1. Introduction
Submandibular glands account for about 79% of all salivary calculi and for about 50% of benign obstructive salivary gland diseases [
1]; among these, 34% are localized in the Wharton’s duct, 57% in the hilum and 9% inside the gland [
2]. Salivary stones are extremely common in submandibular glands because of the mucous nature of its secretum.
Surgically speaking, submandibular gland sialolithiasis can be addressed in two different ways: by gland removal or by stone removal. The removal is easily performed intraorally through duct incision and marsupialization or interventional sialendoscopy if the stone is located in the distal or mid-third of the Wharton’s duct, while duct stenosis or persistence of residual stones is possible especially in case of proximal and deep stones. Submandibular gland excision is still proposed for deep hyloparenchymal stones via traditional transcervical approach with well-known functional and aesthetic sequelae (marginalis mandibulae nerve injury, visible surgery scar); to try and avoid them, a modified transcervical sialadenectomy via a facelift or transhairline incision [
3,
4,
5,
6] has been described for chronic obstructive disease. However, there is mounting clinical and experimental evidence that salivary glands can regain useful function after stone removal [
7]: that is why, in the last twenty years, conservative transoral and sialendoscopy-assisted transoral surgeries for deep hylar and parenchymal submandibular stones have been developed and are increasingly becoming popular. Four main techniques of transoral submandibular gland surgery in the management of submandibular gland lithiasis can be identified: duct slitting procedure, duct preservation technique, sialoendoscopy-assisted approach and intra-oral sialoadenectomy. The role of the newly arising 3D-4K exoscope-assisted sialolithotomy technique will also be discussed.
The first technique that comes to mind involves a prolonged duct dissection of the upper part of Wharton′s duct. This allows the stone to be reached up to the hylo-parenchymal region [
8] without risking damage to the lingual nerve. A conservative transoral approach to the hylar region has been proposed by McGurk et al. [
7] and by Capaccio et al. [
1,
9]: an incision is made at the medial border of the gland while the tongue is medially retracted and the gland is pushed up. This tenses the floor of the mouth and allows localization of the lingual nerve and the Wharton’s duct. A limited longitudinal ducotomy is performed, right above the calculus which is shelled out [
10]. In the aforementioned article, 186 patients underwent this type of surgery, with 76% of patients being free from troublesome symptoms and an overall satisfaction rate of 92%. Most common complications were persistence of illness, which required traditional transcervical submandibular sialadenectomy, and the development of post-operative ranula. A total of 6% of the patients experienced mild lingual nerve impairment. It is worth noting that long-dating chronical sialoadenitis can result in multiple nerve injury (e.g., lingual and hypoglossal nerve) during surgery because of the amount of fibrous and retracting tissue which welds the lingual nerve to the gland’s body [
7]. Sialoendoscopy-assisted transoral surgery (the so-called “combined approach) is a modification of the previous technique that includes the use of the sialendoscope to better locate the stone in the hilo-parenchymal region, or to check for any residual intra-parenchymal stones or debris through the incision [
1]. It can also be used to remove stones smaller than 5 mm but too big to be extracted by the papilla [
9]. A minimal retropapillar incision is performed in order to prepare the main duct and allow the use of endoscopic instruments such as baskets or holmium laser or to facilitate a sialodochotomy to remove the stone. A few complications may arise from this procedure, including ductal wall perforation, unsuccessful ductal dilation and post-operative restenosis of the Wharton’s duct [
11]. In addition, failure may occur in patients with deep stone location, and a 14.3% rate of recurrent obstructive symptoms due to residual stones has been observed during the follow-up period. Nonetheless, should the sialolithiasis occur again, this technique allows for re-exploration of the ductal system which is kept intact during surgery [
1].
To avoid facial nerve damage, an intraoral submandibular sialadenectomy consisting of an incision running from the orifice of the Wharton’s duct to the retromolar region has been described by Hong and Yang [
3,
10]; the submandibular gland is dissected and totally removed, with careful attention to the main anatomical landmarks, i.e., the lingual nerve and the Wharton’s duct (ligated just above its mid-third). Then, transoral robotic surgery (TORS) was introduced, which represented a shift from the oncological objective to the functional one: transoral robotic surgery (TORS) was introduced as an effective treatment of salivary stones under the name of TORS-assisted sialolitothomy (TORS-S), which was proposed in the year 2016 [
12,
13], and in 2019, a robotic approach was described in detail [
14]. Major complications are almost non-existent. A robotic submandibular sialadenectomy can be performed transorally with sialoendoscopic assistance for deep parenchymal stones [
14]. However, this method has been performed on only a small number of patients; it lacks important details, such as a clear explanation of how the patient′s cart is docked. Finally, the introduction of VITOM 3D-4K exoscope (Karl Storz) has proven itself to be useful in terms of surgeon’s aid and learning purposes. Its usefulness in transoral techniques has only recently come to discussion, and to date, only one case report of VITOM-assisted sialolithotomy has been published to treat a stone located in the distal tract of the duct [
2]. The use of the exoscope represents a valid option for transoral removal of calculi that allows precise surgical dissection of the oral floor with a real 3D-4K magnification of the anatomical structures and a wide panoramic view, thus reducing the risks for iatrogenic lesion of the lingual nerve. Furthermore, it has a high potential for training and educational purposes since the operating room staff can better perceive and be involved in the procedure. The three-dimensional visualization of the deep and posterior part of the oral floor with enhanced view of the relation between lingual nerve, Wharton’s duct and hilo-parenchymal tissue and the better post-operative subjective recovery seem to be main strengths of this technique.
The aim of the study was to compare the results of two different transoral surgical techniques (TORSS and VITOM-assisted surgery) used to manage a bilateral hilo-parenchymal submandibular stone in the same patient.
2. Case Report
A 69-year-old man with a history of chronic submandibular sialadenitis came to our attention; a diagnosis of bilateral submandibular stones was assigned after clinical evaluation and palpation of the oral floor. His medical history included heavy smoking and hypertension.
The patient underwent pre-operative CT showing two hilo-parenchymal submandibular gland stones, 20 mm on the right submandibular gland and 10 mm on the left gland (
Figure 1).
The patient met criteria for a transoral surgical approach, and a decision was made to first address the right side with TORSS and then the left side with VITOM-assisted sialolithotomy.
The procedure was performed under general anesthesia with a nasotracheal tube.
TORS-S—Docking of the da Vinci Si system was carried out according to the approach explained in the aforementioned article [
14]: the mouth was held open using a lateral mouth gag which was introduced inside the patient’s oral cavity, the patient’s cart with the three robot arms was docked behind the head of the patient at an angle of 30°, on the side opposite to the affected gland (thus on the left side, in this case), and a downward-facing 30° HD robotic endoscope was placed into the robotic endoscope holder. Two robotic 5 mm instruments, a Maryland dissector and a monopolar cautery with spatula tip were placed into arms 1 and 3 according to the side of the stone. A square-shaped tongue retractor covered by rough gauze was positioned to retract the tongue to the contralateral side and to flatten the oral floor. The location of the stone was carefully marked on the mucosal surface by means of palpation and its borders were drawn over the oral floor’s mucosa with a dermal marker. The first operator sat at the console while surgeon’s aid sat at the patient’s head contralateral to the affected side and was responsible for suction, tongue retraction and pushing up of the submandibular region. Using monopolar cautery, an oblique incision was made just over the calculus area, on the oral pelvis, and prolonged caudally and cranially. The surgical incision was then carefully deepened, preserving both the lingual nerve, by moving it laterally, and the Wharton’s duct (
Figure 2).
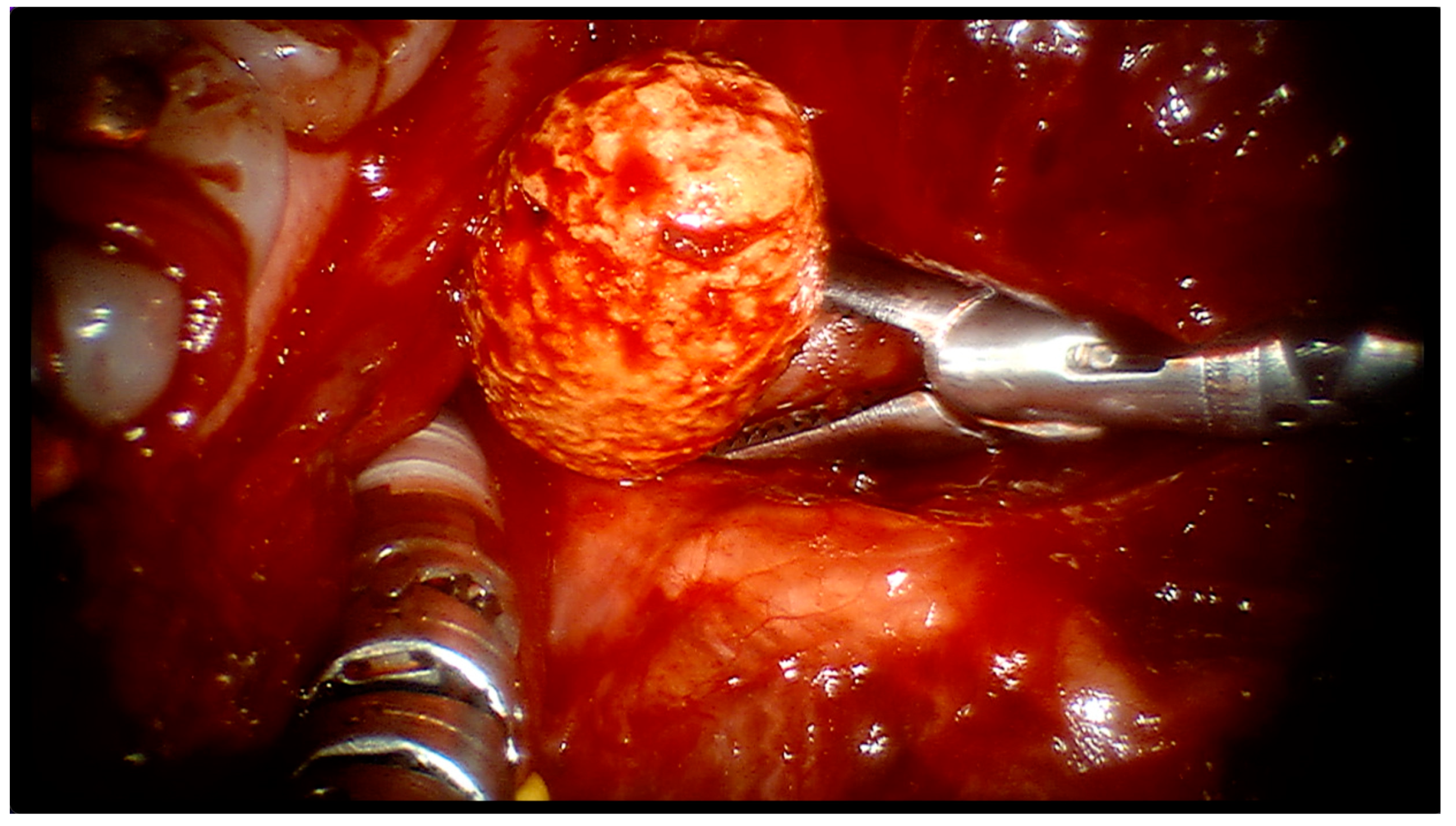
The calculus was then pushed up and away from the gland’s hilo-parenchymal region, and the surgical cavity was carefully and thoroughly irrigated with saline solution to clear out any debris (
Figure 3).
The surgical incision was sutured using Polysorb 3-0 reabsorbable interrupted stitches. The procedure required 35 min in total (15 min setting, 20 min surgery).
VITOM—The VITOM exoscope was then placed over the surgical field to obtain magnification of the left oral hemipelvis and to better identify the Wharton′s duct papilla, and a 3D-4K monitor was placed just over the surgical bed. The first operator and surgeon’s aid both stood at the patient′s head and wore 3D glasses while staring at the monitor and performing sialolithotomy (
Figure 4).
Using monopolar cautery, an incision was made just over the calculus, located by means of bimanual palpation. The hilo-parenchymal region was carefully dissected, and the calculus was extracted. The surgical cavity was thoroughly washed with a saline solution and the surgical incision was then closed with Polysorb 3-0 reabsorbable interrupted stitches. The procedure required 40 min (10 min setting, 30 min surgery). Total surgery time was 75 min.
The patient was discharged two days later, with prescription of antibiotics for one week and chlorexidin-based mouthwash. The patient was also instructed to chew bubblegum and mints to promote salivation and avoid duct stenosis. Soft and cold diet was administered until first post-operative control.
Post-operative control two weeks after surgery showed a complete repair of surgical wounds with no signs of swelling or infection, and no late/minor complications as well. The patient proved to be free of symptoms after a 6-month and 12-month follow-up.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Ethics Committee of the University of Ferrara (ref. no. 184792, approved on 15 July 2022).
3. Discussion
The frequency of application of transoral removal of deep submandibular calculi is growing worldwide, and the procedure is replacing traditional invasive transcervical sialadenectomy. Recent reviews have reported the superiority of the transoral technique in comparison to the transcervical approach in terms of cosmetic and functional results [
15,
16]. However, not all patients are suitable for such a transoral approach: an adequate diagnostic iter (US and CT most importantly, and MRI if needed) is mandatory to identify the exact position of the stones and the presence of inflammatory or infective radiological signs that may influence the result of the surgery; it must not be forgotten that transoral techniques are best applicable when no concurrent sialoadenitis is present. According to this experience (based on the da Vinci Si system produced by Intuitive), best suitable candidates for TORS are large (>7 mm) hilar calculi.
We compared the results of two different transoral surgical approaches for hilo-parenchymal submandibular stones, namely transoral robotic salivary surgery (TORSS) and VITOM-assisted sialolithotomy: surgery time was similar (40 min for TORSS and 35 min for VITOM) and a successful result (i.e., complete removal of the stones) was obtained in both surgical procedures without any major or minor complications, as the patient continues to stay free of symptoms even after a 1-year follow up.
The main goal of both techniques is to obtain a better view and magnification of the surgical field and to avoid injuries to noble structures: the lingual nerve, making its way in a “horseshoe” fashion under the Wharton’s duct, and the Wharton’s duct itself. After stone removal, the recovery of glandular function can then be preserved; in this regard, both techniques obtained the expected result in terms of safety and efficacy. Success percentage in hilar submandibular stones is high, around 94% [
17]. Few data report on initial experience with transoral robotic salivary surgery for deep submandibular stones, and the results are encouraging [
13]. On the other hand, only one case report has been recently published on the use of 3D-4K VITOM to assist the surgeon in removing a stone located in the distal third of the main submandibular duct [
14]. When compared to traditional 2D endoscopy, 3D endoscopy appears to have better sharpness and allows the operator to have stereoscopic depth perception; 2D endoscopy images are, however, brighter. The two procedures are almost similar in terms of outcome, but the 3D guided exploration of the oral floor seems to provide a better view of the Wharton’s duct and the lingual nerve, especially near the submandibular parenchyma [
1].
Both techniques have some downsides: TORS is surely more expensive (1–2.000.000 dollars) than VITOM exoscope (2–300.000 dollars), and a specific training is required to perform the procedure with TORS, not only for the first operator but also for the OR staff, since docking of the robot cart requires some kind of knowledge. During the TORS procedure, two robotic arms work inside the oral cavity, but the optical arm, suction device and one hand of the surgeon’s assistant must be added to the count: the surgical field can become crowded at some point. Major complications, already very low in number with classical transoral technique, are almost nonexistent when using TORS, with only a possible persistent tingling of the tip of the tongue still present at 3 months after surgery [
18]. VITOM-assisted surgery, on the other hand, has become more and more popular among different medical specialties such as reconstructive microsurgery, achieving interesting results. Its use in submandibular gland sialolithotomy appears of utmost interest, because it makes sialolithotomy easier and safer [
19] than the traditional one carried out by direct vision and/or loupe magnification: in this case, the optical arm (that is, the VITOM itself) is positioned outside of the surgical field, thus freeing space for the surgeon to operate with traditional instruments. Following the goal of optimizing a better visualization of surgical planes and due to technological advancements, a 3D video-assisted transoral removal of submandibular stones by a 4K VITOM or 3D VITOM exoscope with the Artip Cruise system has been recently described [
19]: the system allows for a motorized positioning of the VITOM system, which can be stored inside the system’s memory and easily recalled when needed, thus making the system docking easier, faster and precise. Nevertheless, sharing surgery moments in narrow fields has always been a limit when learning ENT surgery (e.g., septoplasty): VITOM has shown itself to have the potential to overcome it.