Abstract
Different brain disorders display distinctive etiologies and pathogenic mechanisms. However, they also share pathogenic events. One event systematically occurring in different brain disorders, both acute and chronic, is the increase of the extracellular ATP levels. Accordingly, several P2 (ATP/ADP) and P1 (adenosine) receptors, as well as the ectoenzymes involved in the extracellular catabolism of ATP, have been associated to different brain pathologies, either with a neuroprotective or neurodegenerative action. The P2Y1 receptor (P2Y1R) is one of the purinergic receptors associated to different brain diseases. It has a widespread regional, cellular, and subcellular distribution in the brain, it is capable of modulating synaptic function and neuronal activity, and it is particularly important in the control of astrocytic activity and in astrocyte–neuron communication. In diverse brain pathologies, there is growing evidence of a noxious gain-of-function of P2Y1R favoring neurodegeneration by promoting astrocyte hyperactivity, entraining Ca2+-waves, and inducing the release of glutamate by directly or indirectly recruiting microglia and/or by increasing the susceptibility of neurons to damage. Here, we review the current evidence on the involvement of P2Y1R in different acute and chronic neurodegenerative brain disorders and the underlying mechanisms.
1. Introduction
Different brain disorders display characteristic etiologies and phenotypes, yet they rely on common pathogenic events. One such common event in the development of neurodegeneration is excitotoxicity [1,2] observed both in acute and chronic brain diseases [3,4,5,6]. It involves an abnormal Ca2+-influx, mainly mediated by the high Ca2+-permeable NMDA receptors (NMDARs) [7,8], which then leads to the activation of calpains and other proteases mediating cytoskeleton damage [9] paralleled by oxidative stress, mitochondrial dysfunction, and subsequent activation of apoptotic pathways, events which are also associated with different acute and chronic neurodegenerative conditions [10,11,12,13].
Another event systematically occurring in diverse brain disorders is the increase of the extracellular levels of ATP. ATP is a ubiquitous intracellular metabolite in the millimolar range. Hence, any insult leading to damaged cell membranes of injured or dying cells causes a rapid increase in their extracellular levels. Accordingly, in mechanical injuries such as traumatic brain injury (TBI), there is evidence of increased ATP release [14,15,16,17]. This increase occurs not only proximal to the point of impact [16], but also in remote regions distant to the location of impact [15,17]. This indicates that the increase in extracellular ATP in TBI should reflect not only ATP leakage from injured cells, but also the involvement of mechanisms to release ATP, most likely from astrocytes [15,17,18]. Indeed, besides ATP leakage from dying cells, there are physiological mechanisms designed to active-release ATP, which are also observed in pathophysiological phenomena. ATP can be released or co-released from nerve terminals [19] in an activity and Ca2+-dependent exocytotic vesicular manner [20]. This occurs particularly at high-frequency stimulations [21,22,23], which suggests that this neuronal activity-dependent release of ATP may be contributing to seizure-induced ATP release [24,25]. Recently, we showed an increase in the evoked release of ATP from rat hippocampal nerve terminals 7 days upon the induction of status epilepticus (SE) [26]. In metabolic stress such as hypoxia or ischemia, the observed increase in ATP release [27,28,29] also seems to have a neuronal source [30]. Moreover, recently, it was shown that the i.c.v. injection of Aβ1–42, which is associated to Alzheimer’s disease (AD), increases the evoked release of ATP from mice hippocampal nerve terminals, as well [31]. Extracellular ATP may also arise from astrocytes, perhaps the major source of extracellular ATP, through a Ca2+-dependent vesicular release by exocytosis [32,33,34], by lysosomes [35], or through hemichannels formed by either pannexins [36,37,38] or connexins [39,40]. Aβ exposure promotes the release of ATP by astrocytes [41,42,43] through hemichannels, in particular, connexin-43 [41,43]. In a mouse model of familial AD, astrocytic hyperactivity was shown to be mediated by paracrine purinergic signaling involving connexin channels [44]. Pannexins have been also reported to be involved in neurotoxicity, namely, in ischemia [45], and has been proposed as a target for neuroprotection [46]. Accordingly, the increase of extracellular ATP during high-potassium-induced ictal discharges on slices obtained from resected tissues of TLE patients was blocked by the inhibition of pannexin-1, which also provided anticonvulsive effects in a mouse model of kainic acid (KA)-induced seizures [47]. This may involve astrocytic pannexin-1 [48]. Notably, neuronal pannexin-1 has also been shown to be activated during ischemia and may constitute an additional neuronal source of pathological extracellular ATP [49]. ATP release from astrocytes can also be mediated by maxi-anion channels as observed in oxygen–glucose deprivation [50]. Extracellular ATP may further arise through P2X7R, either directly through the high-permeability pore formed by prolonged P2X7R activation [51,52] or by a synergistic interaction with pannexins [53,54], suggesting a self-mechanism of sustained increase in the extracellular levels of ATP. In addition to neurons and astrocytes, microglia may also contribute to the release of ATP in pathological conditions, eventually through vesicular exocytosis [55]. For instance, in mouse primary microglial cells, fibrillar and oligomeric Aβ1–42 cause ATP release [56]; and in microglial N13 cells, the active Aβ25–35 peptide causes a dose-dependent release of ATP [57].
Thus, there is now compelling evidence demonstrating a sustained efflux of ATP into the extracellular milieu in brain disorders either through the leak of ATP through damaged membranes, or through mechanisms designed to active-release ATP in pathological phenomena. This supports the concept that extracellular ATP is a danger signal in the brain [58,59], constituting another event shared by different acute and brain disorders. Accordingly, several P2 receptors (P2R) and P1 receptors (P1R) were activated by adenosine upon the extracellular catabolism of ATP, and the respective ectoenzymes have been associated to different brain pathologies, either with neuroprotective or neurodegenerative actions (for review, see e.g., [59,60,61,62,63,64,65,66]). Here, we will review in particular the current knowledge on the contribution of the P2Y1 receptor (P2Y1R) to neurodegeneration in different acute and brain disorders and discuss the underlying mechanisms.
2. The Multimodal P2Y1 Receptor
P2Y1R is a metabotropic receptor activated by ATP/ADP with a widespread regional cellular and subcellular distribution in the brain. In neurons, P2Y1R is located both pre- and postsynaptically [67] and non-synaptically both in dendrites, cell bodies, and axons [68]. Presynaptic P2Y1R modulates neurotransmitter release such as glutamate [67,69] or GABA [70], eventually through its ability to regulate N-type Ca2+-channels in neurons [71,72]. Postsynaptically, P2Y1R inhibits NMDAR [73], impacting the synaptic plasticity [74]. This may also rely on the inhibition of voltage-gated Ca2+- channels [75]. Recently, we have shown in cultured rat hippocampal neurons that P2Y1R modulates the NMDA-induced Ca2+-entry in a bidirectional and subcellular-specific manner, decreasing it in the soma and dendrites and increasing it in the axons, most likely reflecting a differential regulation of NMDARs’ density in the different cellular compartments [68]. P2Y1R also regulates GABA transmission by postsynaptic regulation of GABAA receptors [76] and through the direct control of interneurons’ excitability in different regions [76,77,78,79,80], involving the regulation of K+-conductance [77,79,80]. P2Y1R can also promote rat hippocampal pyramidal neurons’ excitability through the inhibition of M-type K+-currents [81]. In astrocytes, P2Y1Rs are also highly expressed [44,82,83,84,85], playing a key role in the propagation of calcium waves throughout the astrocytic network [34,86,87]. P2Y1R also regulates Ca2+-dependent vesicular glutamate release from astrocytes [88], which is able to activate NMDAR on neurons [83] and modulate neuronal function [80,83,89,90]. It also regulates the release of ATP from astrocytes [91], sustaining an autocrine ATPergic signaling [90] and modulating synaptic function [92]. P2Y1R also controls GABA uptake from cultured rat cortical astrocytes [93]. Hence, P2Y1R regulates astrocytic function, modulating astrocytic network activity and gliotransmission. The expression of P2Y1R has been also reported in microglia [94,95,96]. While motility seems to be associated with P2Y12R [97,98], microglia process retraction may involve P2Y1R [99]. Altogether, the multiple functions so far ascribed to P2Y1R set a transcellular integrative role for P2Y1R in the brain.
3. P2Y1 Receptor in Neurodegenerative Disorders
An increase in the expression levels of P2Y1R has been documented in different acute or chronic neurological disorders such as epilepsy [100,101,102], mechanical injury [103], ischemia [84], or AD [44,104], which suggests the gain of a noxious function of P2Y1R. Accordingly, compelling evidence have been associating P2Y1R with different acute and chronic brain disorders.
In ischemic conditions such as oxygen–glucose deprivation (OGD), the blockade of P2Y1R prevented the depression of field excitatory postsynaptic potentials and anoxic depolarization in rat hippocampal slices, also preventing CA1 pyramidal neuronal damage [105,106]. Similar neuroprotection was afforded by the i.c.v. administration of a selective antagonist of P2Y1R after transient middle cerebral artery occlusion in rats, reducing infarct volume and recovering motor coordination [84]. Moreover, P2Y1R-KO mice displayed reduced hippocampal damage and no cognitive decline upon middle cerebral artery occlusion, an effect mimicked by the pharmacological blockade of P2Y1R in rodents [107]. This has been associated to the control of astrocytic function and glial neuroinflammatory response [84,107,108]. However, neuronal mechanisms should also be involved in the deleterious contribution of P2Y1R in ischemic conditions since in another study, it was observed that P2Y1R blockade attenuated neuronal damage and cognitive performance induced by permanent middle cerebral artery occlusion, without inhibiting the astrocytic or microglial reactivity [109]. On the other hand, a neuroprotective action of P2Y1R has been also reported in ischemia. P2Y1R-KO mice displayed a higher number of injured hippocampal neurons upon OGD [110] and in mouse ischemic models of photo-thrombolysis, a reduction of neuronal damage was observed with the activation of astrocytic P2Y1R [111,112]. A similar neuroprotection provided by astrocytic P2Y1R was observed in oxidative stress through IL-6 release [113]. A neuroprotective vs. neurodegenerative action of P2Y1R may be due to either the degree of P2Y1R-driven activity and/or a time-dependent gain of a noxious function of P2Y1R, shifting astrocytes from a supportive role to a deleterious impact and/or a time-dependent differential impact of neuronal and glial P2Y1R. A similar time-dependent shift from a neuroprotective to a neurodegenerative input of P2Y1R was observed in excitotoxicity. P2Y1R was shown to be required for glutamate-induced synaptic loss and subsequent neuronal death in the rat hippocampus both in vitro and in vivo [68]. This is due at least in part to a P2Y1R-driven increase of NMDARs at the axon, leading to a deleterious Ca2+-entry and subsequent calpain-mediated axonal cytoskeleton damage [68]. However, it also provided evidence that P2Y1R may reduce AMPAR, decreasing the susceptibility of neurons to excitotoxicity [114]. In SE-induced neurodegeneration, the i.c.v. injection of a selective antagonist of P2Y1R reduced hippocampal neuronal death observed with the systemic i.p. administration of KA [68]. However, in a more recent study, it was detailed that there is a time-dependent shift from a neuroprotective to a neurodegenerative contribution of P2Y1R to SE-induced neurodegeneration, correlated with a different impact in SE-induced seizure activity. Using intra-amygdala KA and pilocarpine mouse models, while the antagonism of P2Y1R before SE induction increased seizure activity and neurodegeneration in the hippocampus, the blockade of P2Y1R shortly after the onset of SE reduced seizure activity and degeneration [115]. It was suggested that this may be due to a time-dependent contribution of neuronal and astrocytic P2Y1R [115]. Neuronal P2Y1R can reduce hyperexcitability, either by directly depressing postsynaptic NMDARs [68,73] and/or by a circuit-driven increase of the inhibitory tonus [77,78]; however, then the recruitment of astrocytes and the P2Y1R-induced release of glutamate [88], subsequently activating NMDAR on neurons [83], can lead to hyperexcitability [66,90,116,117]. In addition, this time-dependent neuroprotective to neurodegenerative shift may also be due to the fact that the contribution of neuronal and astrocytic P2Y1Rs may also change at different pathogenic stages. For instance, neuronal P2Y1R tonically depresses dendritic NMDARs, but in excitotoxic conditions, it induces a toxic increase in axonal NMDARs [68]. Interestingly, a similar P2Y1R-driven increase in NMDARs was found in the dorsal root ganglion underlying remifentanil-induced postoperative hyperalgesia [118]. However, this contribution of neuronal P2Y1R to neurodegeneration fades with more intense excitotoxic conditions [68]. Regarding the contribution of astrocytic P2Y1R, astrocytes have a physiological supportive role to neuronal function, namely, glutamate uptake or the release of neurotrophic factors [119] and, as mentioned, astrocytic P2Y1R can have a neuroprotective effect as observed in ischemia, oxidative stress [111,112,113], and TBI (see below) [120]. Nevertheless, the evidence so far provided essentially point to a net neurodegenerative contribution of P2Y1R in excitotoxic conditions. There is an increased density of P2Y1R upon SE as well as in human tissue from temporal lobe epilepsy patients [101,102], supporting microglia and astrocytic-induced hyperexcitability through the P2Y1R-induced release of glutamate from astrocytes [102,116,121]. This is further heralded by the observation that the blockade of P2Y1R post-SE delayed the onset of epilepsy and suppressed epileptic seizures in a reversible manner [115]. In addition to a control of seizure severity, the antagonism of P2Y1R may be also beneficial against epilepsy comorbidities since the blockade of P2Y1R rescued synaptic plasticity, associated to a normalization of astroglial Ca2+-activity in epileptic hippocampus [121]
The blockade of P2Y1Rs also afforded neuroprotection upon TBI even in remote regions from the injury site, improving cognitive outcomes [15]. This effect was dependent on P2Y1R-mediated astrocytic Ca2+-waves and on NMDAR activation [15], indicating an exacerbation/propagation of neuronal injury through a P2Y1R-driven release of glutamate from astrocytes. This is further sustained by the release of ATP in regions distant to the impact point [17]. In addition to having control of astrocytes, it was more recently shown that the blockade of P2Y1R suppressed microglial activation at the injury site [122]. Moreover, evidence was provided that microglia recruited to the injury core is important for the formation of neuroprotective astrocyte scar in the peri-injured region by downregulating P2Y1R in astrocytes [120]. Hence, the neuroprotection afforded by the inhibition of P2Y1R in TBI may be due by the concomitant promotion of a protective scar around the lesion, mimicking the beneficial effects of microglia but inhibiting the microglia-mediated inflammatory response and avoiding the astrocytic-driven hyperexcitability involved in the exacerbation and propagation of neuronal injury.
In AD, P2Y1Rs were found to colocalize with neurofibrillary tangles and amyloid β (Aβ) plaques characteristic to AD [104]. In an APP/PS1 AD mouse model, reactive astrocytes near Aβ plaques showed enhanced P2Y1R-mediated Ca2+ signaling, displaying both significantly higher resting Ca2+ levels and increased propagation of intercellular Ca2+-waves [44], and was suggested to mediate Aβ-induced synaptic dysfunction/loss and neuronal damage [44,123]. Indeed, more recently, it was shown that the chronic blockade of P2Y1R in the APP/PS1 mice reduced/normalized neuronal activity, restored synaptic plasticity and synaptic integrity, reduced neuritic dystrophy, and attenuated cognitive decline [124]. The observation that this was partly observed in mice lacking the IP3 receptor type 2, the signaling downstream of P2Y1R activation, indicates that it is in part due to the inhibition of the astrocytic hyperactivity, similar to that observed in epileptic hippocampus [121]. However, it also indicates that P2Y1Rs other than those located in astrocytes could also be involved. In fact, neuronal P2Y1R may also contribute to the initial synaptic dysfunction/loss by favoring the loss of axonal integrity, observed prior to dendritic damage and later neuronal death through an increase in NMDARs [68]. Besides, additional mechanisms may underlie the contribution of P2Y1R to AD-associated synaptic dysfunction, plasticity deficits, and cognitive impairment, eventually abnormally activated by astrocytic-derived ATP [80,92]. The depression of postsynaptic NMDARs [73,74,75] was shown to have an impact in synaptic plasticity, particularly in pathological conditions such as hypoxia [75]. The selective activation of P2Y1R in the medial prefrontal cortex was shown to be sufficient to impair working memory and learning [125]. In addition, the recently shown Aβ-associated disruption of inhibitory homeostasis mediated by P2Y1R [126] may also promote circuit-driven synaptic dysfunction.
In summary, there is now compelling evidence associating P2Y1R to different acute and chronic neurodegenerative disorders with clear distinctive etiologies and pathogenesis, essentially pointing towards a pro-neurodegenerative action.
4. P2Y1 Receptor as a Catalyst of Neurodegeneration
The major mechanism by which P2Y1R favors neurodegeneration, shared by different brain disorders, is its ability to control astrocytic function, thus entraining Ca2+-waves, inducing the release of inflammatory cytokines [84], and promoting the release of glutamate [15,88,102,116,121], ultimately leading to hyperexcitability and neuronal damage [66,83,90,116,117]. P2Y1R inhibition is also neuroprotective by allowing the development of neuroprotective astrocytic scars, namely in TBI [120]. These deleterious mechanisms of astrocytic P2Y1R are further sustained/enhanced by P2Y1R itself due to its ability to prevent astrocytic damage upon different noxious insults [63,127,128,129] and by mediating the autocrine signaling, inducing a sustained release of ATP from astrocytes [17,44,91,116,130]. This mechanism can be also sustained or potentiated by microglia recruitment through the release of ATP and subsequent P2Y1R-driven stimulation of astrocytes, promoting glutamatergic gliotransmission with an impact in synaptic activity [85], tethering inflammation to synaptic failure. Besides, although the role of P2Y1R in microglia remains elusive, it has been shown that, either directly or indirectly, P2Y1R is involved in the recruitment of microglia in epileptic phenomena [102] in TBI [122] and in ischemia [107]. In addition, neuronal P2Y1R may also contribute to neurodegeneration [68,109], namely, by favoring the initial synaptic loss and later neuronal death by a subcellular-specific upregulation of NMDARs, increasing their density in axons, leading to an initial Ca2+-driven calpain-mediated axonal cytoskeleton damage [68]. Altogether, the ability of P2Y1R to promote astrocyte hyperactivity and consequent glutamate release, to recruit and eventually format microglia response, and to directly increase the susceptibility of neurons to damage, indicate that P2Y1R is endowed with a transcellular capability to catalyze neurodegeneration in different brain disorders (Figure 1), both at the early onset [68,115] and at a chronic stage [44,115,124].
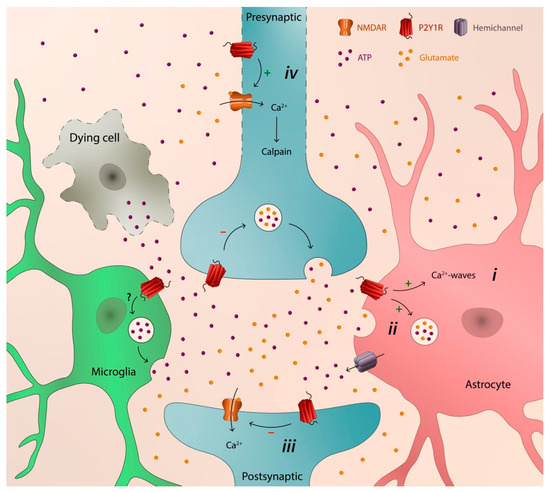
Figure 1.
Schematic illustration depicting the transcellular capability of P2Y1R to catalyze neurodegeneration: (i) astrocytic hyperactivity; (ii) release of glutamate from astrocytes; (iii) depression of synaptic activity; and (iv) early axonal degeneration, synaptic loss, and later neuronal death.
The contribution of the purinergic signaling system to brain pathologies is not limited to P2Y1R. Other P2Rs, adenosine P1Rs, or ectoenzymes involved in the extracellular metabolism of ATP have been associated to the pathogenesis of different brain disorders, displaying both neurodegenerative actions, namely P2X7R, A2AR, and CD73 [59,62,64], and neuroprotective actions such as with P2Y2, P2Y4, P2Y12, and P2Y13 receptors (e.g., [63,65,131,132]). Hence, in order to fully comprehend the pathological contribution of P2Y1R to brain disorders and its potential value as a therapeutic target, it is fundamental to contextualize it within the purinergic signaling system. It will be important to understand the hierarchy, cooperation, and/or redundancy between the different elements that comprise the purinergic signaling system and understand how the contribution of purinergic signaling in pathological conditions is orchestrated. Some studies started to shed light on this topic. Besides the contribution of different purinergic receptors to the release of ATP such as P2X7R or A2AR [43,51,52,59], microglia P2Y13R prevents astrocyte proliferation induced by P2Y1R [133], and more recently, it was shown that A2AR physiologically reduces P2Y1R-driven Ca2+ increases in astrocytes, an effect blunted by Aßexposure [134]. This will allow a better comprehension of the contribution of P2Y1R to neurodegeneration, which is fundamental to define an eventual therapeutic strategy targeting P2Y1R, either directly or indirectly, to prevent its deleterious contribution. This may involve a multitarget time-dependent strategy. Since a sustained ATP release and the pathogenic involvement of P2Y1R is an event shared by different acute and chronic brain disorders, such a strategy targeting P2Y1R function may bring a sole therapeutic intervention to the different neurodegenerative disorders.
Author Contributions
Conceptualization, R.J.R. and J.M.M.; writing—original draft preparation, R.J.R., A.S.F. and J.M.M.; writing—review and editing, R.J.R. and J.M.M.; funding acquisition, R.J.R. and J.M.M.; figure, R.J.R. and A.S.F. All authors have read and agreed to the published version of the manuscript.
Funding
The research activity of the authors has been supported by funding from the European Regional Development Fund (ERDF), through the Centro 2020 Regional Operational Programme under the project CENTRO-01-0145-FEDER-000008 (BrainHealth2020), and through the COMPETE 2020-Operational Programme for Competitiveness and Internationalization and Portuguese national funds via FCT—Fundação para a Ciência e Tecnologia, under the projects POCI-01-0145-FEDER-028160 (to J.M.M), UIDB/04539/2020, UIDP/04539/2020 and LA/P/0058/2020; and by Alzheimer Association under the project NIRG-15-361884 granted to R.J.R.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Olney, J.W. Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate. Science 1969, 164, 719–721. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.W. Glutamate neurotoxicity in cortical cell culture is calcium dependent. Neurosci. Lett. 1985, 58, 293–297. [Google Scholar] [CrossRef]
- Lipton, S.A.; Rosenberg, P.A. Excitatory amino acids as a final common pathway for neurologic disorders. N. Engl. J. Med. 1994, 330, 613–622. [Google Scholar] [PubMed]
- Ikonomidou, C.; Turski, L. Excitotoxicity and neurodegenerative diseases. Curr. Opin. Neurol. 1995, 8, 487–497. [Google Scholar] [CrossRef]
- Dong, X.X.; Wang, Y.; Qin, Z.H. Molecular mechanisms of excitotoxicity and their relevance to pathogenesis of neurodegenerative diseases. Acta Pharmacol. Sin. 2009, 30, 379–387. [Google Scholar] [CrossRef]
- Lewerenz, J.; Maher, P. Chronic Glutamate Toxicity in Neurodegenerative Diseases-What is the Evidence? Front. Neurosci. 2015, 9, 469. [Google Scholar] [CrossRef]
- Choi, D.W. Calcium and excitotoxic neuronal injury. Ann. N. Y. Acad. Sci. 1994, 747, 162–171. [Google Scholar] [CrossRef]
- Rothman, S.M.; Olney, J.W. Excitotoxicity and the NMDA receptor–still lethal after eight years. Trends Neurosci. 1995, 18, 57–58. [Google Scholar]
- Vanderklish, P.W.; Bahr, B.A. The pathogenic activation of calpain: A marker and mediator of cellular toxicity and disease states. Int. J. Exp. Pathol. 2000, 81, 323–339. [Google Scholar] [CrossRef]
- Dawson, V.L.; Dawson, T.M. Deadly conversations: Nuclear-mitochondrial cross-talk. J. Bioenerg. Biomembr. 2004, 36, 287–294. [Google Scholar] [CrossRef]
- Uttara, B.; Singh, A.V.; Zamboni, P.; Mahajan, R.T. Oxidative stress and neurodegenerative diseases: A review of upstream and downstream antioxidant therapeutic options. Curr. Neuropharmacol. 2009, 7, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Sheng, M. NMDA receptors in nervous system diseases. Neuropharmacology 2013, 74, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Yildiz-Unal, A.; Korulu, S.; Karabay, A. Neuroprotective strategies against calpain-mediated neurodegeneration. Neuropsychiatr. Dis. Treat. 2015, 11, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Davalos, D.; Grutzendler, J.; Yang, G.; Kim, J.V.; Zuo, Y.; Jung, S.; Littman, D.R.; Dustin, M.L.; Gan, W.B. ATP mediates rapid microglial response to local brain injury in vivo. Nat. Neurosci. 2005, 8, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Choo, A.M.; Miller, W.J.; Chen, Y.C.; Nibley, P.; Patel, T.P.; Goletiani, C.; Morrison, B., 3rd; Kutzing, M.K.; Firestein, B.L.; Sul, J.Y.; et al. Antagonism of purinergic signalling improves recovery from traumatic brain injury. Brain 2013, 136, 65–80. [Google Scholar] [CrossRef]
- Faroqi, A.H.; Lim, M.J.; Kee, E.C.; Lee, J.H.; Burgess, J.D.; Chen, R.; Di Virgilio, F.; Delenclos, M.; McLean, P.J. In vivo detection of extracellular adenosine triphosphate in a mouse model of traumatic brain injury. J. Neurotrauma 2021, 38, 655–664. [Google Scholar] [CrossRef]
- Moro, N.; Ghavim, S.S.; Sutton, R.L. Massive efflux of adenosine triphosphate into the extracellular space immediately after experimental traumatic brain injury. Exp. Ther. Med. 2021, 21, 575. [Google Scholar] [CrossRef]
- Koizumi, S.; Fujishita, K.; Tsuda, M.; Shigemoto-Mogami, Y.; Inoue, K. Dynamic inhibition of excitatory synaptic transmission by astrocyte-derived ATP in hippocampal cultures. Proc. Natl. Acad. Sci. USA 2003, 100, 11023–11028. [Google Scholar] [CrossRef]
- White, T.D. Direct detection of depolarisation-induced release of AYP from a synaptosomal preparation. Nature 1977, 267, 67–68. [Google Scholar] [CrossRef]
- Pankratov, Y.; Lalo, U.; Verkhratsky, A.; North, R.A. Vesicular release of aTP at central synapses. Pflugers Arch. 2006, 452, 589–597. [Google Scholar] [CrossRef]
- Wieraszko, A.; Goldsmith, G.; Seyfried, T.N. Stimulation-dependent release of adenosine triphosphate from hippocampal slices. Brain Res. 1989, 485, 244–250. [Google Scholar] [CrossRef]
- Cunha, R.A.; Correia-de-Sá, P.; Sebastião, A.M.; Ribeiro, J.A. Preferential activation of excitatory adenosine receptors at rat hippocampal and neuromuscular synapses by adenosine formed from released adenine nucleotides. Br. J. Pharmacol. 1996, 119, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Rebola, N.; Lujan, R.; Cunha, R.A.; Mulle, C. Adenosine A2A receptors are essential for long-term potentiation of NMDA-EPSCs at hippocampal mossy fiber synapses. Neuron 2008, 57, 121–134. [Google Scholar] [CrossRef] [PubMed]
- Wieraszko, A.; Seyfried, T.N. ATP-induced synaptic potentiation in hippocampal slices. Brain Res. 1989, 491, 356–359. [Google Scholar] [CrossRef]
- Dale, N.; Frenguelli, B.G. Release of adenosine and ATP during ischemia and epilepsy. Curr. Neuropharmacol. 2009, 7, 160–179. [Google Scholar] [CrossRef]
- Xu, X.; Beleza, R.O.; Gonçalves, F.Q.; Valbuena, S.; Alçada-Morais, S.; Gonçalves, N.; Magalhães, J.; Rocha, J.M.M.; Ferreira, S.; Figueira, A.S.G.; et al. Adenosine A2A receptors control synaptic remodeling in the adult brain. Sci. Rep. 2022, 12, 14690. [Google Scholar] [CrossRef]
- Lutz, P.L.; Kabler, S. Release of adenosine and ATP in the brain of the freshwater turtle (Trachemys Scripta) during long-term anoxia. Brain Res. 1997, 769, 281–286. [Google Scholar] [CrossRef]
- Juranyi, Z.; Sperlagh, B.; Vizi, E.S. Involvement of P2 purinoceptors and the nitric oxide pathway in [3H] purine outflow evoked by short-term hypoxia and hypoglycemia in rat hippocampal slices. Brain Res. 1999, 823, 183–190. [Google Scholar] [CrossRef]
- Melani, A.; Turchi, D.; Vannucchi, M.G.; Cipriani, S.; Gianfriddo, M.; Pedata, F. ATP extracellular concentrations are increased in the rat striatum during in vivo ischemia. Neurochem. Int. 2005, 47, 442–448. [Google Scholar] [CrossRef]
- Frenguelli, B.G.; Wigmore, G.; Llaudet, E.; Dale, N. Temporal and mechanistic dissociation of ATP and adenosine release during ischaemia in the mammalian hippocampus. J. Neurochem. 2007, 101, 1400–1413. [Google Scholar] [CrossRef]
- Gonçalves, F.Q.; Lopes, J.P.; Silva, H.B.; Lemos, C.; Silva, A.C.; Gonçalves, N.; Tomé, A.R.; Ferreira, S.G.; Canas, P.M.; Rial, D.; et al. Synaptic and memory dysfunction in a β-amyloid model of early Alzheimer’s disease depends on increased formation of ATP-derived extracellular adenosine. Neurobiol. Dis. 2019, 132, 104570. [Google Scholar] [CrossRef] [PubMed]
- Coco, S.; Calegari, F.; Pravettoni, E.; Pozzi, D.; Taverna, E.; Rosa, P.; Matteoli, M.; Verderio, C. Storage and release of ATP from astrocytes in culture. J. Biol. Chem. 2003, 278, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Montana, V.; Malarkey, E.B.; Verderio, C.; Matteoli, M.; Parpura, V. Vesicular transmitter release from astrocytes. Glia 2006, 54, 700–715. [Google Scholar] [CrossRef] [PubMed]
- Bowser, D.N.; Khakh, B.S. Vesicular ATP is the predominant cause of intercellular calcium waves in astrocytes. J. Gen. Physiol. 2007, 129, 485–491. [Google Scholar] [CrossRef]
- Zhang, Z.; Chen, G.; Zhou, W.; Song, A.; Xu, T.; Luo, Q.; Wang, W.; Gu, X.S.; Duan, S. Regulated ATP release from astrocytes through lysosome exocytosis. Nat. Cell Biol. 2007, 9, 945–953. [Google Scholar] [CrossRef]
- Iwabuchi, S.; Kawahara, K. Functional significance of the negative-feedback regulation of ATP release via pannexin-1 hemichannels under ischemic stress in astrocytes. Neurochem. Int. 2011, 58, 376–384. [Google Scholar] [CrossRef]
- Bao, L.; Sachs, F.; Dahl, G. Connexins are mechanosensitive. Am. J. Physiol. Cell Physiol. 2004, 287, C1389–C1395. [Google Scholar] [CrossRef]
- Reigada, D.; Lu, W.; Zhang, M.; Mitchell, C.H. Elevated pressure triggers a physiological release of ATP from the retina: Possible role for pannexin hemichannels. Neuroscience 2008, 157, 396–404. [Google Scholar] [CrossRef][Green Version]
- Cotrina, M.L.; Lin, J.H.; López-García, J.C.; Naus, C.C.; Nedergaard, M. ATP-mediated glia signaling. J. Neurosci. 2000, 20, 2835–2844. [Google Scholar] [CrossRef]
- Stout, C.E.; Constantin, J.L.; Naus, C.C.G.; Charles, A.C. Intercellular calcium signaling in astrocytes via ATP release through connexin hemichannels. J. Biol. Chem. 2002, 277, 10482–10488. [Google Scholar] [CrossRef]
- Orellana, J.A.; Shoji, K.F.; Abudara, V.; Ezan, P.; Amigou, E.; Saez, P.J.; Jiang, J.X.; Naus, C.C.; Saez, J.C.; Giaume, C. Amyloid β-induced death in neurons involves glial and neuronal hemichannels. J. Neurosci. 2011, 31, 4962–4977. [Google Scholar] [CrossRef] [PubMed]
- Jung, E.S.; An, K.; Hong, S.H.; Kim, J.-H.; Mook-Jung, I. Astrocyte-originated ATP protects Aβ1-42-induced impairment of synaptic plasticity. J. Neurosci. 2012, 32, 3081–3087. [Google Scholar] [CrossRef] [PubMed]
- Madeira, D.; Dias, L.; Santos, P.; Cunha, R.A.; Canas, P.M.; Agostinho, P. Association between adenosine A2A receptors and connexin 43 regulates hemichannels activity and ATP release in astrocytes exposed to amyloid-β peptides. Mol. Neurobiol. 2021, 58, 6232–6248. [Google Scholar] [CrossRef] [PubMed]
- Delekate, A.; Fuchtemeier, M.; Schumacher, T.; Ulbrich, C.; Foddis, M.; Petzold, G.C. Metabotropic P2Y1 receptor signalling mediates astrocytic hyperactivity in vivo in an alzheimer’s disease mouse model. Nat. Commun. 2014, 5, 5422. [Google Scholar] [CrossRef]
- Vessey, D.A.; Li, L.; Kelley, M. P2X7 receptor agonists pre- and postcondition the heart against ischemia-reperfusion injury by opening pannexin-1/P2X7 channels. Am. J. Physiol. Heart Circ. Physiol. 2011, 301, H881–H887. [Google Scholar] [CrossRef]
- Shestopalov, V.I.; Slepak, V.Z. Molecular pathways of pannexin1-mediated neurotoxicity. Front. Physiol. 2014, 5, 23. [Google Scholar] [CrossRef][Green Version]
- Dossi, E.; Blauwblomme, T.; Moulard, J.; Chever, O.; Vasile, F.; Guinard, E.; Le Bert, M.; Couillin, I.; Pallud, J.; Capelle, L.; et al. Pannexin-1 channels contribute to seizure generation in human epileptic brain tissue and in a mouse model of epilepsy. Sci. Transl. Med. 2018, 10, eaar3796. [Google Scholar] [CrossRef]
- Wellmann, M.; Álvarez-Ferradas, C.; Maturana, C.J.; Sáez, J.C.; Bonansco, C. Astroglial Ca2+-dependent hyperexcitability requires P2Y1 purinergic receptors and pannexin-1 channel activation in a chronic model of epilepsy. Front. Cell Neurosci. 2018, 12, 446. [Google Scholar] [CrossRef]
- Thompson, R.J.; Zhou, N.; MacVicar, B.A. Ischemia opens neuronal gap junction hemichannels. Science 2006, 312, 924–927. [Google Scholar] [CrossRef]
- Liu, H.T.; Sabirov, R.Z.; Okada, Y. Oxygen-glucose deprivation induces ATP release via maxi-anion channels in astrocytes. Purinergic Signal. 2008, 4, 147–154. [Google Scholar] [CrossRef]
- Duan, S.; Neary, J.T. P2X7 receptors: Properties and relevance to CNS function. Glia 2006, 54, 738–746. [Google Scholar] [CrossRef] [PubMed]
- Cisneros-Mejorado, A.; Pérez-Samartín, A.; Gottlieb, M.; Matute, C. ATP signaling in brain: Release, excitotoxicity and potential therapeutic targets. Cell. Mol. Neurobiol. 2015, 35, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Locovei, S.; Scemes, E.; Qiu, F.; Spray, D.C.; Dahl, G. Pannexin1 is part of the pore forming unit of the P2X(7) receptor death complex. FEBS Lett. 2007, 581, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Iglesias, R.; Locovei, S.; Roque, A.; Alberto, A.P.; Dahl, G.; Spray, D.C.; Scemes, E. P2X7 receptor-pannexin1 complex: Pharmacology and signaling. Am. J. Physiol. Cell Physiol. 2008, 295, C752–C760. [Google Scholar] [CrossRef] [PubMed]
- Imura, Y.; Morizawa, Y.; Komatsu, R.; Shibata, K.; Shinozaki, Y.; Kasai, H.; Moriishi, K.; Moriyama, Y.; Koizumi, S. Microglia release ATP by exocytosis. Glia 2013, 61, 1320–1330. [Google Scholar] [CrossRef]
- Kim, S.Y.; Moon, J.H.; Lee, H.G.; Kim, S.U.; Lee, Y.B. ATP released from beta-amyloid-stimulated microglia induces reactive oxygen species production in an autocrine fashion. Exp. Mol. Med. 2007, 39, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Sanz, J.M.; Chiozzi, P.; Ferrari, D.; Colaianna, M.; Idzko, M.; Falzoni, S.; Fellin, R.; Trabace, L.; Di Virgilio, F. Activation of microglia by amyloid {beta} requires P2X7 receptor expression. J. Immunol. 2009, 182, 4378–4385. [Google Scholar] [CrossRef]
- Di Virgilio, F. Dr. Jekyll/Mr. Hyde: The dual role of extracellular ATP. J. Auton. Nerv. Syst. 2000, 81, 59–63. [Google Scholar] [CrossRef]
- Rodrigues, R.J.; Tomé, A.R.; Cunha, R.A. ATP as a multi-target danger signal in the brain. Front. Neurosci. 2015, 9, 148. [Google Scholar] [CrossRef]
- Burnstock, G.; Krügel, U.; Abbracchio, M.P.; Illes, P. Purinergic signalling: From normal behaviour to pathological brain function. Prog. Neurobiol. 2011, 95, 229–274. [Google Scholar] [CrossRef]
- Weisman, G.A.; Ajit, D.; Garrad, R.; Peterson, T.S.; Woods, L.T.; Thebeau, C.; Camden, J.M.; Erb, L. Neuroprotective roles of the P2Y(2) receptor. Purinergic Signal. 2012, 8, 559–578. [Google Scholar] [CrossRef] [PubMed]
- Illes, P. P2X7 receptors amplify CNS damage in neurodegenerative diseases. Int. J. Mol. Sci. 2020, 21, 5996. [Google Scholar] [CrossRef]
- Forster, D.; Reiser, J. Supportive or detrimental roles of P2Y receptors in brain pathology?—The two faces of P2Y receptors in stroke and neurodegeneration detected in neural cell and in animal model studies. Purinergic Signal. 2015, 11, 441–454. [Google Scholar] [CrossRef] [PubMed]
- Cunha, R.A. How does adenosine control neuronal dysfunction and neurodegeneration? J. Neurochem. 2016, 139, 1019–1055. [Google Scholar] [CrossRef]
- Miras-Portugal, M.T.; Queipo, M.J.; Gil-Redondo, J.C.; Ortega, F.; Gómez-Villafuertes, R.; Gualix, J.; Delicado, E.G.; Pérez-Sen, R. P2 receptor interaction and signalling cascades in neuroprotection. Brain Res. Bull. 2019, 151, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Engel, T.; Smith, J.; Alves, M. Targeting neuroinflammation via purinergic P2 receptors for disease modification in drug-refractory epilepsy. J. Inflamm. Res. 2021, 14, 3367–3392. [Google Scholar] [CrossRef]
- Rodrigues, R.J.; Almeida, T.; Richardson, P.J.; Oliveira, C.R.; Cunha, R.A. Dual presynaptic control by ATP of glutamate release via facilitatory P2X1, P2X2/3, and P2X3 and inhibitory P2Y1, P2Y2, and/or P2Y4 receptors in the rat hippocampus. J. Neurosci. 2005, 25, 6286–6295. [Google Scholar] [CrossRef]
- Simões, A.P.; Silva, C.G.; Marques, J.M.; Pochmann, D.; Porciúncula, L.O.; Ferreira, S.; Oses, J.P.; Beleza, R.O.; Real, J.I.; Köfalvi, A.; et al. Glutamate-induced and NMDA receptor-mediated neurodegeneration entails P2Y1 receptor activation. Cell Death Dis. 2018, 9, 297. [Google Scholar] [CrossRef]
- Mendoza-Fernandez, V.; Andrew, R.D.; Barajas-López, C. ATP inhibits glutamate synaptic release by acting at P2Y receptors in pyramidal neurons of hippocampal slices. J. Pharmacol. Exp. Ther. 2000, 293, 172–179. [Google Scholar]
- Donato, R.; Rodrigues, R.J.; Takahashi, M.; Tsai, M.C.; Soto, D.; Miyagi, K.; Villafuertes, R.G.; Cunha, R.A.; Edwards, F.A. GABA release by basket cells onto Purkinje cells, in rat cerebellar slices, is directly controlled by presynaptic purinergic receptors, modulating Ca2+ influx. Cell Calcium 2008, 44, 521–532. [Google Scholar] [CrossRef]
- Filippov, A.K.; Brown, D.A.; Barnard, E.A. The P2Y1 receptor closes the N-type Ca2+ channel in neurons, with both adenosine triphosphates and diphosphates as potent agonists. Br. J. Pharmacol. 2000, 129, 1063–1066. [Google Scholar] [CrossRef] [PubMed]
- Gerevich, Z.; Borvendeg, S.J.; Schroder, W.; Franke, H.; Wirkner, K.; Norenberg, W.; Furst, S.; Gillen, C.; Illes, P. Inhibition of N-type voltage-activated calcium channels in rat dorsal root ganglion neurons by P2Y receptors is a possible mechanism of ADP-induced analgesia. J. Neurosci. 2004, 24, 797–807. [Google Scholar] [CrossRef] [PubMed]
- Luthardt, J.; Borvendeg, S.J.; Sperlagh, B.; Poelchen, W.; Wirkner, K.; Illes, P. P2Y1 receptor activation inhibits NMDA receptor-channels in layer V pyramidal neurons of the rat prefrontal and parietal cortex. Neurochem. Int. 2003, 42, 161–172. [Google Scholar] [CrossRef]
- Guzman, S.J.; Gerevich, Z.; Hengstler, J.G.; Illes, P.; Kleemann, W. P2Y1 receptors inhibit both strength and plasticity of glutamatergic synaptic neurotransmission in the rat prefrontal cortex. Synapse 2005, 57, 235–238. [Google Scholar] [CrossRef] [PubMed]
- Guzman, S.J.; Schmidt, H.; Franke, H.; Krugel, U.; Eilers, J.; Illes, P.; Gerevich, Z. P2y1 Receptors Inhibit Long-Term Depression in the Prefrontal Cortex. Neuropharmacology 2010, 59, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Saitow, F.; Murakoshi, T.; Suzuki, H.; Konishi, S. Metabotropic P2Y purinoceptor-mediated presynaptic and postsynaptic enhancement of cerebellar GABAergic transmission. J. Neurosci. 2005, 25, 2108–2116. [Google Scholar] [CrossRef] [PubMed]
- Bowser, D.N.; Khakh, B.S. ATP excites interneurons and astrocytes to increase synaptic inhibition in neuronal networks. J. Neurosci. 2004, 24, 8606–8620. [Google Scholar] [CrossRef]
- Kawamura, M.; Gachet, C.; Inoue, K.; Kato, F. Direct excitation of inhibitory interneurons by extracellular ATP mediated by P2Y1 receptors in the hippocampal slice. J. Neurosci. 2004, 24, 10835–41085. [Google Scholar] [CrossRef]
- Coppi, E.; Pedata, F.; Gibb, A.J. P2Y1 receptor modulation of Ca2+-activated K+ currents in medium-sized neurons from neonatal rat striatal slices. J. Neurophysiol. 2012, 107, 1009–1021. [Google Scholar] [CrossRef]
- Tan, Z.; Liu, Y.; Xi, W.; Lou, H.F.; Zhu, L.; Guo, Z.; Mei, L.; Duan, S. Glia-derived ATP inversely regulates excitability of pyramidal and CCK-positive neurons. Nat. Commun. 2017, 8, 13772. [Google Scholar] [CrossRef]
- Filippov, A.K.; Choi, R.C.Y.; Simon, J.; Barnard, E.A.; Brown, D.A. Activation of P2Y1 nucleotide receptors induces inhibition of the M-type K+ current in rat hippocampal pyramidal neurons. J. Neurosci. 2006, 26, 9340–9348. [Google Scholar] [CrossRef] [PubMed]
- Franke, H.; Krugel, U.; Illes, P. P2 receptor-mediated proliferative effects on astrocytes in vivo. Glia, 1999; 28, 190–200. [Google Scholar]
- Jourdain, P.; Bergersen, L.H.; Bhaukaurally, K.; Bezzi, P.; Santello, M.; Domercq, M.; Matute, C.; Tonello, F.; Gundersen, V.; Volterra, A. Glutamate exocytosis from astrocytes controls synaptic strength. Nat. Neurosci. 2007, 10, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Kuboyama, K.; Harada, H.; Tozaki-Saitoh, H.; Tsuda, M.; Ushijima, K.; Inoue, K. Astrocytic P2Y(1) receptor is involved in the regulation of cytokine/chemokine transcription and cerebral damage in a rat model of cerebral ischemia. J. Cereb. Blood Flow Metab. 2011, 31, 1930–1941. [Google Scholar] [CrossRef]
- Pascual, O.; Achour, S.B.; Rostaing, P.; Triller, A.; Bessis, A. Microglia activation triggers astrocyte-mediated modulation of excitatory neurotransmission. Proc. Natl. Acad. Sci. USA 2012, 109, E197–E205. [Google Scholar] [CrossRef] [PubMed]
- Fam, S.R.; Gallagher, C.J.; Kalia, L.V.; Salter, M.W. Differential frequency dependence of P2Y1- and P2Y2-mediated Ca2+ signaling in astrocytes. J. Neurosci. 2003, 23, 4437–4444. [Google Scholar] [CrossRef]
- Neary, J.T.; Kang, Y.; Willoughby, K.A.; Ellis, E.F. Activation of extracellular signal-regulated kinase by stretch-induced injury in astrocytes involves extracellular ATP and P2 purinergic receptors. J. Neurosci. 2003, 23, 2348–2356. [Google Scholar] [CrossRef]
- Domercq, M.; Brambilla, L.; Pilati, E.; Marchaland, J.; Volterra, A.; Bezzi, P. P2Y1 receptor-evoked glutamate exocytosis from astrocytes: Control by tumor necrosis factor-alpha and prostaglandins. J. Biol. Chem. 2006, 281, 30684–93066. [Google Scholar] [CrossRef]
- Santello, M.; Bezzi, P.; Volterra, A. TNFα controls glutamatergic gliotransmission in the hippocampal dentate gyrus. Neuron 2011, 69, 988–1001. [Google Scholar] [CrossRef]
- Shen, W.; Nikolic, L.; Meunier, C.; Pfrieger, F.; Audinat, E. An autocrine purinergic signaling controls astrocyte-induced neuronal excitation. Sci. Rep. 2017, 7, 11280. [Google Scholar] [CrossRef]
- Locovei, S.; Wang, J.; Dahl, G. Activation of pannexin 1 channels by ATP through P2Y receptors and by cytoplasmic calcium. FEBS Lett. 2006, 580, 239–244. [Google Scholar] [CrossRef]
- Zhang, J.M.; Wang, H.K.; Ye, C.Q.; Ge, W.; Chen, Y.; Jiang, Z.L.; Wu, C.P.; Poo, M.M.; Duan, S. ATP released by astrocytes mediates glutamatergic activity-dependent heterosynaptic suppression. Neuron 2003, 40, 971–982. [Google Scholar] [CrossRef]
- Jacob, P.F.; Vaz, S.H.; Ribeiro, J.A.; Sebastiao, A.M. P2Y1 receptor inhibits GABA transport through a calcium signalling-dependent mechanism in rat cortical astrocytes. Glia 2014, 62, 1211–1226. [Google Scholar] [CrossRef] [PubMed]
- Boucsein, C.; Zacharias, R.; Farber, K.; Pavlovic, S.; Hanisch, U.K.; Kettenmann, H. Purinergic receptors on microglial cells: Functional expression in acute brain slices and modulation of microglial activation in vitro. Eur. J. Neurosci. 2003, 17, 2267–2276. [Google Scholar] [CrossRef] [PubMed]
- Bianco, F.; Fumagalli, M.; Pravettoni, E.; D’Ambrosi, N.; Volonte, C.; Matteoli, M.; Abbracchio, M.P.; Verderio, C. Pathophysiological roles of extracellular nucleotides in glial cells: Differential expression of purinergic receptors in resting and activated microglia. Brain Res. Rev. 2005, 48, 144–156. [Google Scholar] [CrossRef] [PubMed]
- Ballerini, P.; Di Iorio, P.; Ciccarelli, R.; Caciagli, F.; Poli, A.; Beraudi, A.; Buccella, S.; D’Alimonte, I.; D’Auro, M.; Nargi, E.; et al. P2Y1 and cysteinyl leukotriene receptors mediate purine and cysteinyl leukotriene co-release in primary cultures of rat microglia. Int. J. Immunopathol. Pharmacol. 2005, 18, 255–268. [Google Scholar] [CrossRef]
- Koizumi, S.; Ohsawa, K.; Inoue, K.; Kohsaka, S. Purinergic receptors in microglia: Functional modal shifts of microglia mediated by P2 and P1 receptors. Glia 2013, 61, 47–54. [Google Scholar] [CrossRef]
- Eyo, U.B.; Peng, J.; Swiatkowski, P.; Mukherjee, A.; Bispo, A.; Wu, L.J. Neuronal hyperactivity recruits microglial processes via neuronal NMDA receptors and microglial P2Y12 receptors after status epilepticus. J. Neurosci. 2014, 34, 10528–10540. [Google Scholar] [CrossRef]
- Milior, G.; Morin-Brureau, M.; Chali, F.; Le Duigou, C.; Savary, E.; Huberfeld, G.; Rouach, N.; Pallud, J.; Capelle, L.; Navarro, V.; et al. Distinct P2Y receptors mediate extension and retraction of microglial processes in epileptic and peritumoral human tissue. J. Neurosci. 2020, 40, 1373–1388. [Google Scholar] [CrossRef]
- Padrão, R.A.; Ariza, C.B.; Canzian, M.; Porcionatto, M.; Araffljo, M.G.L.; Cavalheiro, E.A. The P2 purinergic receptors are increased in the hippocampus of patients with temporal lobe epilepsy: What is the relevance to the epileptogenesis? Purinergic Signal. 2011, 7, 127. [Google Scholar]
- Alves, M.; Gomez-Villafuertes, R.; Delanty, N.; Farrell, M.A.; O’Brien, D.F.; Miras-Portugal, M.T.; Hernandez, M.D.; Henshall, D.C.; Engel, T. Expression and function of the metabotropic purinergic P2Y receptor family in experimental seizure models and patients with drug-refractory epilepsy. Epilepsia 2017, 58, 1603–1614. [Google Scholar] [CrossRef]
- Alves, M.; Smith, J.; Engel, T. Differential expression of the metabotropic P2Y receptor family in the cortex following status epilepticus and neuroprotection via P2Y1 antagonism in mice. Front. Pharmacol. 2020, 10, 1558. [Google Scholar] [CrossRef] [PubMed]
- Franke, H.; Krugel, U.; Grosche, J.; Heine, C.; Hartig, W.; Allgaier, C.; Illes, P. P2Y receptor expression on astrocytes in the nucleus accumbens of rats. Neuroscience 2004, 127, 431–441. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.; Iritani, S.; Chambers, J.; Emson, P. Immunohistochemical localization of the P2Y1 purinergic receptor in Alzheimer’s disease. Neuroreport 2000, 11, 3799–3803. [Google Scholar] [CrossRef] [PubMed]
- Traini, C.; Pedata, F.; Cipriani, S.; Mello, T.; Galli, A.; Giovannini, M.G.; Cerbai, F.; Volpini, R.; Cristalli, G.; Pugliese, A.M. P2 receptor antagonists prevent synaptic failure and extracellular signal-regulated kinase 1/2 activation induced by oxygen and glucose deprivation in rat CA1 hippocampus in vitro. Eur. J. Neurosci. 2011, 33, 2203–2215. [Google Scholar] [CrossRef]
- Maraula, G.; Lana, D.; Coppi, E.; Gentile, F.; Mello, T.; Melani, A.; Galli, A.; Giovannini, M.G.; Pedata, F.; Pugliese, A.M. The selective antagonism of P2X7 and P2Y1 receptors prevents synaptic failure and affects cell proliferation induced by oxygen and glucose deprivation in rat dentate gyrus. PLoS ONE 2014, 9, e115273. [Google Scholar] [CrossRef]
- Chin, Y.; Kishi, M.; Sekino, M.; Nakajo, F.; Abe, Y.; Terazono, Y.; Hiroyuki, O.; Kato, F.; Koizumi, S.; Gachet, C.; et al. Involvement of glial P2Y1 receptors in cognitive deficit after focal cerebral stroke in a rodent model. J. Neuroinflamm. 2013, 10, 95. [Google Scholar] [CrossRef]
- Sun, J.J.; Liu, Y.; Ye, Z.R. Effects of P2Y1 receptor on glial fibrillary acidic protein and glial cell line-derived neurotrophic factor production of astrocytes under ischemic condition and the related signaling pathways. Neurosci. Bull. 2008, 24, 231–243. [Google Scholar] [CrossRef]
- Carmo, M.R.; Simões, A.P.; Fonteles, A.A.; Souza, C.M.; Cunha, R.A.; Andrade, G.M. ATP P2Y1 receptors control cognitive deficits and neurotoxicity but not glial modifications induced by brain ischemia in mice. Eur. J. Neurosci. 2014, 39, 614–622. [Google Scholar] [CrossRef]
- Fukumoto, Y.; Tanaka, K.F.; Parajuli, B.; Shibata, K.; Yoshioka, H.; Kanemaru, K.; Gachet, C.; Ikenaka, K.; Koizumi, S.; Kinouchi, H. Neuroprotective effects of microglial P2Y1 receptors against ischemic neuronal injury. J. Cereb. Blood Flow Metab. 2019, 39, 2144–2156. [Google Scholar] [CrossRef]
- Zheng, W.; Watts, L.T.; Holstein, D.M.; Wewer, J.; Lechleiter, J.D. P2Y1R-initiated, IP3R-dependent stimulation of astrocyte mitochondrial metabolism reduces and partially reverses ischemic neuronal damage in mouse. J. Cereb. Blood Flow Metab. 2013, 33, 600–611. [Google Scholar] [CrossRef]
- Zheng, W.; Watts, L.T.; Holstein, D.M.; Prajapati, S.I.; Keller, C.; Grass, E.H.; Walter, C.A.; Lechleiter, J.D. Purinergic receptor stimulation reduces cytotoxic edema and brain infarcts in mouse induced by photothrombosis by energizing glial mitochondria. PLoS ONE 2010, 5, e14401. [Google Scholar] [CrossRef] [PubMed]
- Fujita, T.; Tozaki-Saitoh, H.; Inoue, K. P2Y1 receptor signaling enhances neuroprotection by astrocytes against oxidative stress via IL-6 release in hippocampal cultures. Glia 2009, 57, 244–257. [Google Scholar] [CrossRef] [PubMed]
- Maiolino, M.; O’Neill, N.; Lariccia, V.; Amoroso, S.; Sylantyev, S.; Angelova, P.R.; Abramov, A.Y. Inorganic polyphosphate regulates AMPA and NMDA receptors and protects against glutamate excitotoxicity via activation of P2Y receptors. J. Neurosci. 2018, 39, 6038–6048. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.; De Diego Garcia, L.; Conte, G.; Jimenez-Mateos, E.M.; D’Orsi, B.; Sanz-Rodriguez, A.; Prehn, J.H.M.; Henshall, D.C.; Engel, T. Context-specific switch from anti- to pro-epileptogenic function of the P2Y1 receptor in experimental epilepsy. J. Neurosci. 2019, 39, 5377–5392. [Google Scholar] [CrossRef]
- Nikolic, L.; Shen, W.; Nobili, P.; Virenque, A.; Ulmann, L.; Audinat, E. Blocking TNFα-driven astrocyte purinergic signaling restores normal synaptic activity during epileptogenesis. Glia 2018, 66, 2673–2683. [Google Scholar] [CrossRef]
- Nobili, P.; Shen, W.; Milicevic, K.; Bogdanovic Pristov, J.; Audinat, E.; Nikolic, L. Therapeutic potential of astrocyte purinergic signalling in epilepsy and multiple sclerosis. Front. Pharmacol. 2022, 13, 900337. [Google Scholar]
- Su, L.; Bai, X.; Niu, T.; Zhuang, X.; Dong, B.; Wang, G.; Yu, Y. P2Y1 purinergic receptor inhibition attenuated remifentanil-induced postoperative hyperalgesia via decreasing NMDA receptor phosphorylation in dorsal root ganglion. Brain Res. Bull. 2021, 177, 352–362. [Google Scholar] [CrossRef]
- Nedergaard, M.; Dirnagl, U. Role of glial cells in cerebral ischemia. Glia 2005, 50, 281–286. [Google Scholar] [CrossRef]
- Shinozaki, Y.; Shibata, K.; Yoshida, K.; Shigetomi, E.; Gachet, C.; Ikenaka, K.; Tanaka, K.F.; Koizumi, S. Transformation of astrocytes to a neuroprotective phenotype by microglia via P2Y1 receptor downregulation. Cell Rep. 2017, 19, 1151–1164. [Google Scholar] [CrossRef]
- Martorell, A.; Wellmann, M.; Guiffa, F.; Fuenzalida, M.; Bonansco, C. P2Y1 receptor inhibition rescues impaired synaptic plasticity and astroglial Ca2+-dependent activity in the epileptic hippocampus. Neurobiol. Dis. 2020, 146, 105132. [Google Scholar] [CrossRef]
- Kumagawa, T.; Moro, N.; Maeda, T.; Kobayashi, M.; Furukawa, Y.; Shijo, K.; Yoshino, A. Anti-inflammatory effect of P2Y1 receptor blocker MRS2179 in a rat model of traumatic brain injury. Brain Res. Bull. 2022, 181, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Kuchibhotla, K.V.; Lattarulo, C.R.; Hyman, B.T.; Bacskai, B.J. Synchronous hyperactivity and intercellular calcium waves in astrocytes in Alzheimer mice. Science 2009, 323, 1211–1215. [Google Scholar] [CrossRef] [PubMed]
- Reichenbach, N.; Delekate, A.; Breithausen, B.; Keppler, K.; Poll, S.; Schulte, T.; Peter, J.; Plescher, M.; Hansen, J.N.; Blank, N.; et al. P2Y1 receptor blockade normalizes network dysfunction and cognition in an Alzheimer’s disease model. J. Exp. Med. 2018, 215, 1649–1663. [Google Scholar] [CrossRef] [PubMed]
- Koch, H.; Bespalov, A.; Drescher, K.; Franke, H.; Krügel, U. Impaired cognition after stimulation of P2Y1 receptors in the rat medial prefrontal cortex. Neuropsychopharmacology 2015, 40, 305–314. [Google Scholar] [CrossRef]
- Shi, A.; Petrache, A.L.; Shi, J.; Ali, A.B. Preserved calretinin interneurons in an APP model of Alzheimer’s disease disrupt hippocampal inhibition via upregulated P2Y1 purinoreceptors. Cereb. Cortex 2020, 30, 1272–1290. [Google Scholar] [CrossRef] [PubMed]
- Shinozaki, Y.; Koizumi, S.; Ishida, S.; Sawada, J.; Ohno, Y.; Inoue, K. Cytoprotection against oxidative stress-induced damage of astrocytes by extracellular ATP via P2Y1 receptors. Glia 2005, 49, 288–300. [Google Scholar] [CrossRef]
- Shinozaki, Y.; Koizumi, S.; Ohno, Y.; Nagao, T.; Inoue, K. Extracellular ATP counteracts the ERK1/2-mediated death-promoting signaling cascades in astrocytes. Glia 2006, 54, 606–618. [Google Scholar] [CrossRef]
- Guo, H.; Liu, Z.Q.; Zhou, H.; Wang, Z.L.; Tao, Y.H.; Tong, Y. P2Y1 receptor antagonists mitigate oxygen and glucose deprivation-induced astrocyte injury. Mol. Med. Rep. 2018, 17, 1819–1824. [Google Scholar] [CrossRef]
- Miller, W.J.; Leventhal, I.; Scarsella, D.; Haydon, P.G.; Janmey, P.; Meaney, D.F. Mechanically induced reactive gliosis causes ATP-mediated alterations in astrocyte stiffness. J. Neurotrauma 2009, 26, 789–797. [Google Scholar] [CrossRef]
- Guzman, S.J.; Gerevich, Z. P2Y receptors in synaptic transmission and plasticity: Therapeutic potential in cognitive dysfunction. Neural Plast. 2016, 2016, 1207393. [Google Scholar] [CrossRef]
- Woods, L.T.; Ajit, D.; Camden, J.M.; Erb, L.; Weisman, G.A. Purinergic receptors as potential therapeutic targets in Alzheimer’s disease. Neuropharmacology 2016, 104, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Quintas, C.; Vale, N.; Gonçalves, J.; Queiroz, G. Microglia P2Y13 receptors prevent astrocyte proliferation mediated by P2Y1 receptors. Front. Pharmacol. 2018, 9, 418. [Google Scholar] [CrossRef] [PubMed]
- Dias, L.; Madeira, D.; Dias, R.; Tomé, Â.R.; Cunha, R.A.; Agostinho, P. Aβ1-42 peptides blunt the adenosine A2A receptor-mediated control of the interplay between P2X7 and P2Y1 receptors mediated calcium responses in astrocytes. Cell. Mol. Life Sci. 2022, 79, 457. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).