Endoscopic Excision of Rare Large Maxillary Sinus Osteoma: A Case Report and Literature Review
Abstract
1. Introduction
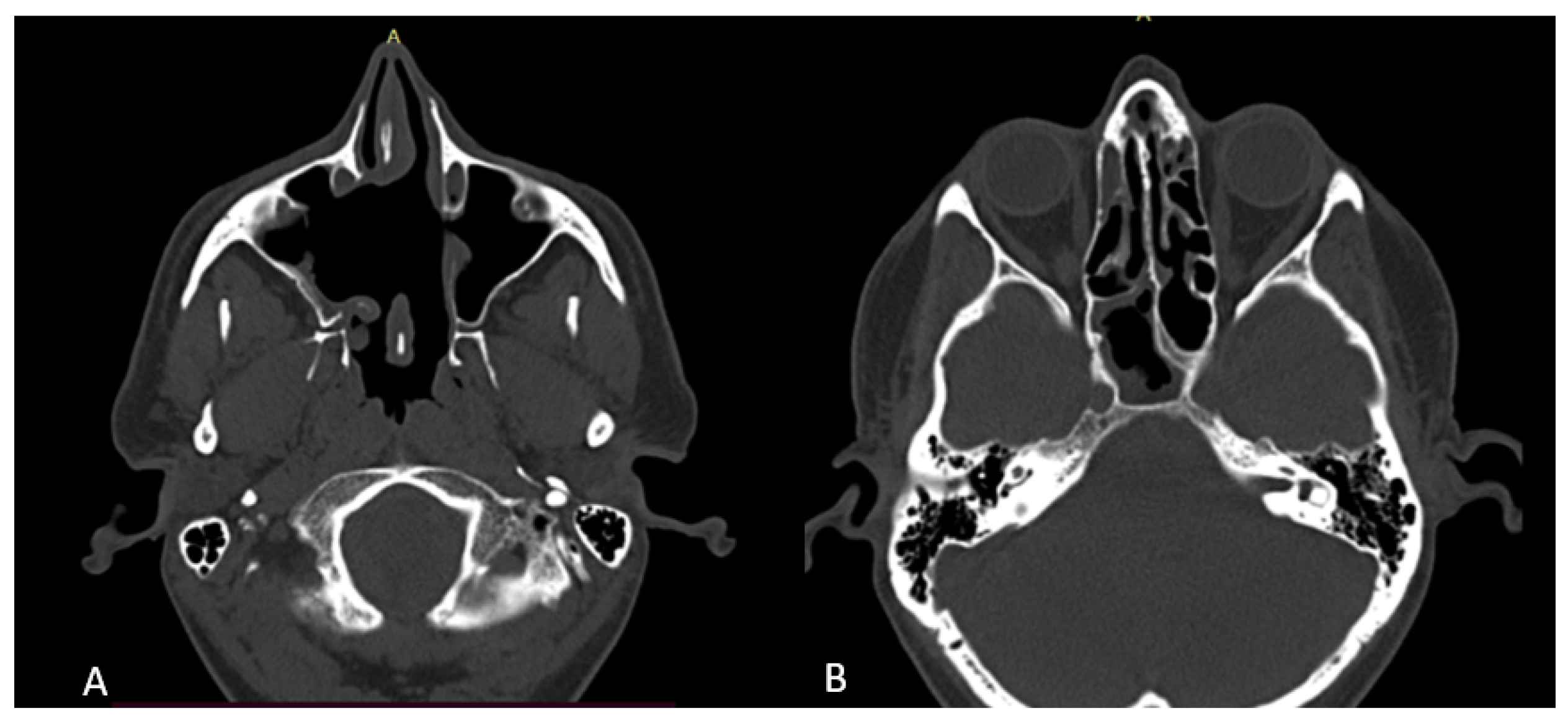
2. Case Presentation
3. Discussion
3.1. Epidemiology, Pathogenesis, Clinical Presentation
3.2. Diagnosis and Radiological Features
3.3. Therapeutical Management
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alotaibi, N.; Hanss, J.; Benoudiba, F.; Bobin, S.; Racy, E. Endoscopic removal of large orbito-ethmoidal osteoma in pediatric patient: Case report. Int. J. Surg. Case Rep. 2013, 4, 1067–1070. [Google Scholar] [CrossRef]
- Edmond, M.; Clifton, N.; Khalil, H. A large atypical osteoma of the maxillary sinus: A report of a case and management challenges. Eur. Arch. Oto-Rhino-Laryngol. 2011, 268, 315–318. [Google Scholar] [CrossRef]
- Sudhoff, H.; Theegarten, D.; Luckhaupt, H. Osteom der kieferhöhle. Laryngorhinootologie 2001, 80, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Arslan, H.H.; Tasli, H.; Cebeci, S.; Gerek, M. The management of the paranasal sinus osteomas. J. Craniofac. Surg. 2017, 28, 741–745. [Google Scholar] [CrossRef] [PubMed]
- Castelnuovo, P.; Valentini, V.; Giovannetti, F.; Bignami, M.; Cassoni, A.; Iannetti, G.M. Osteomas of the maxillofacial district: Endoscopic surgery versus open surgery. J. Craniofac. Surg. 2008, 19, 1446–1452. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Li, X.; Lv, L.; Yu, J.; Yang, C.; Xiong, H.; Liao, R.; Zhou, B.; Huang, X.; Liu, X.; et al. Improving the diagnosis of common parotid tumors via the combination of CT image biomarkers and clinical parameters. BMC Med. Imaging 2020, 20, 38. [Google Scholar] [CrossRef]
- Muderris, T.; Sevil, E.; Bercin, S.; Canda, B.; Kiris, M. Giant paranasal sinus osteomas: Surgical treatment options. J. Craniofac. Surg. 2014, 25, 1287–1291. [Google Scholar] [CrossRef]
- Miman, M.C.; Bayindir, T.; Akarcay, M.; Erdem, T.; Selimoglu, E. Endoscopic removal technique of a huge ethmoido-orbital osteoma. J. Craniofac. Surg. 2009, 20, 1403–1406. [Google Scholar] [CrossRef]
- Schick, B.; Steigerwald, C.; el Rahman el Tahan, A.; Draf, W. The role of endonasal surgery in the management of frontoethmoidal osteomas. Rhinology 2001, 39, 66–70. [Google Scholar]
- Koivunen, P.; Löppönen, H.; Fors, A.P.; Jokinen, K. The growth rate of osteomas of the paranasal sinuses. Clin. Otolaryngol. Allied Sci. 1997, 22, 111–114. [Google Scholar] [CrossRef]
- Eller, R.; Sillers, M. Common Fibro-osseous Lesions of the Paranasal Sinuses. Otolaryngol. Clin. N. A. 2006, 39, 585–600. [Google Scholar] [CrossRef]
- Langlie, J.A.; Hullfish, H.; Jabori, S.K.; Thaller, S.R. Diagnosis and Management of Craniofacial Osteomas. J. Craniofac Surg. 2023, 37253237. [Google Scholar] [CrossRef]
- Alkhaldi, A.S.; Alsalamah, S.; Tatwani, T. A Case of Giant Ethmoid Sinus Osteoma. Cureus 2021, 13, e18011. [Google Scholar] [CrossRef]
- 14. Tarsitano, A.; Ricotta, F.; Spinnato, P.; Chiesa, A.M.; Di Carlo, M.; Parmeggiani, A.; Miceli, M.; Facchini, G. Craniofacial Osteomas: From Diagnosis to Therapy. J. Clin. Med. 2021, 10, 5584. [Google Scholar] [CrossRef]
- Mlouka, M.; Tlili, M.; Hamrouni, A.; Selmi, R.; Khanfir, F.; Khalfi, M.S.; Ben Amor, F. Lateral maxillary sinus floor elevation in the presence of a sinus osteoma: A case report. Clin. Case Rep. 2021, 9, e04124. [Google Scholar] [CrossRef] [PubMed]
- Aldren, C.P.; Soames, J.V.; Birchall, J.P. Bony remodelling in an osteoma of the paranasal sinuses. J. Laryngol. Otol. 1993, 107, 633–635. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.S.; Perzin, K.H. Non-epithelial tumors of the nasal cavity, paranasal sinuses, and nasopharynx: A clinicopathologic study. II. Osseous and fibro-osseous lesions, including osteoma, fibrous dysplasia, ossifying fibroma, osteoblastoma, giant cell tumor, and osteosarcoma. Cancer 1974, 33, 1289–1305. [Google Scholar] [CrossRef] [PubMed]
- Georgalas, C.; Goudakos, J.; Fokkens, W.J. Osteoma of the Skull Base and Sinuses. Otolaryngol. Clin. N. A. 2011, 44, 875–890. [Google Scholar] [CrossRef] [PubMed]
- Humeniuk-Arasiewicz, M.; Stryjewska-Makuch, G.; Janik, M.A.; Kolebacz, B. Giant fronto-ethmoidal osteoma—Selection of an optimal surgical procedure. Braz. J. Otorhinolaryngol. 2018, 84, 232–239. [Google Scholar] [CrossRef]
- Raponi, I.; Giovannetti, F.; Cacciatore, F.; Di Carlo, D.; Valentini, V. Endoscopic Forehead Approach for Minimally Invasive Frontal Osteoma Excision. J. Craniofac. Surg. 2020, 31, e767-9. [Google Scholar] [CrossRef]
- Article, O. Frontoethmoidal and Intraorbital Osteomas. Arch. Otolaryngol.—Head Neck Surg. 2014, 138, 498–504. [Google Scholar]
- Huang, H.M.; Liu, C.M.; Lin, K.N.; Chen, H.T. Giant ethmoid osteoma with orbital extension, a nasoendoscopic approach using an intranasal drill. Laryngoscope 2001, 111, 430–432. [Google Scholar] [CrossRef] [PubMed]
- Tan, B.K.; Chandra, R.K. Postoperative prevention and treatment of complications after sinus surgery. Otolaryngol. Clin. North. Am. 2010, 43, 769–779. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Irimia, I.M.; Gata, A.; Puscas, I.M.; Covaliu, B.F.; Albu, S. Endoscopic Excision of Rare Large Maxillary Sinus Osteoma: A Case Report and Literature Review. Surgeries 2023, 4, 317-324. https://doi.org/10.3390/surgeries4030032
Irimia IM, Gata A, Puscas IM, Covaliu BF, Albu S. Endoscopic Excision of Rare Large Maxillary Sinus Osteoma: A Case Report and Literature Review. Surgeries. 2023; 4(3):317-324. https://doi.org/10.3390/surgeries4030032
Chicago/Turabian StyleIrimia, Ioana Maria, Anda Gata, Irina Maria Puscas, Bogdan Florin Covaliu, and Silviu Albu. 2023. "Endoscopic Excision of Rare Large Maxillary Sinus Osteoma: A Case Report and Literature Review" Surgeries 4, no. 3: 317-324. https://doi.org/10.3390/surgeries4030032
APA StyleIrimia, I. M., Gata, A., Puscas, I. M., Covaliu, B. F., & Albu, S. (2023). Endoscopic Excision of Rare Large Maxillary Sinus Osteoma: A Case Report and Literature Review. Surgeries, 4(3), 317-324. https://doi.org/10.3390/surgeries4030032






