Time Since Bariatric and Metabolic Surgery Is Associated with Ultra-Processed Food Intake and Food Addiction but Not with Culinary Abilities in Adults
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Aspects
2.2. Study Design
2.3. Sample Size Calculation
2.4. Procedures
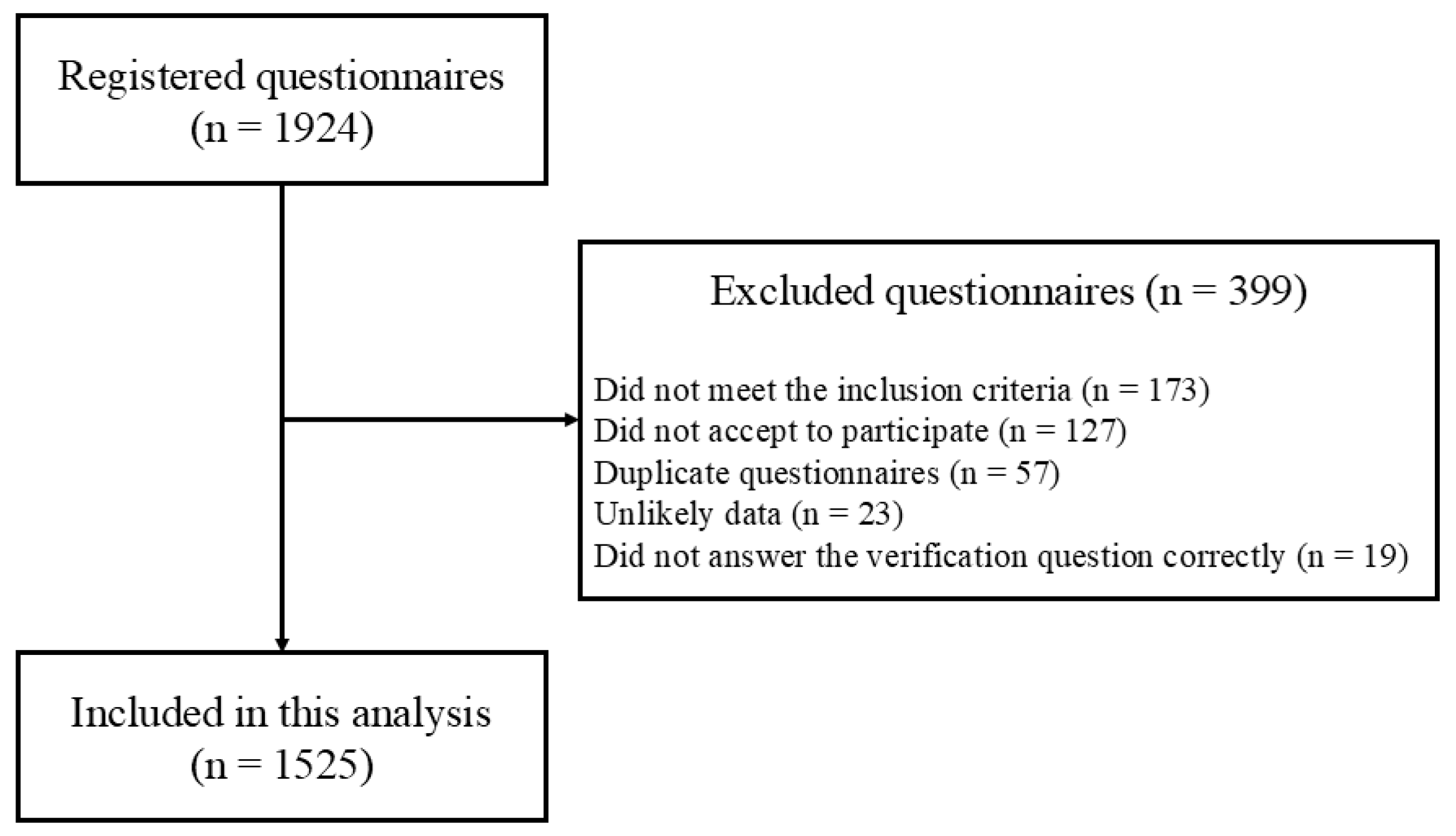
2.5. Recruitment and Sample
2.6. Variables
2.6.1. Exposure
2.6.2. Outcomes
Food Consumption
Ultra-Processed Food Consumption
Culinary Skills
Food Addiction
2.6.3. Additional and Adjustment Data
Social, Demographic, and Clinical Variables
Economic Class
Anthropometry
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. URL World Health Organization. Obesity and Overweight Fact Sheet, 7 May 2025. 2025. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 18 November 2025).
- Ministry of Health. Vigitel Brazil 2023: Surveillance of Risk and Protective Factors for Chronic Diseases by Telephone Survey; Ministry of Health: Brasília, Brazil, 2023. [Google Scholar]
- Araujo, G.B.; Figueiredo, I.H.d.S.; Araujo, B.S.; Oliveira, I.M.M.; Dornelles, C.; Aguiar, J.R.V.; Ferreira, A.R.; Silva, C.V.S.; Araujo, Y.E.L.; Ribeiro, S.E.F.S.; et al. Relationship between overweight and obesity and the development or worsening of chronic non-communicable diseases in adults. Res. Soc. Dev. 2022, 11, e50311225917. [Google Scholar] [CrossRef]
- Goettler, A.; Grosse, A.; Sonntag, D. Productivity loss due to overweight and obesity: A systematic review of indirect costs. BMJ 2017, 7, e014632. [Google Scholar] [CrossRef]
- Kent, S.; Fusco, F.; Gray, A.; Jebb, S.A.; Cairns, B.J.; Mihaylova, B. Body mass index and healthcare costs: A systematic literature review of individual participant data studies. Obes. Rev. 2017, 7, 869–879. [Google Scholar] [CrossRef]
- Nagi, M.A.; Ahmed, H.; Rezq, M.A.A.; Sangroongruangsri, S.; Chaikledkaew, U.; Almalki, Z.; Thavorncharoensap, M. Economic costs of obesity: A systematic review. Int. J. Obes. 2024, 48, 33–43. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.-T.; Minh Nguyet, N.T.; Dinh, T.C.; Lien, N.V.T.; Nguyen, K.-H.; Ngoc, V.T.N.; Tao, Y.; Son, L.H.; Le, D.-H.; Nga, V.B.; et al. An update on physical health and economic consequences of overweight and obesity. Diab. Metab. Syndr. Clin. Res. Rev. 2018, 12, 1095–1100. [Google Scholar] [CrossRef]
- Carter, J.; Husain, F.; Papasavas, P.; Docimo, S.; Albaugh, V.; Aylward, L.; Blalock, C.; Benson-Davies, S.; Clinical Issues Committee of the American Society of Metabolic and Bariatric Surgeons. American Society for Metabolic and Bariatric Surgery review of the body mass index. Surg. Obes. Relat. Dis. 2025, 21, 199–206. [Google Scholar] [CrossRef]
- Eisenberg, D.; Shikora, S.A.; Aarts, E.; Aminian, A.; Angrisani, L.; Cohen, R.V.; Luca, M.d.; Faria, S.L.; Goodpaster, K.P.S.; Haddad, A.; et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obes. Surg. 2023, 33, 3–14, Erratum in Obes. Surg. 2023, 33, 15–16. https://doi.org/10.1007/s11695-022-06369-2. [Google Scholar] [CrossRef]
- Bordalo, L.A.; Teixeira, T.F.S.; Bressan, J.; Mourão, D.M. Bariatric surgery: How and why to supplement. Rev. Assoc. Med. Bras. 2011, 57, 113–120. [Google Scholar] [CrossRef]
- Ghusn, W.; Zeineddine, J.; Betancourt, R.S.; Gajjar, A.; Yang, W.; Robertson, A.G.; Ghanem, O.M. Advances in Metabolic Bariatric Surgeries and Endoscopic Therapies: A Comprehensive Narrative Review of Diabetes Remission Outcomes. Medicina 2025, 61, 350. [Google Scholar] [CrossRef]
- Abi Mosleh, K.; Salameh, Y.; Ghusn, W.; Jawhar, N.; Mundi, M.S.; Collazo-Clavell, M.L.; Kendrick, M.L.; Ghanem, O.M. Impact of metabolic and bariatric surgery on weight loss and insulin requirements in type 1 and insulin-treated type 2 diabetes. Clin. Obes. 2024, 14, e12689. [Google Scholar] [CrossRef]
- Sinclair, P.; Docherty, N.; le Roux, C.W. Metabolic Effects of Bariatric Surgery. Clin. Chem. 2018, 64, 72–81. [Google Scholar] [CrossRef]
- Berino, T.N.; Reis, A.L.; Carvalhal, M.M.L.; Kikuchi, J.L.D.; Teixeira, R.C.R.; Gomes, D.L. Relationship between Eating Behavior, Quality of Life and Weight Regain in Women after Bariatric Surgery. Int. J. Environ. Res. Public Health 2022, 19, 7648. [Google Scholar] [CrossRef]
- Azevedo, E.C.; Diniz, A.S.; Monteiro, J.S.; Cabral, P.C. Dietary risk patterns for non-communicable chronic diseases and their association with body fat—A systematic review. Cien Saude Colet. 2014, 19, 1447–1458. [Google Scholar] [CrossRef]
- Juul, F.; Parekh, N.; Martinez-Steele, E.; Monteiro, C.A.; Chang, V.W. Ultra-processed food consumption among US adults from 2001 to 2018. Am. J. Clin. Nutr. 2022, 115, 211–221. [Google Scholar] [CrossRef]
- Louzada, M.L.C.; Cruz, G.L.; Silva, K.A.A.N.; Grassi, A.G.F.; Andrade, G.C.; Rauber, F.; Levy, R.B.; Monteiro, C.A. Consumption of ultra-processed foods in Brazil: Distribution and temporal evolution 2008–2018. Rev. Saúde Públ. 2023, 57, 12. [Google Scholar] [CrossRef]
- Louzada, M.L.C.; Costa, C.D.S.; Souza, T.N.; Cruz, G.L.; Levy, R.B.; Monteiro, C.A. Impact of the consumption of ultra-processed foods on children, adolescents and adults’ health: Scope review. Cadernos Saúde Públ. 2022, 37, e00323020. [Google Scholar] [CrossRef]
- Pinto, S.L.; Silva, D.C.; Bressan, J. Absolute and Relative Changes in Ultra-processed Food Consumption and Dietary Antioxidants in Severely Obese Adults 3 Months After Roux-en-Y Gastric Bypass. Obes. Surg. 2019, 29, 1810–1815. [Google Scholar] [CrossRef]
- Pinto, S.L.; Juvanhol, L.L.; Bressan, J. Increase in Protein Intake After 3 Months of RYGB Is an Independent Predictor for the Remission of Obesity in the First Year of Surgery. Obes. Surg. 2019, 29, 3780–3785. [Google Scholar] [CrossRef]
- Farias, G.; Silva, R.M.O.; da Silva, P.P.P.; Vilela, R.M.; Bettini, S.C.; Dâmaso, A.R.; Netto, B.D.M. Impact of dietary patterns according to NOVA food groups: 2 y after Roux-en-Y gastric bypass surgery. Nutrition 2020, 74, 110746. [Google Scholar] [CrossRef]
- Lobão, S.L.; Oliveira, A.S.; Bressan, J.; Pinto, S.L. Contribution of Ultra-Processed Foods to Weight Gain Recurrence 5 Years After Metabolic and Bariatric Surgery. Obes. Surg. 2024, 34, 2492–2498. [Google Scholar] [CrossRef]
- Zulin, A.; Rodrigues, T.F.C.S.; Cardoso, L.C.B.; Santos, F.G.T.; Rêgo, A.d.S.; Oliveira, L.D.F.; Radovanovic, C.A.T. Changes that occurred after bariatric surgery: An integrative literature review. Res. Soc. Dev. 2021, 10, e31410313329. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Bueno, N.B.; DiFeliceantonio, A.G.; Roberto, C.A.; Jiménez-Murcia, S.; Fernandez-Aranda, F. Social, clinical, and policy implications of ultra-processed food addiction. BMJ 2023, 383, e075354, Erratum in BMJ 2023, 383, 2679. https://doi.org/10.1136/bmj.p2679. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Corbin, W.R.; Brownell, K.D. Development of the Yale food addiction scale version 2.0. Psychology of addictive behaviors. J. Soc. Psychol. Addict. Behav. 2016, 30, 113–121. [Google Scholar] [CrossRef]
- Pursey, K.M.; Skinner, J.; Leary, M.; Burrows, T. The Relationship between Addictive Eating and Dietary Intake: A Systematic Review. Nutrients 2022, 14, 164. [Google Scholar] [CrossRef]
- Silva Júnior, A.E.D.; Gearhardt, A.N.; Bueno, N.B. Association between food addiction with ultra-processed food consumption and eating patterns in a Brazilian sample. Appetite 2023, 186, 106572. [Google Scholar] [CrossRef]
- LaFata, E.M.; Gearhardt, A.N. Ultra-processed food addiction: An epidemic? Psychother. Psychosom. 2022, 91, 363–372. [Google Scholar] [CrossRef]
- Praxedes, D.R.; Silva-Júnior, A.E.; Macena, M.L.; Gearhardt, A.N.; Bueno, N.B. Prevalence of food addiction among patients undergoing metabolic/bariatric surgery: A systematic review and meta-analysis. Obes. Rev. 2023, 24, e13529. [Google Scholar] [CrossRef]
- Watanabe, J.A.; Nieto, J.A.; Suarez-Diéguez, T.; Silva, M. Influence of culinary skills on ultraprocessed food consumption and Mediterranean diet adherence: An integrative review. Nutrition 2024, 121, 112354. [Google Scholar] [CrossRef]
- Ministry of Health. Dietary Guidelines for the Brazilian Population; Ministry of Health: Brasília, Brazil, 2014. [Google Scholar]
- Wolfson, J.A.; Bleich, S.N. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015, 18, 1397–1406. [Google Scholar] [CrossRef]
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Ministry of Health. Guidelines for Evaluation of Food Consumption Markers in Primary Health Care; Ministry of Health: Brasília, Brazil, 2015. [Google Scholar]
- Costa, C.S.; Faria, F.R.; Gabe, K.T.; Sattamini, I.F.; KhandpurI, N.; Leite, F.H.M.; Steele, E.M.; Louzada, M.L.d.C.; Levy, R.B.; Monteiro, C.A. Nova score for the consumption of ultra-processed foods: Description and performance evaluation in Brazil. Rev. Saude Publ. 2021, 55, 13. [Google Scholar] [CrossRef]
- Martins, C.A.; Baraldi, L.G.; Scagliusi, F.B.; Villar, B.S.; Monteiro, C.A. Cooking Skills Index: Development and reliability assessment. Rev. Nutr. 2019, 32, e180124. [Google Scholar] [CrossRef]
- Schulte, E.M.; Gearhardt, A.N. Development of the Modified Yale Food Addiction Scale Version 2.0. Eur. Eat. Disord. Rev. 2017, 25, 302–308. [Google Scholar] [CrossRef]
- Nunes-Neto, P.R.; Kohler, C.A.; Schuch, F.B.; Solmi, M.; Quevedo, J.; Maes, M.; Murru, A.; Vieta, E.; McIntyre, R.S.; McElroy, S.I.; et al. Psychometric properties of the modified Yale Food Addiction Scale 2.0 in a large Brazilian sample. Braz. J. Psychiatry 2018, 40, 444–448. [Google Scholar] [CrossRef]
- Silva Júnior, A.E.; Bueno, N.B. Comments on the translated version of the modified Yale Food Addiction Scale 2.0 into Brazilian Portuguese. Braz. J. Psychiatry. 2023, 45, 189–199. [Google Scholar] [CrossRef]
- ABEP Brazil Economic Classification Criteria. Available online: http://www.abep.org (accessed on 18 November 2025).
- WHO Expert Committee on Physical Status: The Use and Interpretation of Anthropometry (Ed.) Physical Status: The Use and Interpretation of Anthropometry: Report of a WHO Expert Committee; WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 1995; ISBN 9789241208543.
- Budny, A.; Janczy, A.; Szymanski, M.; Mika, A. Long-Term Follow-Up After Bariatric Surgery: Key to Successful Outcomes in Obesity Management. Nutrients 2024, 16, 4399. [Google Scholar] [CrossRef]
- Guerrero-Pérez, F.; Rojas, N.V.; Sánchez, I.; Munguía, L.; Jiménez-Murcia, S.; Artero, C.; Sobrino, L.; Lazzara, C.; Monseny, R.; Montserrat, M.; et al. Impact of preoperative food addiction on weight loss and weight regain three years after bariatric Surgery. Nutrients 2025, 17, 2114. [Google Scholar] [CrossRef]
- Clark, M.M.; Goetze, R.E.; Howell, L.A.; Grothe, K.B. Psychological assessment and motivational interviewing of patients seeking bariatric and metabolic endoscopic therapies. Tech. Innov. Gastrointest. Endosc. 2020, 22, 120–125. [Google Scholar] [CrossRef]
- Belo, G.D.Q.M.B.; Siqueira, L.T.D.; Melo Filho, D.A.A.; Kreimer, F.; Ramos, V.P.; Ferraz, A.A.B. Predictors of poor follow-up after bariatric surgery. Rev. Col. Bras. Cir. 2018, 45, e1779. [Google Scholar] [CrossRef]
- Scarpellini, E.; Arts, J.; Karamanolis, G.; Laurenius, A.; Siquini, W.; Suzuki, H.; Ukleja, A.; Beek, A.V.; Vanuytsel, T.; Bor, S.; et al. International consensus on the diagnosis and management of dumping syndrome. Nat. Rev. Endocrinol. 2020, 16, 448–466. [Google Scholar] [CrossRef]
- Moslehi, N.; Kamali, Z.; Barzin, M.; Khalaj, A.; Mirmiran, P. Major dietary patterns and their associations with total weight loss and weight loss composition 2–4 years after sleeve gastrectomy. Eur. J. Med. Res. 2024, 29, 417. [Google Scholar] [CrossRef]
- Sundgot-Borgen, C.; Bond, D.S.; Rø, Ø.; Sniehotta, F.; Kristinsson, J.; Kvalem, I.L. Associations of adherence to physical activity and dietary recommendations with weight recurrence 1–5 years after metabolic and bariatric surgery. Surg. Obes. Relat. Dis. 2024, 20, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Nora, C.; Morais, T.; Nora, M.; Coutinho, J.; Carmo, I.; Monteiro, M.P. Sleeve gastrectomy and gastric bypass for the treatment of metabolic syndrome. Rev. Port. Endocrinol. Diabetes Metab. 2016, 11, 23–29. [Google Scholar] [CrossRef]
- Marconi, S.; Covolo, L.; Marullo, M.; Zanini, B.; Viola, G.C.V.; Gelatti, U.; Maroldi, R.; Latronico, N.; Castellano, M. Cooking skills, eating habits and nutrition knowledge among Italian adolescents during COVID-19 pandemic: Sub-analysis from the online survey COALESCENT (Change amOng Italian adoLESCENTs). Nutrients 2023, 15, 4143. [Google Scholar] [CrossRef]
| Total Sample (n = 1525) | 0–6 Months (n = 452) | 6–12 Months (n = 275) | 12–48 Months (n = 414) | >48 Months (n = 384) | p-Value | |
|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Age (years) | 38.53 (8.02) | 35.90 (7.18) a | 38.20 (7.85) b | 38.54 (7.56) c | 41.86 (8.40) d | <0.01 |
| Weight (kg) | 80.85 (17.22) | 92.45 (16.81) a | 77.07 (13.93) b | 70.40 (13.18) c | 81.16 (15.31) d | <0.01 |
| Height (m) | 1.64 (0.07) | 1.64 (0.07) a | 1.64 (0.06) a | 1.63 (0.07) a | 1.64 (0.07) a | 0.41 |
| Body mass index (kg/m2) | 29.97 (5.82) | 34.19 (5.26) a | 28.37 (4.34) b | 26.21 (4.30) c | 30.19 (5.52) d | <0.01 |
| Post BMS time (months) | 37.90 (54.12) | 2.24 (1.63) a | 8.38 (1.72) b | 23.66 (10.22) c | 116.36 (54.97) d | <0.01 |
| Cooking skills index (0–100) | 78.40 (19.33) | 77.91 (19.32) a | 79.55 (19.24) a | 78.27 (19.15) a | 78.29 (19.62) a | 0.73 |
| Number of FA symptoms | 2.42 (2.98) | 3.65 (3.27) a | 2.23 (2.81) b | 1.40 (2.30) c | 2.22 (2.91) b | <0.01 |
| Nova-UPF Score | 2.75 (2.19) | 1.51 (1.56) a | 2.75 (1.78) b | 3.41 (2.28) c | 3.48 (2.34) c | <0.01 |
| n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Sex (Female) | 1458 (95.6) | 430 (95.1) a | 265 (96.4) a | 391 (94.4) a | 372 (96.9) a | 0.33 |
| Economic class | 0.27 | |||||
| A | 138 (9.0) | 48 (10.6) a | 22 (8.0) a | 31 (7.5) a | 37 (9.6) a | |
| B1 | 282 (18.5) | 69 (15.3) a | 46 (16.7) a,b | 79 (19.1) a,b | 88 (22.9) b | |
| B2 | 633 (41.5) | 185 (40.9) a,b | 128 (46.5) b | 181 (43.7) a,b | 139 (36.2) a | |
| C1 | 340 (22.3) | 108 (23.9) a | 57 (20.7) a | 91 (22.0) a | 84 (21.9) a | |
| C2 | 117 (7.7) | 39 (8.6) a | 19 (6.9) a | 28 (6.8) a | 31 (8.1) a | |
| D-E | 15 (1.0) | 3 (0.7) a | 3 (1.1) a | 4 (1.0) a | 5 (1.3) a | |
| Surgical technique | <0.01 | |||||
| Sleeve gastrectomy | 319 (20.9) | 111 (24.6) a | 78 (28.4) a | 93 (22.5) a | 37 (9.6) b | |
| RYGB | 1206 (79.1) | 341 (75.4) a | 197 (71.6) a | 321 (77.5) a | 347 (90.4) b | |
| FA diagnosis | 392 (25.7) | 189 (41.8) a | 64 (23.3) b | 51 (12.3) c | 88 (22.9) b | <0.01 |
| Fresh fruits | 1001 (65.6) | 313 (69.2) a | 198 (72.0) a | 270 (65.2) a,b | 220 (57.3) b | <0.01 |
| Vegetables | 1123 (73.6) | 329 (72.8) a | 211 (76.7) a | 314 (75.8) a | 269 (70.1) a | 0.16 |
| Beans | 823 (54.0) | 218 (48.2) a | 161 (58.5) b | 228 (55.1) a,b | 216 (56.3) a,b | 0.02 |
| Hamburger and/or sausages | 358 (23.5) | 45 (10.0) a | 66 (24.0) b | 124 (30.0) b | 123 (32.0) b | <0.01 |
| Sweetened beverages | 423 (27.7) | 39 (8.6) a | 80 (29.1) b | 150 (36.2) b,c | 154 (40.1) c | <0.01 |
| Instant noodles, packaged snacks, and/or salty cookies | 228 (15.0) | 37 (8.2) a | 45 (16.4) b | 77 (18.6) b | 69 (18.0) b | < 0.01 |
| Sandwich cookies, sweets, and/or treats | 438 (28.7) | 49 (10.8) a | 73 (26.5) b | 175 (42.3) c | 141 (36.7) c | <0.01 |
| Univariable Analysis | Multivariable Analysis 1 | |||
|---|---|---|---|---|
| β | CI95% | β | CI95% | |
| Cooking skills index | 0.04 | −0.79; 0.87 | −0.41 | −1.33; 0.50 |
| Number of FA symptoms | −0.55 | −0.68; −0.42 | −0.31 | −0.45; −0.17 |
| Nova-UPF Score | 0.68 | 0.59; 0.76 | 0.67 | 0.57; 0.76 |
| Univariable Analysis | Multivariable Analysis 1 | |||||
|---|---|---|---|---|---|---|
| 6–12 Months (n = 275) | 12–48 Months (n = 414) | >48 Months (n = 384) | 6–12 Months (n = 275) | 12–48 Months (n = 414) | >48 Months (n = 384) | |
| PR 2 [CI95%] | PR 2 [CI95%] | PR 2 [CI95%] | PR 2 [CI95%] | PR 2 [CI95%] | PR 2 [CI95%] | |
| FA diagnosis | 0.55 [0.43; 0.70] | 0.29 [0.22; 0.38] | 0.54 [0.44; 0.67] | 0.69 [0.53; 0.90] | 0.39 [0.29; 0.54] | 0.63 [0.50; 0.80] |
| Fresh fruits | 1.04 [0.94; 1.14] | 0.94 [0.85; 1.03] | 0.82 [0.74; 0.92] | 0.93 [0.84; 1.04] | 0.81 [0.73; 0.91] | 0.74 [0.66; 0.83] |
| Vegetables | 1.05 [0.96; 1.14] | 1.04 [0.96; 1.12] | 0.96 [0.88; 1.04] | 1.03 [0.94; 1.13] | 1.00 [0.91; 1.10] | 0.92 [0.84; 1.01] |
| Beans | 1.21 [1.05; 1.39] | 1.14 [1.00; 1.29] | 1.16 [1.02; 1.32] | 1.19 [1.02; 1.38] | 1.09 [0.94; 1.27] | 1.15 [1.00; 1.32] |
| Hamburger and/or sausages | 2.41 [1.70; 3.41] | 3.00 [2.19; 4.11] | 3.21 [2.35; 4.40] | 2.54 [1.74; 3.71] | 3.14 [2.18; 4.52] | 3.42 [2.44; 4.81] |
| Sweetened beverages | 3.37 [2.37; 4.79] | 4.19 [3.03; 5.81] | 4.64 [3.36; 6.42] | 3.67 [2.52; 5.33] | 4.64 [3.22; 6.69] | 5.00 [3.55; 7.04] |
| Instant noodles, packaged snacks, and/or salty cookies | 1.99 [1.32; 3.00] | 2.27 [1.57; 3.28] | 2.19 [1.50; 3.19] | 2.15 [1.37; 3.35] | 2.46 [1.58; 3.84] | 2.31 [1.54; 3.48] |
| Sandwich cookies, sweets, and/or treats | 2.44 [1.76; 3.40] | 3.89 [2.92; 5.19] | 3.38 [2.52; 4.55] | 2.53 [1.78; 3.60] | 4.01 [2.88; 5.57] | 3.58 [2.62; 4.90] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva-Júnior, A.E.d.; Lopes, N.G.d.S.; Melo, J.M.F.; da Silva, M.C.T.F.; Macena, M.d.L.; Bueno, N.B. Time Since Bariatric and Metabolic Surgery Is Associated with Ultra-Processed Food Intake and Food Addiction but Not with Culinary Abilities in Adults. Obesities 2025, 5, 85. https://doi.org/10.3390/obesities5040085
Silva-Júnior AEd, Lopes NGdS, Melo JMF, da Silva MCTF, Macena MdL, Bueno NB. Time Since Bariatric and Metabolic Surgery Is Associated with Ultra-Processed Food Intake and Food Addiction but Not with Culinary Abilities in Adults. Obesities. 2025; 5(4):85. https://doi.org/10.3390/obesities5040085
Chicago/Turabian StyleSilva-Júnior, André Eduardo da, Natália Gomes da Silva Lopes, Jennifer Mikaella Ferreira Melo, Maria Clara Tavares Farias da Silva, Mateus de Lima Macena, and Nassib Bezerra Bueno. 2025. "Time Since Bariatric and Metabolic Surgery Is Associated with Ultra-Processed Food Intake and Food Addiction but Not with Culinary Abilities in Adults" Obesities 5, no. 4: 85. https://doi.org/10.3390/obesities5040085
APA StyleSilva-Júnior, A. E. d., Lopes, N. G. d. S., Melo, J. M. F., da Silva, M. C. T. F., Macena, M. d. L., & Bueno, N. B. (2025). Time Since Bariatric and Metabolic Surgery Is Associated with Ultra-Processed Food Intake and Food Addiction but Not with Culinary Abilities in Adults. Obesities, 5(4), 85. https://doi.org/10.3390/obesities5040085






