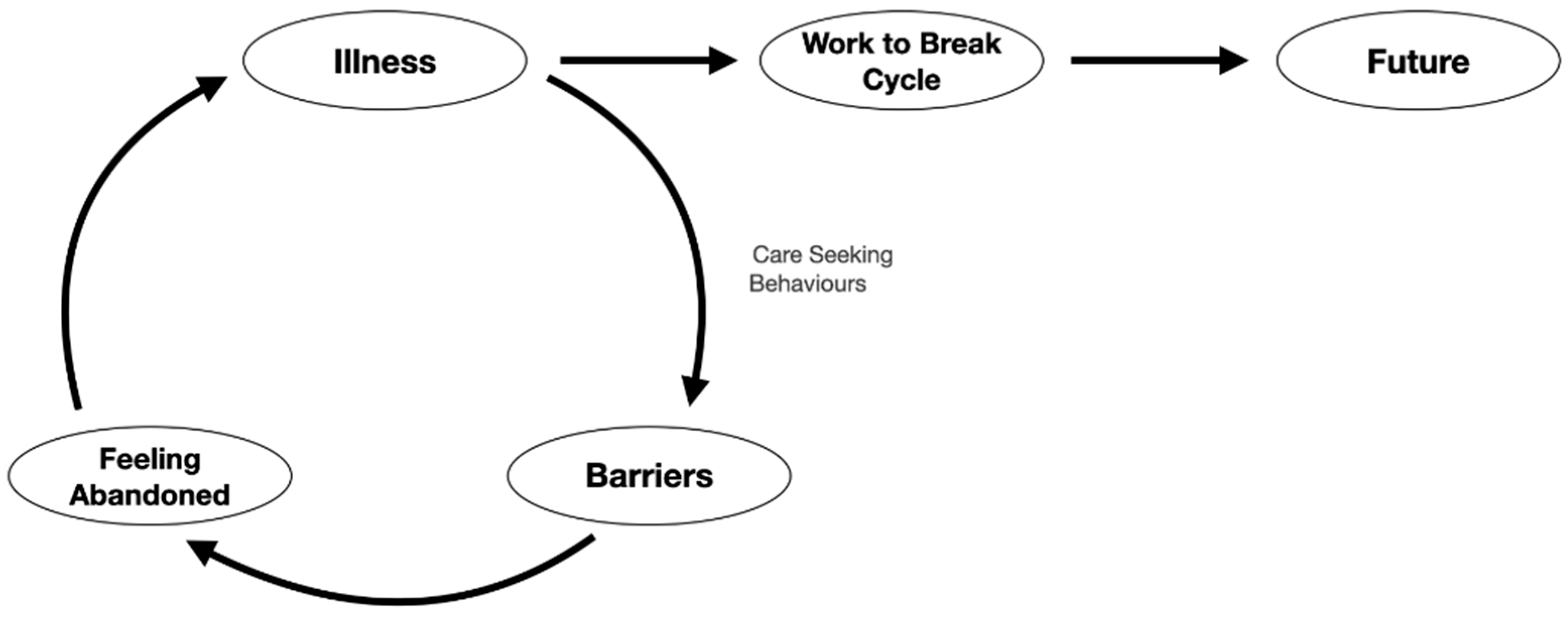
3.6. Theory Development of Central Themes
This paper now presents an overarching theory to describe participants’ experiences. This is performed by exploring the relationships between the five central themes described above.
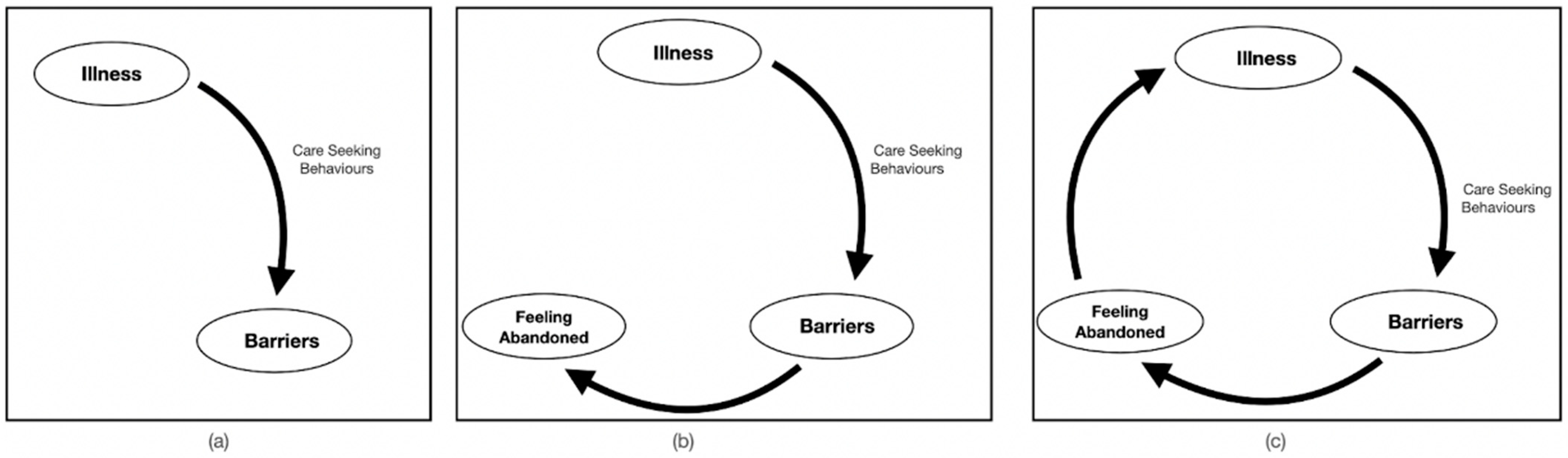
In response to illness, all participants engaged with traditional care-seeking behaviors. One participant highlighted how this experience differed from prior ones, stating, “I have to say last year I had emergency surgery and I had excellent care … so, it’s really shocking to see the difference” (Paula FG2). These unexpected barriers were met when seeking both GP and hospital care and were a direct result of addressing illness (see
Figure 3a). An example barrier was described by one participant as, “My breathing wasn’t considered bad enough, at the time my oxygen saturation levels got down as low as 91 but they said it would [have to] be 89 before they would admit me” (Florence FG1), while Kate from FG1 noted “I actually felt like I should have been in hospital, I would [have] benefited from some oxygen but um 111 was very much keeping people away”.
These care barriers contributed to participants feeling abandoned in their state of illness (see
Figure 3b). These feelings arose both from the care pathway and healthcare interactions. One participant noted, “my GP’s basically admitted they don’t know what to do with me. They can’t refer me anywhere and if my heart rate gets high again, go to accidents and emergency” (Jill FG2). Another participant, who reported to A&E, noted, “I was quite disappointed that they didn’t even see me before they discharged me” (Mary FG1).
Throughout these negative experiences of care, participants remained in their state of illness (see
Figure 3c), with several participants feeling their healthcare interaction has not adequately addressed their needs. One participant noted, “We’ve developed long COVID because we’ve been left to get on with things. Or not get on with things” (Amy FG2). Another participant described how interactions contributed more ailments. She described that, “Early on I didn’t feel any anxiety, but I think every time it was mentioned to me, I started thinking, maybe? You know, I’ll add that to the list of things that I’m struggling with” (Kate FG1).
Figure 3c illustrates the general participant experience during the onset of their illness. Traditional care-seeking behaviors were undertaken to address ongoing symptoms, but these efforts were met with barriers. Persistent barriers contributed to feeling abandoned by the healthcare system. Throughout this process, individuals’ perceived care needs had not been met. Therefore, participants remained in a state of illness, sometimes acquiring additional ailments throughout their experiences.
As participants felt traditional care-seeking behaviors did not address their needs, alternative approaches were undertaken to manage continued illness. Participants chose to engage with society, explaining their condition and advocating for acknowledgement. This was described by one individual as “[the] crux of the issue here is that we’re having to travel, we’re having to educate ourselves, we’re having to advocate for ourselves and I think ultimately, it’s just been hard work and we’re already tired” (Kate FG1).
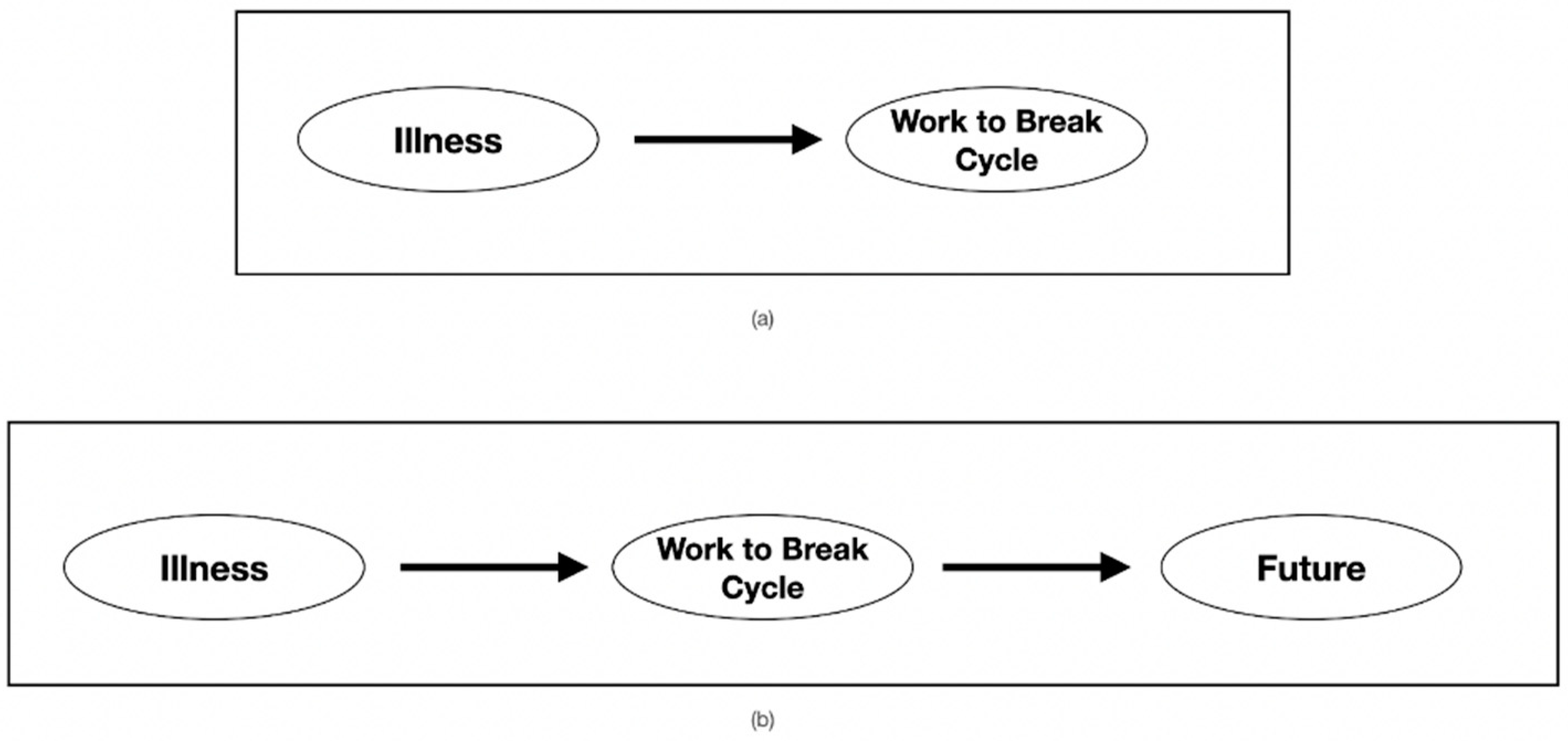
In order to break their cycle of illness and receive what participants felt was necessary care, many accessed private healthcare or alternative treatments (see
Figure 4a). This was viewed by many as the only way to address the illness. One participant noted, “I went to a private doctor because I didn’t know where else to turn” (Denise FG1), while another participant stated, “I have gone private. I had my heart checked privately and it’s OK” (Amy FG2). Seeking alternate care was the only way for many to receive necessary answers. These activities required financial resources, energy, and time to undertake. However, they were viewed by many as the way out of illness and to provide insight into and establish their condition.
Additional work was undertaken by participants in order to address their own health, advocate for establishing long COVID, or to improve the experience for others (see
Figure 4b). One participant noted her motivation to participate in the focus groups as “I’m here because I want it to get recognized and if there’s something that can get done, so I don’t have to just turn myself up to accidents and emergency with my symptoms” (Jill FG2). Another stated her reasons to participate as, “This is very important work, not just to help us, but also for those who undoubtedly will come after us. So thank you all for recognizing us” (Mary FG1). Participants undertook this additional work in a state of illness with visions for a better future in mind.
Figure 5 depicts the overall experience of the focus group participants. Individuals found themselves in a cycle of illness, barriers, and feeling abandoned. Alternative approaches, through care seeking and advocacy, enabled some participants to access the care they needed. This was motivated by their continued state of illness and concern for those who come after.
4. Discussion
Living with an undiagnosed or incompletely understood condition adds complexity to an illness experience [
27]. This complexity was described by the eight focus group participants and is reflected in the above theory. Individuals with long COVID found themselves in a prolonged state of illness where traditional care-seeking behaviors were met with barriers. This created negative feelings while the illness persisted. To access support, participants undertook diverse actions beyond public healthcare system engagement. This was performed to address ongoing illness and out of concern for future long-COVID patients.
This discussion first acknowledges the population and context in which this theory was developed; these both have implications when considering theory applicability. Second, our results are compared with pre-existing qualitative research on long COVID and frameworks encompassing patient experiences. Finally, study limitations, including a critique of an SQDA, will be addressed.
When this study occurred and who participated have implications concerning theory applicability. Recruiting from an online activist group drew individuals who held common experiences of contributing to advocacy and undertaking supplementary activities to address persistent illness. Therefore, this theory may not accurately describe the experience of individuals unable to engage in actions beyond traditional care seeking. Furthermore, this theory represents participants’ experiences at the onset of the COVID-19 pandemic. During this period, the predominant focus of governments, healthcare systems, and media was on acute COVID-19; long COVID received limited attention [
28]. Recently, there has been increased awareness of long COVID, with pathology and management research underway [
29,
30]. Therefore, as the pandemic timeline continues, this theory may no longer be applicable to ongoing experiences.
The thematic results that emerged in this study are consistent with the two prior qualitative studies on individuals’ experiences with long COVID. The first published study on this topic [
31] included interviews with 24 individuals with prolonged COVID-19 symptoms. The analysis revealed similar themes, such as the challenges of persistent illness and finding and accessing appropriate care. However, the theme of fear surrounding recovery or the lack thereof [
31] was less discussed in our focus groups. A second identified study on this topic [
32] contained interviews and focus groups with 114 people with long COVID. Similarly, themes such as problems obtaining care and the difficultly with symptoms being acknowledged emerged. Stigma, which was a central theme in this population [
32], was less prevalent in our sample. However, this relative continuity of experiences across these three studies aids in building a comprehensive picture of long COVID during the pandemic. This is one of several contributions our study adds to the research base.
Our study’s methodological choices and theory development contribute additionally to the large research base. First, at the time of writing, this is the first study to examine long COVID from a phenomenological perspective. Through doing so, a deeper insight into how long COVID impacted participants’ reality was gained. Second, this study proposed an overarching theory describing participants’ experience; theory has been absent from prior studies. Henceforth, this theory can be used by healthcare providers to gain greater insight to a patient’s potential history. As prior interactions with healthcare systems shape future actions [
33], the holistic impact of this illness experience should be considered. Our theory is now explored through pre-existing frameworks on patient experiences.
There are several pre-existing models that illustrate an individual’s experience through illness and receiving care. First, the Patient Experience Framework [
34] describes an individual’s journey from a place of being well to accessing care. This conceptual framework includes elements central to our theory, such as the impact of prior life experiences and healthcare interactions [
34]. However, there is also a key difference, the Patient Experience Framework proposes that an individual remains the same through this process. This deviates from our participants’ narratives, many of whom perceived a shift in self-image. Such a shift has previously been observed in studies exploring people with chronic illness, such as chronic fatigue syndrome or fibromyalgia. For this population, work and social habits, which contribute to identify, were lost, while new perspectives and activities were gained [
35]. Therefore, when considering other models, those that address chronic illness may be more applicable to our population.
Taking on previously unconventional roles and responsibilities to manage chronic illness is illustrated in the Burden of Illness Theory [
36]. This theory describes how those living with a chronic illness are expected to undertake additional work in the oversight of their condition. This may include coordinating care, managing symptom progression, and seeking out potential treatments, all while living in a state of illness [
36]. Though this theory encompasses much of our participants’ self-reported experiences, they additionally had the challenge of advocating for their condition’s existence, furthering the burden.
Study Considerations and Limitations
There are three primary limitations to this study. First, our population consisted of a relatively small and homogeneous sample, with all participants presenting as white women. This study could have been strengthened by including those with diverse ethnic backgrounds; this would aid in applicability. Second, most participants included in this study had not been given a medical diagnosis of COVID-19 or long COVID prior to study participation (please see
Section 2.1). However, this sample provides insight into the experiences of individuals in the early days of the COVID-19 pandemic who advocated for the recognition of this condition. The context of the pandemic also meant that online interviewing was necessary. This may have affected the level of group rapport that formed and therefore the depth of data collected.
Additionally, this research employed an SQDA. The undertaking of an SQDA has raised concern over methodological, theoretical, and ethical factors [
37,
38]. One critique of this method is that data are analyzed though the cultural, political, and social lens of the time and therefore could be misinterpreted with changing norms [
36]. As this analysis was conducted within three months of data collection, concerns of shifting norms are minimal. Though long COVID is receiving greater attention in the public discourse, it is still an emerging condition with limited understanding [
39]. Additionally, four situations are proposed that are appropriate for an SQDA [
40]; an in-depth review is one such situation. As a primary analysis undertook a rapid pragmatic categorization to aid timely reporting, this analysis was intended to provide deeper insight.
Considering the above limitations, future research should seek to explore the experiences of individuals with long COVID who were not captured in this study, specifically women representing diverse ethnic backgrounds. Additionally, as several themes that emerged from this study are similar to those from studies of individuals experiencing chronic noncommunicable illness, such as chronic fatigue syndrome or fibromyalgia, further research should seek to explore commonalities with these incompletely understood conditions.
5. Conclusions
Long COVID is an emerging condition with an incomplete understanding regarding pathology, epidemiology, and clinical management. There has been limited research into the experiences of those living with this illness. Therefore, this qualitative study sought to explore the experiences and perceptions of individuals who identified with the term long COVID. To meet this aim, data were collected by conducting semi-structured focus groups. A thematic analysis employing a phenomenological perspective revealed five central themes: (1) “It’s completely changed my life”: a prolonged, varied, and debilitating illness; (2) barriers to care, “there’s definitely a gap”; (3) “stay away, stay home”: predominantly negative experiences of care; (4) fighting to carry the burden is “a full-time job”; and (5) looking to the future and “those who come after”. An overarching explanatory theory was then proposed. This theory illustrates how participants found themselves in a cycle of illness where care-seeking behaviors were met with barriers, contributing to negative emotions. To break this cycle, participants undertook diverse activities. This was performed in response to their continued illness and out of concern for future long-COVID patients. Several of the thematic results that emerged in our study were consistent with prior qualitative work on long COVID. Additionally, several components described in our theory were consistent with pre-existing frameworks on chronic illness. As we continue to move forward in the pandemic timeline, understanding the holistic experiences of individuals with long COVID will allow for better illness management and healthcare provision.