The Burden of Weight on Joint Replacement: A 1.6 Million-Patient Analysis of BMI and Hip Arthroplasty Outcomes
Abstract
1. Introduction
Research Questions
2. Methods
2.1. Data Source
2.2. Study Population and Variables
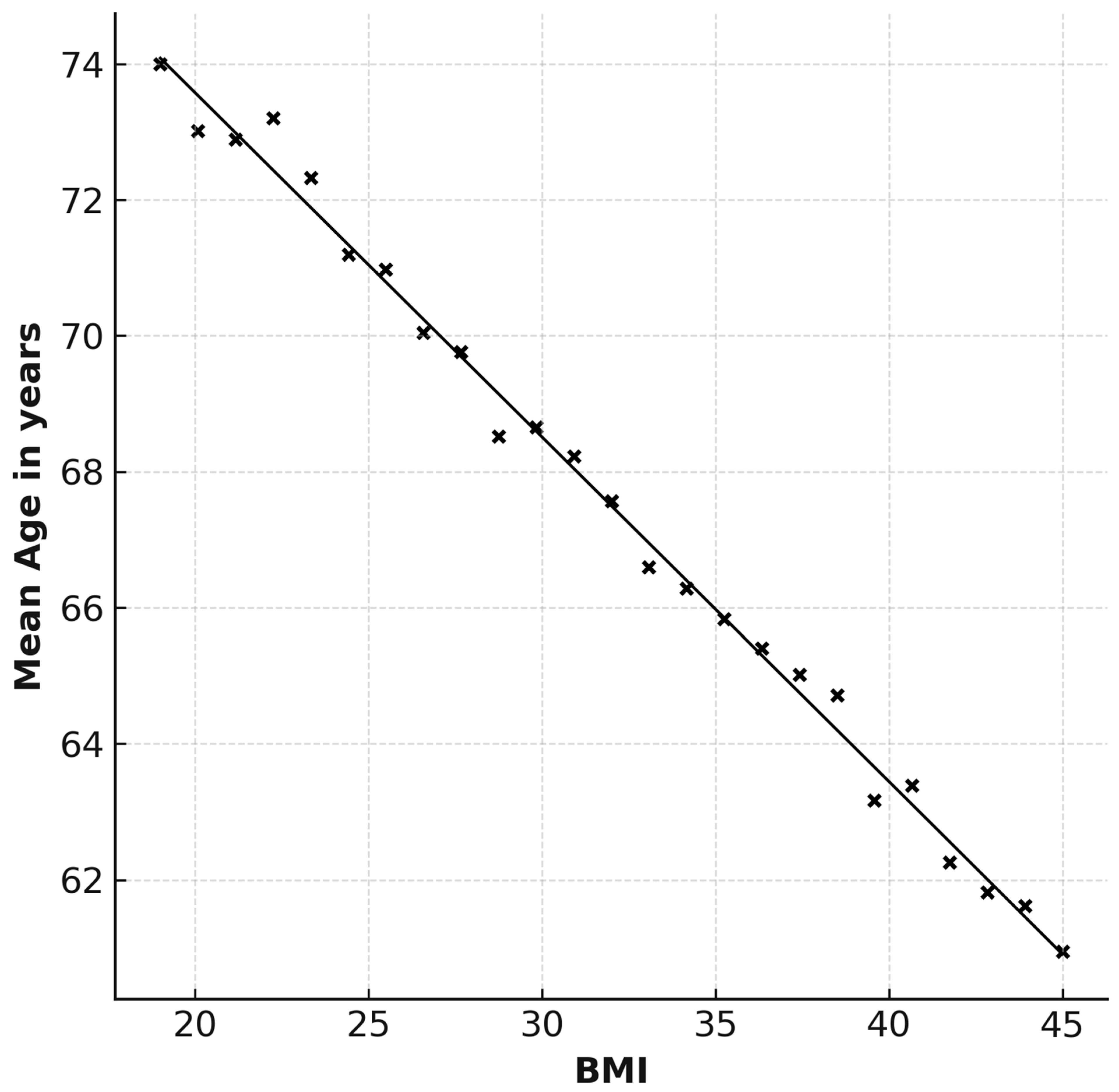
2.3. Correlation Between BMI and Age of THA
2.4. Patient Identification and Comorbidities
2.5. Outcome Measures
2.6. Statistical Analysis
2.7. Ethical Aspects
3. Results
3.1. BMI Classification and Distribution
3.2. Correlation Between BMI and Age of THA
3.3. Baseline Characteristics of Patients by BMI Classification
3.4. Etiologies of Total Hip Arthroplasty by BMI Classification
3.5. Comorbidities by BMI Classification
3.6. Complications and Outcomes by BMI Classification
3.7. Mortality, Length of Stay, and Charges by BMI Classification
3.8. Age-Specific Complications and Outcomes by BMI Classification
4. Discussion
4.1. Main Findings
4.2. Time to THA
4.3. Complications
4.4. Hospitalization Factors
4.5. Limitations and Strengths
5. Conclusions
- Higher BMI is significantly associated with younger age at THA.
- Obesity increases perioperative complications, including anemia, acute kidney injury, and venous thromboembolism.
- Hospital stay length rises with BMI, while total hospital charges remain relatively stable.
- These findings emphasize the importance of BMI-tailored perioperative optimization and long-term risk assessment.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| HCUP | Healthcare Cost and Utilization Project |
| ICD-10 | International Classification of Diseases, 10th Revision |
| LOS | Length of Stay |
| NIS | Nationwide Inpatient Sample |
| SPSS | Statistical Package for the Social Sciences |
| THA | Total Hip Arthroplasty |
References
- Lawrence, R.C.; Felson, D.T.; Helmick, C.G.; Arnold, L.M.; Choi, H.; Deyo, R.A.; Gabriel, S.; Hirsch, R.; Hochberg, M.C.; Hunder, G.G.; et al. Estimates of the Prevalence of Arthritis and Other Rheumatic Conditions in the United States, Part II for the National Arthritis Data Workgroup. Arthritis Rheum. 2008, 58, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.H.; Sledge, C.B. Total Hip and Total Knee Replacement. N. Engl. J. Med. 1990, 323, 725–731. [Google Scholar] [CrossRef]
- Ethgen, O.; Bruyère, O.; Richy, F.; Dardennes, C.; Reginster, J.Y. Health-Related Quality of Life in Total Hip and Total Knee Arthroplasty. J. Bone Jt. Surg. 2004, 86, 963–974. [Google Scholar] [CrossRef]
- Pivec, R.; Johnson, A.J.; Mears, S.C.; Mont, M.A. Hip arthroplasty. Lancet 2012, 380, 1768–1777. [Google Scholar] [CrossRef]
- Bastick, A.N.; Runhaar, J.; Belo, J.N.; Bierma-Zeinstra, S.M.A. Prognostic factors for progression of clinical osteoarthritis of the knee: A systematic review of observational studies. Arthritis Res. Ther. 2015, 17, 152. [Google Scholar] [CrossRef]
- Holliday, K.L.; McWilliams, D.F.; Maciewicz, R.A.; Muir, K.R.; Zhang, W.; Doherty, M. Lifetime body mass index, other anthropometric measures of obesity and risk of knee or hip osteoarthritis in the GOAL case-control study. Osteoarthr. Cartil. 2011, 19, 37–43. [Google Scholar] [CrossRef]
- Sasaki, E.; Ota, S.; Chiba, D.; Kimura, Y.; Sasaki, S.; Yamamoto, Y.; Tsuda, E.; Nakaji, S.; Ishibashi, Y. Early knee osteoarthritis prevalence is highest among middle-aged adult females with obesity based on new set of diagnostic criteria from a large sample cohort study in the Japanese general population. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 984–994. [Google Scholar] [CrossRef]
- Kuroda, Y.; Hashimoto, S.; Saito, M.; Hayashi, S.; Nakano, N.; Matsushita, T.; Niikura, T.; Kuroda, R.; Matsumoto, T. Obesity is associated with less favorable outcomes following hip arthroscopic surgery: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1483–1493. [Google Scholar] [CrossRef] [PubMed]
- Andrew, J.G.; Palan, J.; Kurup, H.V.; Gibson, P.; Murray, D.W.; Beard, D.J. Obesity in total hip replacement. J. Bone Jt. Surg. Br. 2008, 90-B, 424–429. [Google Scholar] [CrossRef]
- Patel, V.P.; Walsh, M.; Sehgal, B.; Preston, C.; DeWal, H.; Di Cesare, P.E. Factors Associated with Prolonged Wound Drainage After Primary Total Hip and Knee Arthroplasty. J. Bone Jt. Surg. 2007, 89, 33–38. [Google Scholar] [CrossRef]
- Namba, R.S.; Paxton, L.; Fithian, D.C.; Stone, M.L. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J. Arthroplast. 2005, 20, 46–50. [Google Scholar] [CrossRef]
- Azodi, O.S.; Bellocco, R.; Eriksson, K.; Adami, J. The impact of tobacco use and body mass index on the length of stay in hospital and the risk of post-operative complications among patients undergoing total hip replacement. J. Bone Jt. Surg. 2006, 88-B, 1316–1320. [Google Scholar] [CrossRef]
- Lübbeke, A.; Stern, R.; Garavaglia, G.; Zurcher, L.; Hoffmeyer, P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Care Res. 2007, 57, 327–334. [Google Scholar] [CrossRef]
- Haverkamp, D.; Klinkenbijl, M.N.; Somford, M.P.; Albers, G.H.R.; Van Der Vis, H.M. Obesity in total hip arthroplasty does it really matter? Acta Orthop. 2011, 82, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Rubin, J.; Potluri, A.S.; Jan, K.; Dandamudi, S.; Levine, B.R. A Systematic Review and Meta-Analysis of Periprosthetic Joint Infection Rates in Morbidly Obese Patients Undergoing Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2025, 9, e24.00306. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Liu, W.; Wahafu, T.; Cheng, M.; Cheng, T.; Zhang, Y.; Zhang, X. The influence of obesity on primary total hip arthroplasty outcomes: A meta-analysis of prospective cohort studies. Orthop. Traumatol. Surg. Res. 2015, 101, 289–296. [Google Scholar] [CrossRef]
- Wu, Y.; Li, D.; Vermund, S.H. Advantages and Limitations of the Body Mass Index (BMI) to Assess Adult Obesity. Int. J. Environ. Res. Public Health 2024, 21, 757. [Google Scholar] [CrossRef]
- Bayliss, L.E.; Culliford, D.; Monk, A.P.; Glyn-Jones, S.; Prieto-Alhambra, D.; Judge, A.; Cooper, C.; Carr, A.J.; Arden, N.K.; Beard, D.J.; et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: A population-based cohort study. Lancet 2017, 389, 1424–1430. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016 Key Findings Data from the National Health and Nutrition Examination Survey. 2015. Available online: https://www.cdc.gov/nchs/data/databriefs/db288_table.pdf#1 (accessed on 15 October 2025).
- Keener, J.D.; Callaghan, J.J.; Goetz, D.D.; Pederson, D.R.; Sullivan, P.M.; Johnston, R.C. Twenty-five-year results after Charnley total hip arthroplasty in patients less than fifty years old. J. Bone Jt. Surg.-Am. Vol. 2003, 85, 1066–1072. [Google Scholar] [CrossRef]
- Prieto-Alhambra, D.; Judge, A.; Javaid, M.K.; Cooper, C.; Diez-Perez, A.; Arden, N.K. Incidence and risk factors for clinically diagnosed knee, hip and hand osteoarthritis: Influences of age, gender and osteoarthritis affecting other joints. Ann. Rheum. Dis. 2014, 73, 1659–1664. [Google Scholar] [CrossRef]
- Pottie, P.; Presle, N.; Terlain, B.; Netter, P.; Mainard, D.; Berenbaum, F. Obesity and osteoarthritis: More complex than predicted! Ann. Rheum. Dis. 2006, 65, 1403–1405. [Google Scholar] [CrossRef]
- Johnson, C.A.; White, C.C.; Kunkle, B.F.; Eichinger, J.K.; Friedman, R.J. Effects of the Obesity Epidemic on Total Hip and Knee Arthroplasty Demographics. J. Arthroplast. 2021, 36, 3097–3100. [Google Scholar] [CrossRef]
- Duwelius, P.J.; Southgate, R.D.; Crutcher, J.P.; Rollier, G.M.; Li, H.-F.; Sypher, K.S.; Tompkins, G.S. Registry Data Show Complication Rates and Cost in Revision Hip Arthroplasty. J. Arthroplast. 2023, 38, S29–S33. [Google Scholar] [CrossRef]
- Lie, S.A.; Havelin, L.I.; Furnes, O.N.; Engesæter, L.B.; Vollset, S.E. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J. Bone Jt. Surg. Br. 2004, 86-B, 504–509. [Google Scholar] [CrossRef]
- Ong, K.L.; Lau, E.; Suggs, J.; Kurtz, S.M.; Manley, M.T. Risk of Subsequent Revision after Primary and Revision Total Joint Arthroplasty. Clin. Orthop. Relat. Res. 2010, 468, 3070–3076. [Google Scholar] [CrossRef]
- Moran, M.; Walmsley, P.; Gray, A.; Brenkel, I.J. Does body mass index affect the early outcome of primary total hip arthroplasty? J. Arthroplast. 2005, 20, 866–869. [Google Scholar] [CrossRef] [PubMed]
- Friedman, R.J.; Hess, S.; Berkowitz, S.D.; Homering, M. Complication rates after hip or knee arthroplasty in morbidly obese patients. Clin. Orthop. Relat. Res. 2013, 471, 3358–3366. [Google Scholar] [CrossRef]
- Wallace, G.; Judge, A.; Prieto-Alhambra, D.; de Vries, F.; Arden, N.K.; Cooper, C. The effect of body mass index on the risk of post-operative complications during the 6 months following total hip replacement or total knee replacement surgery. Osteoarthr. Cartil. 2014, 22, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Telang, S.; Palmer, R.; Chung, B.C.; Ball, J.R.; Hong, K.; Lieberman, J.R.; Heckmann, N.D. Total Hip Arthroplasty Among Superobese Patients: Proceed with Caution. Arthroplast. Today 2025, 34, 101770. [Google Scholar] [CrossRef] [PubMed]
- Chee, Y.H.; Teoh, K.H.; Sabnis, B.M.; Ballantyne, J.A.; Brenkel, I.J. Total hip replacement in morbidly obese patients with osteoarthritis. J. Bone Jt. Surg. Br. 2010, 92-B, 1066–1071. [Google Scholar] [CrossRef] [PubMed]
- McLaughlin, J.R.; Lee, K.R. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J. Bone Jt. Surg. Br. 2006, 88-B, 1286–1292. [Google Scholar] [CrossRef]
- Zeyda, M.; Stulnig, T.M. Obesity, Inflammation, and Insulin Resistance—A Mini-Review. Gerontology 2009, 55, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Di Costanzo, J. Influence de l’état nutritionnel préopératoire sur la morbidité postopératoire. Ann. Françaises Anesth. Reanim. 1995, 14, 33–38. [Google Scholar] [CrossRef]
- Parratte, S.; Pesenti, S.; Argenson, J.N. Obesity in orthopedics and trauma surgery. Orthop. Traumatol. Surg. Res. 2014, 100, S91–S97. [Google Scholar] [CrossRef]
- Søballe, K.; Christensen, F.; Luxhøj, T. Hip replacement in obese patients. Acta Orthop. Scand. 1987, 58, 223–225. [Google Scholar] [CrossRef]
- Matar, H.E.; Pincus, D.; Paterson, J.M.; Aktar, S.; Jenkinson, R.; Ravi, B. Early Surgical Complications of Total Hip Arthroplasty in Patients with Morbid Obesity: Propensity-Matched Cohort Study of 3683 Patients. J. Arthroplast. 2020, 35, 2646–2651. [Google Scholar] [CrossRef]
- Schroer, W.C.; Diesfeld, P.J.; LeMarr, A.R.; Morton, D.J.; Reedy, M.E. Modifiable Risk Factors in Primary Joint Arthroplasty Increase 90-Day Cost of Care. J. Arthroplast. 2018, 33, 2740–2744. [Google Scholar] [CrossRef] [PubMed]
- Shaka, H.; Ojemolon, P.E. Impact of Obesity on Outcomes of Patients with Hip Osteoarthritis Who Underwent Hip Arthroplasty. Cureus 2020, 12, e10876. [Google Scholar] [CrossRef]
- Sambandam, S.; Serbin, P.; Senthil, T.; Varatharaj, S.; Sakthivelnathan, V.; Ramanan, S.P.; Mounasamy, V. Patient Characteristics, Length of Stay, Cost of Care, and Complications in Super-Obese Patients Undergoing Total Hip Arthroplasty: A National Database Study. Clin. Orthop. Surg. 2023, 15, 380. [Google Scholar] [CrossRef] [PubMed]
- Wilkie, W.A.; Remily, E.A.; Mohamed, N.S.; McDermott, S.; Shalit, B.; Baird, A.; Brand, K.; Nace, J.; Delanois, R. Obesity in Total Hip Arthroplasty: Demographic Disparities and Outcome Incongruities. Cureus 2020, 12, e7955. [Google Scholar] [CrossRef]
| Parameter | BMI < 29.9 | 29.9 < BMI < 34.9 Class I Obesity | 34.9 < BMI Class II Obesity + Class III Obesity | Significance |
|---|---|---|---|---|
| Total Surgeries (%) | 76.50% | 11.20% | 12.30% | - |
| Average Age (y) | 66.14 | 64.86 | 62.04 | p < 0.0001 |
| Female (%) | 55.5% | 51.8% | 57.2% | p < 0.0001 |
| Payer—Medicare (%) | 56.5% | 52.2% | 45.4% | p < 0.0001 |
| Payer—Medicaid (%) | 4.8% | 5.0% | 6.5% | |
| Payer—Private (%) | 35.6% | 39.8% | 44.8% | |
| Payer—Other (including self-pay) (%) | 3.1% | 3.0% | 3.3% | |
| Median Household Income 0–25% (%) | 19.0% | 18.6% | 21.6% | p < 0.0001 |
| Median Household Income 26th–50th% (%) | 24.9% | 23.9% | 27.4% | |
| Median Household Income 51st–75th% (%) | 27.2% | 27.8% | 27.9% | |
| Median Household Income 76th–100th% (%) | 28.9% | 29.7% | 23.1% |
| Etiologies | BMI < 29.9 | 29.9 < BMI < 34.9 | 34.9 < BMI | Significance |
|---|---|---|---|---|
| Primary osteoarthritis | 91.42% | 93.09% | 93.63% | p < 0.0001 |
| Revision | 4.10% | 3.51% | 3.65% | |
| Osteonecrosis | 4.11% | 3.08% | 2.41% | |
| Rheumatoid arthritis | 0.16% | 0.13% | 0.10% | |
| Post-traumatic arthritis | 0.11% | 0.09% | 0.09% | |
| Legg-Calvé-Perthes | 0.05% | 0.04% | 0.05% | |
| Leg Deformity | 0.04% | 0.05% | 0.07% |
| BMI < 29.9 | 29.9 < BMI < 34.9 | 34.9 < BMI | Significance | |
|---|---|---|---|---|
| Hypertension Diagnosis | 49.5% | 57.7% | 63.4% | p < 0.0001 |
| Dyslipidemia Diagnosis | 40.3% | 51.1% | 47.3% | p < 0.0001 |
| Sleep Apnea Diagnosis | 6.7% | 15.3% | 26.1% | p < 0.0001 |
| Chronic Anemia | 5.7% | 5.8% | 5.9% | p < 0.0001 |
| Alcohol Abuse | 1.5% | 1.6% | 1.1% | p < 0.0001 |
| Osteoporosis | 5.00% | 3.80% | 2.30% | p < 0.0001 |
| Mental Disorders | 29.2% | 33.0% | 34.5% | p < 0.0001 |
| Type 2 Diabetes | 12.3% | 20.4% | 26.7% | p < 0.0001 |
| Renal Disease | 5.8% | 8.4% | 8.4% | p < 0.0001 |
| CHF | 1.1% | 1.4% | 1.7% | p < 0.0001 |
| Chronic Lung Disease | 6.5% | 6.9% | 7.5% | p < 0.0001 |
| Use of anticoagulants | 5.2% | 6.4% | 7.2% | p < 0.0001 |
| BMI < 29.9 | 29.9 < BMI < 34.9 | 34.9 < BMI | Significance | |
|---|---|---|---|---|
| Blood Loss Anemia | 17.49% | 19.09% | 19.15% | p < 0.0001 |
| Blood Transfusion | 3.00% | 2.46% | 2.53% | p < 0.0001 |
| Acute Kidney Injury | 1.50% | 2.00% | 3.10% | p < 0.0001 |
| Intraoperative Fracture | 0.77% | 0.72% | 0.89% | p < 0.0001 |
| Venous Thromboembolism | 0.16% | 0.20% | 0.24% | p < 0.0001 |
| Hip Dislocation | 0.15% | 0.15% | 0.13% | p = 0.044 |
| Acute Coronary Artery Disease | 0.09% | 0.08% | 0.06% | p = 0.001 |
| Pneumonia | 0.13% | 0.14% | 0.15% | p = 0.031 |
| Pulmonary Embolism | 0.07% | 0.09% | 0.11% | p < 0.0001 |
| Heart Failure | 0.08% | 0.14% | 0.13% | p < 0.0001 |
| Pulmonary Edema | 0.04% | 0.04% | 0.07% | p < 0.0001 |
| Infection | 0.03% | 0.03% | 0.04% | p = 0.013 |
| BMI < 29.9 | 29.9 < BMI < 34.9 | 34.9 < BMI | Significance | |
|---|---|---|---|---|
| Died during hospitalization | 0.04% | 0.03% | 0.03% | 0.087 |
| Length of stay mean in days | 2.00 | 2.01 | 2.21 | p < 0.0001 |
| Total charges mean in $ | 63,490 | 63,920 | 63,819 | p < 0.0001 |
| BMI < 29.9 | 29.9 < BMI < 34.9 | 34.9 < BMI | Significance | |
|---|---|---|---|---|
| Blood Loss Anemia (age under 60) | 15.2% | 17.0% | 17.5% | p < 0.0001 |
| Blood Loss Anemia (age 60–70) | 16.1% | 18.1% | 19.1% | p < 0.0001 |
| Blood Loss Anemia (age over 70) | 20.6% | 22.6% | 22.8% | p < 0.0001 |
| Blood Transfusion (age under 60) | 2.4% | 2.1% | 2.3% | p < 0.0001 |
| Blood Transfusion (age 60–70) | 2.4% | 2.0% | 2.3% | p < 0.0001 |
| Blood Transfusion (age over 70) | 4.0% | 3.4% | 3.4% | p < 0.0001 |
| Acute Kidney Injury (age under 60) | 0.8% | 1.1% | 1.9% | p < 0.0001 |
| Acute Kidney Injury (age 60–70) | 1.1% | 1.7% | 3.3% | p < 0.0001 |
| Acute Kidney Injury (age over 70) | 2.5% | 3.4% | 5.4% | p < 0.0001 |
| Intraoperative Fracture (age under 60) | 0.7% | 0.6% | 0.9% | p < 0.0001 |
| Intraoperative Fracture (age 60–70) | 0.7% | 0.6% | 0.8% | p < 0.0001 |
| Intraoperative Fracture (age over 70) | 0.9% | 0.9% | 1.1% | p = 0.001 |
| Length of stay mean in days (age under 60) | 1.85 | 1.86 | 2.08 | p < 0.0001 |
| Length of stay mean in days (age 60–70) | 1.86 | 1.91 | 2.2 | p < 0.0001 |
| Length of stay mean in days (age over 70) | 2.25 | 2.3 | 2.52 | p < 0.0001 |
| Total charges mean in $ (age under 60) | 63,624 | 64,067 | 63,741 | p < 0.0001 |
| Total charges mean in $ (age 60–70) | 62,658 | 62,591 | 63,423 | p = 0.052 |
| Total charges mean in $ (age over 70) | 64,183 | 65,425 | 64,724 | p < 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berkovich, Y.; Feygelman, S.; Cohen Nissan, E.; Fournier, L.; Steinfeld, Y.; Maman, D. The Burden of Weight on Joint Replacement: A 1.6 Million-Patient Analysis of BMI and Hip Arthroplasty Outcomes. Surgeries 2025, 6, 95. https://doi.org/10.3390/surgeries6040095
Berkovich Y, Feygelman S, Cohen Nissan E, Fournier L, Steinfeld Y, Maman D. The Burden of Weight on Joint Replacement: A 1.6 Million-Patient Analysis of BMI and Hip Arthroplasty Outcomes. Surgeries. 2025; 6(4):95. https://doi.org/10.3390/surgeries6040095
Chicago/Turabian StyleBerkovich, Yaron, Shelly Feygelman, Ela Cohen Nissan, Linor Fournier, Yaniv Steinfeld, and David Maman. 2025. "The Burden of Weight on Joint Replacement: A 1.6 Million-Patient Analysis of BMI and Hip Arthroplasty Outcomes" Surgeries 6, no. 4: 95. https://doi.org/10.3390/surgeries6040095
APA StyleBerkovich, Y., Feygelman, S., Cohen Nissan, E., Fournier, L., Steinfeld, Y., & Maman, D. (2025). The Burden of Weight on Joint Replacement: A 1.6 Million-Patient Analysis of BMI and Hip Arthroplasty Outcomes. Surgeries, 6(4), 95. https://doi.org/10.3390/surgeries6040095






