1. Introduction
Meniscal injuries are common and are associated with an increased risk of knee osteoarthritis. Occupations involving high biomechanical loads may precipitate such injuries, either acutely or progressively [
1]. These lesions are typically classified by aetiology as degenerative or traumatic. Degenerative meniscal tears arise from age-related change or repetitive joint use and are more prevalent in middle-aged and older adults [
2]. Traumatic tears are generally caused by compressive and shear forces within the joint. They occur in isolation or—more commonly—in conjunction with ligamentous and chondral injuries [
3], often during twisting or pivoting movements when the ipsilateral foot is fixed to the ground.
The incidence of meniscal tears is approximately 60 per 100,000 population, a figure that has risen with increased public participation in sport and wider access to diagnostic imaging [
4]. The prevalence of degenerative meniscal injury increases with age [
5]; in middle-aged and elderly populations, MRI-detected tears may be present in up to 35% of knees, even when asymptomatic [
2].
When conservative management fails and symptoms persist with functional impairment, surgery—most commonly meniscectomy—is the treatment of choice. This procedure, used for both degenerative and traumatic tears, is typically performed arthroscopically as a day case [
6]. Arthroscopic partial meniscectomy, which removes unstable meniscal tissue, remains one of the most frequently performed orthopaedic procedures for this indication [
7].
Meniscectomy aims to alleviate pain in patients with persistent symptoms or mechanical phenomena after unsuccessful conservative care [
6]. Postoperatively, substantial pain reduction is generally observed within 6–12 months, particularly when mechanical symptoms are addressed. However, in the presence of degenerative change or pre-existing osteoarthritis, pain often re-emerges over time owing to progressive joint deterioration [
8].
The removal of damaged meniscal tissue is generally performed with the expectation of improving joint mobility and restoring functional capacity, thereby contributing to meaningful gains in patients’ overall quality of life [
9]. In the immediate postoperative period and during the first stages of recovery, many individuals indeed experience a reduction in pain and mechanical symptoms, which facilitates a return to daily activities. Nevertheless, accumulating evidence indicates that these short-term benefits may not be sustained for all patients. A considerable proportion of individuals subsequently report a decrease in participation in sports and recreational activities, together with a gradual shift towards a more sedentary lifestyle [
10]. This decline in activity levels has been attributed to several interrelated factors, including progressive reductions in muscle strength and muscle mass, impaired neuromuscular control, and the loss of the meniscus’s intrinsic shock-absorbing capacity after partial resection. The alteration of this key biomechanical role of the meniscus contributes to increased load transmission to the articular cartilage and subchondral bone, which in turn may promote discomfort, reduce confidence in knee stability, and ultimately limit physical activity [
10].
Meniscectomy is also associated with an increased risk of knee osteoarthritis. Partial or total meniscal removal compromises load distribution, alters knee biomechanics, and increases contact pressures on the articular cartilage, potentially contributing to chondrolysis and reduced joint space [
11]. Contemporary clinical practice prioritises meniscal preservation whenever feasible, reserving partial meniscectomy for selected cases in which mechanical symptoms or tissue quality preclude repair.
Younger patients generally display a superior biological capacity for tissue regeneration and neuromuscular adaptation, which allows them to respond more effectively to structured rehabilitation protocols. This enhanced recovery potential facilitates faster improvements in functional outcomes and a more reliable return to pre-injury levels of activity. In contrast, older individuals tend to exhibit a diminished regenerative response following meniscectomy, a factor that is often compounded by age-related sarcopenia, reduced neuromuscular plasticity, and the presence of degenerative joint changes. These elements collectively increase the likelihood of persistent symptoms, slower recovery trajectories, and a higher risk of developing or accelerating osteoarthritic alterations in the knee joint after surgery [
12]. With regard to sex-related differences, several studies have consistently demonstrated that men, on average, present with higher baseline levels of muscle strength and greater muscle mass prior to undergoing meniscectomy [
13]. These attributes may contribute to an enhanced mechanical environment for the knee and allow for more rapid functional recovery, which can translate into an earlier resumption of occupational duties, social participation, and engagement in recreational or competitive sporting activities compared with their female counterparts [
13].
Postoperative rehabilitation can accelerate functional recovery, alleviate pain, and prevent complications [
14]. Early, individualised programmes centred on progressive therapeutic exercise yield meaningful improvements in range of motion, pain control, and joint stability [
15]. Neuromuscular control exercises, proprioceptive and balance training, and task-specific functional activities have proven effective in restoring physical performance and facilitating return to work or sport [
14]. Moreover, rehabilitation may address psychosocial factors such as kinesiophobia, improving confidence in the operated knee and contributing to more complete and sustained recovery [
16].
The aim of this study was to evaluate the clinical and functional status of patients undergoing meniscal surgery and to identify the optimal predictive model for postoperative functional performance according to receipt of postoperative rehabilitation.
2. Materials and Methods
2.1. Study Design
This study was an ambispective, multicentre cohort study and was reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [
17].
2.2. Ethical Considerations
Confidentiality and anonymity of all collected data were ensured in accordance with the ethical principles of the Declaration of Helsinki. All participants were fully informed about the study and provided written informed consent prior to enrolment. The study protocol was approved by the Ethics Committee of the Catholic University of San Antonio of Murcia (code: CE112415; date: 29 November 2024). The study was registered at ClinicalTrials.gov (NCT06920394; date: 1 April 2025).
2.3. Participants
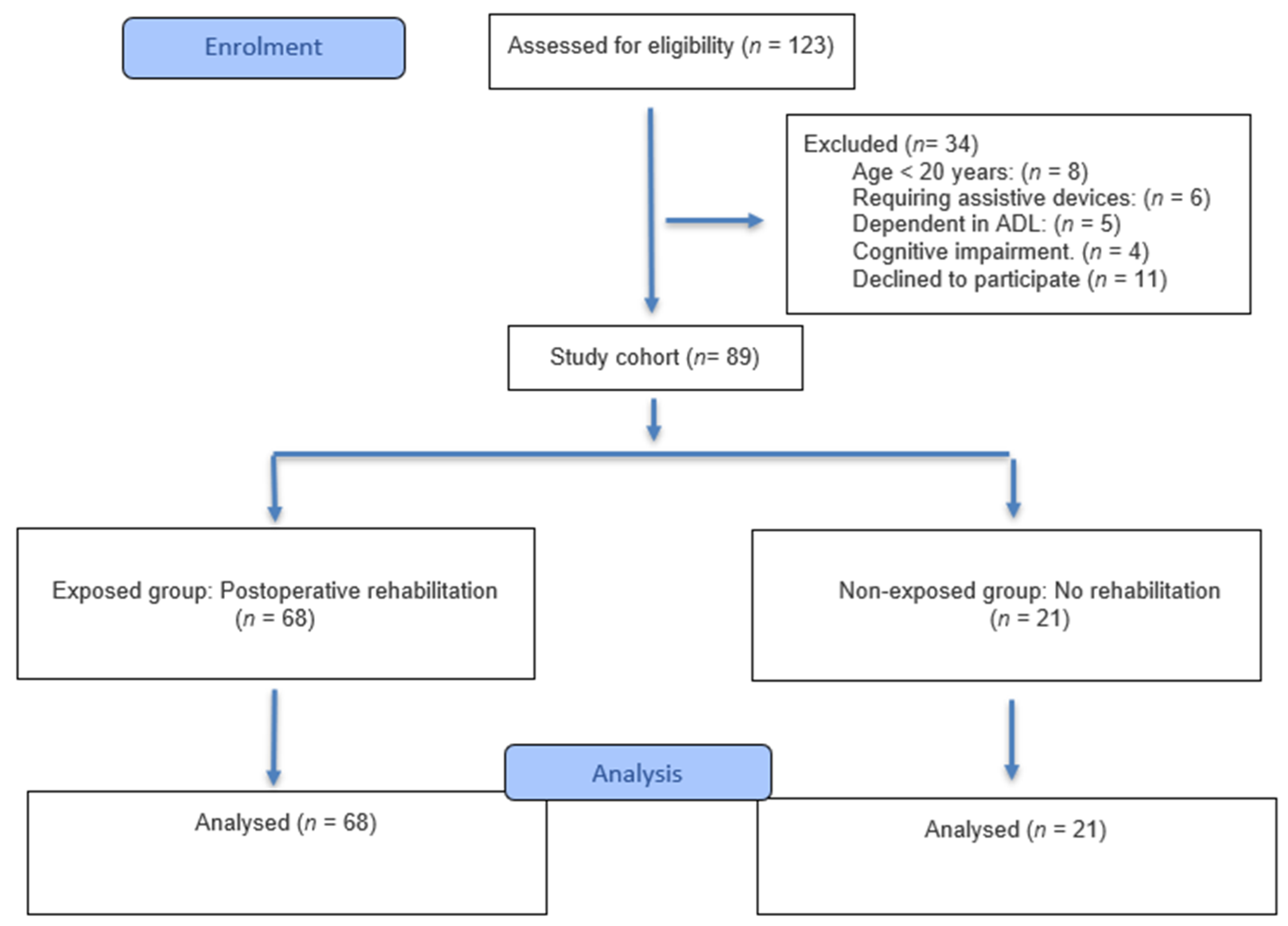
The inclusion criteria were (i) individuals aged between 20 and 65 years; (ii) of either sex; (iii) with a history of unilateral knee meniscectomy performed within the past five years; and (iv) who signed the informed consent form. All patients included in the study presented with traumatic meniscal tears, confirmed by clinical examination and magnetic resonance imaging at the hospital centre where the surgical intervention was performed.
The exclusion criteria included (i) individuals requiring assistive devices for ambulation; (ii) individuals dependent in activities of daily living (ADLs); and (iii) individuals with cognitive impairments that could affect understanding of the assessments and procedures.
Data collection was conducted between April and May 2025 at two clinical centres, Fisiomaturana and Fisialty, both located in the city of Murcia, Spain. All surgical procedures were performed at two reference hospital centres by surgeons with extensive clinical and surgical experience in meniscectomy. Although protocol variations between centres cannot be ruled out, all included patients presented with traumatic meniscal tears, which contributes to the homogeneity of the study cohort. Patients in the rehabilitation group received a standardised programme comprising five sessions per week, each lasting 45 min. Each session incorporated manual therapy techniques (including joint mobilisations and soft-tissue treatment) together with individualised therapeutic exercises designed to improve mobility, strength, and motor control.
2.4. Outcome Measures
The primary outcome was functional performance, treated as a continuous variable. The primary exposure was receipt of postoperative rehabilitation following meniscectomy, analysed as a dichotomous categorical variable (yes/no) and used as the grouping variable for between-group comparisons. The measurement instruments were as follows:
Functional performance: assessed with the Timed Up and Go (TUG) test [
18], which involves standing from a chair, walking three metres around a marker, and returning to the seated position. The outcome is time (seconds); shorter times indicate better functional performance.
Knee range of motion (ROM): measured by goniometry following the protocol of Hancock et al. [
19]. The stationary arm was aligned between the centre of the greater trochanter and the lateral femoral epicondyle; the moving arm was aligned with the tibial axis, between the lateral femoral epicondyle and the centre of the lateral malleolus. Participants performed maximal active knee flexion and extension. The unit of measurement was degrees; higher values indicate greater ROM.
Joint pain intensity: measured using a visual analogue scale (VAS) from 0 (no pain) to 10 (worst pain imaginable) [
20].
Kinesiophobia: assessed with the 11-item Tampa Scale for Kinesiophobia (TSK-11), with each item scored 1 (“strongly disagree”) to 4 (“strongly agree”); total scores range from 11 to 44, with higher scores indicating greater fear of movement [
21].
In addition, anthropometric measures and sociodemographic characteristics were collected as covariates: age (years, continuous); sex (male/female, dichotomous); weight (kg) and height (cm) to derive body mass index (BMI, kg/m2); occupational type (active/sedentary, dichotomous); and engagement in physical exercise before and after surgery (yes/no, dichotomous). Time since surgery was defined as the interval (days) between the index meniscectomy and the study assessment. A single assessment time point was used, and all data were analysed in anonymised form.
2.5. Sample Size
The required sample size was computed using G*Power (version 3.1.9.2; Heinrich Heine University, Düsseldorf, Germany). Assuming a moderate effect size (f2 = 0.15) to assess functional performance in adults undergoing knee meniscectomy, an α of 0.05, a power of 90% (1−β = 0.90), and 14 predictors, the minimum sample size was 89 participants with a prior history of knee meniscectomy.
2.6. Statistical Analysis
Quantitative variables were summarised as mean (standard deviation), and categorical variables as absolute frequencies and percentages. Normality of quantitative variables was assessed using the Kolmogorov–Smirnov test. Between-group comparisons (postoperative rehabilitation vs. no rehabilitation) employed the independent-samples t-test when normality was satisfied, or the non-parametric Mann–Whitney U test otherwise; categorical variables were compared using the chi-squared test.
A multiple linear regression model was fitted to identify independent predictors of functional performance. Time since surgery was entered as a continuous covariate (days) in the regression model. Multicollinearity was assessed using the variance inflation factor (VIF). Model fit was evaluated with the adjusted coefficient of determination (R2adj) and the overall F-test.
All analyses were performed using IBM SPSS Statistics, version 26.0 (IBM Corp., Armonk, NY, USA). A two-sided p-value < 0.05 was considered statistically significant.
4. Discussion
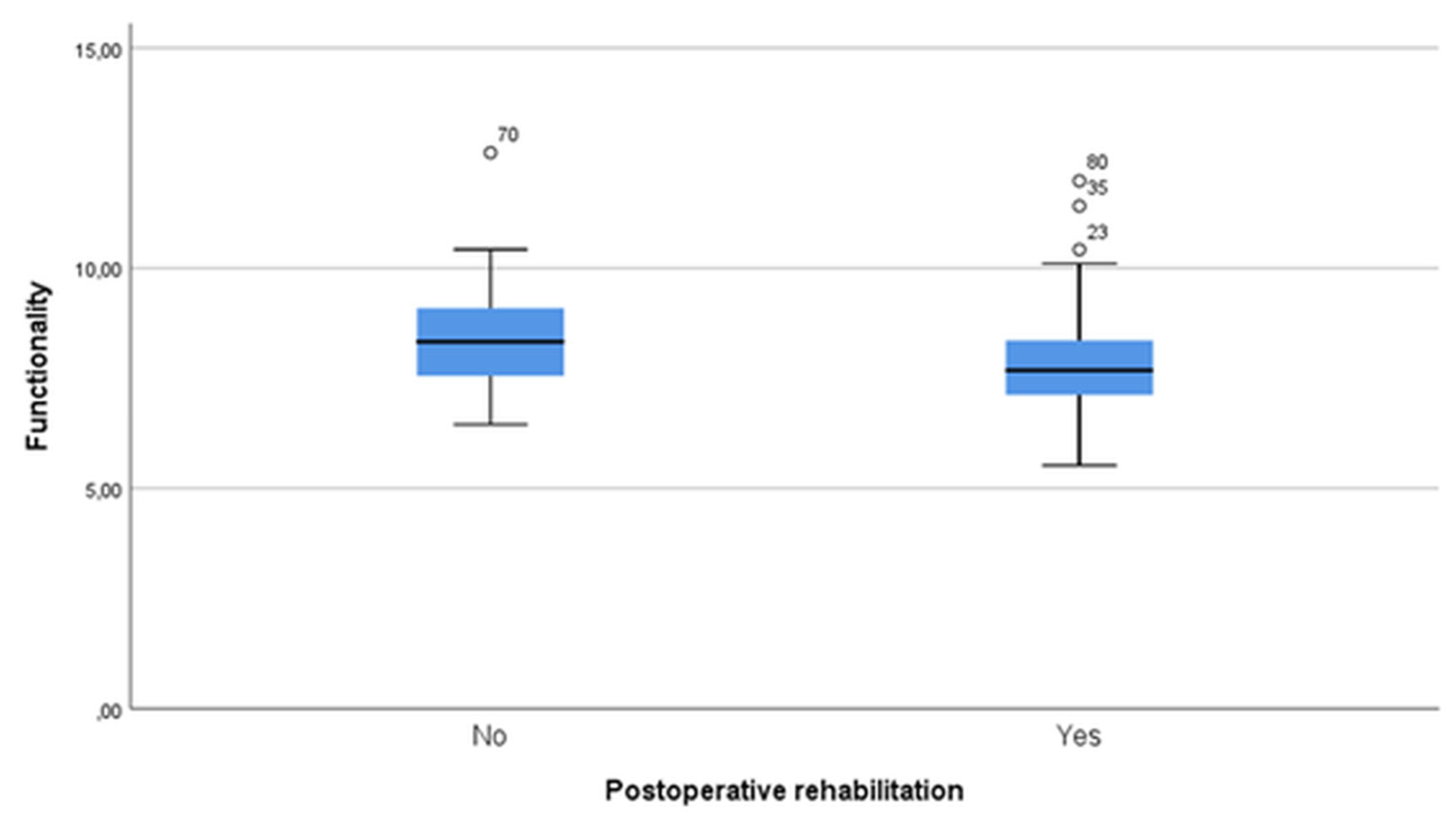
The aim of this study was to compare clinical and functional status in patients undergoing meniscectomy according to receipt of postoperative rehabilitation. We also examined sociodemographic and clinical determinants to develop a predictive model of functional performance. The principal finding was that objective functional performance was superior in the rehabilitation group. This occurred despite the already favourable clinical profile of reduced pain, greater range of motion, and lower kinesiophobia observed with rehabilitation, and contrasts with our a priori expectation of a null difference. The between-group effect size for the primary endpoint was small to moderate (r ≈ 0.23), indicating a measurable advantage.
Dias et al. [
22] reported that postoperative rehabilitation combined with home-based exercises appears to improve patient-reported knee function and range of motion after arthroscopic meniscectomy. However, the randomised controlled trials included in their meta-analysis were judged to be at moderate-to-high risk of bias, which necessitates cautious interpretation of these results. Similarly, Nutarelli et al. [
23] observed no clear superiority of supervised programmes over home-based rehabilitation in terms of physical, functional, occupational, or patient-reported outcomes. Nonetheless, they concluded that home-based postoperative rehabilitation may constitute an effective therapeutic approach after isolated arthroscopic meniscectomy. More recently, the international consensus published by Pujol et al. [
24] emphasised that, although the overall quality of the available evidence remains low, there is strong expert agreement supporting the use of criterion-based, milestone-driven rehabilitation protocols rather than rigid, time-based schemes, with adjustments made according to the type of lesion and the surgical procedure undertaken.
Several factors should be considered when comparing our results with previous evidence. First, differences in outcome measures: we used the Timed Up and Go test as the primary endpoint—an objective, performance-based test—whereas many prior studies relied on patient-reported questionnaires, which are more sensitive to subjective perceptions of improvement than to actual motor performance. Second, sample characteristics: our cohort comprised exclusively traumatic meniscal tears, unlike many reports that included degenerative or mixed populations, in which the role and magnitude of rehabilitation effects may differ. Third, unmeasured confounders—including preoperative function, lesion severity, and psychosocial or hormonal influences—may have shaped recovery trajectories. Finally, real-world variability in rehabilitation practice (content, intensity, and timing) contrasts with the structured, standardised interventions typically delivered in clinical trials and may also account for differences in effect estimates.
Taken together, our findings support a beneficial role of postoperative rehabilitation in a homogeneous cohort with traumatic meniscal tears—typically younger and clinically active—by demonstrating measurable advantages in an objective performance-based outcome (TUG) alongside improvements in pain, mobility, and kinesiophobia. While the magnitude of the functional effect appears small-to-moderate, these results, together with prior evidence, favour criterion-based, milestone-driven protocols tailored to lesion type and surgical procedure.
Women in our cohort demonstrated superior functional performance following meniscectomy. The role of sex as a determinant of recovery after this surgical procedure has been debated for several decades, and previous investigations addressing sex-related differences have yielded inconsistent and sometimes contradictory findings. Certain studies have reported that men are more likely to achieve superior functional outcomes after meniscectomy, a result often attributed to their generally higher baseline muscle strength and greater muscle mass, which may provide a mechanical advantage for postoperative recovery [
13]. In contrast, other studies have found no statistically significant differences between men and women once potential confounding variables—such as lesion severity, tear location, or concomitant degenerative changes—are accounted for, thereby suggesting that sex per se may not constitute an independent determinant of postoperative function [
25]. Beyond these physiological considerations, behavioural and psychosocial factors may also influence recovery. In particular, women have been consistently observed to demonstrate greater adherence to prescribed rehabilitation exercises, reflecting a higher level of consistency, discipline, and long-term commitment to therapeutic protocols [
26]. This greater adherence is likely to promote more sustained improvements in neuromuscular control and muscular endurance, which in turn may contribute to enhanced functional performance over time. Taken together, these findings highlight that sex-related differences in outcomes after meniscectomy may be the result of a multifactorial interaction between biological predispositions and behavioural determinants, rather than a simple dichotomy based solely on sex.
Younger patients achieved superior functional results. Multiple studies indicate that age is a key determinant of outcome after meniscectomy, with a clear trend towards superior recovery in younger individuals. This advantage is attributed primarily to a lower prevalence of advanced cartilage lesions and more favourable joint alignment in younger patients [
27], alongside generally better baseline physical condition, greater muscle strength, and superior proprioception [
28]. In addition, acute traumatic injuries—typically associated with a better prognosis—predominate in younger cohorts, whereas degenerative tears are more common in older adults. Consequently, clinically meaningful improvements are more frequently observed in patients under 50 years of age [
29]. Interestingly, time since surgery did not emerge as a significant predictor of functional performance in our adjusted model. This result contrasts with previous studies that have reported progressive deterioration in knee function and performance within 2–5 years after meniscectomy [
30,
31]. Several explanations may account for this apparent discrepancy. First, our cohort comprised exclusively traumatic meniscal tears, which generally involve younger patients with less degenerative burden compared with the mixed or degenerative populations studied previously. Second, time since surgery was treated as a continuous covariate, which may have limited sensitivity to detect non-linear effects across different follow-up intervals. Finally, the relatively small non-rehabilitation subgroup (
n = 21) may have reduced statistical power. For these reasons, our findings should be interpreted with caution and confirmed in larger, prospective longitudinal cohorts.
Overall, these findings suggest that the process of functional recovery following meniscectomy cannot be attributed exclusively to the implementation of postoperative rehabilitation programmes. Although structured rehabilitation is undoubtedly a cornerstone of recovery, the outcomes achieved by patients are also shaped by a complex interplay of additional determinants. Among these, biological sex and chronological age emerge as particularly relevant, given their established influence on muscle strength, regenerative capacity, and susceptibility to degenerative joint changes. Likewise, the degree of adherence to prescribed rehabilitation exercises, together with the level of habitual physical activity prior to surgery, substantially conditions the trajectory of recovery. Patients who maintain higher levels of preoperative activity, for instance, may possess superior baseline strength and neuromuscular control, thereby facilitating faster gains postoperatively, while those with lower levels of adherence to physiotherapy are at risk of suboptimal recovery. Understanding how these diverse factors interact, rather than considering them in isolation, is essential to design rehabilitation strategies that are not only more effective but also tailored to the specific characteristics, needs, and expectations of each patient. Such an individualised approach could maximise functional outcomes and ultimately improve quality of life after meniscectomy.
Study Limitations
This ambispective, observational design precludes causal inference and is susceptible to residual confounding, including confounding by indication. Several potentially influential variables were not available for adjustment, notably baseline functional performance, meniscal tear severity/morphology, and details of postoperative rehabilitation protocols (exercise type, dose/intensity, and timing). Hormonal and psychosocial factors (e.g., pain tolerance, fear-avoidance, and self-efficacy) were also not assessed systematically. To mitigate these constraints as much as possible, strict inclusion criteria were applied (traumatic meniscal tears only) to reduce clinical heterogeneity; all procedures were conducted in reference centres by experienced knee arthroscopists to minimise surgical variability; the primary functional endpoint (Timed Up and Go) was analysed using a non-parametric approach (Mann–Whitney); and a multivariable model was fitted adjusting for relevant sociodemographic and clinical covariates (rehabilitation, sex, age, time since surgery, and pre- and postoperative exercise), with low collinearity. Nevertheless, residual confounding cannot be excluded.
Although the total cohort was adequate for the primary analyses, the comparatively small non-rehabilitation subgroup limits the precision of estimates and increases the risk of type II error for clinically meaningful contrasts; hence, generalisability should be interpreted with caution. Post hoc matching or truncation of follow-up to ≤2 years was considered; however, given the ambispective design and the comparatively small non-rehabilitation subgroup, such a restriction would have substantially reduced statistical power and potentially introduced selection bias. We therefore modelled time since surgery as a continuous covariate, while acknowledging that time-related residual confounding cannot be fully excluded.
Assessments were performed at a single medium-to-long-term time point, and time since surgery differed between groups—being longer in the non-rehabilitation group than in the rehabilitation group. Although this variable was included as a covariate in the multivariable model, time-related residual confounding remains possible, and longitudinal trajectories could not be examined.
Two reference hospital centres contributed patients. While all procedures were undertaken by experienced arthroscopists, we could not verify that identical operative protocols were used across centres, and unmeasured centre effects cannot be ruled out.
Finally, some outcomes (e.g., pain intensity) were self-reported and thus subject to perception bias, which may affect objectivity, whereas the primary functional performance (Timed Up and Go) was performance-based. The restriction of the cohort to traumatic meniscal tears enhances internal comparability but may limit external validity to degenerative populations.
5. Conclusions
Objective functional performance was higher in patients who received postoperative rehabilitation after meniscectomy than in those who did not. Furthermore, rehabilitation was associated with favourable clinical effects, including reduced pain intensity, improved range of motion, and lower kinesiophobia.
Sex and age were the strongest positive predictors of functional recovery: females outperformed males, and younger patients achieved superior outcomes, likely reflecting more favourable baseline joint status and a lower degenerative burden.
Preoperative physical inactivity was associated with better postoperative functional performance, whereas postoperative exercise showed no clear association with functional performances in this cohort.
Overall, recovery after meniscectomy appears to be shaped by a combination of demographic, clinical, and lifestyle factors rather than by postoperative rehabilitation alone. While rehabilitation may not consistently enhance objective functional performance, it confers meaningful clinical benefits that support its role in comprehensive care.
These findings should be interpreted cautiously in light of potential residual confounding and the small non-rehabilitation subgroup, and require validation in larger, ideally randomised, cohorts.