Discontinuation of Cerebro-Spinal Fluid (CSF) Drainage in Acute Hydrocephalus: A Prospective Cohort Study and Exploratory Data Analysis
Abstract
1. Introduction
2. Methods
2.1. Reporting Guidelines
2.2. Ethics
2.3. Participants
2.4. Data Collection
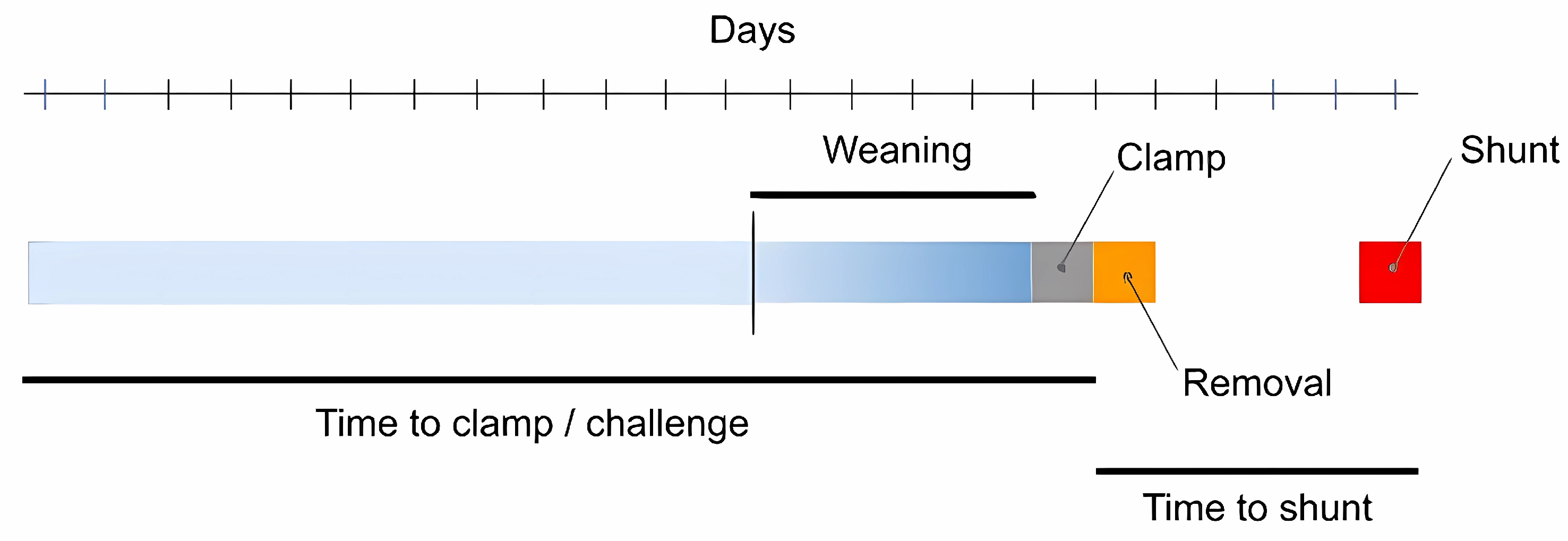
2.5. Weaning
2.6. Outcomes
2.7. Data Analysis
3. Results
3.1. Demographics
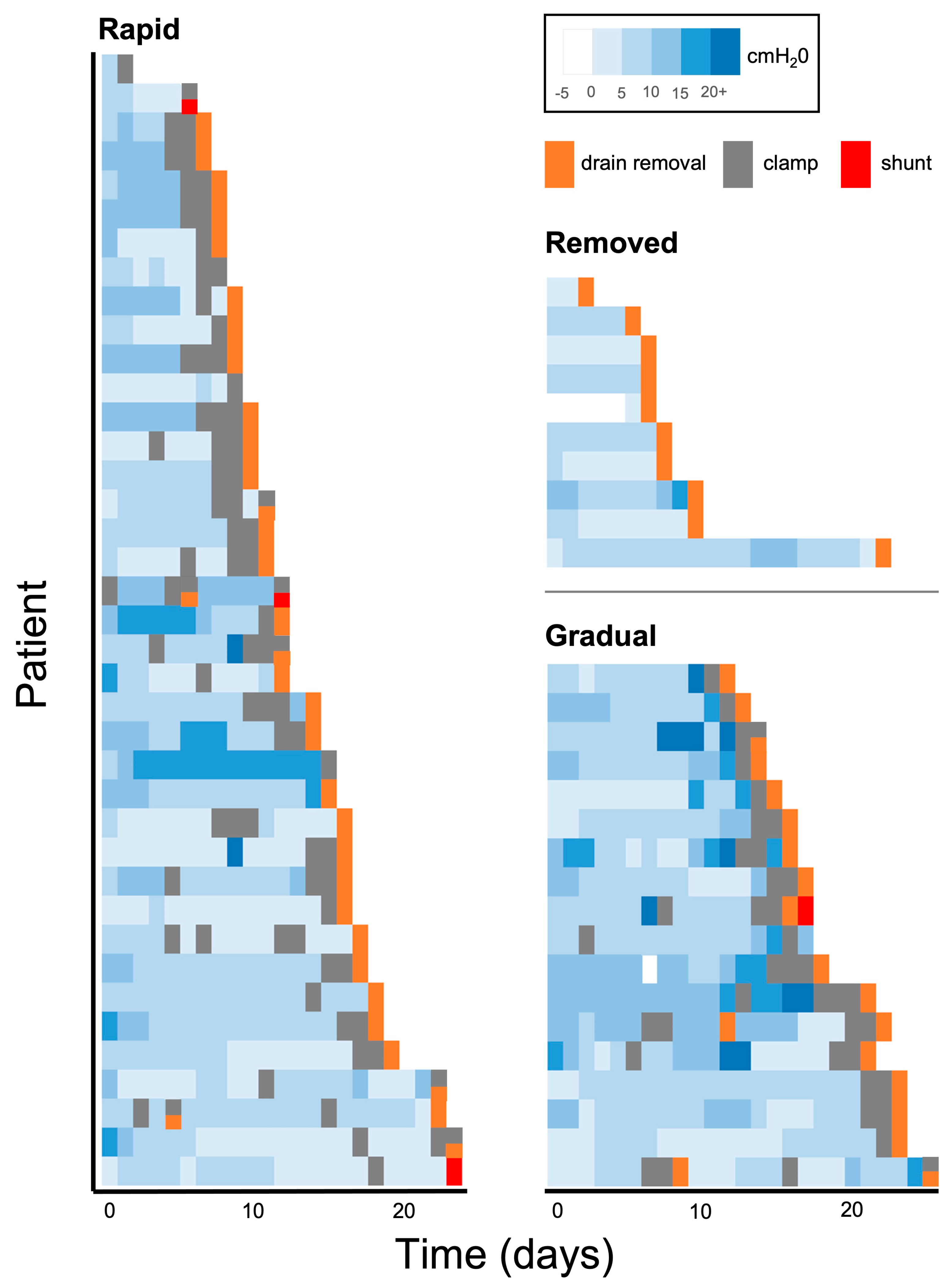
3.2. Wean Patterns
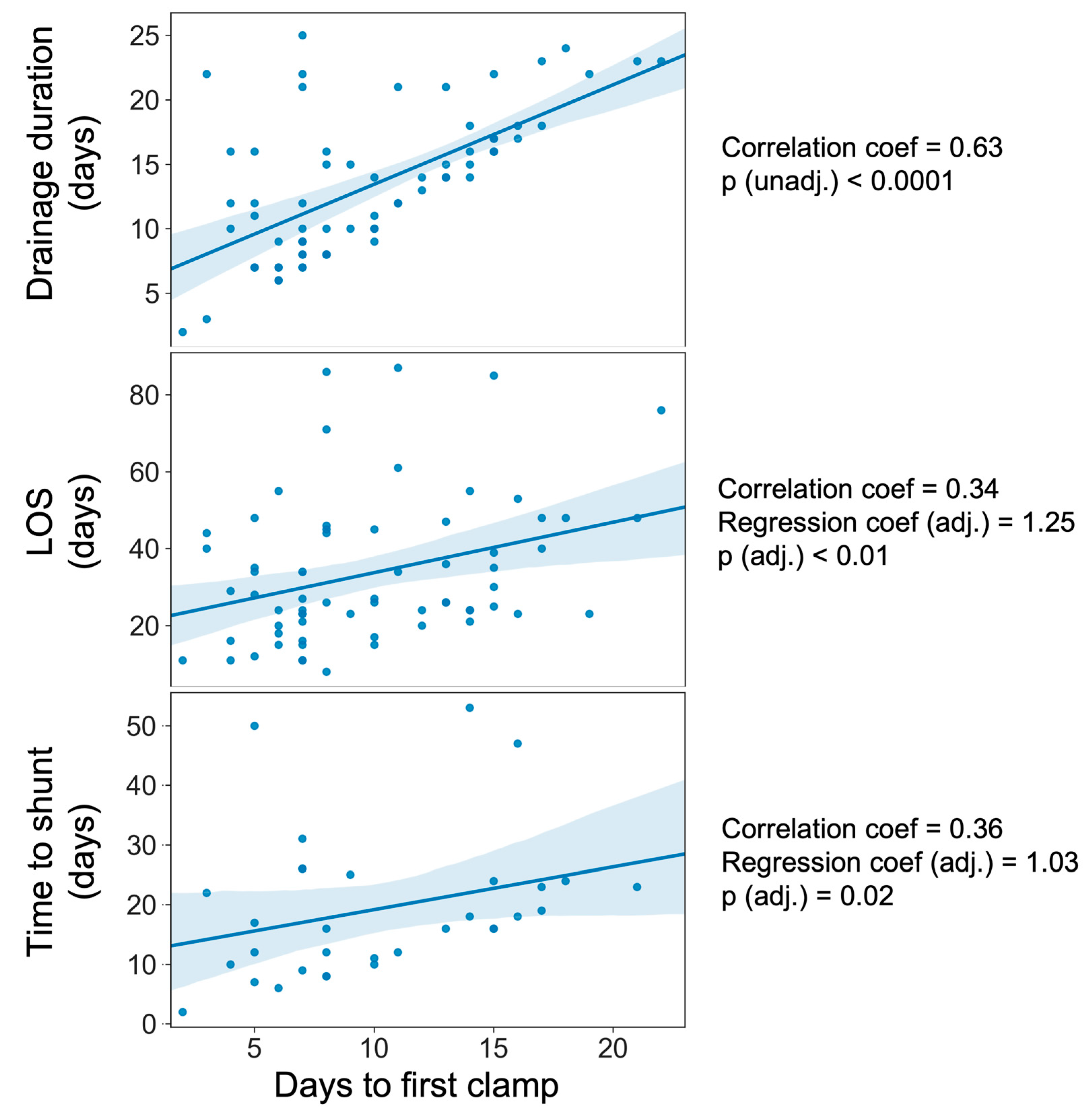
3.3. Influence of Weaning on Hospital Length of Stay
3.4. Influence of Weaning on Shunt Frequency and Timing
3.5. Influence of Weaning on CNS Infection
3.6. Influence of Weaning on Mechanical Drain Complications
4. Discussion
4.1. Summary of Results
4.2. Principal Findings and Interpretation
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dey, M.; Stadnik, A.; Riad, F.; Zhang, L.; McBee, N.; Kase, C.; Carhuapoma, J.R.; Ram, M.; Lane, K.; Ostapkovich, N.; et al. Bleeding and Infection with External Ventricular Drainage: A Systematic Review in Comparison with Adjudicated Adverse Events in the Ongoing Clot Lysis Evaluating Accelerated Resolution of Intraventricular Hemorrhage Phase III (CLEAR-III IHV) Trial. Neurosurgery 2015, 76, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.D.; Puffer, R.; Rabinstein, A.A. Risk factors for hydrocephalus requiring external ventricular drainage in patients with intraventricular hemorrhage. J. Neurosurg. 2015, 123, 1439–1446. [Google Scholar] [CrossRef]
- Lyke, K.E.; Obasanjo, O.O.; Williams, M.A.; O’Brien, M.; Chotani, R.; Perl, T.M. Ventriculitis Complicating Use of Intraventricular Catheters in Adult Neurosurgical Patients. Clin. Infect. Dis. 2001, 33, 2028–2033. [Google Scholar] [CrossRef] [PubMed]
- Roach, J.; Gaastra, B.; Bulters, D.; Shtaya, A. Safety, Accuracy, and Cost Effectiveness of Bedside Bolt External Ventricular Drains (EVDs) in Comparison with Tunneled EVDs Inserted in Theaters. World Neurosurg. 2019, 125, e473–e478. [Google Scholar] [CrossRef] [PubMed]
- Chung, D.Y.; Leslie-Mazwi, T.M.; Patel, A.B.; Rordorf, G.A. Management of External Ventricular Drains After Subarachnoid Hemorrhage: A Multi-Institutional Survey. Neurocrit. Care 2017, 26, 356–361. [Google Scholar] [CrossRef]
- Capion, T.; Lilja-Cyron, A.; Bartek, J.; Forsse, A.; Logallo, N.; Juhler, M.; Mathiesen, T. Discontinuation of External Ventricular Drainage in Patients with Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage—A Scandinavian Multi-institutional Survey. Acta Neurochir. 2020, 162, 1363–1370. [Google Scholar] [CrossRef]
- Connolly, E.S.; Rabinstein, A.A.; Carhuapoma, J.R.; Derdeyn, C.P.; Dion, J.; Higashida, R.T.; Hoh, B.L.; Kirkness, C.J.; Naidech, A.M.; Ogilvy, C.S.; et al. Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage. Stroke 2012, 43, 1711–1737. [Google Scholar] [CrossRef]
- Fried, H.I.; Nathan, B.R.; Rowe, A.S.; Zabramski, J.M.; Andaluz, N.; Bhimraj, A.; Guanci, M.M.; Seder, D.B.; Singh, J.M. The Insertion and Management of External Ventricular Drains: An Evidence-Based Consensus Statement. Neurocrit. Care 2016, 24, 61–81. [Google Scholar] [CrossRef]
- Klopfenstein, J.D.; Kim, L.J.; Feiz-Erfan, I.; Hott, J.S.; Goslar, P.; Zabramski, J.M.; Spetzler, R.F. Comparison of rapid and gradual weaning from external ventricular drainage in patients with aneurysmal subarachnoid hemorrhage: A prospective randomized trial. J. Neurosurg. 2004, 100, 225–229. [Google Scholar] [CrossRef]
- Dey, M.; Jaffe, J.; Stadnik, A.; Awad, I.A. External Ventricular Drainage for Intraventricular Hemorrhage. Curr. Neurol. Neurosci. 2012, 12, 24–33. [Google Scholar] [CrossRef]
- Chau, C.Y.C.; Craven, C.L.; Rubiano, A.M.; Adams, H.; Tülü, S.; Czosnyka, M.; Servadei, F.; Ercole, A.; Hutchinson, P.J.; Kolias, A.G. The Evolution of the Role of External Ventricular Drainage in Traumatic Brain Injury. J. Clin. Med. 2019, 8, 1422. [Google Scholar] [CrossRef] [PubMed]
- Valadka, A.B. Are External Ventricular Drains Better than Parenchymal Intracranial Pressure Monitors in Trauma Patients? World Neurosurg. 2015, 84, 211–213. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Wu, H.; Chen, X.; Feng, J.; Gao, G.; Jiang, J.; Mao, Q. Intracranial Pressure during External Ventricular Drainage Weaning Is an Outcome Predictor of Traumatic Brain Injury. Biomed. Res. Int. 2020, 2020, 8379134. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Sedgwick, P.; Greenwood, N. Understanding the Hawthorne effect. BMJ Br. Med. J. 2015, 351, h4672. [Google Scholar] [CrossRef] [PubMed]
- Chung, D.Y.; Thompson, B.B.; Kumar, M.A.; Mahta, A.; Rao, S.S.; Lai, J.H.; Tadevosyan, A.; Kessler, K.; Locascio, J.J.; Patel, A.B.; et al. Association of External Ventricular Drain Wean Strategy with Shunt Placement and Length of Stay in Subarachnoid Hemorrhage: A Prospective Multicenter Study. Neurocrit. Care 2021, 36, 536–545. [Google Scholar] [CrossRef]
- Jabbarli, R.; Pierscianek, D.; RÖlz, R.; Reinhard, M.; Oppong, M.D.; Scheiwe, C.; Dammann, P.; Kaier, K.; Wrede, K.H.; Shah, M.; et al. Gradual External Ventricular Drainage Weaning Reduces The Risk of Shunt Dependency After Aneurysmal Subarachnoid Hemorrhage: A Pooled Analysis. Oper. Neurosurg. 2018, 15, 498–504. [Google Scholar] [CrossRef]
- Rao, S.S.; Chung, D.Y.; Wolcott, Z.; Sheriff, F.; Khawaja, A.M.; Lee, H.; Guanci, M.M.; Leslie-Mazwi, T.M.; Kimberly, W.T.; Patel, A.B.; et al. Intermittent CSF drainage and rapid EVD weaning approach after subarachnoid hemorrhage: Association with fewer VP shunts and shorter length of stay. J. Neurosurg. 2020, 132, 1583–1588. [Google Scholar] [CrossRef]
- Pandit, A.S.; Palasz, J.; Nachev, P.; Toma, A.K. Mechanical Complications of External Ventricular and Lumbar Drains. World Neurosurg. 2022, 166, e140–e154. [Google Scholar] [CrossRef]
- Parry, S.M.; Puthucheary, Z.A. The impact of extended bed rest on the musculoskeletal system in the critical care environment. Extrem. Physiol. Med. 2015, 4, 16. [Google Scholar] [CrossRef]
- Karic, T.; Røe, C.; Nordenmark, T.H.; Becker, F.; Sorteberg, W.; Sorteberg, A. Effect of early mobilization and rehabilitation on complications in aneurysmal subarachnoid hemorrhage. J. Neurosurg. 2017, 126, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Perry, A.; Graffeo, C.S.; Kleinstern, G.; Carlstrom, L.P.; Link, M.J.; Rabinstein, A.A. Quantitative Modeling of External Ventricular Drain Output to Predict Shunt Dependency in Aneurysmal Subarachnoid Hemorrhage: Cohort Study. Neurocrit. Care 2020, 33, 218–229. [Google Scholar] [CrossRef] [PubMed]
- Park, P.; Garton, H.J.L.; Kocan, M.J.; Thompson, B.G. Risk of Infection with Prolonged Ventricular Catheterization. Neurosurgery 2004, 55, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Camacho, E.F.; Boszczowski, Í.; Basso, M.; Jeng, B.C.P.; Freire, M.P.; Guimarães, T.; Teixeira, M.J.; Costa, S.F. Infection rate and risk factors associated with infections related to external ventricular drain. Infection 2011, 39, 47–51. [Google Scholar] [CrossRef]
- Jamjoom, A.A.B.; Joannides, A.J.; Poon, M.T.-C.; Chari, A.; Zaben, M.; Abdulla, M.A.; Roach, J.; Glancz, L.J.; Solth, A.; Duddy, J.; et al. Prospective, multicentre study of external ventricular drainage-related infections in the UK and Ireland. J. Neurol. Neurosurg. Psychiatry 2018, 89, 120. [Google Scholar] [CrossRef]
- Dakson, A.; Kameda-Smith, M.; Staudt, M.D.; Lavergne, P.; Makarenko, S.; Eagles, M.E.; Ghayur, H.; Guo, R.C.; Althagafi, A.; Chainey, J.; et al. A nationwide prospective multicenter study of external ventricular drainage: Accuracy, safety, and related complications. J. Neurosurg. 2022, 137, 249–257. [Google Scholar] [CrossRef]
| Patients | 69 |
| Total number of drains inserted | 80 |
| Mean age in years (SD) | 59.4 (46.7–72.1) |
| Gender (F/M [%]) | 36/33 [52.1/47.8] |
| Primary pathology (%) | Aneurysmal SAH = 41 (59.4) * Stroke = 15 (21.7) Tumour = 9 (13.0) Non-aneurysmal SAH = 2 (2.9) Meningitis = 2 (2.9) |
| Drain type (%) | Bolt EVD = 48 (69.5) Tunnel EVD = 13 (18.8) Lumbar drain = 8 (11.6) |
| Drainage system (%) | Becker = 46 (66.7) LiquoGuard = 19 (27.5) Mixed = 4 (5.8) |
| Mean consecutive length of drainage (median, range) | 13.3 days (13, 2–25) |
| Wean method (%) | Rapid = 39 (56.5) Gradual = 19 (27.5) Removed = 11 (15.9) |
| Mean duration before first drain clamp (median, range) | 9.9 days (8, 2–22) |
| Number shunted (median time to shunt, range) | 32 (16.5, 2–53 days) |
| Univariate | Multivariate (Adjusted) | ||||||
|---|---|---|---|---|---|---|---|
| Predictor | Outcome | Stat | p | Stat | Coef (CI) | p | |
| LOS | Time to first clamp | Hospital LOS (days) | Rank = 0.34 | <0.01 | t = 2.73 | 1.25 (0.33–2.16) | <0.01 |
| Drain duration (days) | Rank = 0.63 | <0.0001 | - | - | |||
| Shunt | Wean method | Time to shunt (days) | KW = 7.96 | 0.02 | t = −1.93 (removed) | −12.40 (−22.87–−0.73) | 0.06 |
| Time to first clamp | Time to shunt (days) | Rank = 0.36 | 0.04 | t = 2.46 | 1.03 (0.17–1.88) | 0.02 | |
| CNS infection | Wean method | Time to first infection (days) | KW = 11.1 | <0.01 | t = −5.0 (rapid wean) | −6.31 (−9.07–−3.54) | <0.0001 |
| Mechanical complications | Wean method | Number of discrete episodes | MWU = 42 | 0.04 | t = −2.19 (rapid wean) | −0.54 (−1.04–−0.05) | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pandit, A.S.; Palasz, J.; Harris, L.; Nachev, P.; Toma, A.K. Discontinuation of Cerebro-Spinal Fluid (CSF) Drainage in Acute Hydrocephalus: A Prospective Cohort Study and Exploratory Data Analysis. NeuroSci 2024, 5, 396-406. https://doi.org/10.3390/neurosci5040030
Pandit AS, Palasz J, Harris L, Nachev P, Toma AK. Discontinuation of Cerebro-Spinal Fluid (CSF) Drainage in Acute Hydrocephalus: A Prospective Cohort Study and Exploratory Data Analysis. NeuroSci. 2024; 5(4):396-406. https://doi.org/10.3390/neurosci5040030
Chicago/Turabian StylePandit, Anand S., Joanna Palasz, Lauren Harris, Parashkev Nachev, and Ahmed K. Toma. 2024. "Discontinuation of Cerebro-Spinal Fluid (CSF) Drainage in Acute Hydrocephalus: A Prospective Cohort Study and Exploratory Data Analysis" NeuroSci 5, no. 4: 396-406. https://doi.org/10.3390/neurosci5040030
APA StylePandit, A. S., Palasz, J., Harris, L., Nachev, P., & Toma, A. K. (2024). Discontinuation of Cerebro-Spinal Fluid (CSF) Drainage in Acute Hydrocephalus: A Prospective Cohort Study and Exploratory Data Analysis. NeuroSci, 5(4), 396-406. https://doi.org/10.3390/neurosci5040030






