Trends and Disparities in Alzheimer’s Disease Mortality in the United States: The Impact of COVID-19
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Overall
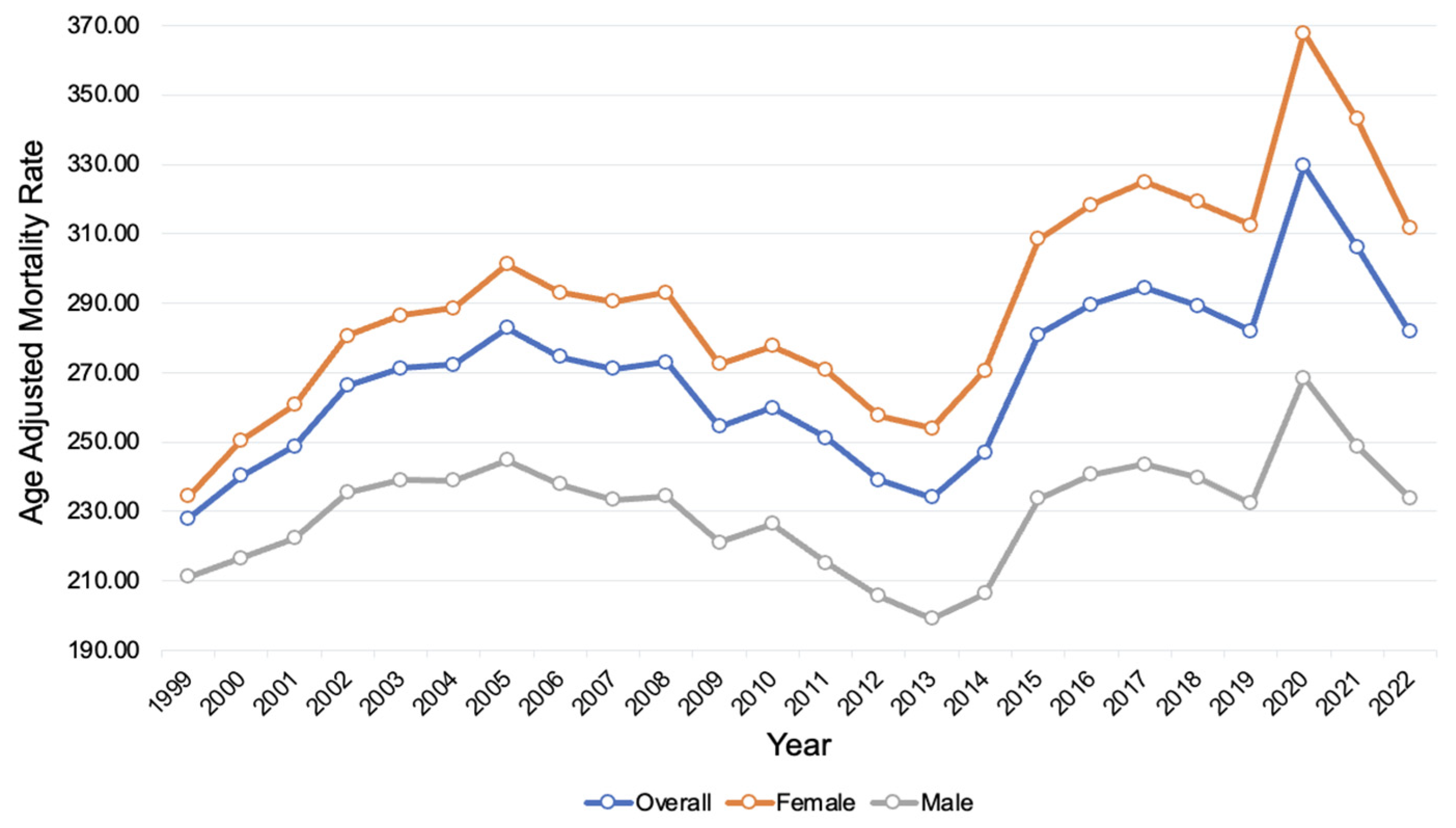
3.2. Disparities in AD-Related Mortality by Sex
3.3. Disparities in AD-Related Mortality by Race and Ethnicity
3.4. Disparities in AD-Related Mortality by Race and Sex
3.5. Disparities of AD-Related Mortality by Place of Death
3.6. Disparities in AD-Related Mortality by Age Group
3.7. Regional Disparities in AD-Related Mortality by State
3.8. Census-Region Disparities in AD-Related Mortality
3.9. Comparison Between Trends of AD-Related AAMR and All-Cause AAMR
4. Discussion
4.1. Overall Findings
4.2. Disparities in AD-Related Mortality by Sex
4.3. Disparities in AD-Related Mortality by Race and Ethnicity
4.4. Place of Death
4.5. Regional Differences
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Dzamba, D.; Harantova, L.; Butenko, O.; Anderova, M. Glial Cells—The Key Elements of Alzheimer’s Disease. Curr. Alzheimer Res. 2016, 13, 894–911. [Google Scholar] [CrossRef] [PubMed]
- Ray, B.; Lahiri, D.K. Neuroinflammation in Alzheimer’s disease: Different molecular targets and potential therapeutic agents including curcumin. Curr. Opin. Pharmacol. 2009, 9, 434–444. [Google Scholar] [CrossRef]
- Bhole, R.P.; Chikhale, R.V.; Rathi, K.M. Current biomarkers and treatment strategies in Alzheimer disease: An overview and future perspectives. IBRO Neurosci. Rep. 2023, 16, 8–42. [Google Scholar] [CrossRef]
- 2023 Alzheimer’s disease facts and figures. Alzheimers Dement. 2023, 19, 1598–1695. [CrossRef] [PubMed]
- Mayo Foundation for Medical Education and Research. Alzheimer’s Stages: How the Disease Progresses. Mayo Clinic. 7 June 2023. Available online: https://www.mayoclinic.org/diseases-conditions/alzheimers-disease/in-depth/alzheimers-stages/art-20048448 (accessed on 15 December 2024).
- 2021 Alzheimer’s disease facts and figures. Alzheimers Dement. 2021, 17, 327–406. [CrossRef] [PubMed]
- Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1999–2020 on CDC WONDER Online Database, released in 2021. Data Are from the Multiple Cause of Death Files, 1999–2020, as Compiled from Data Provided by the 57 Vital Statistics Jurisdictions Through the Vital Statistics Cooperative Program. Available online: http://wonder.cdc.gov/mcd-icd10.html (accessed on 30 January 2024).
- Anderson, R.N.; Rosenberg, H.M. Age Standardization of Death Rates: Implementation of the Year 2000 Standard. Available online: https://stacks.cdc.gov/view/cdc/13357 (accessed on 15 December 2024).
- Joinpoint Regression Program, Version 5.0.2—May 2023; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute. Available online: https://surveillance.cancer.gov/joinpoint/ (accessed on 10 December 2024).
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- Zhao, X.; Li, C.; Ding, G.; Heng, Y.; Li, A.; Wang, W.; Hou, H.; Wen, J.; Zhang, Y. The Burden of Alzheimer’s Disease Mortality in the United States, 1999–2018. J. Alzheimers Dis. 2021, 82, 803–813. [Google Scholar] [CrossRef]
- Mobaderi, T.; Kazemnejad, A.; Salehi, M. Exploring the impacts of risk factors on mortality patterns of global Alzheimer’s disease and related dementias from 1990 to 2021. Sci. Rep. 2024, 14, 15583. [Google Scholar] [CrossRef]
- Gilstrap, L.; Zhou, W.; Alsan, M.; Nanda, A.; Skinner, J.S. Trends in Mortality Rates Among Medicare Enrollees With Alzheimer Disease and Related Dementias Before and During the Early Phase of the COVID-19 Pandemic. JAMA Neurol. 2022, 79, 342–348. [Google Scholar] [CrossRef] [PubMed]
- Mogharab, V.; Ostovar, M.; Ruszkowski, J.; Hussain, S.Z.M.; Shrestha, R.; Yaqoob, U.; Aryanpoor, P.; Nikkhoo, A.M.; Heidari, P.; Jahromi, A.R.; et al. Global burden of the COVID-19 associated patient-related delay in emergency healthcare: A panel of systematic review and meta-analyses. Glob. Health 2022, 18, 58. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G. Mortality for Alzheimer’s disease during the COVID-19 pandemic. Eur. Geriatr. Med. 2024; advance online publication. [Google Scholar] [CrossRef]
- Raji, C.A.; Lopez, O.L.; Kuller, L.H.; Carmichael, O.T.; Becker, J.T. Age, Alzheimer disease, and brain structure. Neurology 2009, 73, 1899–1905. [Google Scholar] [CrossRef]
- Gao, S.; Hendrie, H.C.; Hall, K.S.; Hui, S. The relationships between age, sex, and the incidence of dementia and Alzheimer disease: A meta-analysis. Arch. Gen. Psychiatry 1998, 55, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Rudnicka-Drożak, E.; Drożak, P.; Mizerski, G.; Zaborowski, T.; Ślusarska, B.; Nowicki, G.; Drożak, M. Links between COVID-19 and Alzheimer’s Disease—What Do We Already Know? Int. J. Environ. Res. Public Health 2023, 20, 2146. [Google Scholar] [CrossRef]
- Shajahan, S.R.; Kumar, S.; Ramli, M.D.C. Unravelling the connection between COVID-19 and Alzheimer’s disease: A comprehensive review. Front. Aging Neurosci. 2024, 15, 1274452. [Google Scholar] [CrossRef]
- Li, W.; Sun, L.; Yue, L.; Xiao, S. Alzheimer’s disease and COVID-19: Interactions, intrinsic linkages, and the role of immunoinflammatory responses in this process. Front. Immunol. 2023, 14, 1120495. [Google Scholar] [CrossRef]
- Fernández Alonso, C.; Fuentes Ferrer, M.E.; García-Lamberechts, E.J.; Aguiló Mir, S.; Jiménez, S.; Jacob, J.; Piñera Salmerón, P.; Gil-Rodrigo, A.; Llorens, P.; Burillo-Putze, G.; et al. Members of the SIESTA network Impact of dementia on 30-, 180-, and 365-day mortality during the first pandemic wave in older adults seen in spanish emergency departments diagnosed with or without COVID-19. Aging Ment. Health 2024, 28, 1110–1118. [Google Scholar] [CrossRef]
- Kostev, K.; Gessler, N.; Wohlmuth, P.; Arnold, D.; Bein, B.; Bohlken, J.; Herrlinger, K.; Jacob, L.; Koyanagi, A.; Nowak, L.; et al. Is Dementia Associated with COVID-19 Mortality? A Multicenter Retrospective Cohort Study Conducted in 50 Hospitals in Germany. J. Alzheimers Dis. 2023, 91, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Fisher, D.W.; Bennett, D.A.; Dong, H. Sexual dimorphism in predisposition to Alzheimer’s disease. Neurobiol. Aging 2018, 70, 308–324. [Google Scholar] [CrossRef]
- Zhu, D.; Montagne, A.; Zhao, Z. Alzheimer’s pathogenic mechanisms and underlying sex difference. Cell. Mol. Life Sci. 2021, 78, 4907–4920. [Google Scholar] [CrossRef] [PubMed]
- Casaletto, K.B.; Nichols, E.; Aslanyan, V.; Simone, S.M.; Rabin, J.S.; La Joie, R.; Brickman, A.M.; Dams-O’Connor, K.; Palta, P.; Kumar, R.G.; et al. Sex-specific effects of microglial activation on Alzheimer’s disease proteinopathy in older adults. Brain 2022, 145, 3536–3545. [Google Scholar] [CrossRef]
- Seshadri, S.; Wolf, P.A.; Beiser, A.; Au, R.; McNulty, K.; White, R.; D’Agostino, R.B. Lifetime risk of dementia and Alzheimer’s disease. The impact of mortality on risk estimates in the Framingham Study. Neurology 1997, 49, 1498–1504. [Google Scholar] [CrossRef]
- Avila, J.F.; Vonk, J.M.J.; Verney, S.P.; Witkiewitz, K.; Arce Rentería, M.; Schupf, N.; Mayeux, R.; Manly, J.J. Sex/gender differences in cognitive trajectories vary as a function of race/ethnicity. Alzheimers Dement. 2019, 15, 1516–1523. [Google Scholar] [CrossRef] [PubMed]
- Mielke, M.M.; Aggarwal, N.T.; Vila-Castelar, C.; Agarwal, P.; Arenaza-Urquijo, E.M.; Brett, B.; Brugulat-Serrat, A.; DuBose, L.E.; Eikelboom, W.S.; Flatt, J.; et al. Diversity and Disparity Professional Interest Area Sex and Gender Special Interest Group Consideration of sex and gender in Alzheimer’s disease and related disorders from a global perspective. Alzheimers Dement. 2022, 18, 2707–2724. [Google Scholar] [CrossRef] [PubMed]
- Helzner, E.P.; Scarmeas, N.; Cosentino, S.; Tang, M.X.; Schupf, N.; Stern, Y. Survival in Alzheimer disease: A multiethnic, population-based study of incident cases. Neurology 2008, 71, 1489–1495. [Google Scholar] [CrossRef]
- Mehta, K.M.; Yaffe, K.; Pérez-Stable, E.J.; Stewart, A.; Barnes, D.; Kurland, B.F.; Miller, B.L. Race/ethnic differences in AD survival in US Alzheimer’s Disease Centers. Neurology 2008, 70, 1163–1170. [Google Scholar] [CrossRef]
- Morris, J.C.; Schindler, S.E.; McCue, L.M.; Moulder, K.L.; Benzinger, T.L.S.; Cruchaga, C.; Fagan, A.M.; Grant, E.; Gordon, B.A.; Holtzman, D.M.; et al. Assessment of Racial Disparities in Biomarkers for Alzheimer Disease. JAMA Neurol. 2019, 76, 264–273. [Google Scholar] [CrossRef]
- Belloy, M.E.; Andrews, S.J.; Le Guen, Y.; Cuccaro, M.; Farrer, L.A.; Napolioni, V.; Greicius, M.D. APOE Genotype and Alzheimer Disease Risk Across Age, Sex, and Population Ancestry. JAMA Neurol. 2023, 80, 1284–1294. [Google Scholar] [CrossRef] [PubMed]
- Akushevich, I.; Kolpakov, S.; Yashkin, A.P.; Kravchenko, J. Vulnerability to Hypertension Is a Major Determinant of Racial Disparities in Alzheimer’s Disease Risk. Am. J. Hypertens. 2022, 35, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Ebisu, K. Environmental inequality in exposures to airborne particulate matter components in the United States. Environ. Health Perspect. 2012, 120, 1699–1704. [Google Scholar] [CrossRef] [PubMed]
- Younan, D.; Wang, X.; Gruenewald, T.; Gatz, M.; Serre, M.L.; Vizuete, W.; Braskie, M.N.; Woods, N.F.; Kahe, K.; Garcia, L.; et al. Racial/Ethnic Disparities in Alzheimer’s Disease Risk: Role of Exposure to Ambient Fine Particles. J. Gerontol. Ser. A 2022, 77, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Kosar, C.M.; Mor, V.; Werner, R.M.; Rahman, M. Risk of Discharge to Lower-Quality Nursing Homes Among Hospitalized Older Adults With Alzheimer Disease and Related Dementias. JAMA Netw. Open 2023, 6, e2255134. [Google Scholar] [CrossRef]
- Cross, S.H.; Kaufman, B.G.; Taylor, D.H., Jr.; Kamal, A.H.; Warraich, H.J. Trends and Factors Associated with Place of Death for Individuals with Dementia in the United States. J. Am. Geriatr. Soc. 2020, 68, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Schorr, C.A.; Angelo, M.; John, G.; LeCompte, K.; Dellinger, R.P. The Association of Increasing Hospice Use With Decreasing Hospital Mortality: An Analysis of the National Inpatient Sample. J. Healthc. Manag. 2020, 65, 107–120. [Google Scholar] [CrossRef] [PubMed]
- Hallas, L.; Hatibie, A.; Majumdar, S.; Pyarali, M.; Hale, T. Variation in US states’ Responses to COVID-19; University of Oxford: Oxford, UK, 2021. [Google Scholar]
- Ailshire, J.A.; Walsemann, K.M.; Fisk, C.E. Regional variation in U.S dementia trends from 2000–2012. SSM—Popul. Health 2022, 19, 101164. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaddha, J.; Blaney, E.; Al-Salahat, A.; Noor, A.; Billion, T.; Chen, Y.-T.; Tauseef, A.; Sood, A.; Abdul Jabbar, A.B. Trends and Disparities in Alzheimer’s Disease Mortality in the United States: The Impact of COVID-19. NeuroSci 2025, 6, 16. https://doi.org/10.3390/neurosci6010016
Chaddha J, Blaney E, Al-Salahat A, Noor A, Billion T, Chen Y-T, Tauseef A, Sood A, Abdul Jabbar AB. Trends and Disparities in Alzheimer’s Disease Mortality in the United States: The Impact of COVID-19. NeuroSci. 2025; 6(1):16. https://doi.org/10.3390/neurosci6010016
Chicago/Turabian StyleChaddha, Jasleen, Eli Blaney, Ali Al-Salahat, Amna Noor, Taylor Billion, Yu-Ting Chen, Abubakar Tauseef, Akshat Sood, and Ali Bin Abdul Jabbar. 2025. "Trends and Disparities in Alzheimer’s Disease Mortality in the United States: The Impact of COVID-19" NeuroSci 6, no. 1: 16. https://doi.org/10.3390/neurosci6010016
APA StyleChaddha, J., Blaney, E., Al-Salahat, A., Noor, A., Billion, T., Chen, Y.-T., Tauseef, A., Sood, A., & Abdul Jabbar, A. B. (2025). Trends and Disparities in Alzheimer’s Disease Mortality in the United States: The Impact of COVID-19. NeuroSci, 6(1), 16. https://doi.org/10.3390/neurosci6010016





