1. Introduction
The paranasal sinuses (maxillary, frontal, ethmoidal, sphenoidal) begin their development during intrauterine life, but only the maxillary and the ethmoidal sinuses are appreciable at birth.
At birth the maxillary sinus dimensions are: 4 mm in height, 2.7 mm in width and the anteroposterior diameter has a mean of 7 mm. Its pneumatization is very quick between 1 and 8 years of age. At the end of its growth, it reaches the nasal floor following the exfoliation and exchange time of the primary dentition [
1].
The maxillary sinus is covered internally by the Schneider membrane. Unlike the nasal epithelium, it does not present the basal lamina but it only consists of pseudostratified epithelium with cilia cells and mucus-producing goblet cells [
2].
With their synchronous and metachronous movement, cilia push mucus from the floor to the ostium of the sinus [
3].
The ostiomeatal complex is the key to sinus pathologies. It represents the first site of the deposition of foreign bodies from inhaled air. The normal functionality of the paranasal sinuses is determined mainly by three factors: the ostiomeatal patency; the maintenance of the ciliary apparatus; and the quality of nasal secretions. The interruption of this balance necessarily leads to sinus pathology [
4].
In the literature, odontogenic sinusitis is underestimated. Previous studies suggest the incidence rate of odontogenic sinusitis being 10–15% (5), but some recent studies have shown an increase, between 25% and 45% [
5].
Dental root inflammation and infection can reach maxillary alveolar bone and sinusal mucosa, causing this pathological condition.
Pulpal necrosis, periapical lesions (cysts, abscesses, granulomas), periodontitis, foreign bodies from dental endodontic treatments, dental extractions, maxillary osteotomies, placement of implants, bone grafts and orosinusal communications can be the cause of sinusitis defined as odontogenic [
5].
A combined intraoral and endoscopic approach has been proposed to solve this pathology, but there is no univocal view on the timing of these treatments or on their real indications. Nowadays, there is no gold standard of treatment and universal diagnostic method for odontogenic sinusitis without a rhinogenic component [
6].
In our opinion, the real indication for the use of the combined approach is the presence of anatomical predisposition to sinusitis. But in the absence of this predisposition, we have observed, based on the data emerging from this study, that the resolution of the odontogenic pathology allows the resolution of the sinus pathology also.
Usually, the combination of the two approaches solved the nasal component and the odontogenic component of sinusitis: the aim of this study is to verify whether, in the absence of a rhinogenic component, it is necessary to combine transnasal and oral intervention or if oral procedure only is sufficient to solve the pathology.
Aim of the Study
To evaluate if, in the absence of an anatomical predisposition, the exclusive intraoral approach to solving odontogenic sinusitis is equally successful to a combined intraoral and nasal endoscopic approach.
2. Materials and Methods
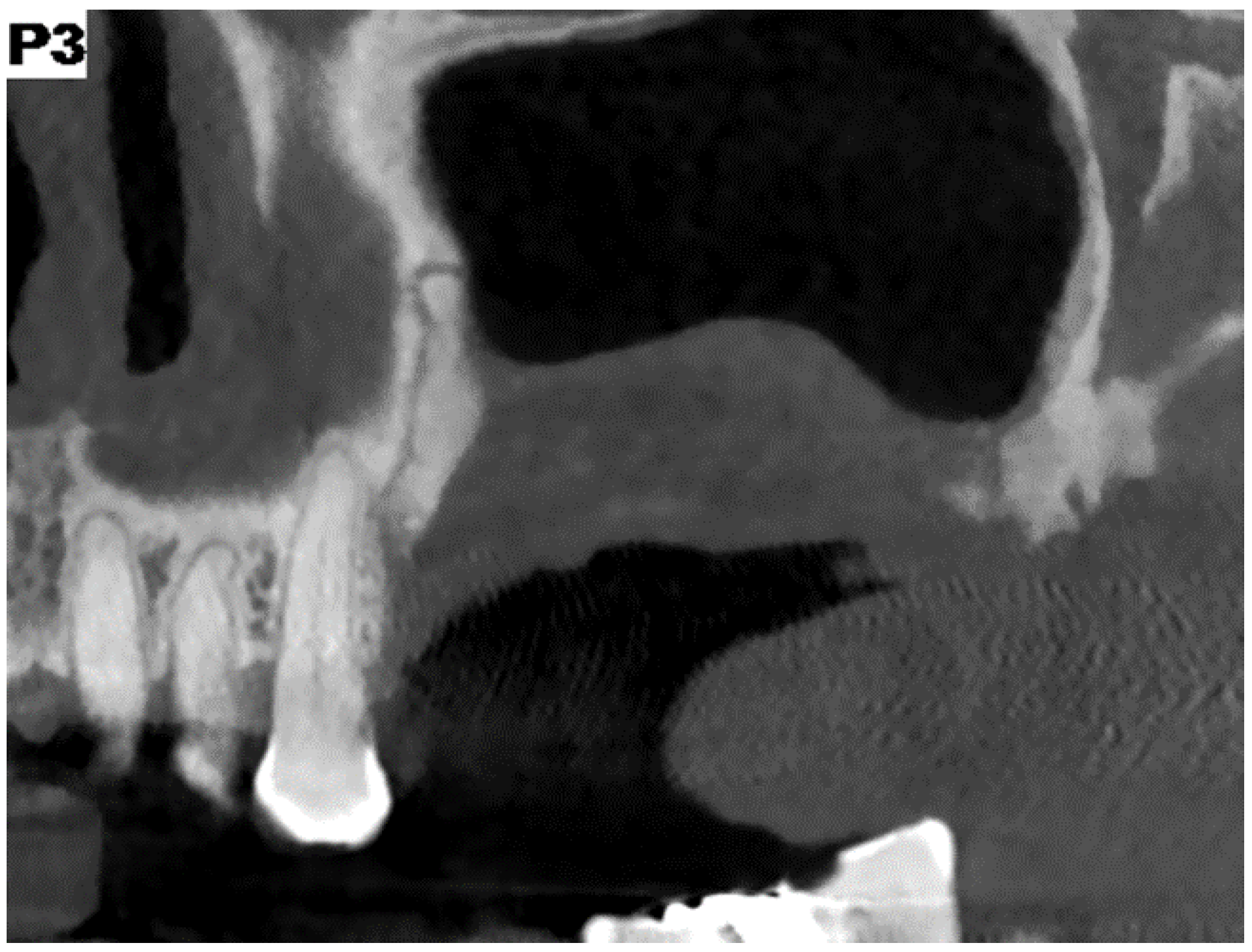
All patients undergoing odontostomatological examination from January 2018 to September 2019, were enrolled in this retrospective study. According to CT radiographic survey and clinical history, these patients had to show signs and symptoms of odontogenic sinusitis with obliteration (appreciable radiopacity) of a unilateral maxillary sinus and were not responsive to a previous systemic antibiotic therapy.
The inclusion criteria was: unilateral chronic odontogenic sinusitis with maxillary sinus obliteration that was not responsive to systemic antibiotic therapy.
The exclusion criteria were as follows: rhinosinusitis; presence of anatomical abnormalities (such as concha bullosa, turbinate with paradoxical curvature, important septal deviations); maxillary sinusitis without odontogenic cause; or resolution of sinus pathology with systemic antibiotic therapy.
In the beginning, patients underwent a clinical odontostomatological evaluation to localize any orosinusal communication and any radiographically identifiable pathologies from CT and orthopantomography (OPT). A Williams periodontal probe was usually used to diagnose a fistulous communication, if necessary.
Cacosmia, nocturnal roncopathy and possible apnea, nasal obstruction, and nasal congestion, hyposmia or anosmia, headaches, facial pain, mucopurulent nasal or oral secretions, otalgia, hypovisus and epiphora were the symptoms recorded.
The surgical approaches were: a combined surgical approach in general anesthesia FESS and simultaneous closure of oroantral communication with advancement of the Bichat’s fat pad (case group); or an exclusive oral surgical approach in local anesthesia and conscious sedation for a toilet of the maxillary sinus and closure of oroantral communication with advancement of Bichat’s fat pad (controls group).
An Excel table was created to collect patients’ data in compliance with privacy policy. To preserve personal data, the patients were identified with a code and the data were recorded and processed only as just mentioned.
For both groups, clinical control was performed 10, 15 and 30 days after therapeutic intervention.
The variable “success of the surgical procedure” in the two groups was compared by a Student test (with p < 0.05).
For the case group, local anesthesia was obtained with maxillary nerve block [
7] and vestibular paraperiosteal anesthesia of the middle and/or posterior superior alveolar nerve with mepivacaine and adrenaline 1:100,000. This choice was made in order to have a better visibility of the operative field and to induce analgesia that was not obtained with the dissociative activity given by general anesthesia alone. Local anesthesia has two main benefits: it reduces the need of analgesic requests in the post-operative period and it guarantees greater safety in maintaining vital parameters during general anesthesia [
8].
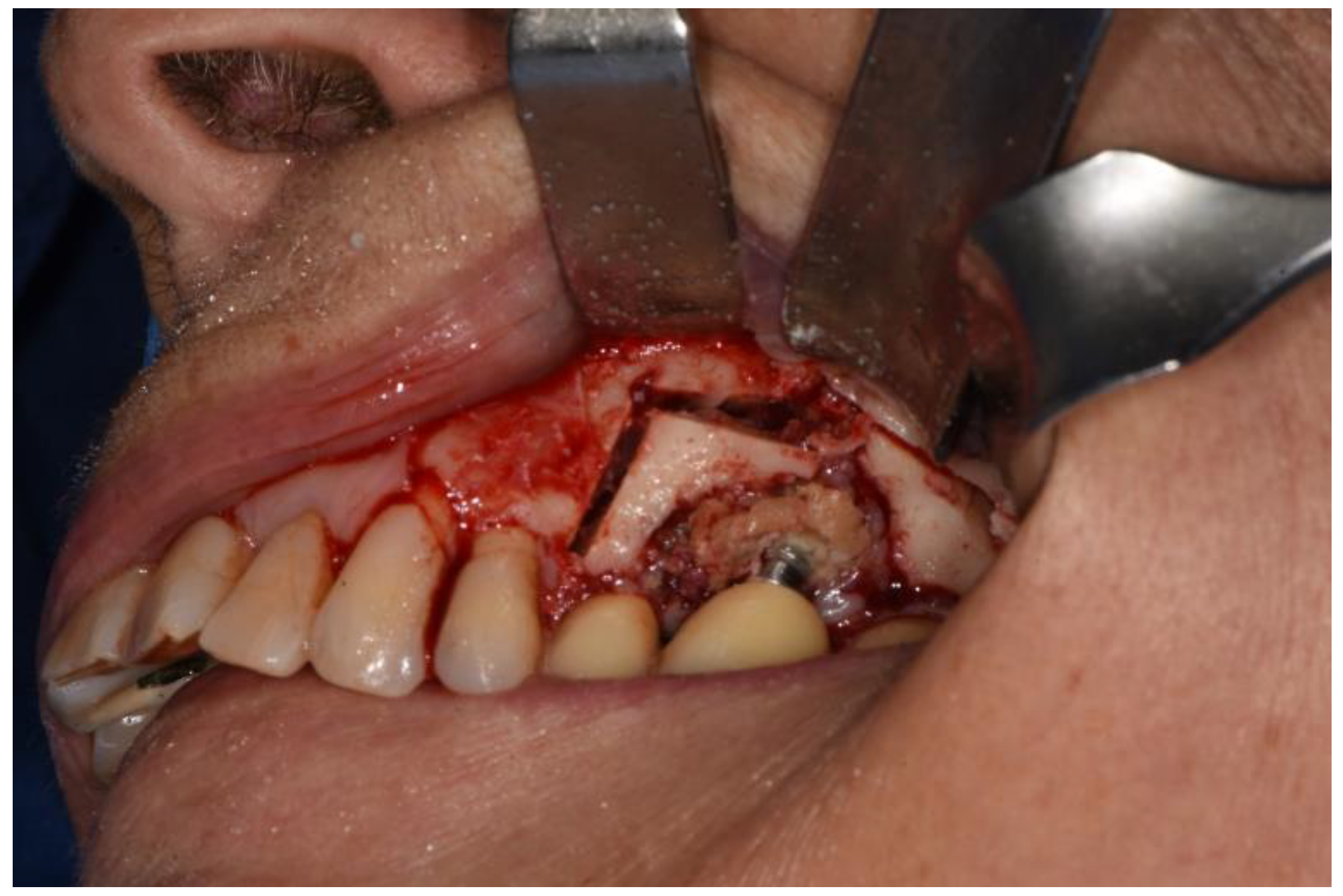
Therefore, a full-thickness vestibular flap was set up with medial and distal release incisions to oroantral communication (already present or induced as a result of extraction of dental element, bone implant or excision of lesion due to sinus pathology) and bone defects known. Ostectomy and osteoplasty were performed, if necessary.
After a horizontal periosteum incision, the Bichat’s fat pad was isolated and then advanced.
Below follows the description of the endoscopic procedures FESS performed by ENT.
Under endoscopic control, the nasal mucosa was decongested through the use of cotton swabs with a solution of mepivacaine and adrenaline with a ratio of 1:200,000, and then the mucous membrane was infiltrated with the same solution.
Under the control of a rigid endoscope at 0°, a partial inferior uncinectomy and a medium meatal antrostomy were performed, preserving ventilation and physiological drainage of the maxillary sinus involved.
The maxillary sinus was irrigated with a saline solution to eliminate the secretions. Thanks to the visibility allowed by washing, the mucous membrane was checked using a rigid endoscope at 70°.
In the case of inflammation and/or other pathological conditions (neoformations, foreign bodies), a biopsy was performed.
Usually, the day after, patients were dismissed and antibiotic therapy was routinely given. Topical application three times a day for 10 days of chlorhexidine 1% in an intraoral gel with antiseptic function was recommended.
At last, the patients underwent clinical and endoscopic follow-up at 10 and/or 15 days and finally at 30 days.
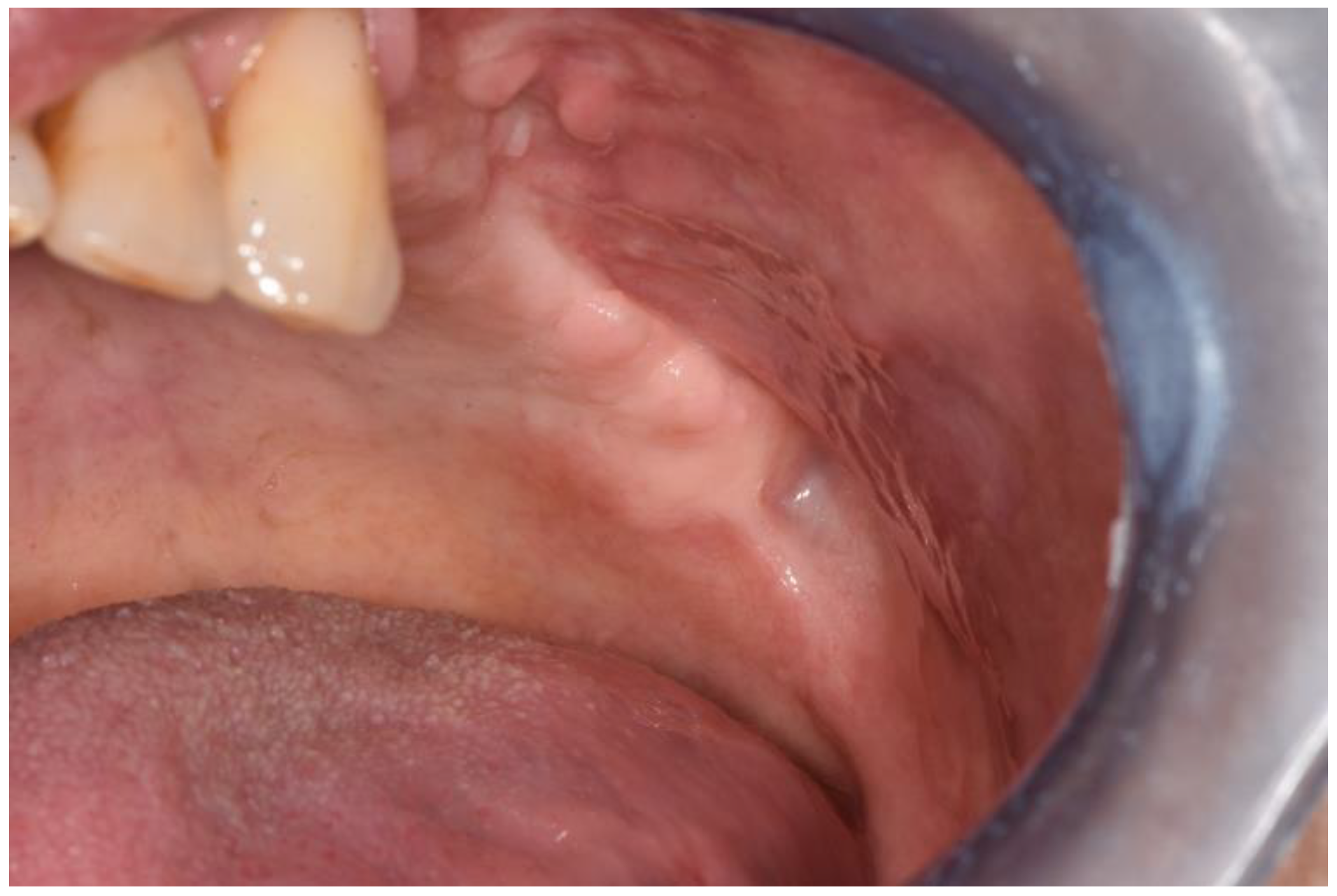
At the first postoperative check, healing of intraoral and nasal soft tissues were evaluated through an oral inspection and endoscopy.
For the control group, to achieve the best compliance from the patient, conscious sedation was induced with chloromethyl diazepam at 2 mg per os associated with diazepam or intravenous midazolam, following described protocols in the literature [
9].
Local anesthesia of the affected maxillary sinus was performed with maxillary nerve block (7) and paraperiosteal anesthesia with 2% mepivacaine and adrenaline at a ratio of 1:100,000 for better visibility of the operative field.
A full-thickness vestibular flap was then set up with medial and distal release incisions. If necessary, we proceeded with ostectomy and osteoplasty [
10]. A delicate toilet of the maxillary sinus was performed by aspiration.
The maxillary sinus was irrigated without performing procedures regarding the enlargement of the ostium.
With horizontal periosteum incision, Bichat’s fat pad could be isolated and advanced
In cases of evident inflammation and/or other pathological conditions (neoformations, foreign bodies), a biopsy was performed.
After 12 months, the control CTs were performed (
Figure 1,
Figure 2,
Figure 3,
Figure 4,
Figure 5,
Figure 6,
Figure 7,
Figure 8,
Figure 9,
Figure 10,
Figure 11 and
Figure 12).
To evaluate healing, the primary outcome was measured by symptom resolution, absence of purulent discharge at endoscopy and pathological obliterations on CT; the secondary outcome was to collect the characteristics of the sample.
Informed consent was always obtained, privacy was respected the research was approved by the Ethics Committee for Clinical Trials (CESC) at Padua University Hospital (163n/AO/2).
3. Results
10 patients (aged between 42 and 70) formed the case group and 10 patients (aged between 51 and 74) formed the control group (
Table 1).
None of them showed absolute contraindications for any type of proposed intervention or for general anesthesia.
The anamnestic characteristics of the two groups are summarized in
Table 1.
In the control group, the intraoral and endoscopic clinical checks at 10 or 15 days and 30 days showed excellent epithelization. There were no cases of dehiscence or oroantral communications relapse. The endoscopic control investigation showed inflammation and edema resolution and sinus patency.
Intraoral clinical checks were performed 10 or 15 days and 30 days after surgery to the patients belonging in the case group. Excellent epithelialization, no dehiscence or oroantral communications relapses were observed.
In one case, during the oral surgery, we appreciated the pterygopalatine fossa due to the erosion of the posterior wall of the maxillary sinus affected by pathology.
The histological examination in both groups gave similar results, such as: ulcerated respiratory mucosa with hyperplastic alterations; lymphocyte infiltrate; granulocytosis; and focal vasculitic aspects.
In the case group there was one case of a cyst with non-keratinized multi-layered epithelium, with chronic inflammation, cholesterin crystals and necrotic amorphous material including fungal hyphae and spores. There were also two cases of bone resection of osteonecrosis areas, which were histologically confirmed and potentially related to Denosumab and previously Zoledronate systemic therapy [
11].
After 12 months, the control CT scans were performed confirming the resolution of the disease; no symptoms were detected.
Comparing the therapeutic success of the two groups t student distribution values (p < 0.025) CI (95%) 1.11 < CI < 4.28; OR = 2.18 show no statistically significant difference.
4. Discussion
Traditional Cadwell-Luc sinus revision with an inferior antrostomy and opening in the lower meatus can maintain a residual inflammatory process which leaves scar tissue that alters the physiology of the sinus, even after long-term healing [
12].
However, the recovery of nasal sinus physiology is well documented when endoscopically assisted surgery is performed.
The Bichat’s fat pad use was motivated not only by the possibility of creating a double layer flap, but also by its osteoprogenious potential, which would promote the regeneration of bone tissue [
13].
The interesting result is the resolution of the odontogenic sinusitis with obliteration of ostiomeatal complex via an oral approach only, without general anesthesia nor a multidisciplinary approach.
In addition, this would allow a more conservative surgery with the preservation of the specialized epithelium of the maxillary sinus and with the maintenance of the ostium integrity without any ostectomy, as happens in FESS.
Both surgical procedures analyzed in this case–control retrospective study are described in the literature. However, it is only recently that, in a similar manner, “modified endoscopy-assisted maxillary sinus surgery (MESS)” was described for the reduction of exploded orbital fractures, removal of sinus pathologies and removal of implants migrated under the optic canal. The aims of this easy surgical procedure are to maintain the sinus physiology and preserve the middle meatus [
14].
Numerous articles [
15] and consensus conferences [
16] have discussed which classification should be applied, but there is no defined one yet, therefore no classification was used in this study. Felisati’s 2013 [
17] classification proposes ESS as a treatment for any case of maxillary sinusitis; however, as our data suggest, it is not always necessary.