Abstract
Breast implant illness refers to a combination of different symptoms related to breast implant surgery, including fatigue, brain fog, and arthralgias. This malaise occurs after cosmetic and reconstructive breast surgeries, although it has not been proven to be a disease. Even recent studies have reported concluding statements of the etiology, diagnosis, and treatment as unclear and widely unknown. Therefore, this review aimed to determine the associations between the manifestations of breast implant illness in surgery and breast reconstruction, as well as the autoimmune responses involved. Complications associated with breast implants include breast pain, capsular contracture, infections, as well as other manifestations specific to breast reconstruction. Moreover, patients with implants may present with new-onset systemic sclerosis, Sjögren’s syndrome, and connective tissue diseases. However, the incidence of capsular contracture has steadily decreased with each generation of implants, particularly since the development of textured implants, as well as with the use of antibiotics and antiseptic pocket irrigation. However, the incidence of anaplastic large cell lymphoma has increased with the use of textured implants. Remarkably, the autoimmune response to these implants remains unclear. Therefore, close follow-up, careful observation of any symptom presentation, and evidence-based treatment decisions are necessary for patients with breast implants.
1. Introduction
Outstanding advancements have been made in the medical field since the inception of synthetic prosthetics [1,2]. Presently, prosthetics have changed disease therapeutics and improved the quality of life for many patients [3]. Globally, a portion of the medical community has been skeptical about the use and safety of cosmetic silicone breast implants (SBI) [4]. This is mainly due to the absence of physiologic function and the immense popularity of breast surgery worldwide, with 287,085 interventions in 2019 and 193,073 in 2020 in the United States alone [5].
New concerns regarding the use of SBI have emerged apart from infection and immune rejection [6]. Asymmetry, breast pain, capsular contracture, implant rupture, infections, and breast implant-associated anaplastic large cell lymphoma have been reported to date [7,8]. Particularly, patients have reported symptoms of new-onset autoimmune disorder (18%), depression (19%), hair loss (21%), anxiety (24%), arthralgias (25%), brain fog (25%), and fatigue (49%) after SBI surgery, leading to a new term being coined for this syndrome: breast implant illness (BII) [9,10].
BII refers to a state of patient-reported malaise including various symptoms after cosmetic as well as reconstructive breast surgeries, although it is not yet proven to be a disease per se [11]. Correspondingly, an increasing number of patients attribute their symptoms to SBI surgery, with 969 reports of BII as of 2018 [12,13]. However, no association has been found between SBI and BII [14]. Moreover, recent studies on the spectrum of symptoms have not been able to determine the etiology or diagnosis of BII or identify a treatment protocol for it [9,15].
Therefore, this review aimed to analyze the known associations of the surgical, autoimmune, and breast reconstruction treatment fields of BII. Further, capsular contracture, breast implant-associated anaplastic large cell lymphoma, biofilms, and infections, as well as the role of silicone, related somatic syndromes, explantation, and reported signs and symptoms of BII are intricately discussed herein.
Methodology of Literature Research
We searched the Google Scholar and PubMed databases using “breast”, “implant”, and “illness” as the keywords from 2016 to date. Original and review articles were included and indistinctly revised for content having the specific keywords.
2. Surgical Implications
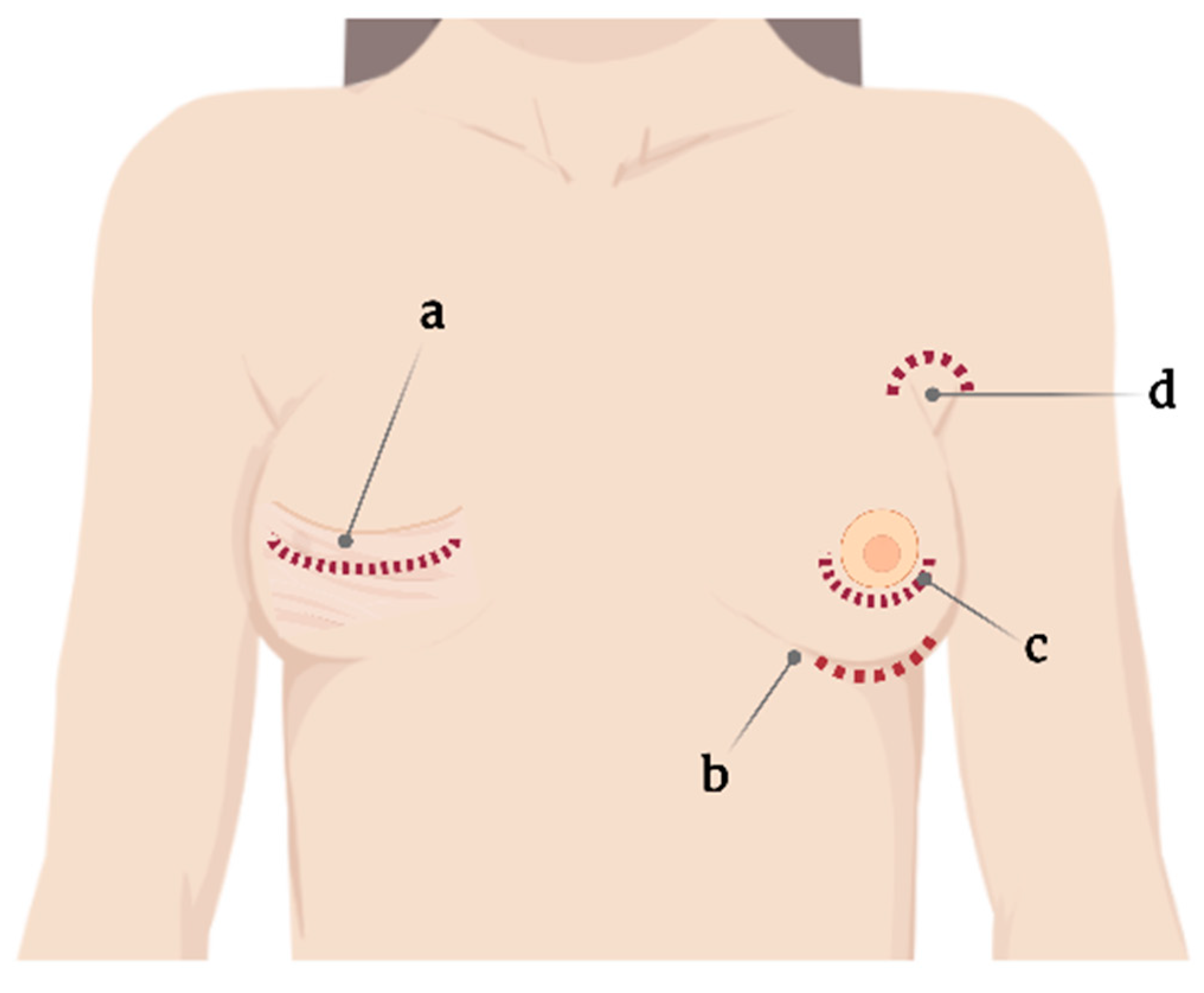
One standard type of SBI and surgical planning cannot be used for all, and the choice is usually based on the surgeon’s experience [16]. Correspondingly, SBI placement involves several incision sites that appear as axillary, inframammary, periareolar, and mastectomy scars [16,17] (Figure 1). Moreover, each incision site provides different degrees of tissue manipulation [18].
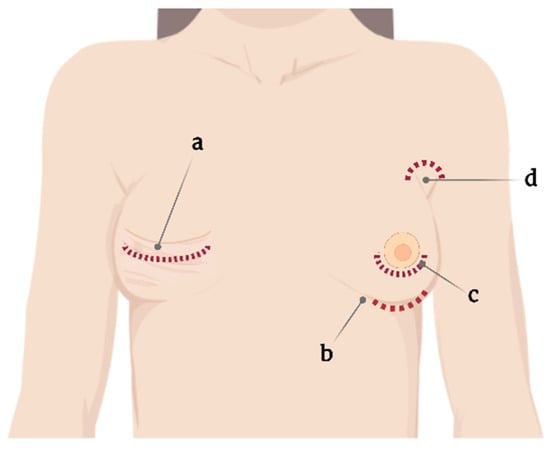
Figure 1.
Current incision sites for silicone breast implant placement. (a) Mastectomy scar, (b) submammary, (c) periareolar, and (d) axillary.
Specifically, the periareolar incision site shows a higher incidence of capsular contracture (6.9%) compared with inframammary incision (4.5%) [19]. When using such an approach, large ducts containing endogenous bacteria are dissected, resulting in potential implant contamination, subsequently leading to biofilm formation and further capsular contracture [20].
2.1. Capsular Contracture
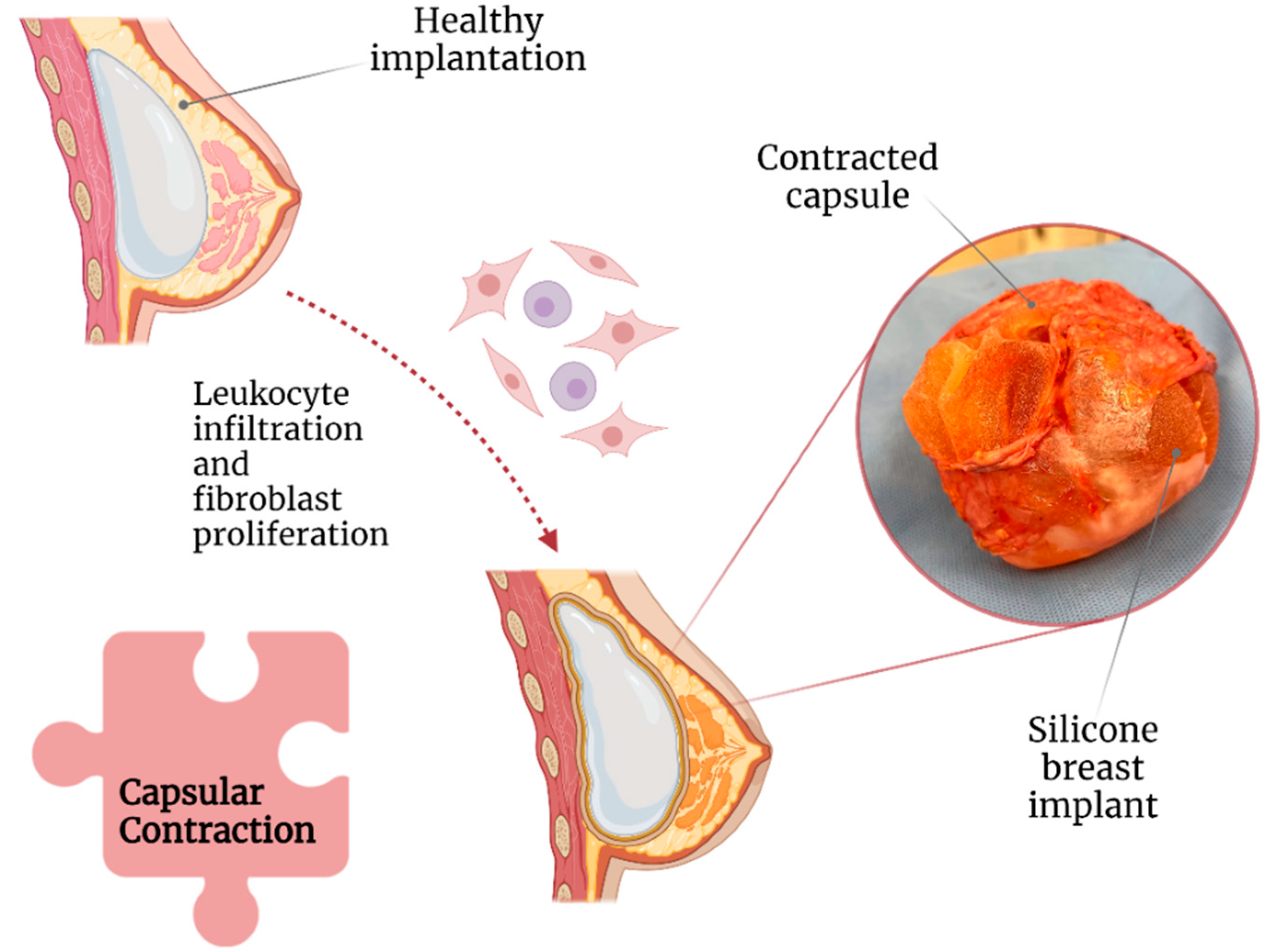
Capsular contracture is one of the most common complications after breast implant surgery (Figure 2) [21]. Currently, according to Baker staging, capsular contracture can be of four degrees [22] and is believed to be caused by leukocytic infiltration and fibroblast proliferation around the implant [23]. Capsular contracture is observed in up to 20% of patients with SBI, with patients with a body mass index of >30 kg/m2 and undergoing complete breast reconstructions being at an increased risk [24,25].
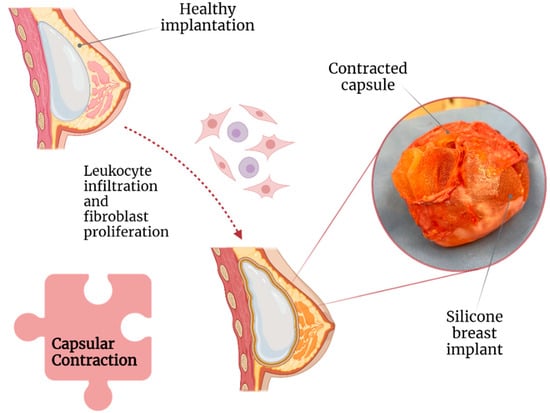
Figure 2.
Association of capsular contraction with breast implant illness.
Moreover, based on its stage, capsular contracture can result in significant breast pain, deformity, and induration [26]. A study revealed that capsular contracture and BII were the cause of explantation in 14.7% and 11.2% of 197 patients, respectively [11]. Correspondingly, a meta-analysis concluded that the following factors could play a role in capsular contracture development: (1) breast reconstructive surgery, (2) postoperative hematoma, and (3) axillary surgical approach. All of them are possibly due to increased tissue manipulation and dissection [16].
Capsular contracture is more common in submammary implants, perhaps because of insufficient barrier protection from the pectoral muscle against local bacteria [16,27]. Some studies have suggested that the degree of capsular contracture is correlated with capsular thickness, but this remains controversial [28,29]. In terms of the texture of the SBI, a follow-up study including 2560 patients revealed an adjusted relative risk of 2.25 (95% confidence interval) for capsular contracture in smooth implants compared with textured ones [27]. Similarly, microtextured implants have lower rates of capsular contracture compared with macrotextured ones [30].
Since its commercialization in 1962, the SBI has been used in plastic surgery [31]. Throughout the years, each generation of SBI evolved to create a more “natural feel” through the addition of a silicone shell (first generation) and gel (second generation), as well as a polyurethane textured surface [32]. Eventually, the third generation of SBI was created using a polymer shell to mimic the effects of polyurethane to reduce capsular contracture [16,25].
The use of a surgical bra has been associated with higher rates of capsular contracture, showing an adjusted relative risk of 2.9 [27]. In contrast, the use of acellular dermal meshes for implant support reduced the incidence of capsular contracture [33]; this indicates that the mesh can serve as a protective barrier against breast microbiota and potentially alleviate the immune response against the implant [34].
2.2. Texture of SBI and Anaplastic Large Cell Lymphoma
Textured implants were introduced around 1970 in an attempt to reduce the incidence of capsular contracture [29]. Among the micropatterning techniques that were used, imprinted textured SBI has had the lowest rate of capsular contracture (3.8%) compared with foam (4.9%), salt-loss textured (5.27%), and smooth (15.5%) SBIs [35].
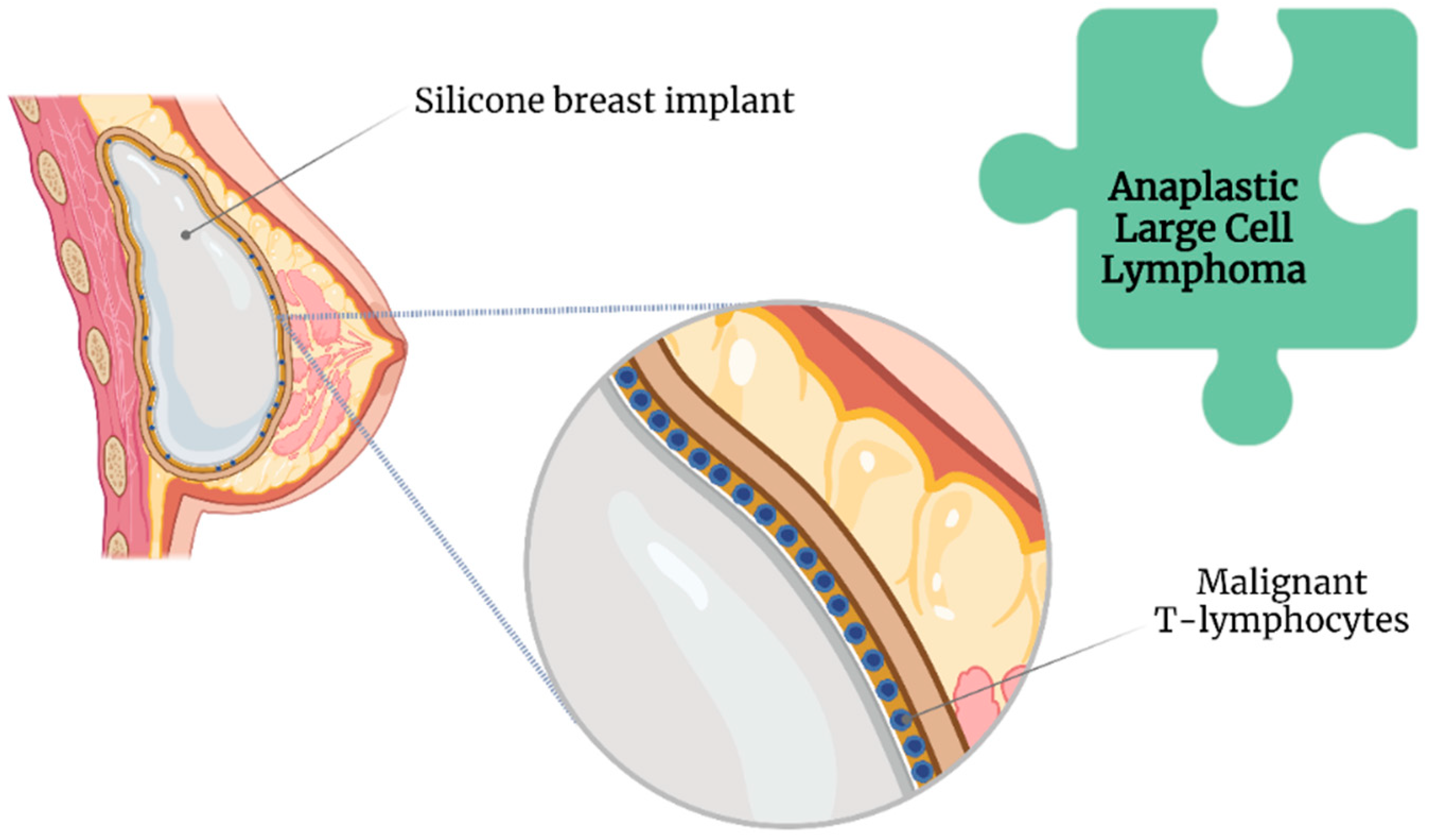
Nonetheless, compared with smooth SBI, a textured SBI has been highly associated with breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) [36] (Figure 3).
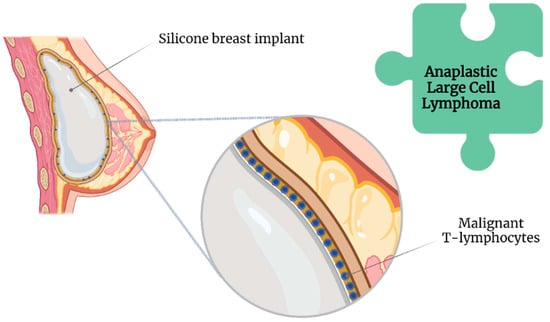
Figure 3.
Association of anaplastic large cell lymphoma with breast implant illness.
The Food and Drug Administration has requested the withdrawal of all Biocell textured SBI because of this association [37]. Likewise, Allergan has issued a global recall of their implants [37]. However, the lifelong risk of developing BII ranges between 0.0017 and 0.028, even with an increased incidence of BIA-ALCL [38].
Although routinely performed, en bloc capsulectomy, consisting of complete SBI removal within the capsule along with a margin of healthy tissue [39], is only recommended in the presence of BIA-ALCL [40]. This recommendation is given because of the reported invasiveness as well as increased surgical risk, discomfort, recovery time, and the absence of proven additional benefits in patients with mild symptoms [41].
Furthermore, no current evidence indicates that a prophylactic capsulectomy reduces the risk of BIA-ALCL [42].
2.3. Biofilms
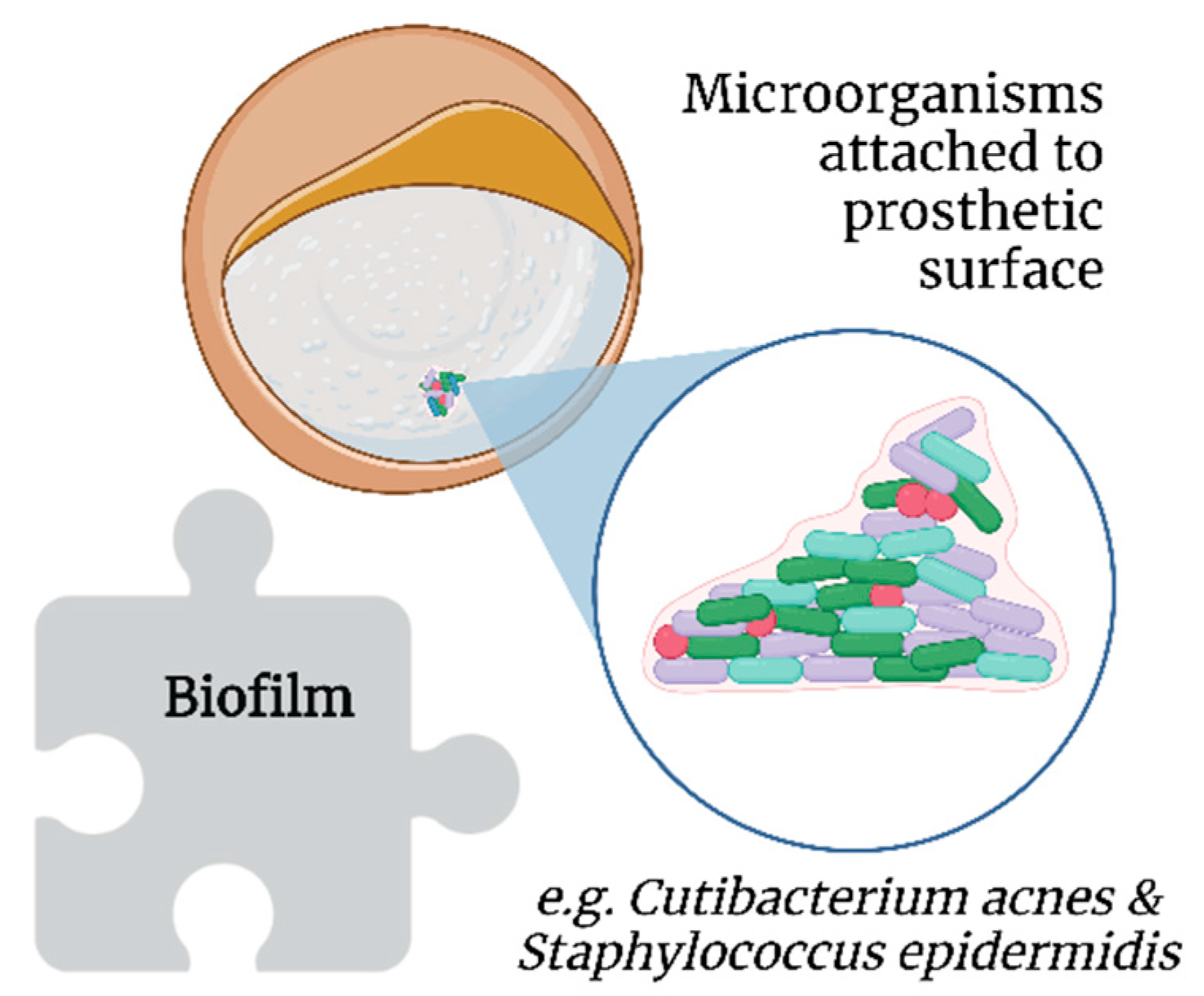
By definition, biofilms are colonies of one or more types of microorganisms living in symbiosis [34,43]. Unlike bacteremia, a biofilm does not present with the classic symptoms of infection as it induces a different immunological response [44]; this is more worrisome in the long term, as it involves chronic and significant immunological activation [45] unless the patient is immunosuppressed [46].
Biofilms further protect bacteria from host immune responses and antimicrobial therapy [47]. Extracellular insoluble polysaccharides secreted by microorganisms allow the adhesion of biofilms to the surface of prosthetic materials, such as SBI (Figure 4) [48]. However, biofilms are not exclusive to SBI [49].
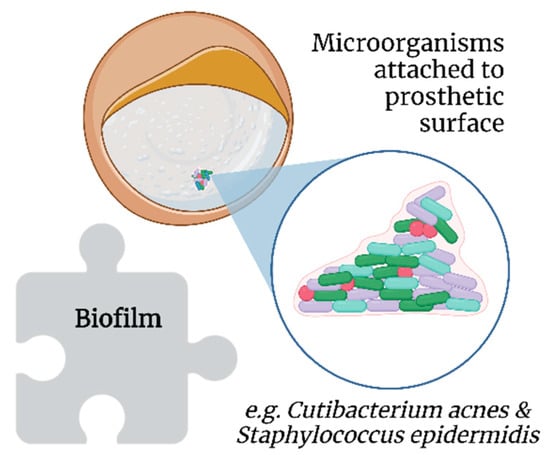
Figure 4.
Association of biofilms with breast implant illness.
Cutibacterium acnes (formerly Propionibacterium acnes) and Staphylococcus epidermidis, which are part of breast microbiota, are common in implant biofilms [50]. Additionally, thicker biofilms have been observed on textured SBI in vitro, probably because of the increased surface area compared with smooth SBI [51]. Moreover, C. acnes has been posited to contribute to the development of BII, as its presence allows for persistent low-grade inflammation and resultant capsular contracture, which are two mechanisms proposed as key factors in the genesis and progression of BII [52].
Two comparative clinical trials reported a 10-fold decrease in capsular contracture with the use of antibiotic or antiseptic pocket irrigation during cosmetic breast surgeries, thus supporting the role of biofilms in capsular contracture [19,53,54]. Further, povidone–iodine [30] and chlorhexidine gluconate have been shown to reduce biofilm-related capsular contracture [55,56].
2.4. Infections
As in many other circumstances, the introduction of foreign material into the body increases the risk of infection [49]. Specifically, infections are reported in 2.6% of SBI surgeries, predominantly because of inoculation during the surgical procedure, followed by hematogenous or contiguous spread [16,18].
Several authors have reported chronic infections in SBI capsules [21,34,55]. Such infections can cause capsule growth and further contraction [57]. Chronic infections have been posited to play a role in the genesis of breast implant-associated anaplastic large-cell lymphoma [28,58].
Patients with chronically infected capsules or synovial metaplasia reportedly have the best symptom resolution after explantation [57]. Notwithstanding, false-negative results account for 30% of cases in the field of SBI swab testing [59]. Thus, techniques such as extended culturing protocols and sonication have been suggested [60], which have shown 20% higher sensitivity (81% vs. 61%) and 99% specificity for bacterial detection in other prosthetic infections compared to simple culturing techniques [59,61].
3. Autoimmune Responses
SBI surgery requires a specialized and highly detailed procedure that must consider certain biological aspects, including BII [24]. The role of autoimmune responses on the implant is a major concern associated with to BII [62,63,64,65]. Nevertheless, some authors are of the opinion that the term BII must be included with other autoimmune disorders or functional somatic syndromes [63,66,67,68].
3.1. The Immune Response to SBI
Somatic syndromes are predominantly characterized by subjective symptoms rather than clinical signs by a physician, such as tissue abnormalities or specific physical findings [13,66,68]. Frequent patient-reported symptoms of brain fog, mood disturbances, xerophthalmia, fever, paresthesia, and arthralgia, among others, after SBI surgery have led authors to coin the term “siliconosis” or “silicone reactive disorder” [24,63,68,69,70,71,72].
However, other authors posit these symptoms represent a subtype of an adjuvant-induced autoimmune syndrome, a broad term that includes BII and other implant-associated diseases [63,71], termed as silicone implant incompatibility syndrome (SIIS) [73,74].
SIIS is presumed to share pathophysiological features with fibromyalgia [75]. The nociceptive stimulus (silicone) combined with extensive worries about the safety of the SBI can lead to disturbances in pain signaling pathways, with excessive neurotransmitter stimulation resulting in systemic complaints [76]. Additionally, cytokines released during chronic inflammation may lead to persistent alterations in dopaminergic pathways and basal ganglia, leading to persistent anhedonia, fatigue, and psychomotor slowing [77].
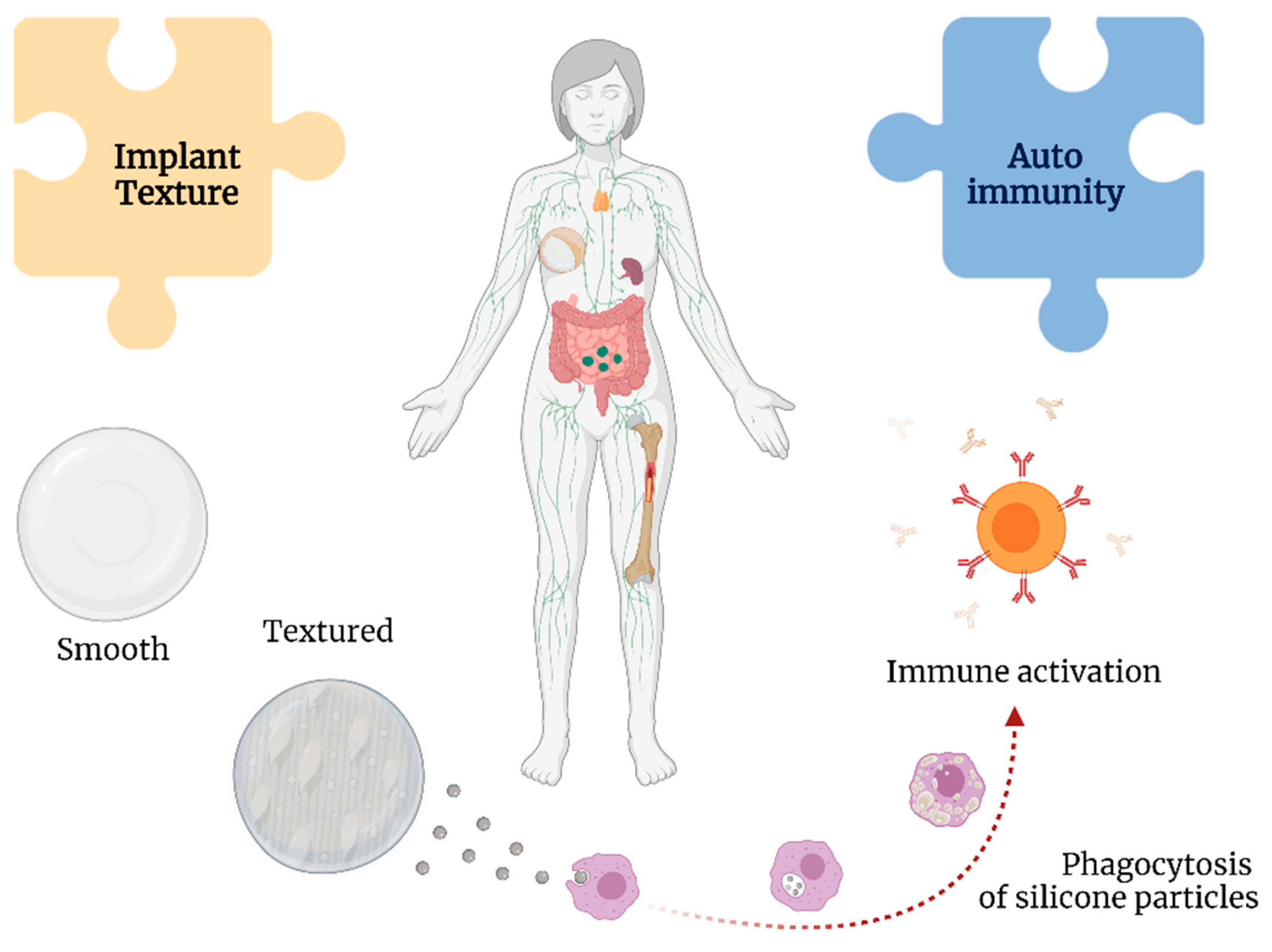
Silicone particles can be shed from the textured implants, leading to a chronic immunological stimulus in the body [41] (Figure 5). This theory is supported by the findings in the lymphoid tissue and thymus related to silicone-activated inflammasomes, cytokine production, and neutrophil and macrophage recruitment, even leading to granulomas [65,78].
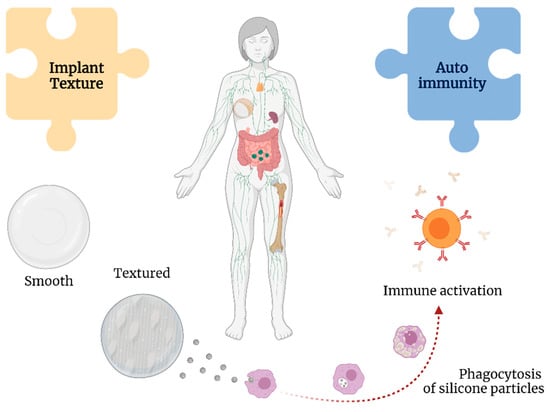
Figure 5.
Associations between implant texture and autoimmunity with breast implant illness.
Shedding from the implant may result in the formation of silicone-induced granuloma of the breast implant capsule. This condition is posited to represent autoimmune syndrome induced by adjuvants (ASIA), with the adjuvants in this instance being silicone [79]. This leads to the activation of macrophages and increased levels of interleukin-1β and reactive oxygen and nitrogen species [80].
Moreover, silicone particles can elicit a type 2 inflammatory response and increase levels of immunoglobulins G1 and E [81], resulting in the chronic activation of fibroblasts, myofibroblasts, and T lymphocytes contributing to increased collagen deposition and, ultimately, capsular contracture [82].
The surface charge of nanoparticles may play an important role in their cytotoxicity [83]. Silicone particles have been shown to decrease phagocytosis, induce the production of intracellular reactive oxygen species, and reduce mitochondrial metabolic activities [84]. Multiple studies have demonstrated the development of autoantibodies in response to silicone implants, such as anti-nuclear antibodies and rheumatoid factor, suggesting a persistent antigenic role of SBI [76,85].
These findings are highly suggestive of silicone lymphadenopathy, a condition that pathologically resembles and is often misdiagnosed as cancer or other immune-mediated pathologies [63,86,87,88,89]. Research has also suggested that ASIA involves an interplay between immunogenetic factors, such as human leukocyte agent, as well as environmental factors, such as smoking and obesity [90].
Interestingly, several patients with SBI have reported new-onset systemic sclerosis, Sjögren’s syndrome, connective tissue diseases, and other mucocutaneous syndromes [63,66,67,91]. Correspondingly, microscopic evidence of silicone detachment has been observed in distant tissues (e.g., liver), suggesting that these particles stimulate the immune system and produce autoantibodies, such as anti-DNA, anti-collagen II, and anti-SSB [92].
Furthermore, silicone adjuvants reportedly induce cytokine dysfunction and possibly fibrosis [69]. Specifically, cytokine dysfunction was observed in patients with symptoms that mimic Sjögren’s syndrome [70], predominantly mononuclear cell infiltrate, a key distinguishing factor from classical Sjögren’s syndrome [69].
However, even with the previously presented evidence and the possibility that silicone may not be an inert substance [64,93], the association between SBI and autoimmunity remains unclear [92].
3.2. Somatic Syndromes
A number of other functional somatic syndromes with an unclear etiology share common symptoms with BII, such as chronic fatigue syndrome and fibromyalgia [66,67]. A previous study demonstrated that the presence of these syndromes as well as a chronic disease and an advanced age were independent predictors for the development of BII-related symptoms [62].
As mentioned in Section 3.1, somatic symptoms may be due to a range of implant-related autoimmune conditions induced by adjuvants, including BII [63,71], with a wide range of associated symptoms reportedly linked to these conditions [67,68]. Many patients with adjuvant-induced autoimmune syndrome share two common psychological conditions: (1) the belief that they have a serious disease, which will only worsen and (2) a certain interest in adopting a “sick role” [66].
The role of SBI in the genesis or worsening of connective tissue disorders has been previously reported [70]. Specifically, a study including 220 women with SBI and 879 women without SBI reported a relative risk of 1.24 for any connective tissue diseases in women with SBI compared with the general population [94]. Moreover, the relative risk for explantation was 5.6-fold higher in patients meeting the major criteria for adjuvant-induced autoimmune syndrome and 4.3-fold higher for those meeting the minor criteria [95].
3.3. Explantation and Reported Symptoms of BII
Some authors have argued that explantation ameliorates the symptoms and complaints of BII, as some patients report improvements in systemic and local symptoms after implant removal [96,97,98]. Further, symptom relief is typically immediate after explantation and capsulectomy [57].
A previous study reported that symptom improvement is noted within the first 30 postoperative days after explantation, continues over subsequent months, and is greater in patients with a body mass index of >30 kg/m2 and a more advanced stage of capsular contracture [24,98]. However, a study by Wee et al. (2020) showed a significant loss of patients to follow-up, with only 5% of patients attending follow-up appointments beyond 6 months postoperatively [24]. Loss to follow-up after SBI represents a significant limitation for studies evaluating the long-term effects of silicone implants.
Rohrich et al. reported improved musculoskeletal symptoms, mental health, and body image after explantation [99]. Likewise, de Boer et al. demonstrated improvements in symptoms of fatigue, arthralgia, and myalgia as well as in memory and sleep disturbances in 76% of patients after explantation [98]. A recent study by Miseré and van der Hulst reported subjective improvements in complaints in 60% of patients [11]. Similar findings have been reported by other authors as well [68,100,101,102,103,104,105,106], suggesting that a decreased inflammatory response and elimination of the nociceptive stimulus explains the improvements in highly symptomatic patients after explantation [98,99].
Another study revealed that only patients with elevated serologic markers of autoimmune disorders experienced a short-lived improvement in symptoms after explantation; however, symptoms recurred within the first 6–12 months postoperatively, whereas patients with a previously diagnosed autoimmune disorder showed no improvement in symptoms [13,106]. These findings are supported by a recent systematic review [98].
The relationship between autoimmunity, connective tissue diseases, and SBI remains controversial [38,92,107], with many studies indicating ambivalent results regarding the role of SBI in autoimmunity [108,109], whereas others conclude that there is no objective supporting evidence [38,110].
4. Breast Reconstruction
Postmastectomy breast reconstruction, immediate or delayed, has been performed with increasing frequency over the past few decades and has become an appealing option for patients [111]. In 2019, 100,000 implant-based breast cancer reconstructions were performed in the United States alone [38].
Compared with aesthetic breast augmentation, patients with breast cancer report the eradication of cancer and long-term survival as a priority, with aesthetics less of a concern [112]. Nonetheless, breast reconstruction has become an increasingly important aspect of breast cancer therapy, as it can contribute to the restoration of body image and quality of life [113].
Postmastectomy reconstruction can involve a single- or double-staged approach [114]. The former relies on the placement of an SBI or autologous tissue immediately following mastectomy [115], whereas the latter initially places a tissue expander that is eventually replaced with an SBI [116].
Special consideration is given to patients undergoing radiotherapy [79]. Such patients may receive up to 25–28 sessions of radiotherapy, which may lead to the distortion of the breast shape, fat necrosis, fibrosis, implant loss, infection, and volume loss [117,118,119]. The effects of radiation on SBI include a reduction in maximum elongation strain, decreasing the flexibility of the SBI and predisposing it to microtears; this further increases the risk of ASIA and silicone-induced granuloma of the breast implant capsule (SIGBIC) [79,80].
Some authors have characterized SIGBIC as a radiological marker of BII [120]. SIGBIC appears as the “black drop” sign on magnetic resonance imaging and is yet another manifestation of the effects of silicone on the body [111]. Although patients with expanders who underwent radiation are less likely to experience capsular contracture, they are reportedly 2.33 times more likely to face reconstruction failure than those undergoing radiotherapy with SBI [119].
Further concerns regarding autoimmunity have arisen following a recent study wherein patients who underwent reconstructive surgery had more than twice the incidence rate of dermatomyositis, polymyositis, scleroderma, and Sjögren’s syndrome at a 7-year follow-up compared with the general population [91,121]. Moreover, patients with increased manipulation or those undergoing radiotherapy are more likely to experience gel bleeding and implant rupture [118]. These findings are of utmost concern for patients undergoing breast reconstruction.
5. Discussion
As stated in the previous sections, BII and SBI removal have recently attracted widespread attention [122], as reflected by an eight-fold increase in Google searches for SBI-related complications [123] and a 30.7% increase in breast implant explantation from 2006 to 2019 [124]. Despite the reported health and safety concerns regarding SBI, millions of women worldwide have undergone breast augmentation or reconstruction [125,126].
In response, a newer anatomic-shaped SBI has been developed to decrease capsular contracture. These new implants have a stable form and cohesive gel filling, commonly referred to as “gummy bear” implants [127]. Consequently, the incidence of capsular contracture has steadily decreased with the development of new implants, a trend that can be attributed to improved SBI design, enhanced surgical techniques, or a combination of both [53].
However, the degree of capsular contracture is reported to vary among patients, further supporting the hypothesis that capsular contracture and possibly BII are due to local rather than systemic effects [59]. This notion has paved the way for innovations such as micro and nanotextured implants that are designed to address the risk of both capsular contracture and BIA-ALCL [128,129]. Nevertheless, long-term studies are required to assess the association between risk of BIA-ALCL and nanotextured SBI, as BIA-ALCL typically appears 9 years after implant insertion [130].
Regarding SBI infections, the use of irrigation techniques is expected to decrease the number of cases of SBI-related infections and, more importantly, chronic cases. The association between autoimmunity and SBI remains unclear [92]. The chronic effects of implants have even been demonstrated in other species, with studies on Gryllus assimilis demonstrating that chronic implants have deleterious effects on survival, reproduction, and nutrition [131]. Furthermore, some studies that have supported favorable claims have been found to have design flaws, a high proportion of patients lost during follow-up, or included populations at increased risk of autoimmune disorders, such women aged 30–50 years [9,38].
However, other factors have been posited as more plausible explanations for the development or worsening of autoimmune disorders following SBI insertion, such as smoking, allergies, and a higher incidence of autoimmunity in young women [38,132]. Others have suggested that BII may be the combined expression of psychological and immunological factors, as well as a systemic response to the antigenicity of silicone since many patients that develop BII have comorbid syndromes such as fibromyalgia, irritable bowel syndrome, connective tissue diseases, and capsular contracture [112].
Explantation is not always an adequate solution, as not all patients undergoing explantation show positive outcomes [13]. Furthermore, attention has been drawn to the existence of a communication gap between patients and their physicians, probably because of the underreporting of BII-related symptoms or its dismissal because of insufficient physical evidence [133].
Postmastectomy patients undergoing breast reconstruction with or without radiotherapy are especially susceptible to capsular contracture and silicone gel bleeding [79,80]. Therefore, specialized intervention methods must be developed to prevent SIGBIC [80], autoimmune manifestations [121], and cancer recurrence [111], especially when breast cancer accounts for more than 10% of cases worldwide [134].
Therefore, physicians should create a safe and welcoming environment for patients to bridge the gap between physician and patient communication [10,127,135]. Moreover, they should validate all patient concerns and educate their patients regarding the implants, possible complications, and symptoms to be aware of.
6. Conclusions
The complexity of BII has been indicated by the lack of a universal definition, diagnostic criteria, defined high-risk populations, and standardized treatment guidelines because of the heterogeneity of implants and surgical approaches used. At present, appropriate recommendations should include the use of a pre-established follow-up schedule, the implementation of a standardized symptom report chart after SBI surgery, and the development of clear indications for explantation and other surgical interventions in patients with possible BII.
Author Contributions
Conceptualization, C.D.V.-C., G.S.-M., N.d.l.Á.S.-A. and P.A.T.-C.; investigation, C.D.V.-C. and G.S.-M.; writing—original draft preparation, C.D.V.-C., G.S.-M., N.d.l.Á.S.-A. and P.A.T.-C.; writing—review and editing, C.D.V.-C. and P.A.T.-C.; supervision, N.d.l.Á.S.-A. and P.A.T.-C.; project administration, P.A.T.-C.; funding acquisition, G.S.-M., C.D.V.-C. and P.A.T.-C. All authors have read and agreed to the published version of the manuscript.
Funding
Article processing charges for this article were self-sponsored by the authors. Tecnológico de Monterrey sponsored language revision service.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
All the authors personally thank Luis Andrés Arreguin Bribiesca, and Rodrigo Merino Arellano for their technical revision as plastic surgeons, as well as providing an image of capsular contracture. Likewise, they acknowledge biorender.com (accessed 5 May 2022) for its tool to create our figures, as well as to Laura Margarita López-Castillo by the financial support for the premium membership. Additionally, P.A.T.-C thanks CONACyT for his grant 627107 for doctoral studies. Likewise, he thanks Tecnológico de Monterrey for his full-tuition scholarship, and its support as part of the Teaching Assistant program.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Nahabedian, M.Y. Innovations and advancements with prosthetic breast reconstruction. Breast J. 2018, 24, 586–591. [Google Scholar] [CrossRef]
- Harvey, Z.T.; Potter, B.K.; Vandersea, J.; Wolf, E. Prosthetic advances. J. Surg. Orthop. Adv. 2012, 21, 58–64. [Google Scholar] [PubMed]
- Arabian, A.; Varotsis, D.; McDonnell, C.; Meeks, E. Global social acceptance of prosthetic devices. In Proceedings of the GHTC 2016—2016 IEEE Global Humanitarian Technology Conference (GHTC) Technology for the Benefit of Humanity Conference Proceedings, Seattle, WA, USA, 13–16 October 2016; Institute of Electrical and Electronics Engineers Inc.: New York, NY, USA, 2016; pp. 563–568. [Google Scholar] [CrossRef]
- Son, W.J.; Kang, S.G.; Seo, B.F.; Choi, N.-K. A Systematic Review of the National Breast Implant Registry for Application in Korea: Can We Predict “Unpredictable” Complications? Medicina 2020, 56, 370. [Google Scholar] [CrossRef]
- American Society of Plastic Surgeons. Plastic Surgery Statistics Report 2020—ASPS National Clearinghouse of Plastic Surgery Procedural Statistics; SPS: West Valley City, UT, USA, 2021; pp. 1–26. [Google Scholar]
- U. S. Food and Drug Administration. Risks and Complications of Breast Implants Breast Implants—Certain Labeling Recommendations to Improve; FDA; Silver Spring: Montgomery County, MD, USA, 2021; pp. 1–10. [Google Scholar]
- Vasey, F.B.; Zarabadi, S.A.; Seleznick, M.; Ricca, L. Where there’s smoke there’s fire: The silicone breast implant controversy continues to flicker: A new disease that needs to be defined. J. Rheumatol. 2003, 30, 2092–2094. [Google Scholar] [PubMed]
- Bouhadana, G.; Chocron, Y.; Azzi, A.J.; Davison, P.G. Perception of implants among breast reconstruction patients in montreal. Plast. Reconstr. Surg.—Glob. Open. 2020, 8, e3116. [Google Scholar] [CrossRef]
- Siling, Y.; Klietz, M.-L.; Harren, A.K.; Wei, Q.; Hirsch, T.; Aitzetmüller, M.M. Understanding Breast Implant Illness: Etiology is the Key. Aesthet. Surg. J. 2021, 42, 370–377. [Google Scholar] [CrossRef]
- Tang, S.Y.Q.; Israel, J.S.; Afifi, A.M. Breast Implant Illness: Symptoms, Patient Concerns, and the Power of Social Media. Plast. Reconstr. Surg. 2017, 140, 765e–766e. [Google Scholar] [CrossRef]
- Miseré, R.M.L.; van der Hulst, R.R.W.J. Self-Reported Health Complaints in Women Undergoing Explantation of Breast Implants. Aesthet. Surg. J. 2022, 42, 171–180. [Google Scholar] [CrossRef]
- U. S. Food and Drug Administration. FDA Executive Summary: Breast Implant Special Topics, Prepared for the Meeting of the General and Plastic Surgery Devices Advisory Panel; FDA; Silver Spring: Montgomery County, MD, USA, 2019; pp. 1–42. [Google Scholar]
- Magnusson, M.R.; Cooter, R.D.; Rakhorst, H.; McGuire, P.A.; Adams, W.P.; Deva, A.K. Breast Implant Illness: A Way Forward. Plast. Reconstr. Surg. 2019, 143, 74S–81S. [Google Scholar] [CrossRef]
- Rohrich, R.J.; Kaplan, J.; Dayan, E. Silicone Implant Illness: Science versus Myth? Plast. Reconstr. Surg. 2019, 144, 98–109. [Google Scholar] [CrossRef]
- Magnusson, M.R.; McGuire, P. Commentary on: Understanding Breast Implant Illness: Etiology is the Key. Aesthet. Surg. J. 2022, 42, 378–380. [Google Scholar] [CrossRef]
- Bachour, Y.; Bargon, C.A.; de Blok, C.J.M.; Ket, J.C.F.; Ritt, M.J.P.F.; Niessen, F.B. Risk factors for developing capsular contracture in women after breast implant surgery: A systematic review of the literature. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, e29–e48. [Google Scholar] [CrossRef]
- Jacobson, J.M.; Gatti, M.E.; Schaffner, A.D.; Hill, L.M.; Spear, S.L. Effect of incision choice on outcomes in primary breast augmentation. Aesthet. Surg. J. 2012, 32, 456–462. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Chen, L.; Liu, W.; Mu, D.; Luan, J. Capsular Contracture Rate After Breast Augmentation with Periareolar Versus Other Two (Inframammary and Transaxillary) Incisions: A Meta-Analysis. Aesthet. Plast. Surg. 2018, 42, 32–37. [Google Scholar] [CrossRef]
- Blount, A.L.; Martin, M.D.; Lineberry, K.D.; Kettaneh, N.; Alfonso, D.R. Capsular contracture rate in a low-risk population after primary augmentation mammaplasty. Aesthet. Surg. J. 2013, 33, 516–521. [Google Scholar] [CrossRef]
- Wiener, T.C. Relationship of incision choice to capsular contracture. Aesthet. Plast. Surg. 2008, 32, 303–306. [Google Scholar] [CrossRef]
- Galdiero, M.; Larocca, F.; Iovene, M.R.; Francesca, M.; Pieretti, G.; D’Oriano, V.; Franci, G.; Ferraro, G.; D’Andrea, F.; Nicoletti, G.F. Microbial Evaluation in Capsular Contracture of Breast Implants. Plast. Reconstr. Surg. 2018, 141, 23–30. [Google Scholar] [CrossRef]
- Prantl, L.; Angele, P.; Schreml, S.; Ulrich, D.; Pöppl, N.; Eisenmann-Klein, M. Determination of serum fibrosis indexes in patients with capsular contracture after augmentation with smooth silicone gel implants. Plast. Reconstr. Surg. 2006, 118, 224–229. [Google Scholar] [CrossRef]
- Sood, A.; Xue, E.Y.; Sangiovanni, C.; Therattil, P.J.; Lee, E.S. Breast Massage, Implant Displacement, and Prevention of Capsular Contracture After Breast Augmentation With Implants: A Review of the Literature. Eplasty 2017, 17, e41. [Google Scholar]
- Wee, C.E.; Younis, J.; Isbester, K.; Smith, A.; Wangler, B.; Sarode, A.L.; Patil, N.; Grunzweig, K.; Boas, S.; Harvey, D.J.; et al. Understanding Breast Implant Illness, Before and After Explantation: A Patient-Reported Outcomes Study. Ann. Plast. Surg. 2020, 85, S82–S86. [Google Scholar] [CrossRef]
- Calobrace, M.B.; Schwartz, M.R.; Zeidler, K.R.; Pittman, T.A.; Cohen, R.; Stevens, W.G. Long-term safety of textured and smooth breast implants. Aesthet. Surg. J. 2018, 38, 38–48. [Google Scholar] [CrossRef] [Green Version]
- Hammond, J.B.; Kosiorek, H.E.; Cronin, P.A.; Rebecca, A.M.; Casey, W.J.; Wong, W.W.; Vargas, C.E.; Vern-Gross, T.Z.; McGee, L.A.; Pockaj, B.A. Capsular contracture in the modern era: A multidisciplinary look at the incidence and risk factors after mastectomy and implant-based breast reconstruction. Am. J. Surg. 2021, 221, 1005–1010. [Google Scholar] [CrossRef]
- Stevens, W.G.; Nahabedian, M.Y.; Calobrace, M.B.; Harrington, J.L.; Capizzi, P.J.; Cohen, R.; D’incelli, R.C.; Beckstrand, M. Risk factor analysis for capsular contracture: A 5-year sientra study analysis using round, smooth, and textured implants for breast augmentation. Plast. Reconstr. Surg. 2013, 132, 1115–1123. [Google Scholar] [CrossRef]
- Jones, P.; Mempin, M.; Hu, H.; Chowdhury, D.; Foley, M.; Cooter, R.; Adams, W.P.; Vickery, K.; Deva, A.K. The functional influence of breast implant outer shell morphology on bacterial attachment and growth. Plast. Reconstr. Surg. 2018, 142, 837–849. [Google Scholar] [CrossRef]
- Munhoz, A.M.; Clemens, M.W.; Nahabedian, M.Y. Breast Implant Surfaces and Their Impact on Current Practices. Plast. Reconstr. Surg.—Glob. Open 2019, 7, e2466. [Google Scholar] [CrossRef] [Green Version]
- Luvsannyam, E.; Patel, D.; Hassan, Z.; Nukala, S.; Somagutta, M.R.; Hamid, P. Overview of Risk Factors and Prevention of Capsular Contracture Following Implant-Based Breast Reconstruction and Cosmetic Surgery: A Systematic Review. Cureus 2020, 12, e10341. [Google Scholar] [CrossRef] [PubMed]
- Mallucci, P.; Bistoni, G. The Use of Anatomic Implants in Aesthetic Breast Surgery. Clin. Plast. Surg. 2021, 48, 141–156. [Google Scholar] [CrossRef] [PubMed]
- Vinci, V.; Domenico, C.; Luca, M.; Silvia, G.; Alessandra, V.; Barbara, C.; Valeria, B.; Andrea, B.; Mattia, S.; Federico, B.; et al. The evolution of breast prostheses. Breast J. 2020, 26, 1801–1804. [Google Scholar] [CrossRef]
- Mowlds, D.S.; Salibian, A.A.; Scholz, T.; Paydar, K.Z.; Wirth, G.A. Capsular contracture in implant-based breast reconstruction: Examining the role of acellular dermal matrix fenestrations. Plast. Reconstr. Surg. 2015, 136, 629–635. [Google Scholar] [CrossRef]
- Ajdic, D.; Zoghbi, Y.; Gerth, D.; Panthaki, Z.J.; Thaller, S. The relationship of bacterial biofilms and capsular contracture in breast implants. Aesthet. Surg. J. 2016, 36, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Shauly, O.; Gould, D.J.; Patel, K.M. Microtexture and the cell/biomaterial interface: A systematic review and meta-analysis of capsular contracture and prosthetic breast implants. Aesthet. Surg. J. 2019, 39, 603–614. [Google Scholar] [CrossRef]
- Turner, S.D.; Inghirami, G.; Miranda, R.N.; Kadin, M.E. Cell of Origin and Immunologic Events in the Pathogenesis of Breast Implant–Associated Anaplastic Large-Cell Lymphoma. Am. J. Pathol. 2020, 190, 2–10. [Google Scholar] [CrossRef] [Green Version]
- Swanson, E. The Food and Drug Administration Bans Biocell Textured Breast Implants: Lessons for Plastic Surgeons. Ann. Plast. Surg. 2020, 84, 343–345. [Google Scholar] [CrossRef]
- McKernan, C.D.; Vorstenbosch, J.; Chu, J.J.; Nelson, J.A. Breast Implant Safety: An Overview of Current Regulations and Screening Guidelines. J. Gen. Intern. Med. 2022, 37, 212–216. [Google Scholar] [CrossRef]
- Johal, K.S.; Floyd, D. To bloc or not to bloc: Challenges in the management of patients requesting “En-Bloc capsulectomy”. Aesthet. Surg. J. 2020, 40, NP561–NP563. [Google Scholar] [CrossRef]
- Keane, G.; Chi, D.; Ha, A.Y.; Myckatyn, T.M. En Bloc Capsulectomy for Breast Implant Illness: A Social Media Phenomenon? Aesthet. Surg. J. 2021, 41, 448–459. [Google Scholar] [CrossRef]
- Swanson, E. Evaluating the necessity of capsulectomy in cases of textured breast implant replacement. Ann. Plast. Surg. 2020, 85, 691–698. [Google Scholar] [CrossRef]
- Abi-Rafeh, J.; Safran, T.; Winocour, S.; Dionisopoulos, T.; Davison, P.; Vorstenbosch, J. Lack of Evidence on Complication Profile of Breast Implant Capsulectomy: A Call to Action for Plastic Surgeons. Plast. Reconstr. Surg. 2021, 148, 157e–158e. [Google Scholar] [CrossRef]
- Venkatesan, N.; Perumal, G.; Doble, M. Bacterial resistance in biofilm-associated bacteria. Future Microbiol. 2015, 10, 1743–1750. [Google Scholar] [CrossRef]
- Nguyen, T.H.; Park, M.D.; Otto, M. Host response to Staphylococcus epidermidis colonization and infections. Front. Cell. Infect. Microbiol. 2017, 7, 90. [Google Scholar] [CrossRef] [Green Version]
- Beam, E.; Osmon, D. Prosthetic Joint Infection Update. Infect. Dis. Clin. N. Am. 2018, 32, 843–859. [Google Scholar] [CrossRef] [PubMed]
- Dowsett, C.; Bellingeri, A.; Carville, K.; Garten, A.; Woo, K. A route to more effective infection management: The Infection Management Pathway. Wounds Int. 2020, 11, 50–57. [Google Scholar]
- Rabin, N.; Zheng, Y.; Opoku-Temeng, C.; Du, Y.; Bonsu, E.; Sintim, H.O. Biofilm formation mechanisms and targets for developing antibiofilm agents. Future Med. Chem. 2015, 7, 493–512. [Google Scholar] [CrossRef] [PubMed]
- Veerachamy, S.; Yarlagadda, T.; Manivasagam, G.; Yarlagadda, P.K. Bacterial adherence and biofilm formation on medical implants: A review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2014, 228, 1083–1099. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Moure, J.S.; Mydlowska, A.; Shin, C.; Vella, M.; Kaplan, L.J. Nanometric Considerations in Biofilm Formation. Surg. Infect. 2019, 20, 167–173. [Google Scholar] [CrossRef]
- Achermann, Y.; Goldstein, E.J.C.; Coenye, T.; Shirtliffa, M.E. Propionibacterium acnes: From Commensal to opportunistic biofilm-associated implant pathogen. Clin. Microbiol. Rev. 2014, 27, 419–440. [Google Scholar] [CrossRef] [Green Version]
- James, G.A.; Boegli, L.; Hancock, J.; Bowersock, L.; Parker, A.; Kinney, B.M. Bacterial Adhesion and Biofilm Formation on Textured Breast Implant Shell Materials. Aesthet. Plast. Surg. 2019, 43, 490–497. [Google Scholar] [CrossRef] [Green Version]
- McCarthy, P.H.; Teitler, N.A.; Hon, H.H.; Miller, J.J. Breast Implant Illness and Cutibacterium acnes: A Case Report. Plast. Reconstr. Surg.—Glob. Open 2022, 10, E4146. [Google Scholar] [CrossRef]
- Mempin, M.; Hu, H.; Chowdhury, D.; Deva, A.; Vickery, K. The A, B and C’s of silicone breast implants: Anaplastic large cell lymphoma, biofilm and capsular contracture. Materials 2018, 11, 2393. [Google Scholar] [CrossRef] [Green Version]
- Giordano, S.; Peltoniemi, H.; Lilius, P.; Salmi, A. Povidone-iodine combined with antibiotic topical irrigation to reduce capsular contracture in cosmetic breast augmentation: A comparative study. Aesthet. Surg. J. 2013, 33, 675–680. [Google Scholar] [CrossRef] [Green Version]
- Carvajal, J.; Carvajal, M.; Hernández, G. Back to Basics: Could the Preoperative Skin Antiseptic Agent Help Prevent Biofilm-Related Capsular Contracture? Aesthet. Surg. J. 2019, 39, 848–859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yalanis, G.C.; Liu, E.W.; Cheng, H.T. Efficacy and safety of povidone-iodine irrigation in reducing the risk of capsular contracture in aesthetic breast augmentation: A systematic review and meta-analysis. Plast. Reconstr. Surg. 2015, 136, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Ponraja, G.; McLeod, K.; Chong, S. Breast Implant Illness: A Biofilm Hypothesis. Plast. Reconstr. Surg.—Glob. Open 2020, 8, e2755. [Google Scholar] [CrossRef] [PubMed]
- Loch-Wilkinson, A.; Beath, K.J.; Knight, R.J.W.; Wessels, W.L.F.; Magnusson, M.; Papadopoulos, T.; Connell, T.; Lofts, J.; Locke, M.; Hopper, I.; et al. Breast implant-associated anaplastic large cell lymphoma in Australia and New Zealand: High-surface-area textured implants are associated with increased risk. Plast. Reconstr. Surg. 2017, 140, 645–654. [Google Scholar] [CrossRef]
- Rieger, U.M.; Pierer, G.; Lüscher, N.J.; Trampuz, A. Sonication of removed breast implants for improved detection of subclinical infection. Aesthet. Plast. Surg. 2009, 33, 404–408. [Google Scholar] [CrossRef] [Green Version]
- Schäfer, P.; Fink, B.; Sandow, D.; Margull, A.; Berger, I.; Frommelt, L. Prolonged bacterial culture to identify late periprosthetic joint infection: A promising strategy. Clin. Infect. Dis. 2008, 47, 1403–1409. [Google Scholar] [CrossRef] [Green Version]
- Portillo, M.E.; Salvadó, M.; Alier, A.; Martínez, S.; Sorli, L.; Horcajada, J.P.; Puig, L. Advantages of sonication fluid culture for the diagnosis of prosthetic joint infection. J. Infect. 2014, 69, 35–41. [Google Scholar] [CrossRef]
- Miseré, R.; Maartje, C.; van der Hulst, R.R.W.J. The Prevalence of Self-Reported Health Complaints and Health-Related Quality of Life in Women With Breast Implants. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2021, 41, 661–668. [Google Scholar] [CrossRef]
- Shoenfeld, Y.; Agmon-Levin, N. “ASIA”—Autoimmune/inflammatory syndrome induced by adjuvants. J. Autoimmun. 2011, 36, 4–8. [Google Scholar] [CrossRef]
- Watad, A.; Rosenberg, V.; Tiosano, S.; Tervaert, J.W.C.; Yavne, Y.; Shoenfeld, Y.; Shalev, V.; Chodick, G.; Amital, H. Silicone breast implants and the risk of autoimmune/rheumatic disorders: A real-world analysis. Int. J. Epidemiol. 2018, 47, 1846–1854. [Google Scholar] [CrossRef]
- Moraitis, S.D.; Agrafiotis, A.C.; Kapranou, A.; Kanakakis, K. Mediastinal silicone lymphadenopathy revealed after thymectomy for autoimmune myasthenia gravis. Monaldi Arch. Chest Dis. 2018, 88, 83–86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barsky, A.J.; Borus, J.F. Functional somatic syndromes. Ann. Intern. Med. 1999, 130, 910–921. [Google Scholar] [CrossRef] [PubMed]
- Vera-Lastra, O.; Medina, G.; Cruz-Dominguez, M.D.P.; Jara, L.J.; Shoenfeld, Y. Autoimmune/inflammatory syndrome induced by adjuvants (Shoenfeld’s syndrome): Clinical and immunological spectrum. Expert Rev. Clin. Immunol. 2013, 9, 361–373. [Google Scholar] [CrossRef]
- Maijers, M.C.; de Blok, C.J.M.; Niessen, F.B.; van der Veldt, A.A.M.; Ritt, M.J.P.F.; Winters, H.A.H.; Kramer, M.H.H.; Nanayakkara, P.W.B. Women with silicone breast implants and unexplained systemic symptoms: A descriptive cohort study. Neth. J. Med. 2014, 71, 534–540. [Google Scholar]
- Gadarowski, M.B.; Pukhalskaya, T.; Farah, R.; Smoller, B.R. Acquired anhidrosis in a patient with Sjogren syndrome and silicone breast implants. JAAD Case Rep. 2020, 6, 414–416. [Google Scholar] [CrossRef] [PubMed]
- Akyol, L.; Onem, S.; Ozgen, M.; Sayarlioglu, M. Sjögren’s syndrome after silicone breast implantation. Eur. J. Rheumatol. 2015, 2, 165–166. [Google Scholar] [CrossRef]
- Jara, L.J.; Medina, G.; Gómez-Bañuelos, E.; Saavedra, M.A.; Vera-Lastra, O. Still’s disease, lupus-like syndrome, and silicone breast implants. A case of “ASIA” (Shoenfeld’s syndrome). Lupus 2012, 21, 140–145. [Google Scholar] [CrossRef]
- Lappe, M.A. Silicone-reactive disorder: A new autoimmune disease caused by immunostimulation and superantigens. Med. Hypotheses 1993, 41, 348–352. [Google Scholar] [CrossRef]
- Tervaert, J.W.C.; Kappel, R.M. Silicone implant incompatibility syndrome (SIIS): A frequent cause of ASIA (Shoenfeld’s syndrome). Immunol. Res. 2013, 56, 293–298. [Google Scholar] [CrossRef]
- Fuzzard, S.K.; Teixeira, R.; Zinn, R. A Review of the Literature on the Management of Silicone Implant Incompatibility Syndrome. Aesthet. Plast. Surg. 2019, 43, 1145–1149. [Google Scholar] [CrossRef]
- Khoo, T.; Proudman, S.; Limaye, V. Silicone breast implants and depression, fibromyalgia and chronic fatigue syndrome in a rheumatology clinic population. Clin. Rheumatol. 2019, 38, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- Colaris, M.J.L.; de Boer, M.; van der Hulst, R.R.; Tervaert, J.W.C. Two hundreds cases of ASIA syndrome following silicone implants: A comparative study of 30 years and a review of current literature. Immunol. Res. 2017, 65, 120–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Felger, J.C.; Miller, A.H. Cytokine effects on the basal ganglia and dopamine function: The subcortical source of inflammatory malaise. Front. Neuroendocrinol. 2012, 33, 315–327. [Google Scholar] [CrossRef] [Green Version]
- Tervaert, J.W.C.; Colaris, M.J.; van der Hulst, R.R. Silicone breast implants and autoimmune rheumatic diseases: Myth or reality. Curr. Opin. Rheumatol. 2017, 29, 348–354. [Google Scholar] [CrossRef] [PubMed]
- de Faria Castro Fleury, E.; Rêgo, M.M.; Ramalho, L.C.; Ayres, V.J.; Seleti, R.O.; Ferreira, C.A.P.; Roveda, D., Jr. Silicone-induced granuloma of breast implant capsule (SIGBIC): Similarities and differences with anaplastic large cell lymphoma (ALCL) and their differential diagnosis. Breast Cancer Targets Ther. 2017, 9, 133–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Faria Castro Fleury, E.; D’Alessandro, G.S.; Wludarski, S.C.L. Silicone-induced granuloma of breast implant capsule (SIGBIC): Histopathology and radiological correlation. J. Immunol. Res. 2018, 2018, 6784971. [Google Scholar] [CrossRef] [Green Version]
- Caravantes-Cortes, M.I.; Roldan-Valadez, E.; Zwojewski-Martinez, R.D.; Salazar-Ruiz, S.Y.; Carballo-Zarate, A.A. Breast Prosthesis Syndrome: Pathophysiology and Management Algorithm. Aesthet. Plast. Surg. 2020, 44, 1423–1437. [Google Scholar] [CrossRef]
- Fleury, E.d.C.; Gianini, A.C.; Ayres, V.; Ramalho, L.C.; Seleti, R.O.; Roveda, D. Breast magnetic resonance imaging: Tips for the diagnosis of silicone-induced granuloma of a breast implant capsule (SIGBIC). Insights Imaging 2017, 8, 439–446. [Google Scholar] [CrossRef]
- Favi, P.M.; Valencia, M.M.; Elliott, P.R.; Restrepo, A.; Gao, M.; Huang, H.; Pavon, J.J.; Webster, T.J. Shape and surface chemistry effects on the cytotoxicity and cellular uptake of metallic nanorods and nanospheres. J. Biomed. Mater. Res.—Part A 2015, 103, 3940–3955. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; de Haan, L.H.J.; Evers, N.M.; Jiang, X.; Marcelis, A.T.M.; Zuilhof, H.; Rietjens, I.M.C.M.; Alink, G.M. Role of surface charge and oxidative stress in cytotoxicity of organic monolayer-coated silicon nanoparticles towards macrophage NR8383 cells. Part. Fibre Toxicol. 2010, 7, 25. [Google Scholar] [CrossRef] [Green Version]
- Tervaert, J.W.C.; Mohazab, N.; Redmond, D.; van Eeden, C.; Osman, M. Breast implant illness: Scientific evidence of its existence. Expert Rev. Clin. Immunol. 2022, 18, 15–29. [Google Scholar] [CrossRef] [PubMed]
- Katzin, W.E.; Centeno, J.A.; Feng, L.J.; Kiley, M.; Mullick, F.G. Pathology of lymph nodes from patients with breast implants: A histologic and spectroscopic evaluation. Am. J. Surg. Pathol. 2005, 29, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Ganau, S.; Tortajada, L.; Rodríguez, X.; González, G.; Sentís, M. Silicone lymphadenopathy: An unusual cause of internal mammary lymph node enlargement. Breast J. 2008, 14, 502–503. [Google Scholar] [CrossRef] [PubMed]
- Soudack, M.; Yelin, A.; Simansky, D.; Ben-Nun, A. Fluorodeoxyglucose-positive internal mammary lymph node in breast cancer patients with silicone implants: Is it always metastatic cancer? Eur. J. Cardio-Thoracic Surg. 2013, 44, 79–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grubstein, A.; Cohen, M.; Steinmetz, A.; Cohen, D. Siliconomas mimicking cancer. Clin. Imaging 2011, 35, 228–231. [Google Scholar] [CrossRef]
- Cohen Tervaert, J.W. Autoinflammatory/autoimmunity syndrome induced by adjuvants (ASIA; Shoenfeld’s syndrome): A new flame. Autoimmun. Rev. 2018, 17, 1259–1264. [Google Scholar] [CrossRef]
- Coroneos, C.J.; Selber, J.C.; Offodile, A.C.; Butler, C.E.; Clemens, M.W. US FDA Breast Implant Postapproval Studies: Long-term Outcomes in 99,993 Patients. Ann. Surg. 2019, 269, 30–36. [Google Scholar] [CrossRef]
- Hortolam, J.G.; de Carvalho, J.F.; Appenzeller, S. Connective tissue diseases following silicone breast implantation: Where do we stand? Clinics 2013, 68, 281. [Google Scholar] [CrossRef]
- Dijkman, H.B.P.M.; Slaats, I.; Bult, P. Assessment of Silicone Particle Migration among Women Undergoing Removal or Revision of Silicone Breast Implants in the Netherlands. JAMA Netw. Open 2021, 4, e2125381. [Google Scholar] [CrossRef]
- Karlson, E.W.; Lee, I.M.; Cook, N.R.; Manson, J.A.E.; Buring, J.E.; Hennekens, C.H. Comparison of self-reported diagnosis of connective tissue disease with medical records in female health professionals. The women’s health cohort study. Am. J. Epidemiol. 1999, 150, 652–660. [Google Scholar] [CrossRef] [Green Version]
- Valente, D.S.; Zanella, R.K.; Mulazzani, C.M.; Valente, S.S. Risk Factors for Explantation of Breast Implants: A Cross-Sectional Study. Aesthet. Surg. J. 2021, 41, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Virevialle, C.; Labbé, A.; Dupont-Monod, S.; Parent, F.; Baudouin, C. Can breast implants be responsible for dry eye? Eye 2014, 28, 633–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teuber, S.S.; Howell, L.P.; Yoshida, S.H.; Gershwin, M.E. Remission of sarcoidosis following removal of silicone gel breast implants. Int. Arch. Allergy Immunol. 1994, 105, 404–407. [Google Scholar] [CrossRef] [PubMed]
- de Boer, M.; Colaris, M.; van der Hulst, R.R.W.J.; Tervaert, J.W.C. Is explantation of silicone breast implants useful in patients with complaints? Immunol. Res. 2017, 65, 25–36. [Google Scholar] [CrossRef] [Green Version]
- Rohrich, R.J.; Kenkel, J.M.; Adams, W.P.; Beran, S.; Conner, W.C.H. A prospective analysis of patients undergoing silicone breast implant explantation. Plast. Reconstr. Surg. 2000, 105, 2529–2537. [Google Scholar] [CrossRef]
- Vasey, F.B.; Havice, D.L.; Bocanegra, T.S.; Seleznick, M.J.; Bridgeford, P.H.; Martinez-Osuna, P.; Espinoza, L.R. Clinical findings in symptomatic women with silicone breast implants. Semin. Arthritis Rheum. 1994, 24, 22–28. [Google Scholar] [CrossRef]
- Aziz, N.; Vasey, F.; Leaverton, P. Comparison of clinical status among women retaining or removing gel breast implants. Am. J. Epidemiol. 1997, 145, 191. [Google Scholar]
- Thomas, W., 3rd; Harper, L.; Wong, S.; Michalski, J.; Harris, C.; Moore, J.; Rodning, C. Explantation of silicone breast implants. Am. Surg. 1997, 63, 421–429. [Google Scholar]
- Kappel, R.M.; Pruijn, G.J.M. The monobloc hydrogel breast implant, experiences and ideas. Eur. J. Plast. Surg. 2012, 35, 229–233. [Google Scholar] [CrossRef] [Green Version]
- Svahn, J.; Vastine, V.; Landon, B.; Dobke, M. Outcome of mammary prostheses explantation: A patient perspective. Ann. Plast. Surg. 1996, 36, 594–600. [Google Scholar] [CrossRef]
- Godfrey, P.; Godfrey, N. Response of locoregional and systemic symptoms to breast implant replacement with autologous tissues: Experience in 37 consecutive patients. Plast. Reconstr. Surg. 1996, 97, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Peters, W.; Smith, D.; Fornasier, V.; Lugowski, S.; Ibanez, D. An outcome analysis of 100 women after explantation of silicone gel breast implants. Ann. Plast. Surg. 1997, 39, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Picha, G.J.; Hardas, B.; Schumacher, A.; Murphy, D.K. Five-year safety data for more than 55,000 subjects following breast implantation: Comparison of rare adverse event rates with silicone implants versus national norms and saline implants. Plast. Reconstr. Surg. 2017, 140, 666–679. [Google Scholar] [CrossRef] [PubMed]
- Santiago, E.A.; de Paula, I.B. Autoimmune/Inflammatory Syndrome Induced by Adjuvants (Asia Syndrome) Associated with Silicone Breast Implant Rupture. Arch. Breast Cancer 2021, 8, 156–161. [Google Scholar] [CrossRef]
- Jara, L.J.; García-Collinot, G.; Medina, G.; Cruz-Dominguez, M.d.; Vera-Lastra, O.; Carranza-Muleiro, R.A.; Saavedra, M.A. Severe manifestations of autoimmune syndrome induced by adjuvants (Shoenfeld’s syndrome). Immunol. Res. 2017, 65, 8–16. [Google Scholar] [CrossRef]
- Barbosa, M.R.; Makris, U.E.; Mansi, I.A. Association of Breast Implants with Nonspecific Symptoms, Connective Tissue Diseases, and Allergic Reactions: A Retrospective Cohort Analysis. Plast. Reconstr. Surg. 2021, 147, 42E–49E. [Google Scholar] [CrossRef]
- Fleury, E.d.C.; Bernal, K.J.H.; Madeiro, A.L.M.; Ocana, W.L.C.; Fleury, J.C.V.; Caobianco, L. Side effects in breast implants related to radiotherapy in breast cancer reconstructive surgery. Tech. Innov. Patient Support Radiat. Oncol. 2021, 18, 8–11. [Google Scholar] [CrossRef]
- Roy, P.G.; Yan, Z.; Nigam, S.; Maheshwari, K. Aesthetic breast surgery: Putting in context—a narrative review. Gland Surg. 2021, 10, 2832–2846. [Google Scholar] [CrossRef]
- Miseré, R.M.; van Kuijk, S.M.; Claassens, E.L.; Heuts, E.M.; Piatkowski, A.A.; van der Hulst, R.R. Breast-related and body-related quality of life following autologous breast reconstruction is superior to implant-based breast reconstruction—A long-term follow-up study. Breast 2021, 59, 176–182. [Google Scholar] [CrossRef]
- Susarla, S.M.; Ganske, I.; Helliwell, L.; Morris, D.; Eriksson, E.; Chun, Y.S. Comparison of clinical outcomes and patient satisfaction in immediate single-stage versus two-stage implant-based breast reconstruction. Plast. Reconstr. Surg. 2015, 135, 1e–8e. [Google Scholar] [CrossRef]
- Rodriguez-Feliz, J.; Codner, M.A. Embrace the change: Incorporating single-stage implant breast reconstruction into your practice. Plast. Reconstr. Surg. 2015, 136, 221–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, G.K.; Sheckter, C.C. Breast Reconstruction Following Breast Cancer Treatment—2018. JAMA 2018, 320, 1277. [Google Scholar] [CrossRef] [PubMed]
- Ho, A.L.; Bovill, E.S.; Macadam, S.A.; Tyldesley, S.; Giang, J.; Lennox, P.A. Postmastectomy Radiation Therapy after Immediate Two-Stage Tissue Expander/Implant Breast Reconstruction. Plast. Reconstr. Surg. 2014, 134, 1e–10e. [Google Scholar] [CrossRef] [PubMed]
- Magill, L.J.; Ricketts, K.; Keshtgar, M.; Mosahebi, A.; Jell, G. Impact of post mastectomy radiotherapy on the silicone breast implant. Mater. Sci. Eng. C 2019, 98, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Ricci, J.A.; Epstein, S.; Momoh, A.O.; Lin, S.J.; Singhal, D.; Lee, B.T. A meta-analysis of implant-based breast reconstruction and timing of adjuvant radiation therapy. J. Surg. Res. 2017, 218, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Fleury, E.D.F.C. Silicone Induced Granuloma of Breast Implant Capsule (SIGBIC) diagnosis: Breast Magnetic Resonance (BMR) sensitivity to detect silicone bleeding. PLoS ONE 2020, 15, e0235050. [Google Scholar] [CrossRef]
- Kaplan, J.; Rohrich, R. Breast implant illness: A topic in review. Gland Surg. 2021, 10, 430–443. [Google Scholar] [CrossRef]
- Fleury, E.; Nimir, C.; D’alessandro, G.S. The breast tumor microenvironment: Could silicone breast implant elicit breast carcinoma? Breast Cancer Targets Ther. 2021, 13, 45–58. [Google Scholar] [CrossRef]
- Adidharma, W.; Latack, K.R.; Colohan, S.M.; Morrison, S.D.; Cederna, P.S. Breast Implant Illness: Are Social Media and the Internet Worrying Patients Sick? Plast. Reconstr. Surg. 2020, 145, 225e–227e. [Google Scholar] [CrossRef]
- Tian, W.M.; Rames, J.D.; Blau, J.A.; Taskindoust, M.; Hollenbeck, S.T. Contextualizing Breast Implant Removal Patterns with Google Trends: Big Data Applications in Surgical Demand. Plast. Reconstr. Surg.—Glob. Open 2022, 10, e4005. [Google Scholar] [CrossRef]
- Cole, N.M. Consequences of the U.S. Food and Drug Administration-Directed Moratorium on Silicone Gel Breast Implants: 1992 to 2006. Plast. Reconstr. Surg. 2018, 141, 1137–1141. [Google Scholar] [CrossRef] [PubMed]
- Kricheldorff, J.; Fallenberg, E.M.; Solbach, C.; Gerber-Schäfer, C.; Rancsó, C.; von Fritschen, U. Breast Implant-Associated Lymphoma The Diagnosis and Treatment of a New Disease Entity. Dtsch. Arztebl. Int. 2018, 115, 625–635. [Google Scholar] [CrossRef]
- Kaderbhai, A.; Broomfield, A.; Cuss, A.; Shaw, K.; Deva, A.K. Breast implants: A guide for general practice. Aust. J. Gen. Pract. 2021, 50, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Montemurro, P.; Tay, V. Transitioning from Conventional Textured to Nanotextured Breast Implants: Our Early Experience and Modifications for Optimal Breast Augmentation Outcomes. Aesthet. Surg. J. 2021, 41, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Asaad, M.; Offodile, A.C.; di Pompeo, F.S.; Bevers, T.B.; Stelly, S.; Carew, L.A.; Barnea, Y.; Miranda, R.N.; Butler, C.E.; Clemens, M.W. Management of Symptomatic Patients with Textured Implants. Plast. Reconstr. Surg. 2021, 147, 58S–68S. [Google Scholar] [CrossRef] [PubMed]
- Groth, A.K.; Graf, R. Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) and the Textured Breast Implant Crisis. Aesthet. Plast. Surg. 2020, 44, 1–12. [Google Scholar] [CrossRef]
- Limberger, G.M.; Esteves, K.P.; Halal, L.M.; Nery, L.E.M.; da Fonseca, D.B. Chronic immune challenge is detrimental to female survival, feeding behavior, and reproduction in the field cricket Gryllus assimilis (Fabricius, 1775). J. Comp. Physiol. B 2022, 2022, 1–12. [Google Scholar] [CrossRef]
- Atiyeh, B.; Enisieh, S. Breast Implant Illness (BII): Real Syndrome or a Social MediaPhenomenon? A Narrative Review of the Literature. Aesthet. Plast. Surg. 2021, 46, 43–57. [Google Scholar] [CrossRef]
- Mcguire, P.A.; Haws, M.J.; Nahai, F. Breast Implant Illness: How Can We Help? Aesthet. Surg. J. 2019, 39, 1260–1263. [Google Scholar] [CrossRef]
- Trinidad-Calderón, P.A.; López-Castillo, L.M.; Gallegos-Martínez, S.; Trujillo-de Santiago, G.; García-Lara, S.; Álvarez, M.M. nurP28, a New-to-Nature Zein-Derived Peptide, Enhances the Therapeutic Effect of Docetaxel in Breast Cancer Monolayers and Spheroids. Molecules 2022, 27, 2824. [Google Scholar] [CrossRef]
- Logothetis, M.L. Women’s Reports of Breast Implant Problems and Silicone-Related Illness. J. Obstet. Gynecol. Neonatal Nurs. 1995, 24, 609–616. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).