Self-Administered Cognitive Rehabilitation Using an Electronic Device in Subacute Stroke Patients: A Proof-of-Concept Study on Safety, Feasibility, and Preliminary Efficacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Participants
2.3. Blinding and Allocation
2.4. Treatment Procedures
2.4.1. Face-to-Face Treatment
2.4.2. Self-Treatment
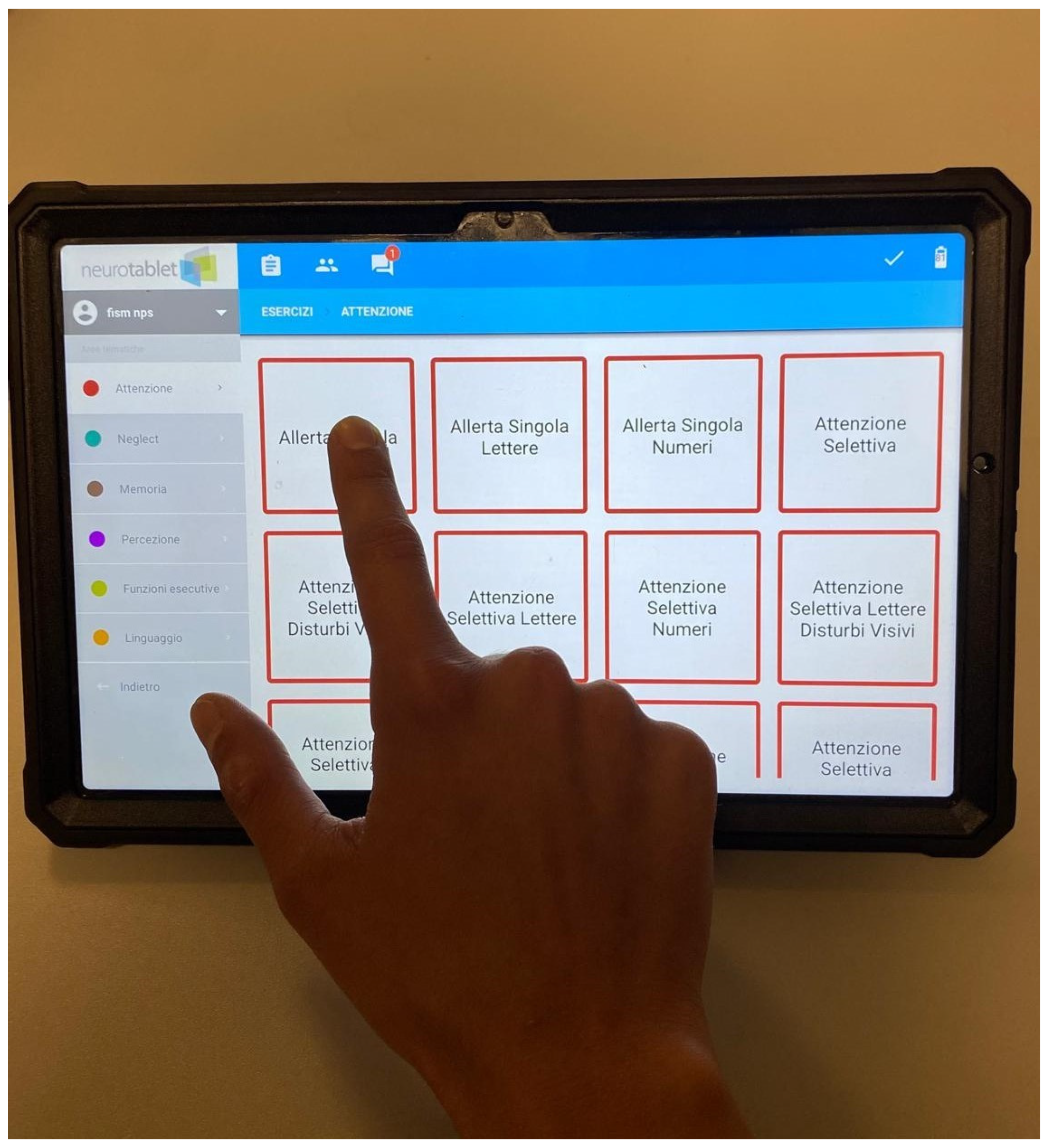
Experimental Group
Control Group
2.5. Outcome Measures
2.5.1. Primary Outcome
2.5.2. Secondary Outcomes
2.6. Statistical Analysis
3. Results
3.1. Baseline
3.2. Post-Intervention
3.2.1. Primary Outcomes
3.2.2. Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| EG | Experimental Group |
| CG | Control Group |
| OCS | Oxford Cognitive Screen |
| TMT-A | Trail Making Test A |
| TMT-B | Trail Making Test B |
| EPMT | Elithorn’s Perceptual Maze Test |
| ANOVA | Analysis of Variance |
| SD | Standard Deviation |
References
- De Luca, R.; Leonardi, S.; Spadaro, L.; Russo, M.; Aragona, B.; Torrisi, M.; Maggio, M.G.; Bramanti, A.; Naro, A.; De Cola, M.C.; et al. Improving Cognitive Function in Patients with Stroke: Can Computerized Training Be the Future? J. Stroke Cerebrovasc. Dis. 2018, 27, 1055–1060. [Google Scholar] [CrossRef] [PubMed]
- Tagliente, S.; Minafra, B.; Aresta, S.; Santacesaria, P.; Buccoliero, A.; Palmirotta, C.; Lagravinese, G.; Mongelli, D.; Gelao, C.; Macchitella, L.; et al. Effectiveness of a home-based computerized cognitive training in Parkinson’s disease: A pilot randomized cross-over study. Front. Psychol. 2025, 15, 1531688. [Google Scholar] [CrossRef]
- Li, X.; He, Y.; Wang, D.; Rezaei, M.J. Stroke rehabilitation: From diagnosis to therapy. Front. Neurol. 2024, 15, 1402729. [Google Scholar] [CrossRef]
- Tong, Y.; Ding, Y.; Han, Z.; Duan, H.; Geng, X. Optimal rehabilitation strategies for early postacute stroke recovery: An ongoing inquiry. Brain Circ. 2023, 9, 201–204. [Google Scholar] [CrossRef]
- Stapleton, T.; Ashburn, A.; Stack, E. A pilot study of attention deficits, balance control and falls in the subacute stage following stroke. Clin. Rehabil. 2001, 15, 437–444. [Google Scholar] [CrossRef]
- Turunen, K.E.; Laari, S.P.; Kauranen, T.V.; Uimonen, J.; Mustanoja, S.; Tatlisumak, T.; Poutiainen, E. Domain-Specific Cognitive Recovery after First-Ever Stroke: A 2-Year Follow-Up. J. Int. Neuropsychol. Soc. 2017, 24, 117–127. [Google Scholar] [CrossRef]
- Hyndman, D.; Pickering, R.M.; Ashburn, A. The influence of attention deficits on functional recovery post stroke during the first 12 months after discharge from hospital. J. Neurol. Neurosurg. Psychiatry 2007, 79, 656–663. [Google Scholar] [CrossRef]
- Hochstenbach, J.; Mulder, T.; van Limbeek, J.; Donders, R.; Schoonderwaldt, H. Cognitive Decline Following Stroke: A Comprehensive Study of Cognitive Decline Following Stroke*. J. Clin. Exp. Neuropsychol. 1998, 20, 503–517. [Google Scholar] [CrossRef] [PubMed]
- Rasquin, S.M.; Lodder, J.; Ponds, R.W.; Winkens, I.; Jolles, J.; Verhey, F.R. Cognitive Functioning after Stroke: A One-Year Follow-Up Study. Dement. Geriatr. Cogn. Disord. 2004, 18, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Hochstenbach, J.B.; Otter, R.D.; Mulder, T.W. Cognitive recovery after stroke: A 2-year follow-up. Arch. Phys. Med. Rehabil. 2003, 84, 1499–1504. [Google Scholar] [CrossRef]
- Barker-Collo, S.; Feigin, V.; Parag, V.; Lawes, C.; Senior, H. Auckland Stroke Outcomes Study. Neurology 2010, 75, 1608–1616. [Google Scholar] [CrossRef]
- Hyndman, D.; Ashburn, A. People with stroke living in the community: Attention deficits, balance, ADL ability and falls. Disabil. Rehabil. 2003, 25, 817–822. [Google Scholar] [CrossRef]
- Middleton, L.E.; Lam, B.; Fahmi, H.; Black, S.E.; McIlroy, W.E.; Stuss, D.T.; Danells, C.; Ween, J.; Turner, G.R. Frequency of domain-specific cognitive impairment in sub-acute and chronic stroke. NeuroRehabilitation 2014, 34, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Jang, J.-W.; Park, S.Y.; Wang, M.J.; Lim, J.-S.; Baek, M.J.; Kim, B.J.; Han, M.-K.; Bae, H.-J.; Ahn, S.; et al. Executive Function as a Strong Predictor of Recovery from Disability in Patients with Acute Stroke: A Preliminary Study. J. Stroke Cerebrovasc. Dis. 2015, 24, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Loetscher, T.; Potter, K.-J.; Wong, D.; das Nair, R.; Cochrane Stroke Group. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst. Rev. 2019, 2019, CD002842. [Google Scholar] [CrossRef] [PubMed]
- Navarro, M.D.; Llorens, R.; Borrego, A.; Alcañiz, M.; Noé, E.; Ferri, J. Competition Enhances the Effectiveness and Motivation of Attention Rehabilitation After Stroke. A Randomized Controlled Trial. Front. Hum. Neurosci. 2020, 14, 575403. [Google Scholar] [CrossRef]
- Lezak, M.D.; Howieson, D.B.; Loring, D.W.; Hannay, H.J.; Fischer, J.S. Neuropsychological Assessment, 4th ed.; Oxford University Press: New York, NY, USA, 2004; p. xiv, 1016. [Google Scholar]
- Mancuso, M.; CogniReMo Study Group; Iosa, M.; Abbruzzese, L.; Matano, A.; Coccia, M.; Baudo, S.; Benedetti, A.; Gambarelli, C.; Spaccavento, S.; et al. The impact of cognitive function deficits and their recovery on functional outcome in subjects affected by ischemic subacute stroke: Results from the Italian multicenter longitudinal study CogniReMo. Eur. J. Phys. Rehabil. Med. 2023, 59, 284–293. [Google Scholar] [CrossRef]
- Cho, H.-Y.; Kim, K.-T.; Jung, J.-H. Effects of computer assisted cognitive rehabilitation on brain wave, memory and attention of stroke patients: A randomized control trial. J. Phys. Ther. Sci. 2015, 27, 1029–1032. [Google Scholar] [CrossRef] [PubMed]
- Mitrovic, A.; Mathews, M.; Ohlsson, S.; Holland, J.; McKinlay, A. Computer-based post-stroke rehabilitation of prospective memory. J. Appl. Res. Mem. Cogn. 2016, 5, 204–214. [Google Scholar] [CrossRef]
- Westerberg, H.; Jacobaeus, H.; Hirvikoski, T.; Clevberger, P.; Östensson, M.-L.; Bartfai, A.; Klingberg, T. Computerized working memory training after stroke—A pilot study. Brain Inj. 2007, 21, 21–29. [Google Scholar] [CrossRef]
- Yoo, C.; Yong, M.-H.; Chung, J.; Yang, Y. Effect of computerized cognitive rehabilitation program on cognitive function and activities of living in stroke patients. J. Phys. Ther. Sci. 2015, 27, 2487–2489. [Google Scholar] [CrossRef]
- Svaerke, K.; Niemeijer, M.; Mogensen, J.; Christensen, H. The effects of computer-based cognitive rehabilitation in patients with visuospatial neglect following stroke: A systematic review. Top. Stroke Rehabil. 2018, 26, 214–225. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Huang, L.; Yi, J.; Zhang, T.; Zhu, G.; Zhang, Q.; Tian, J.; Zhao, R.; Duan, X.; Liu, Z. The Effectiveness of Computerized Cognitive Training in Patients with Post-Stroke Cognitive Impairment: A Systematic Review and Meta-analysis (Preprint). J. Med. Internet Res. 2025, 27, e73140. [Google Scholar] [CrossRef]
- Dardiotis, E.; Nousia, A.; Siokas, V.; Tsouris, Z.; Andravizou, A.; Mentis, A.-F.A.; Florou, D.; Messinis, L.; Nasios, G. Efficacy of computer-based cognitive training in neuropsychological performance of patients with multiple sclerosis: A systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2018, 20, 58–66. [Google Scholar] [CrossRef]
- Moghadasi, A.N.; Mirmosayyeb, O.; Bagherieh, S.; Sahraian, M.A.; Ghajarzadeh, M. Computerized cognitive rehabilitation in patients with multiple sclerosis (MS): A systematic review and meta-analysis. Casp. J. Intern. Med. 2025, 16, 9–19. [Google Scholar] [CrossRef]
- Nousia, A.; Martzoukou, M.; Tsouris, Z.; Siokas, V.; Aloizou, A.-M.; Liampas, I.; Nasios, G.; Dardiotis, E. The Beneficial Effects of Computer-Based Cognitive Training in Parkinson’s Disease: A Systematic Review. Arch. Clin. Neuropsychol. 2020, 35, 434–447. [Google Scholar] [CrossRef]
- Veisi-Pirkoohi, S.; Hassani-Abharian, P.; Kazemi, R.; Vaseghi, S.; Zarrindast, M.-R.; Nasehi, M. Efficacy of RehaCom cognitive rehabilitation software in activities of daily living, attention and response control in chronic stroke patients. J. Clin. Neurosci. 2020, 71, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Polanowska, K.E.; Iwański, S.; Leśniak, M.M.; Seniów, J. Computer-assisted training of executive functions in adult patients with non-progressive acquired brain damage—A pilot study on efficacy of a new therapeutic application. Appl. Neuropsychol. Adult 2022, 31, 1180–1191. [Google Scholar] [CrossRef]
- Maresca, G.; Maggio, M.G.; De Luca, R.; Manuli, A.; Tonin, P.; Pignolo, L.; Calabrò, R.S. Tele-Neuro-Rehabilitation in Italy: State of the Art and Future Perspectives. Front. Neurol. 2020, 11, 563375. [Google Scholar] [CrossRef]
- Rahmani-Katigari, M.; Mohammadian, F.; Shahmoradi, L. Development of a serious game-based cognitive rehabilitation system for patients with brain injury. BMC Psychiatry 2023, 23, 893. [Google Scholar] [CrossRef]
- Nie, P.; Liu, F.; Lin, S.; Guo, J.; Chen, X.; Chen, S.; Yu, L.; Lin, R. The effects of computer-assisted cognitive rehabilitation on cognitive impairment after stroke: A systematic review and meta-analysis. J. Clin. Nurs. 2021, 31, 1136–1148. [Google Scholar] [CrossRef]
- Fava-Felix, P.E.; Bonome-Vanzelli, S.R.C.; Ribeiro, F.S.; Santos, F.H. Systematic review on post-stroke computerized cognitive training: Unveiling the impact of confounding factors. Front. Psychol. 2022, 13, 985438. [Google Scholar] [CrossRef]
- Maggio, M.G.; De Bartolo, D.; Calabrò, R.S.; Ciancarelli, I.; Cerasa, A.; Tonin, P.; Di Iulio, F.; Paolucci, S.; Antonucci, G.; Morone, G.; et al. Computer-assisted cognitive rehabilitation in neurological patients: State-of-art and future perspectives. Front. Neurol. 2023, 14, 1255319. [Google Scholar] [CrossRef]
- The Italian OCS Group; Mancuso, M.; Varalta, V.; Sardella, L.; Capitani, D.; Zoccolotti, P.; Antonucci, G. Italian normative data for a stroke specific cognitive screening tool: The Oxford Cognitive Screen (OCS). Neurol. Sci. 2016, 37, 1713–1721. [Google Scholar] [CrossRef] [PubMed]
- Giovagnoli, A.R.; Del Pesce, M.; Mascheroni, S.; Simoncelli, M.; Laiacona, M.; Capitani, E. Trail making test: Normative values from 287 normal adult controls. Ital. J. Neurol. Sci. 1996, 17, 305–309. [Google Scholar] [CrossRef]
- Baddeley, A.; Della Sala, S.; Papagno, C.; Spinnler, H. Dual-task performance in dysexecutive and nondysexecutive patients with a frontal lesion. Neuropsychology 1997, 11, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Caffarra, P.; Vezzadini, G.; Francesca, D.; Zonato, F.; Venneri, A. Una versione abbreviata del test di Stroop: Dati normativi nella popolazione italiana. Nuova Riv. Di Neurol. 2002, 12, 111–115. [Google Scholar]
- Spinnler, H.; Tognoni, G.; Gruppo Italiano per lo Studio Neuropsicologico dell’Invecchiamento. Standardizzazione e Taratura Italiana di Test Neuropsicologici; Masson Italia Periodici: Milano, Italy, 1987. [Google Scholar]
- Kim, H.S.; Lim, K.-B.; Yoo, J.; Kim, Y.W.; Lee, S.W.; Son, S.; Kim, C.; Kim, J. The efficacy of computerized cognitive rehabilitation in improving attention and executive functions in acquired brain injury patients, in acute and postacute phase. Eur. J. Phys. Rehabil. Med. 2021, 57, 551–559. [Google Scholar] [CrossRef]
- Zampolini, M.; Selb, M.; Boldrini, P.; Branco, C.A.; Golyk, V.; Hu, X.; Kiekens, C.; Negrini, S.; Nulle, A.; Oral, A.; et al. The Individual Rehabilitation Project as the core of person-centered rehabilitation: The Physical and Rehabilitation Medicine Section and Board of the European Union of Medical Specialists Framework for Rehabilitation in Europe. Eur. J. Phys. Rehabil. Med. 2022, 58, 503–510. [Google Scholar] [CrossRef]
- Manocchio, N.; Ljoka, C.; Ferdinandi, V.; Cicchi, L.; Foti, C. Commentary on “The learning rehabilitation system: Strengthening an intersectoral strategy to improve functioning of an ageing population” by Bickenbach et al. Health Policy 2025, 155, 105303. [Google Scholar] [CrossRef]
- Bertoni, D.; Bruni, S.; Saviola, D.; De Tanti, A.; Costantino, C. The Role of Cognitive Reserve in Post-Stroke Rehabilitation Outcomes: A Systematic Review. Brain Sci. 2024, 14, 1144. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.S.M.; Liu, T.-W.; Tsoh, J.; Chen, P.; Cheng, T.S.; Cheung, M.C.H.; Leung, A.H.H.; Ng, L.L.Y.; So, K.Y.K.; Tse, M.M.Y. Psychometric Properties of the Trail Walking Test for People With Stroke. Front. Neurol. 2022, 13, 821670. [Google Scholar] [CrossRef] [PubMed]
- Williams, O.A.; Demeyere, N. Association of Depression and Anxiety with Cognitive Impairment 6 Months After Stroke. Neurology 2021, 96, e1966–e1974. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Kim, G. Functional Recovery in Acute and Subacute Stroke Patients with or Without Post-stroke Fatigue. Brain Neurorehabilit. 2024, 17, e22. [Google Scholar] [CrossRef]

| Sessions | Exercises and Duration |
|---|---|
| SESSION 1 (day 1–2–3) | -15 min Selective Attention Letters Visual Disorders -10 min Selective Attention Aligned Numbers -15 min Flow Free |
| SESSION 2 (day 4–5) | -15 min Alternate Attention Letters -10 min Selective Attention Aligned Numbers -15 min Flow Free |
| SESSION 3 (day 6–7–8) | -15 min Single Uniform Attention -10 min Alternate Attention Visual Multiple Letters -15 min Split Screen Control/Inhibition |
| SESSION 4 (day 9–10) | -15 min Multiple Uniform Attention -10 min Control/Inhibition Acoustic Screen -15 min Stroop Arrows |
| Sessions | Exercises and Duration |
|---|---|
| SESSION 1 (day 1–2–3) | -15 min Selective Attention Numbers Visual Disorders -15 min Flow Free -15 min Selective Attention Aligned Letters |
| SESSION 2 (day 4–5) | -15 min Alternate Attention Numbers -15 min Flow Free -15 min Selective Attention Aligned Letters |
| SESSION 3 (day 6–7–8) | -15 min Single Uniform Attention -15 min Split Screen Control/Inhibition -15 min Alternate Attention Visual Multiple Numbers |
| SESSION 4 (day 9–10) | -15 min Multiple Uniform Attention -15 min Control/Inhibition Acoustic Screen -15 min Stroop Arrows |
| Characteristic | EG n = 11 | CG n = 12 | p-Value (Z) |
|---|---|---|---|
| Sex—M/F | 4/7 | 6/6 | 0.519 (−0.645) |
| Age—years | 67 (±9.64) | 66.92 (±10.52) | 0.926 (−0.092) |
| Education level—years | 10.36 (±5.04) | 8.42 (±3.75) | 0.297 (−1.043) |
| Stroke type—I/H | 7/4 | 8/4 | 0.881 (−0.149) |
| Lesion-side (left/right/bilateral) | 4/4/3 | 7/5/0 | 0.344 (−0.946) |
| Time from onset (days) | 20.91 (±13.74) | 23.92 (±19.59) | 0.829 (−0.216) |
| Semantics subtest—OCS | 3 | 3 | 1 (0) |
| Broken hearts subtest—OCS | 34.82 (±10.71) | 36.75 (±10.69) | 0.44 (−0.772) |
| Spatial asymmetry—OCS | −0.64 (±1.63) | 0.75 (±1.54) | 0.061(−1.875) |
| Trails task subtest—OCS | 8.63 (±4.47) | 7.83 (±4.06) | 0.64 (−0.468) |
| Outcome Measure | Group | T0 | T1 |
|---|---|---|---|
| TMT-A (s) | EG | 138.09 (±115.65) | 102.27 (±52.55) |
| CG | 120.5 (±61.14) | 95.42 (±56.39) | |
| Dual Task (mu) | EG | 72.18 (±13.91) | 90.42 (±22.12) |
| CG | 84.49 (±13.16) | 90.50 (±14.71) | |
| Stroop-time (s) | EG | 59.35 (±33.75) | 43.6 (±26.56) |
| CG | 47.08 (±29.82) | 37.98 (±25.02) |
| Outcome Measure | Group | T0 | T1 | p-Value (Z) |
|---|---|---|---|---|
| TMT-B (s) | EG | 401.54 (±107.06) | 342.73 (±158.28) | 0.043 * (−2.028) |
| CG | 333.33 (±142.25) | 309.92 (±214.37) | 0.214 (−1.244) | |
| Stroop- errors (0–30) | EG | 7.9 (±8.03) | 2.2 (±2.11) | 0.038 * (−2.075) |
| CG | 8.58 (±7.83) | 7.04 (±8.71) | 0.168 (−1.378) | |
| EPMT (0–16) | EG | 9.45 (±3.25) | 12.04 (±3.53) | 0.049 * (−1.968) |
| CG | 10.68 (±3.88) | 11.79 (±4.13) | 0.046 * (−1.994) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fonte, C.; Damora, A.; Abbruzzese, L.; Rotundo, G.; Picelli, A.; Gallinaro, Y.; Evangelista, E.; Mancuso, M.; Smania, N.; Varalta, V. Self-Administered Cognitive Rehabilitation Using an Electronic Device in Subacute Stroke Patients: A Proof-of-Concept Study on Safety, Feasibility, and Preliminary Efficacy. NeuroSci 2025, 6, 109. https://doi.org/10.3390/neurosci6040109
Fonte C, Damora A, Abbruzzese L, Rotundo G, Picelli A, Gallinaro Y, Evangelista E, Mancuso M, Smania N, Varalta V. Self-Administered Cognitive Rehabilitation Using an Electronic Device in Subacute Stroke Patients: A Proof-of-Concept Study on Safety, Feasibility, and Preliminary Efficacy. NeuroSci. 2025; 6(4):109. https://doi.org/10.3390/neurosci6040109
Chicago/Turabian StyleFonte, Cristina, Alessio Damora, Laura Abbruzzese, Giorgia Rotundo, Alessandro Picelli, Ylenia Gallinaro, Elisa Evangelista, Mauro Mancuso, Nicola Smania, and Valentina Varalta. 2025. "Self-Administered Cognitive Rehabilitation Using an Electronic Device in Subacute Stroke Patients: A Proof-of-Concept Study on Safety, Feasibility, and Preliminary Efficacy" NeuroSci 6, no. 4: 109. https://doi.org/10.3390/neurosci6040109
APA StyleFonte, C., Damora, A., Abbruzzese, L., Rotundo, G., Picelli, A., Gallinaro, Y., Evangelista, E., Mancuso, M., Smania, N., & Varalta, V. (2025). Self-Administered Cognitive Rehabilitation Using an Electronic Device in Subacute Stroke Patients: A Proof-of-Concept Study on Safety, Feasibility, and Preliminary Efficacy. NeuroSci, 6(4), 109. https://doi.org/10.3390/neurosci6040109







