Anthropometric and Body Composition Changes over Five Years after Bariatric Surgery in Patients with Obesity, Diagnosed or Not Diagnosed with Binge Eating Disorder (BED) in the Preoperative Period
Abstract
1. Introduction
2. Materials and Methods
2.1. Anthropometric and Body Composition Assessment
2.2. Psychiatric Evaluation
2.3. Binge Eating Scale (BES)
2.4. Beck Depression Inventory (BDI)
2.5. Beck Anxiety Inventory (BAI)
2.6. Statistical Analysis
3. Results
3.1. Sociodemographic, Anthropometric, and Body Composition Data
3.2. Depression and Anxiety Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. PharmacoEconomics 2015, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Kelly, T.; Yang, W.; Chen, C.-S.; Reynolds, K.; He, J. Global burden of obesity in 2005 and projections to 2030. Int. J. Obes. 2008, 32, 1431–1437. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef] [PubMed]
- Cossrow, N.; Pawaskar, M.; Witt, E.A.; Ming, E.E.; Victor, T.W.; Herman, B.K.; Wadden, T.A.; Erder, M.H. Estimating the Prevalence of Binge Eating Disorder in a Community Sample From the United States: Comparing DSM-IV-TR and DSM-5 Criteria. Br. J. Psychol. 2016, 77, e968–e974. [Google Scholar] [CrossRef]
- Agüera, Z.; Lozano-Madrid, M.; Mallorquí-Bagué, N.; Jiménez-Murcia, S.; Menchón, J.M.; Fernández-Aranda, F. A review of binge eating disorder and obesity. Neuropsychiatrie 2021, 35, 57–67. [Google Scholar] [CrossRef]
- American Psychiatric Association; American Psychiatric Association. DSM-5 Task Force. In Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Nonino, C.B.; Barato, M.; Ferreira, F.C.; Delfino, H.B.P.; Noronha, N.Y.; Nicoletti, C.F.; Junior, W.S.; Welendorf, C.R.; Souza, D.R.S.; Ferreira-Julio, M.A.; et al. DRD2 and BDNF polymorphisms are associated with binge eating disorder in patients with weight regain after bariatric surgery. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2021, 27, 1505–1512. [Google Scholar] [CrossRef]
- Treasure, J.; Claudino, A.M.; Zucker, N. Eating disorders. Lancet 2010, 375, 583–593. [Google Scholar] [CrossRef]
- Leehr, E.J.; Krohmer, K.; Schag, K.; Dresler, T.; Zipfel, S.; Giel, K.E. Emotion regulation model in binge eating disorder and obesity—A systematic review. Neurosci. Biobehav. Rev. 2015, 49, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Sansone, R.A.; Schumacher, D.; Wiederman, M.W.; Routsong-Weichers, L. The prevalence of binge eating disorder and borderline personality symptomatology among gastric surgery patients. Eat. Behav. 2008, 9, 197–202. [Google Scholar] [CrossRef]
- Kalarchian, M.A.; Marcus, M.D.; Levine, M.D.; Courcoulas, A.P.; Pilkonis, P.A.; Ringham, R.M.; Soulakova, J.N.; Weissfeld, L.A.; Rofey, D.L. Psychiatric disorders among bariatric surgery candidates: Relationship to obesity and functional health status. Am. J. Psychiatry 2007, 164, 328–334. [Google Scholar] [CrossRef]
- Dawes, A.J.; Maggard-Gibbons, M.; Maher, A.R.; Booth, M.J.; Miake-Lye, I.; Beroes, J.M.; Shekelle, P.G. Mental Health Conditions Among Patients Seeking and Undergoing Bariatric Surgery: A Meta-analysis. JAMA 2016, 315, 150–163. [Google Scholar] [CrossRef] [PubMed]
- Jones-Corneille, L.R.; Wadden, T.A.; Sarwer, D.B.; Faulconbridge, L.F.; Fabricatore, A.N.; Stack, R.M.; Cottrell, F.A.; Pulcini, M.E.; Webb, V.L.; Williams, N.N. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: Results of structured clinical interviews. Obes. Surg. 2012, 22, 389–397. [Google Scholar] [CrossRef] [PubMed]
- King, W.C.; Hinerman, A.S.; Belle, S.H.; Wahed, A.S.; Courcoulas, A.P. Comparison of the Performance of Common Measures of Weight Regain after Bariatric Surgery for Association with Clinical Outcomes. JAMA 2018, 320, 1560–1569. [Google Scholar] [CrossRef]
- Sarwer, D.B.; Wadden, T.A.; Fabricatore, A.N. Psychosocial and behavioral aspects of bariatric surgery. Obes. Res. 2005, 13, 639–648. [Google Scholar] [CrossRef]
- Gormally, J.; Black, S.; Daston, S.; Rardin, D. The assessment of binge eating severity among obese persons. Addict. Behav. 1982, 7, 47–55. [Google Scholar] [CrossRef]
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Grupski, A.E.; Hood, M.M.; Hall, B.J.; Azarbad, L.; Fitzpatrick, S.L.; Corsica, J.A. Examining the Binge Eating Scale in screening for binge eating disorder in bariatric surgery candidates. Obes. Surg. 2013, 23, 1–6. [Google Scholar] [CrossRef]
- Mitchell, J.E.; King, W.C.; Courcoulas, A.; Dakin, G.; Elder, K.; Engel, S.; Flum, D.; Kalarchian, M.; Khandelwal, S.; Pender, J.; et al. Eating behavior and eating disorders in adults before bariatric surgery. Int. J. Eat. Disord. 2015, 48, 215–222. [Google Scholar] [CrossRef]
- Cella, S.; Fei, L.; D’amico, R.; Giardiello, C.; Allaria, A.; Cotrufo, P. Binge Eating Disorder and Related Features in Bariatric Surgery Candidates. Open Med. 2019, 14, 407–415. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Untangling Waist Circumference and Hip Circumference from Body Mass Index with a Body Shape Index, Hip Index, and Anthropometric Risk Indicator. Metab. Syndr. Relat. Disord. 2018, 16, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Maleckas, A.; Gudaitytė, R.; Petereit, R.; Venclauskas, L.; Veličkienė, D. Weight regain after gastric bypass: Etiology and treatment options. Gland. Surg. 2016, 5, 617–624. [Google Scholar] [CrossRef]
- Acevedo, M.B.; Teran-Garcia, M.; Bucholz, K.K.; Eagon, J.C.; Bartholow, B.D.; Burd, N.A.; Khan, N.; Rowitz, B.; Pepino, M.Y. Alcohol sensitivity in women after undergoing bariatric surgery: A cross-sectional study. Surg. Obes. Relat. Dis. 2020, 16, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Kushner, R.F.; Sorensen, K.W. Prevention of Weight Regain Following Bariatric Surgery. Curr. Obes. Rep. 2015, 4, 198–206. [Google Scholar] [CrossRef] [PubMed]
- McGarrity, L.A.; Perry, N.S.; Derbidge, C.M.; Trapp, S.K.; Terrill, A.L.; Smith, T.W.; Ibele, A.R.; MacKenzie, J.J. Associations Between Approach and Avoidance Coping, Psychological Distress, and Disordered Eating Among Candidates for Bariatric Surgery. Obes. Surg. 2019, 29, 3596–3604. [Google Scholar] [CrossRef]
- Gravani, S.; Matiatou, M.; Nikolaidis, P.T.; Menenakos, E.; Zografos, C.G.; Zografos, G.; Albanopoulos, K. Anxiety and Depression Affect Early Postoperative Pain Dimensions after Bariatric Surgery. J. Clin. Med. 2020, 10, 53. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; White, M.A.; Masheb, R.M. DSM-IV psychiatric disorder comorbidity and its correlates in binge eating disorder. Int. J. Eat. Disord. 2009, 42, 228–234. [Google Scholar] [CrossRef]
- Azarbad, L.; Corsica, J.; Hall, B.; Hood, M. Psychosocial correlates of binge eating in Hispanic, African American, and Caucasian women presenting for bariatric surgery. Eat. Behav. 2010, 11, 79–84. [Google Scholar] [CrossRef]
- Peterson, R.E.; Latendresse, S.J.; Bartholome, L.T.; Warren, C.S.; Raymond, N.C. Binge Eating Disorder Mediates Links between Symptoms of Depression, Anxiety, and Caloric Intake in Overweight and Obese Women. J. Obes. 2012, 2012, 407103. [Google Scholar] [CrossRef]
- Khorgami, Z.; Zhang, C.; Messiah, S.E.; de la Cruz-Muñoz, N. Predictors of Postoperative Aftercare Attrition among Gastric Bypass Patients. Bariatr. Surg. Pract. Patient Care 2015, 10, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Harper, J.; Madan, A.K.; Ternovits, C.A.; Tichansky, D.S. What happens to patients who do not follow-up after bariatric surgery? Am. Surg. 2007, 73, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Higa, K.; Ho, T.; Tercero, F.; Yunus, T.; Boone, K.B. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg. Obes. Relat. Dis. 2011, 7, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Lujan, J.; Tuero, C.; Landecho, M.F.; Moncada, R.; Cienfuegos, J.A.; Rotellar, F.; Silva, C.; Lapuente, F.; Martínez, P.; Frühbeck, G.; et al. Impact of Routine and Long-Term Follow-Up on Weight Loss after Bariatric Surgery. Obes. Surg. 2020, 30, 4293–4299. [Google Scholar] [CrossRef]
- Meany, G.; Conceição, E.; Mitchell, J.E. Binge eating, binge eating disorder and loss of control eating: Effects on weight outcomes after bariatric surgery. Eur. Eat. Disord. Rev. 2014, 22, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Pekkarinen, T.; Koskela, K.; Huikuri, K.; Mustajoki, P. Long-Term Results of Gastroplasty for Morbid Obesity: Binge-Eating as a Predictor of Poor Outcome. Obes. Surg. 1994, 4, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Kofman, M.D.; Lent, M.R.; Swencionis, C. Maladaptive eating patterns, quality of life, and weight outcomes following gastric bypass: Results of an Internet survey. Obesity 2010, 18, 1938–1943. [Google Scholar] [CrossRef] [PubMed]
- Barbuti, M.; Carignani, G.; Weiss, F.; Calderone, A.; Fierabracci, P.; Salvetti, G.; Menculini, G.; Tortorella, A.; Santini, F.; Perugi, G. Eating disorders and emotional dysregulation are associated with insufficient weight loss after bariatric surgery: A 1-year observational follow-up study. Eat. Weight Disord.-Stud. Anorex. Bulim. Obes. 2023, 28, 49. [Google Scholar] [CrossRef]
- Hilbert, A.; Petroff, D.; Herpertz, S.; Pietrowsky, R.; Tuschen-Caffier, B.; Vocks, S.; Schmidt, R. Meta-analysis of the efficacy of psychological and medical treatments for binge-eating disorder. J. Consult. Clin. Psychol. 2019, 87, 91–105. [Google Scholar] [CrossRef]
- Bianciardi, E.; Raimondi, G.; Samela, T.; Innamorati, M.; Contini, L.M.; Procenesi, L.; Fabbricatore, M.; Imperatori, C.; Gentileschi, P. Neurocognitive and Psychopathological Predictors of Weight Loss After Bariatric Surgery: A 4-Year Follow-Up Study. Front. Endocrinol. 2021, 12, 662252. [Google Scholar] [CrossRef]
| Variables | With BED | Without BED | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n = 61 | n = 57 | |||||||||
| Sociodemographic | n | % | n | % | ||||||
| Female | 53 | 86.9 | 44 | 77.2 | 0.07 | |||||
| Male | 8 | 13.1 | 13 | 22.8 | ||||||
| Anthropometric | Preoperative | PO 1 | PO 2 | Preoperative | PO 1 | PO 2 | ||||
| M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | |||||
| Age (years) | 40.1 ± 9.9 | - | - | 39.0 ± 10.5 | - | - | 0.58 | |||
| Weight (kg) | 133.4 ± 23.0 | 83.5 ± 15.5 ** | 92.6 ± 16.5 *** | 132.4 ± 27.3 | 86.5 ± 19.6 ** | 94.2 ± 20.8 | # | |||
| Height (m) | 1.63 ± 0.09 | - | - | 1.65 ± 0.09 | - | - | 0.23 | |||
| BMI (kg/m2) | 51.0 ± 7.9 | 32.1 ± 5.7 *** | 34.3 ± 7.2 ** | 50.2 ± 8.2 | 32.4 ± 5.6 *** | 32.8 ± 10.6 | # | |||
| Ideal weight (kg) | 66.7 ± 7.4 | - | - | 68.3 ± 7.3 | - | - | 0.23 | |||
| Overweight (kg) | 29.5 ± 22.0 | - | - | 23.4 ± 20.1 | - | - | 0.42 | |||
| Regain (%) | - | - | 18.8 ± 23.2 | - | - | 9.1 ± 38.7 | 0.32 | |||
| WC-F (cm) | 137.6 ± 27.0 | 101.5 ± 12.4 * | 107.1 ± 10.8 | 141.1 ± 15.1 | 111.5 ± 13.1 *** | 102.0 ± 17.6 | # | |||
| WC-M (cm) | 155.9 ± 16.0 | 111.6 ± 13.2 *** | 119.0 ± 9.9 | 155.9 ± 16.0 | 111.6 ± 13.2 ** | 119.0 ± 9.9 | # | |||
| LM (kg) | 66.9 ± 16.4 | 55.4 ± 10.9 * | 56.6 ± 13.0 | 70.2 ± 15.1 | 55.6 ± 9.9 *** | 52.2 ± 6.9 | # | |||
| LM (%) | 51.1 ± 8.1 | 67.7 ± 10.2 *** | 65.5 ± 4.6 | 52.1 ± 6.9 | 67.6 ± 10.3 * | 66.6 ± 13.1 | # | |||
| FM (kg) | 70.8 ± 18.9 | 31.6 ± 14.7 *** | 35.9 ± 12.4 | 67.9 ± 15.4 | 26.3 ± 13.0 *** | 27.5 ± 14.6 | # | |||
| FM (%) | 51.14 ± 8.99 | 33.31 ± 7.63 *** | 36.59 ± 4.79 | 47.58 ± 7.99 | 30.56 ± 10.63 * | 33.37 ± 13.1 | # | |||
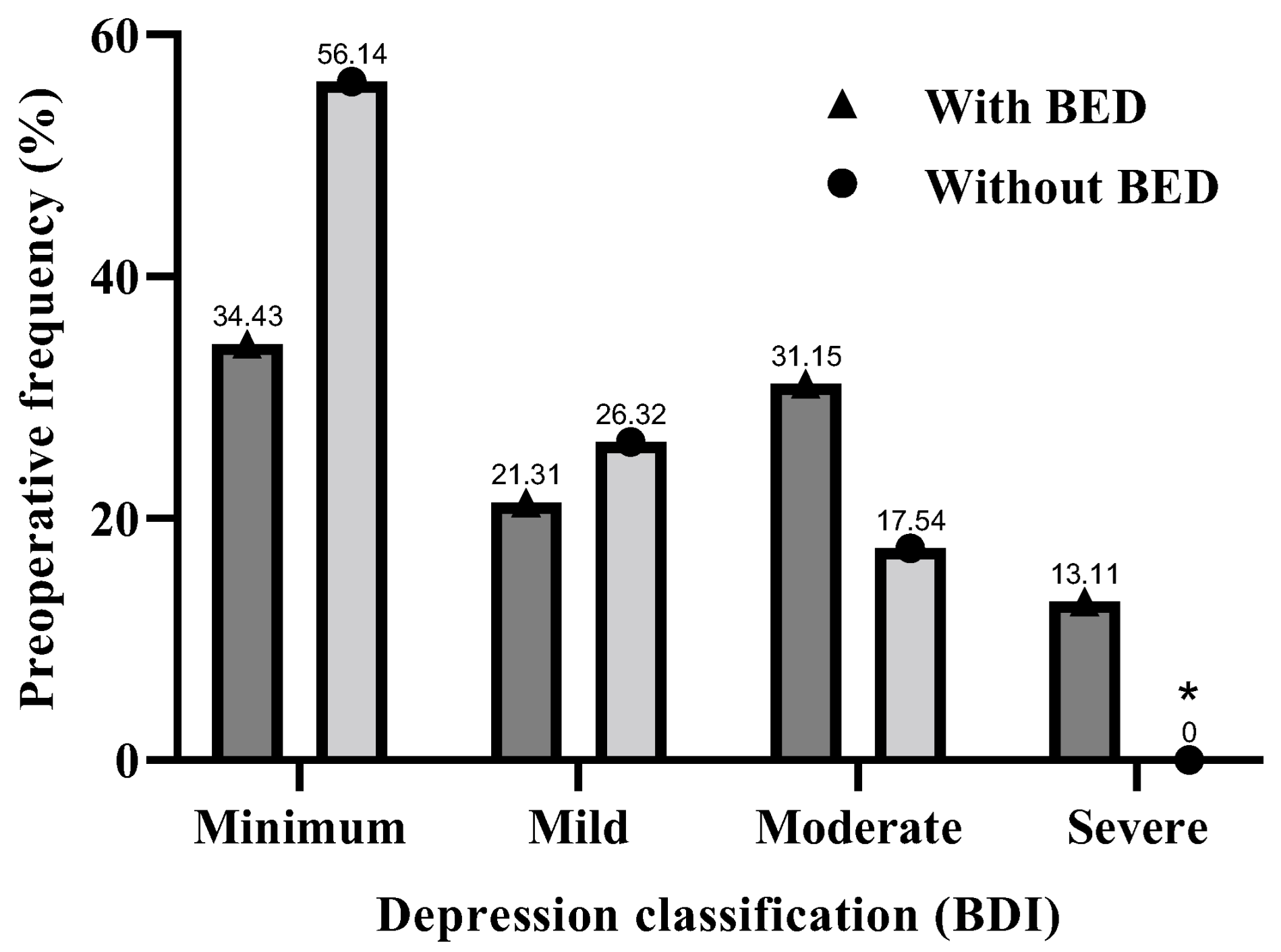
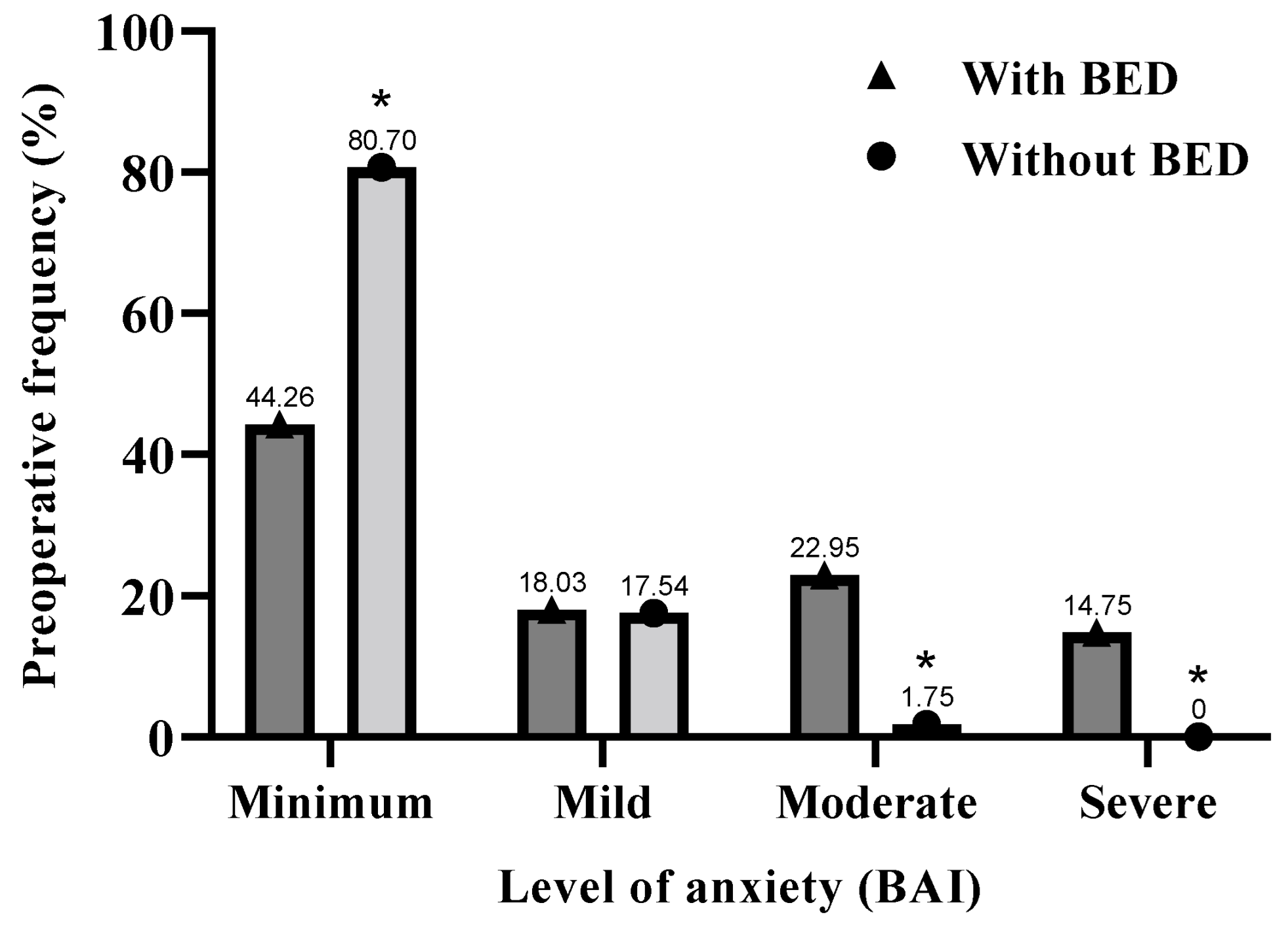
| Variables | BDI with BED n = 61 | BDI without BED n = 57 | p-Value | BAI with BED n = 61 | BAI without BED n = 57 | p-Value |
|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | |||
| Preoperative | 18.9 ± 12.9 ** | 11.6 ± 7.9 | 0.0082 | 15.7 ± 11.0 *** | 6.6 ± 5.2 | <0.0001 |
| Average rating | Mild | Minimum | Mild | Minimum |
| Variables | BDI with BED n = 61 | BDI without BED n = 57 | p-Value (OR/CI) | BAI with BED n = 61 | BAI without BED n = 57 | p-Value (OR/CI) |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Minimum | 21 (34.43) | 32 (56.14) | 0.14 | 27 * (44.26) | 46 (80.70) | 0.0475 |
| (1.63/0.84–3.11) | (1.82/1.01–3.24) | |||||
| Mild | 13 (21.32) | 15 (26.32) | 0.62 | 11 (18.03) | 10 (17.54) | 0.95 |
| (1.24/0.55–2.87) | (0.97/0.37–2.46) | |||||
| Moderate | 19 (31.15) | 10 (17.54) | 0.18 | 14 ** (22.95) | 1 (1.75) | 0.0022 |
| (0.56/0.24–1.29) | (0.07/0.007–0.51) | |||||
| Severe | 8 ** (13.11) | 0 (0.0) | 0.0079 | 9 ** (14.75) | 0 (0.0) | 0.005 |
| (0.00/0.00–0.52) | (0.00/0.00–0.44) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delfino, H.B.P.; Pinhel, M.A.d.S.; Ferreira, F.C.; Nicoletti, C.F.; de Oliveira, S.T.P.; Baumgartner, L.B.B.; Welendorf, C.R.; Pastore, T.A.d.A.C.; Malek-Zadeh, C.H.; Watanabe, L.M.; et al. Anthropometric and Body Composition Changes over Five Years after Bariatric Surgery in Patients with Obesity, Diagnosed or Not Diagnosed with Binge Eating Disorder (BED) in the Preoperative Period. Obesities 2024, 4, 55-65. https://doi.org/10.3390/obesities4020006
Delfino HBP, Pinhel MAdS, Ferreira FC, Nicoletti CF, de Oliveira STP, Baumgartner LBB, Welendorf CR, Pastore TAdAC, Malek-Zadeh CH, Watanabe LM, et al. Anthropometric and Body Composition Changes over Five Years after Bariatric Surgery in Patients with Obesity, Diagnosed or Not Diagnosed with Binge Eating Disorder (BED) in the Preoperative Period. Obesities. 2024; 4(2):55-65. https://doi.org/10.3390/obesities4020006
Chicago/Turabian StyleDelfino, Heitor Bernardes Pereira, Marcela Augusta de Souza Pinhel, Flávia Campos Ferreira, Carolina Ferreira Nicoletti, Sofia Teixeira Prates de Oliveira, Lidia Barbieri Belarmino Baumgartner, Caroline Rossi Welendorf, Thaís Alves de Azevedo Chaves Pastore, Carolina Hunger Malek-Zadeh, Ligia Moriguchi Watanabe, and et al. 2024. "Anthropometric and Body Composition Changes over Five Years after Bariatric Surgery in Patients with Obesity, Diagnosed or Not Diagnosed with Binge Eating Disorder (BED) in the Preoperative Period" Obesities 4, no. 2: 55-65. https://doi.org/10.3390/obesities4020006
APA StyleDelfino, H. B. P., Pinhel, M. A. d. S., Ferreira, F. C., Nicoletti, C. F., de Oliveira, S. T. P., Baumgartner, L. B. B., Welendorf, C. R., Pastore, T. A. d. A. C., Malek-Zadeh, C. H., Watanabe, L. M., Noronha, N. Y., Salgado Junior, W., & Nonino, C. B. (2024). Anthropometric and Body Composition Changes over Five Years after Bariatric Surgery in Patients with Obesity, Diagnosed or Not Diagnosed with Binge Eating Disorder (BED) in the Preoperative Period. Obesities, 4(2), 55-65. https://doi.org/10.3390/obesities4020006







