Abstract
The expected rate and timing of return to work (RTW) following hip arthroscopy is an important consideration for patients. The purpose of this study was to evaluate the rates of RTW following hip arthroscopy, the time required to RTW, and factors correlated with successful RTW. A retrospective review was performed of patients who underwent hip arthroscopy for the treatment of femoroacetabular impingement syndrome (FAIS) from 2018–2021. Data were collected regarding pre-injury employment, work activity level, workers’ compensation (WC) status, ability to return to work, the pre- and postoperative pain visual analog score (VAS), and the Nonarthritic Hip Score (NAHS). Overall, 76 patients (90.5%) returned to their pre-surgical occupation at an average of 9.3 weeks (range: 0.14–56 weeks) postoperatively. Of those who returned, 62 patients (81.6%) returned to full work duties. The NAHSs improved significantly from the preoperative period to follow-up at 1 year (64.7 vs. 83.7, p < 0.001). A linear regression found elevated BMI to be associated with an increased time to return (β = 0.757, p = 0.012). On average, patients with WC status returned to work 9 weeks later than non-WC patients, though this difference did not reach statistical significance (18.4 vs. 9.9 weeks, p = 0.130). There is a high rate of return to full work duties at an average of 9.3 weeks following hip arthroscopy for FAIS.
1. Introduction
Hip arthroscopy has gained popularity as the primary surgical treatment option for femoroacetabular impingement syndrome (FAIS) and/or labral tears given its minimally invasive nature and low complication rate [1,2]. FAIS is a hip condition associated with abnormal contact of the femoral head and neck with the acetabulum due to bony irregularities in the hip joint, which may result in chondral or labral injuries [3]. FAIS can be classified as cam-type, involving abnormalities at the femoral head–neck junction; pincer-type, involving irregularities around the acetabular rim; or a combination of either. Hip arthroscopy is often indicated due to significant hip pain, chondral injury, labral tearing, or the early development of hip osteoarthritis. With careful patient selection, hip arthroscopy has demonstrated favorable outcomes when considering demographics, radiographic measures, and intraoperative prognostic factors. Patients who undergo hip arthroscopy are typically otherwise working-age, healthy adults who contribute significantly to the workforce and economic productivity [4]. As postoperative recovery requires time away from work and potential restrictions upon return, patients undergoing hip arthroscopy should be aware of any work-related or economic implications.
Hip arthroscopy has demonstrated excellent outcomes with substantial improvement in overall function [5,6]. Similarly, return to sport following hip arthroscopy has been documented at greater than 80% for athletes being treated for FAIS, with a majority of patients able to return to pre-surgical performance levels [7,8,9]. While the outcomes are certainly promising for athletic populations, attention should also be given to meaningful benchmarks such as rate of return to work (RTW), timing of return to work, and post-surgical occupational performance. While return to sport following hip arthroscopy has been frequently reported in the literature, RTW data remain relatively sparse. Furthermore, most studies reporting on RTW focus on smaller cohorts, often conducted with military populations [10,11,12,13].
The orthopedic community has witnessed ongoing advancements and increasing acceptance of minimally invasive techniques, including hip arthroscopy. As a result, it is imperative to comprehend the potential socioeconomic implications for patients undergoing this procedure, namely the likelihood and timing of successful return to work. The purpose of this study was to evaluate the rates of RTW following hip arthroscopy, the time required to RTW, and patient characteristics associated with successful RTW. The hypothesis was that workers undergoing hip arthroscopy would have high rates of return to work and that factors such as labor physical intensity and WC status would affect patients’ ability to make a full return to work.
2. Materials and Methods
2.1. Ethical Approval and Cohort Selection
We conducted a retrospective case series of patients undergoing hip arthroscopy for FAIS and/or a labral tear from January 2018 to December 2021. All procedures were performed by a single fellowship-trained sports medicine orthopedic surgeon (T.Y.). All patients included in this study provided informed consent as outlined in the approved Institutional Review Board protocol (New York University School of Medicine; protocol i20-01686).
The following comprised our inclusion criteria: age between 18 to 75 years old, minimum follow-up time of 1 year, and pre-injury employment. The exclusion criteria were revision hip arthroscopy or previous open hip surgery, staged bilateral hip arthroscopy, or history of rheumatologic joint disease.
2.2. Diagnostic Criteria and Surgical Indications
Subjects were diagnosed with FAIS based on a clinical history of pain localized to the hip and physical exam and radiographic findings. Provocative testing with the anterior impingement and Patrick tests were performed in clinics. FAI morphology was identified on plain hip radiographs with standing anteroposterior (AP) and 45-degree Dunn and 90-degree Dunn views. Magnetic resonance imaging (MRI) and/or magnetic resonance arthrography (MRA) were used to identify concomitant soft tissue pathology of the cartilage, labrum, and chondrolabral junction. Radiographic evidence of FAI morphology included alpha angle ≥55° (cam morphology) and/or crossover sign (pincer morphology due to acetabular retroversion).
All patients involved had been experiencing symptoms for at least 6 months and had failed non-operative management for FAIS. Non-operative management included a trial of non-steroidal anti-inflammatory medications, activity modification, and physical therapy for at least six weeks. In addition, patients with atypical hip pain underwent a diagnostic injection to the symptomatic hip joint to further confirm the diagnosis of FAIS when the patient had atypical hip pain. Patients were offered surgery if these non-operative measures failed to provide lasting relief.
Demographic data (age, gender, and body mass index (BMI)), insurance type, presence of connective tissue disease, and surgical characteristics (laterality and procedures performed) were abstracted from the electronic medical records. All intraoperative and postoperative complications were recorded.
2.3. Surgical Technique
All patients received general anesthesia or regional anesthesia and were placed into a supine position on a hip distraction system. Anterolateral and mid-anterior portals were created and an interportal capsulotomy was performed to access the intra-articular space. All labral tears at the chondrolabral junction were repaired using tape and suture anchors. Superficial or irreparable labral tears were debrided. The chondrolabral junction was inspected, as was the remaining articular cartilage, and chondroplasty was performed where necessary. Any damaged chondral or synovial surfaces were debrided. Shaving chondroplasty was used to stabilize chondral borders for Outerbridge grade I–III lesions. None of the patients in this cohort underwent microfracture. Acetabular rim trimming and femoral cam resection were performed under fluoroscopic guidance, and the senior author (T.Y.) utilized dynamic examination to ensure sufficient resection [14]. A water-tight capsular repair was conducted at the conclusion of surgery and a pericapsular local anesthetic was infiltrated following skin closure.
2.4. Postoperative Protocol
Following surgery patients were braced, restricting hip hyperextension and excessive external rotation for 2 weeks while restricting activity to flatfoot weightbearing with crutch assistance. After 4 weeks, patients were allowed gradual return to weightbearing as tolerated. All patients were discharged with three days of cephalexin (500 mg, four times daily) for infection prophylaxis, Celebrex (200 mg per day) for 14 days for heterotopic ossification prevention, and aspirin (81 mg per day) for seven days for deep venous thrombosis (DVT) prophylaxis.
2.5. Clinical Outcome Evaluation
Patients completed a survey that pertained to the following information: pre-injury employment, level of activity at work, time to return to work, complete or partial return to work, crutch use upon return, any re-operation following the index hip arthroscopy within one year, and the visual analog scores (VAS) for pain and the validated Nonarthritic Hip Score (NAHS) collected both preoperatively and at latest follow-up [15]. Preoperative work activity level classifications were defined based on the strength level criteria established by the U.S. Department of Labor, which are dependent on the amount of weight lifted during the workday as well as the frequency of these activities (Table 1) [16]:

Table 1.
U.S. Department of Labor classification of work level intensity [16].
2.6. Statistical Analysis
Descriptive statistics were reported for all variables. The Shapiro–Wilk test was used to assess continuous variables for normality with Student’s t-test used to compare the means of normally distributed variables and Mann–Whitney U test for non-normally distributed variables. Categorical variables were compared between groups using Pearson’s Chi squared test or Fisher’s exact test when appropriate. Welch’s t-test assuming unequal variance was used to compare patients with WC insurance to those without. Multivariable linear regression was performed to assess the variables of age, gender, BMI, and work intensity with time to RTW as the dependent outcome. Regression coefficients (β) were reported with 95% confidence intervals. Analyses were performed on GraphPad Prism 8.3 (GraphPad, La Jolla, CA, USA). A p-value of less than 0.05 was considered statistically significant.
3. Results
3.1. Patient Demographics
There were 137 patients who underwent hip arthroscopy in the study period. Of these, 10 patients were excluded because they underwent staged bilateral procedures and 5 patients were excluded because had presented for revision of a prior hip arthroscopic procedure. There were 24 patients further excluded because they were not employed prior to undergoing hip arthroscopy, leaving 85 patients in for final analysis. The mean age of the cohort was 37.1 ± 10.7 years, the mean BMI was 25.2 ± 4.3, and the majority of patients were female (71.8%). A majority of the cohort had preoperative work that required sedentary or light physical activity levels (68.2%; Figure 1). The mean postoperative follow-up was 16.2 months (range: 12.0–32.2). Demographic details are detailed in Table 2.
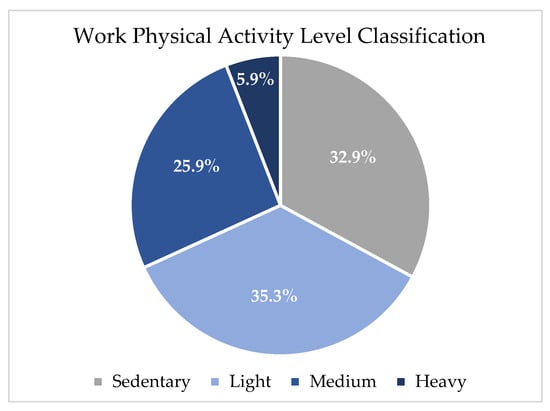
Figure 1.
Work physical activity level classification.

Table 2.
Patient demographics and return to work.
3.2. Surgical Characteristics
All patients included in this analysis underwent hip arthroscopy for the treatment of clinically symptomatic FAIS with a concomitant labral tear which was confirmed by radiologic imaging prior to surgery. Nearly all patients had mixed FAIS and underwent femoral osteochondroplasty (100%) and acetabuloplasty (95.3%). There were no intra- or postoperative complications recorded. Two patients underwent revision hip arthroscopy and labral reconstruction at 10 and 12 months postoperatively. A detailed summary of the surgical procedures performed can be found in Table 3.

Table 3.
Intraoperative characteristics.
3.3. Patient-Reported Outcomes
On average, the VAS of pain improved by 5.2 ± 3.0 points at the most recent follow up (7.8 ± 4.5 vs. 2.6 ± 5.9, p < 0.001). There was no significant difference found in the postoperative VASs at rest versus during work-related activities (2.6 ± 2.5 vs. 2.8 ± 2.7, p = 0.610). The average NAHS increased significantly from the preoperative period to a minimum 1-year follow-up (64.7 ± 19.8 vs. 83.7 ± 15.2, p < 0.001).
3.4. Return to Work and Time to Return
Of the 85 patients included in analysis, 76 patients (90.5%) were able to return to work at an average of 9.3 weeks (range: 0.14–56 weeks) following surgery. Of the patients that were able to return to their preoperative occupation, 76 (89.4%) patients successfully returned to work in any capacity. Among those who returned, 62 (72.9%) patients were able to resume full work duties, while 14 (16.5%) patients reported modified work duties. With respect to the 14 patients who required modification to their duties upon returning to work, reasons that were cited included pain in the operative limb (n = 8, 57.2%), physical inability to perform work duties (n = 3, 21.4%), and physician restrictions (n = 3, 21.4%). Upon return to work, 28 patients (36.8%) required the use of two crutches, 12 patients (15.8%) required the use of one crutch, and 36 patients (47.5%) were able to return to work fully weight-bearing. With respect to the patients who were unable to return to work, seven patients (77.8%) cited pain in the operative limb as the reason they were unable to return to work. One patient reported that their inability to return was not due to their operative limb but did not specify a reason.
The multivariable linear regression found that increased BMI was a significant predictor of an increased time prior to return (p = 0.012) after controlling for age, gender, BMI, and intensity of work duties. These findings are further detailed in Table 4.

Table 4.
Linear regression model for time return to work.
3.5. Gender
Overall, there were 61 female patients and 24 male patients included in the analysis. There were no statistically significant differences found in the rate of return between females and males (88.5% vs. 91.7%, p = 0.672), nor was there a significant difference in the time to return to work between the two groups.
3.6. Workers’ Compensation
Thirteen patients (15.3%) qualified for workers’ compensation status. While age, sex distribution, and work activity level distribution were not significantly different between non-WC and WC groups (Table 5), WC patients had significantly higher BMIs (28.9 vs. 24.6, p = 0.017). There was no significant difference in the rate of return between patients with WC status versus without (83.3% vs. 91.7%, p = 0.490). Additionally, there was no significant difference in the average time to return to work between groups (WC: 18.4 weeks; non-WC: 9.9 weeks, p = 0.130). While there were no significant differences between groups with respect to the pre- or postoperative VAS of pain at rest, there was a significant difference in the postoperative VAS of pain during work-related activities between WC versus non-WC patients (4.2 vs. 2.6, p = 0.045).

Table 5.
Subgroup analysis based on workers’ compensation status.
4. Discussion
The main finding of this study is a high rate of return to full work duties following hip arthroscopy for FAIS and labral tears. On average, patients with workers’ compensation insurance status required nearly double the time to return to work compared to non-WC patients, though this difference was not found to be statistically significant. Increasing BMI was associated with increased time to return to work.
Though return to sport following hip arthroscopy has been well studied within the existing literature, the exploration of return to work is relatively sparse [2,8,17]. Rates of return to sport tend to be high, with studies reporting rates ranging from 59–100% [8,9], with two recent meta-analyses reporting rates of 84.6% and 87.7% [2,8]. The high rate of return to work found in this study aligns well with existing literature regarding rates of return to play. Though relatively scarce, studies on RTW following hip arthroscopy may be found within the existing literature. Previous studies investigating RTW have reported rates ranging from 55% to 78% [12,18,19,20], with most rates notably lower than what was found in the current study. One potential explanation for this discrepancy is the focus of previous studies on specific patient populations, such as workers’ compensation patients or military personnel. It is plausible that these groups are not representative of the general hip arthroscopy population. Therefore, inherent differences in patient characteristics or the course of postoperative care may have contributed to the differences observed between our results and prior studies.
Previous studies have repeatedly shown that WC patients attain poorer outcomes after a range of arthroscopic procedures [21,22,23,24]. Following surgery, WC patients have demonstrated decreased recovery of range of motion, greater postoperative pain, and a higher risk of complications compared to controls [22,23]. In a meta-analysis involving multiple orthopedic specialties, de Moraes et al. [24] found that, regardless of the procedure type, anatomical surgical site, or underlying diagnosis, WC patients were less satisfied with their postoperative results compared to patients without WC insurance. Given the substantial evidence, it seems likely that WC patients might also have a lower rate of RTW compared to non-WC patients, though the data are inconsistent and consist of lower-level evidence. In a recent meta-analysis, Blaeser et al. [10] found that WC patients returned to any work at a rate of 85%, which was higher than the overall RTW rate of 71% of all included patients. On the other hand, Sabetien et al. [13] found that 66% of WC patients were able to return to work following hip arthroscopy. While the rate of RTW was not reported for the matched control group in their study, WC patients showed a significantly greater pre- to postoperative improvement in several patient-reported outcome measures compared to the control group but underwent revision arthroscopy at a significantly higher rate (17.1% vs. 4.5%, p < 0.001). In a study of exclusively WC patients who underwent hip arthroscopy, Salvo et al. [12] reported a RTW rate of 55%, considerably lower than the rate identified among our WC patients. The high rates of RTW in this series could be potentially explained by the practice setting of the senior author, which is an academic center in a metropolitan area. This patient population may have different motivations and economic considerations in the calculation of RTW compared to other populations previously reported in the literature. Despite extensive data reporting that WC patients experience inferior postoperative outcomes, our findings demonstrated no significant difference in the rate of return when comparing patients with and without WC status. However, VAS of pain during work-related activities were significantly higher in WC patients compared to non-WC patients. It should be noted that while not statistically significant, the average time to RTW for WC patients was nearly twice as long as for non-WC patients (18.4 weeks vs. 9.9 weeks).
The reasoning behind investigations of WC patients is largely driven by a potentially misaligned economic incentive to delay a return to work. Active claims for workers’ compensation provide patients with a monetary incentive, as they may receive compensation for disability benefits or lost wages. These benefits may consciously or subconsciously prolong the rehabilitation process for WC patients. Once surgeons and employers grant work clearance, these claims are closed, and the associated benefits are terminated. There are many variables in the aggregate calculation, and WC insurance status is only one aspect that may affect patient motivation for a successful and expedient recovery. Despite potential delays in the return to work for patients with WC claims, their motivation to ultimately resume work is likely similar to that of non-WC patients. From this perspective, the results of this study are better explained with respect to the longer time taken to return to work among WC patients but not the overall rate of return.
Although WC status did not make a significant difference in the RTW analysis, we evaluated several other potential predictors of return. Adjusting for age, gender, BMI, and work intensity, we found that only BMI significantly correlated with time to return to work. Cohn et al. [25] evaluated return to work among non-WC patients undergoing hip arthroscopy and found a significant correlation between increasing work intensity and longer time to return. In comparison, the present study did not find any relationship between work intensity and the rate or time to RTW, but we also were not able to assess patients of “very heavy” work intensity. Age, gender, and BMI should all be considered when investigating the outcomes of hip arthroscopy. In their meta-analysis, Sogbein et al. [26] found that young, male patients with a BMI < 24.5 achieved significantly higher patient-reported outcome scores following hip arthroscopy, which certainly may play a role in the ability to resume employment. In the present study, the multivariable linear regression allowed us to account for these demographic variables as well as the level of work intensity when analyzing the amount of time patients took to return to work.
The work intensity level is an important aspect to consider with return to work. In the current study, most patients had occupations that were either “sedentary” or “light” as defined by the U.S. Bureau of Labor Statistics, which likely correspond to occupations that are primarily conducted at a desk. Since hip flexion and extended periods in a sitting position are some of the most common limitations of patients with FAIS, the resolution of these symptoms may explain the high rates of observed return to work in this cohort. Though the current study was underpowered to compare the rate of return to work between patients involved in heavy labor (n = 5), a prior systematic review found that patients with less physically demanding occupations demonstrated a significantly greater rate of return to work after hip arthroscopy [10]. Interestingly, those authors identified several studies which found patients that had more physically demanding professions actually returned to work at a greater rate [11,19,20,27]. Specifically, Thomas et al. [20] discovered within their military cohort that the highest return-to-duty rates were observed among individuals who had the most physically demanding positions. An interesting further area of research may be to compare military versus civilian patients who have similar levels of work intensity. The reasons for this are unclear, but a psychological aspect that could be further explored in this population might be patient resilience, which has been investigated in the hip arthroscopy and the anterior cruciate ligament reconstruction patient populations with respect to return to sports. Several studies have found significant positive correlations between increased resilience and a greater rate of return to play [28,29]. One investigation at the West Point U.S. Military Academy found that “grit”, a measure of psychological resilience, was correlated with successful completion of cadets’ initiation training and ultimately graduation, while cognitive ability was less predictive [30]. While psychological aspects of return to sport have become increasingly explored, this area of investigation with respect to a return to work is lacking, especially beyond the military population. It is important to note that while return to duty studies conducted in the military population account for a substantial portion of the hip arthroscopy RTW literature, these findings are not necessarily generalizable to the civilian population. For example, RTW has been examined extensively in the setting of rotator cuff repair (RCR), as this population is typically older and RTW may be a larger priority among these patients. A recent systematic review focusing on RTW after RCR found that the rate of return decreased significantly with increasing work intensity [31]. Furthermore, patients who returned to more physically demanding occupations after RCR were found to experience higher failure rates and achieved poorer patient-reported outcome scores [31].
These findings suggest that the relationship between labor intensity and RTW is complex, with multiple factors influencing the outcome. While physical demands may hinder RTW in certain cases, protective psychological patient characteristics, such as resilience or motivation, could negate those barriers. Therefore, understanding the relationship between physical and psychological factors is imperative to evaluate the likelihood of patients returning to work after surgical interventions. The findings in this study are valuable for patients who will undergo this procedure in the future, as a majority are working age will consider potential economic ramifications in their decision to undergo surgery. This study contributes to a growing body of work on data-driven preoperative counseling, enhancing the surgeon’s ability to establish realistic expectations and ultimately help patients enjoy greater satisfaction with their postoperative results [32,33]. These data have meaningful implications for patients undergoing hip arthroscopy, since many are at the peak of the economic productivity when they present with symptoms of FAIS. Lastly, these data may assist patients in making informed decisions and better plan for their timeline of postoperative rehabilitation and return to work.
This study is limited due to its retrospective design and is subject to selection bias. As patients were required to recall their baseline pain level and work activities, this study may be affected by recall bias. The limited size of the workers’ compensation group would not permit a rigorous comparative analysis due to risks of type II error. This was potentially observed in the comparison of time to return to work between WC and non-WC patients. Lastly, the existing hip arthroscopy literature provides little consistency across definitions for the type and intensity of work, full versus modified return to work, and whether permanent or temporary restrictions were placed on patients returning to the workplace [10]. Several measures were taken to address these issues, including defining work intensity levels using categories established by the U.S. Department of Labor [16]. Furthermore, we administered a detailed work activity survey, which distinguished between whether patients returned to full duties and the reasons for why they may not have returned to their preoperative work level.
5. Conclusions
Following hip arthroscopy for FAIS, there is a high rate of return to full work duties at an average of 9.3 weeks following surgery. Patients with workers’ compensation insurance status returned to work 9 weeks later than non-worker’s compensation patients. Increasing BMI was found to be a predictor of increased time to return to work.
Author Contributions
Conceptualization, T.Y.; methodology, A.J.H.; formal analysis, A.M.B.; investigation, J.T.; data curation, S.G.; writing—original draft preparation, Z.I.L.; writing—review and editing, D.S.S. and T.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of New York University School of Medicine (protocol code i20-01686, approved October 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available upon reasonable request to the authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jamil, M.; Dandachli, W.; Noordin, S.; Witt, J. Hip Arthroscopy: Indications, Outcomes and Complications. Int. J. Surg. 2018, 54, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Minkara, A.A.; Westermann, R.W.; Rosneck, J.; Lynch, T.S. Systematic Review and Meta-Analysis of Outcomes After Hip Arthroscopy in Femoroacetabular Impingement. Am. J. Sports Med. 2019, 47, 488–500. [Google Scholar] [CrossRef]
- Nho, S.J.; Beck, E.C.; Nwachukwu, B.U.; Cvetanovich, G.L.; Neal, W.H.; Harris, J.D.; Weber, A.E.; Mather, R.C. Survivorship and Outcome of Hip Arthroscopy for Femoroacetabular Impingement Syndrome Performed with Modern Surgical Techniques. Am. J. Sports Med. 2019, 47, 1662–1669. [Google Scholar] [CrossRef] [PubMed]
- Ricciardi, B.F.; Fabricant, P.D.; Fields, K.G.; Poultsides, L.; Zaltz, I.; Sink, E.L. What Are the Demographic and Radiographic Characteristics of Patients with Symptomatic Extraarticular Femoroacetabular Impingement? Clin. Orthop. Relat. Res. 2015, 473, 1299–1308. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Griffin, D.W.; Kinnard, M.J.; Formby, P.M.; McCabe, M.P.; Anderson, T.D. Outcomes of Hip Arthroscopy in the Older Adult: A Systematic Review of the Literature. Am. J. Sports Med. 2017, 45, 1928–1936. [Google Scholar] [CrossRef]
- Menge, T.J.; Briggs, K.K.; Dornan, G.J.; McNamara, S.C.; Philippon, M.J. Survivorship and Outcomes 10 Years Following Hip Arthroscopy for Femoroacetabular Impingement: Labral Debridement Compared with Labral Repair. J. Bone Jt. Surg. Am. 2017, 99, 997–1004. [Google Scholar] [CrossRef]
- Lovett-Carter, D.; Jawanda, A.S.; Hannigan, A. Meta-Analysis of the Surgical and Rehabilitative Outcomes of Hip Arthroscopy in Athletes with Femoroacetabular Impingement. Clin. J. Sport. Med. 2020, 30, 404–411. [Google Scholar] [CrossRef]
- O’Connor, M.; Minkara, A.A.; Westermann, R.W.; Rosneck, J.; Lynch, T.S. Return to Play After Hip Arthroscopy: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2018, 46, 2780–2788. [Google Scholar] [CrossRef]
- Davey, M.S.; Hurley, E.T.; Davey, M.G.; Fried, J.W.; Hughes, A.J.; Youm, T.; McCarthy, T. Criteria for Return to Play After Hip Arthroscopy in the Treatment of Femoroacetabular Impingement: A Systematic Review. Am. J. Sports Med. 2022, 50, 3417–3424. [Google Scholar] [CrossRef]
- Blaeser, A.M.; Mojica, E.S.; Mannino, B.J.; Youm, T. Return to Work After Primary Hip Arthroscopy: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2022, 51, 1340–1346. [Google Scholar] [CrossRef]
- Lee, S.; Cvetanovich, G.L.; Mascarenhas, R.; Wuerz, T.H.; Mather, R.C.; Bush-Joseph, C.A.; Nho, S.J. Ability to Return to Work without Restrictions in Workers Compensation Patients Undergoing Hip Arthroscopy. J. Hip Preserv. Surg. 2017, 4, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Salvo, J.P.; Hammoud, S.; Flato, R.; Sgromolo, N.; Mendelsohn, E.S. Outcomes after Hip Arthroscopy in Patients with Workers’ Compensation Claims. Orthopedics 2015, 38, e94–e98. [Google Scholar] [CrossRef]
- Sabetian, P.W.; Monahan, P.F.; Fox, J.D.; Jimenez, A.E.; Maldonado, D.R.; Saks, B.R.; Ankem, H.K.; Lall, A.C.; Domb, B.G. Workers’ Compensation Patients Improved After Hip Arthroscopy for Labral Tears: A 5-Year Outcome Propensity Score-Matched Study. Am. J. Sports Med. 2022, 50, 1281–1290. [Google Scholar] [CrossRef]
- Larson, C.M.; Wulf, C.A. Intraoperative Fluoroscopy for Evaluation of Bony Resection during Arthroscopic Management of Femoroacetabular Impingement in the Supine Position. Arthroscopy 2009, 25, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- Christensen, C.P.; Althausen, P.L.; Mittleman, M.A.; Lee, J.; McCarthy, J.C. The Nonarthritic Hip Score: Reliable and Validated. Clin. Orthop. Relat. Res. 2003, 406, 75–83. [Google Scholar] [CrossRef]
- Strength Levels: U.S. Bureau of Labor Statistics. Available online: https://www.bls.gov/ors/factsheet/strength.htm (accessed on 17 March 2023).
- Bolia, I.K.; Ihn, H.; Kang, H.P.; Mayfield, C.K.; Briggs, K.K.; Bedi, A.; Jay Nho, S.; Philippon, M.J.; Weber, A.E. Cutting, Impingement, Contact, Endurance, Flexibility, and Asymmetric/Overhead Sports: Is There a Difference in Return-to-Sport Rate After Arthroscopic Femoroacetabular Impingement Surgery? A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2021, 49, 1363–1371. [Google Scholar] [CrossRef] [PubMed]
- Mansell, N.S.; Rhon, D.I.; Meyer, J.; Slevin, J.M.; Marchant, B.G. Arthroscopic Surgery or Physical Therapy for Patients with Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial With 2-Year Follow-Up. Am. J. Sports Med. 2018, 46, 1306–1314. [Google Scholar] [CrossRef]
- Dutton, J.R.; Kusnezov, N.A.; Lanzi, J.T.; Garcia, E.J.; Pallis, M.P. The Success of Hip Arthroscopy in an Active Duty Population. Arthroscopy 2016, 32, 2251–2258. [Google Scholar] [CrossRef]
- Thomas, D.D.; Bernhardson, A.S.; Bernstein, E.; Dewing, C.B. Hip Arthroscopy for Femoroacetabular Impingement in a Military Population. Am. J. Sports Med. 2017, 45, 3298–3304. [Google Scholar] [CrossRef]
- Gigi, R.; Rath, E.; Sharfman, Z.T.; Shimonovich, S.; Ronen, I.; Amar, E. Hip Arthroscopy for Femoral-Acetabular Impingement: Do Active Claims Affect Outcomes? Arthroscopy 2016, 32, 595–600. [Google Scholar] [CrossRef]
- Kim, K.C.; Lee, W.-Y.; Shin, H.D.; Han, S.-C.; Yeon, K.-W. Do Patients Receiving Workers’ Compensation Who Undergo Arthroscopic Rotator Cuff Repair Have Worse Outcomes than Non-Recipients? Retrospective Case-Control Study. J. Orthop. Surg. (Hong Kong) 2018, 26, 2309499018802507. [Google Scholar] [CrossRef]
- Mirzayan, R.; McCrum, C.; Butler, R.K.; Alluri, R.K. Risk Factors and Complications Following Arthroscopic Tenotomy of the Long Head of the Biceps Tendon. Orthop. J. Sports Med. 2020, 8, 2325967120904361. [Google Scholar] [CrossRef]
- de Moraes, V.Y.; Godin, K.; Tamaoki, M.J.S.; Faloppa, F.; Bhandari, M.; Belloti, J.C. Workers’ Compensation Status: Does It Affect Orthopaedic Surgery Outcomes? A Meta-Analysis. PLoS ONE 2012, 7, e50251. [Google Scholar] [CrossRef]
- Cohn, M.R.; Wichman, D.M.; Newhouse, A.C.; Mehta, N.; Fu, M.C.; Chahla, J.; Nho, S.J. High Rate of Full Duty Return to Work After Hip Arthroscopy for Femoroacetabular Impingement Syndrome in Workers Who Are Not on Workers’ Compensation. Am. J. Sports Med. 2021, 49, 729–736. [Google Scholar] [CrossRef]
- Sogbein, O.A.; Shah, A.; Kay, J.; Memon, M.; Simunovic, N.; Belzile, E.L.; Ayeni, O.R. Predictors of Outcomes After Hip Arthroscopic Surgery for Femoroacetabular Impingement: A Systematic Review. Orthop. J. Sports Med. 2019, 7, 2325967119848982. [Google Scholar] [CrossRef]
- Silverman, A.R.; DeFroda, S.F.; Cohen, B.H.; Quinn, M.S.; Tabaddor, R.R. The Brief Resilience Scale Is Associated with Pre- and Short-Term Postoperative Outcomes Following Hip Arthroscopy. Hip Int. 2022, 32, 641–647. [Google Scholar] [CrossRef]
- Zhang, J.K.; Barron, J.; Arvesen, J.; Israel, H.; Kim, C.; Kaar, S.G. Effect of Patient Resilience and the Single Assessment Numeric Evaluation (SANE) Score on Return to Sport Following Anterior Cruciate Ligament Reconstruction Surgery. Arch. Bone Jt. Surg. 2021, 9, 512–518. [Google Scholar] [CrossRef]
- Duckworth, A.L.; Quirk, A.; Gallop, R.; Hoyle, R.H.; Kelly, D.R.; Matthews, M.D. Cognitive and Noncognitive Predictors of Success. Proc. Natl. Acad. Sci. USA 2019, 116, 23499–23504. [Google Scholar] [CrossRef] [PubMed]
- Perets, I.; Prat, D.; Close, M.R.; Chaharbakhshi, E.O.; Rabe, S.M.; Battaglia, M.R.; Domb, B.G. Patients Undergoing Hip Arthroscopy with Active Workers’ Compensation Claims Do Not Demonstrate Inferior Outcomes at Mid-Term. Hip Int. 2019, 29, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Haunschild, E.D.; Gilat, R.; Lavoie-Gagne, O.; Fu, M.C.; Tauro, T.; Forsythe, B.; Cole, B.J. Return to Work After Primary Rotator Cuff Repair: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2021, 49, 2238–2247. [Google Scholar] [CrossRef] [PubMed]
- Becker, R.; Döring, C.; Denecke, A.; Brosz, M. Expectation, Satisfaction and Clinical Outcome of Patients after Total Knee Arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1433–1441. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Kämpfen, S.; Munzinger, U.; Kramers-de Quervain, I. The Role of Patient Expectations in Predicting Outcome after Total Knee Arthroplasty. Arthritis Res. Ther. 2009, 11, R139. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).