A National Survey Evaluating the Impact of the COVID-19 Pandemic on Students Pursuing Careers in Neurosurgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Survey Design and Administration
2.3. Statistical Analysis
3. Results
3.1. Study Demographics
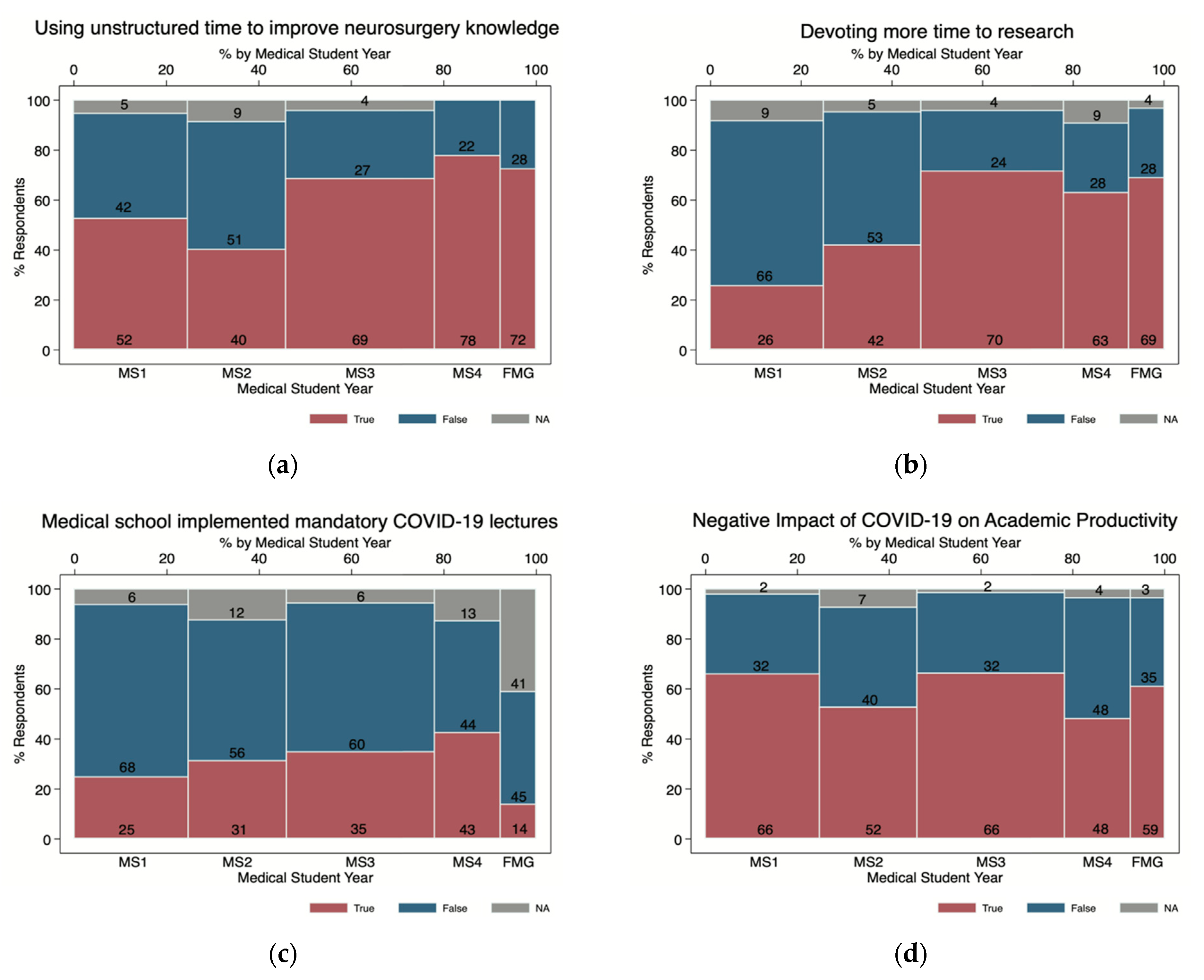
3.2. Impact of COVID-19 on Academic Productivity, Research Activities, and Career in Neurosurgery
3.3. Third- and Fourth-Year Specific Factors
3.4. Foreign Medical Graduate Specific Issues
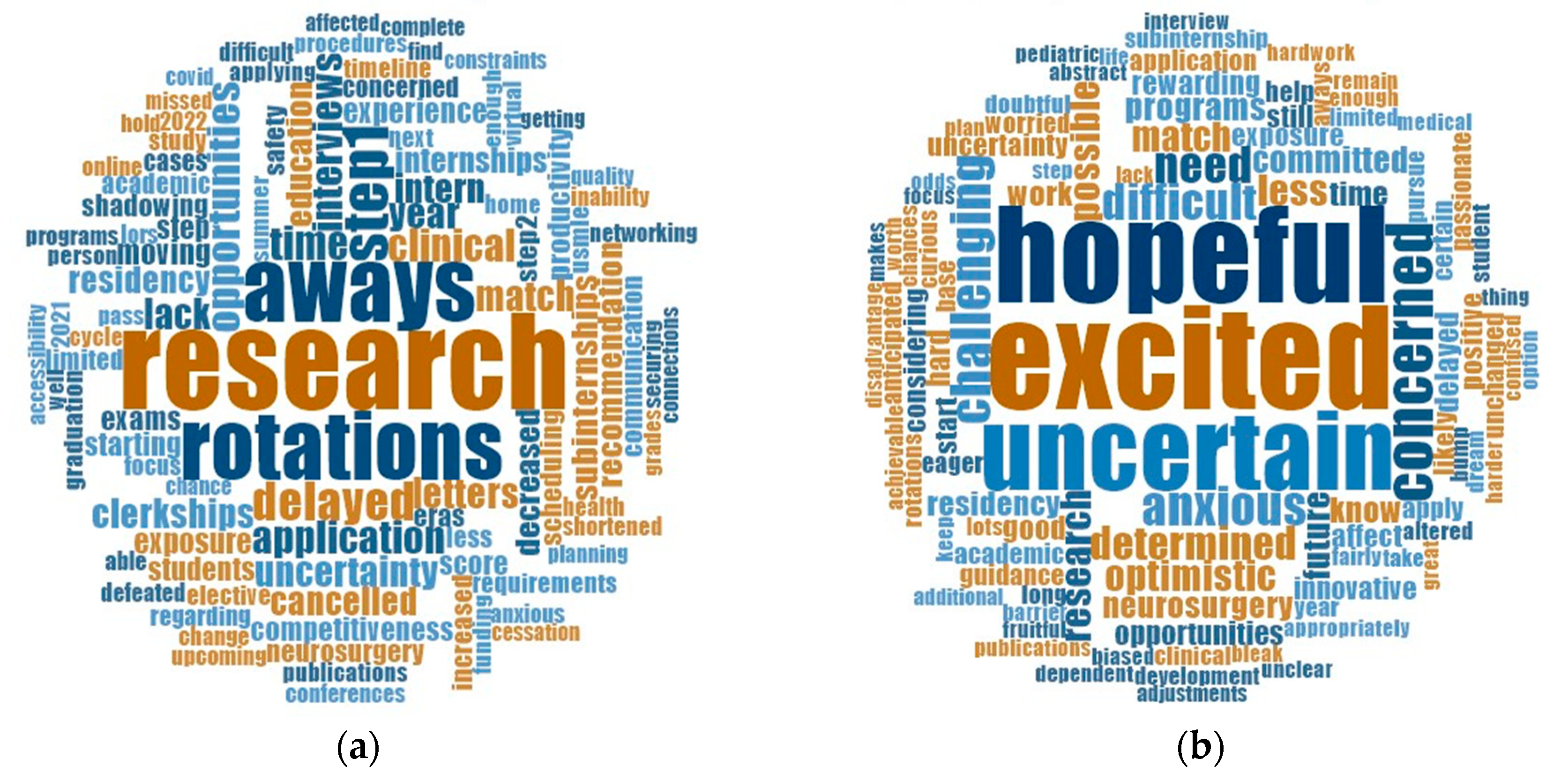
3.5. Communication, Immediate Concerns, Perceptions, and Supporting the Future of Neurosurgery
4. Discussion
4.1. Issues and Solutions by Medical School Class
4.2. Best Practices and Action Items for Program Directors
4.3. Beyond the COVID-19 Pandemic
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategy Used to Identify Respondents
References
- Rose, S. Medical Student Education in the Time of COVID-19. JAMA 2020, 323, 2131–2132. [Google Scholar] [CrossRef]
- Bambakidis, N.C.; Tomei, K.L. Impact of COVID-19 on neurosurgery resident training and education. J. Neurosurg. 2020, 133, 10–11. [Google Scholar] [CrossRef] [Green Version]
- Burke, J.F.; Chan, A.K.; Mummaneni, V.; Chou, D.; Lobo, E.P.; Berger, M.S.; Theodosopoulos, P.V.; Mummaneni, P.V. Letter: The Coronavirus Disease 2019 Global Pandemic: A Neurosurgical Treatment Algorithm. Neurosurgery 2020, 87, E50–E56. [Google Scholar] [CrossRef] [Green Version]
- Eichberg, D.G.; Shah, A.H.; Luther, E.M.; Menendez, I.; Jimenez, A.; Perez-Dickens, M.; O’Phelan, K.H.; Ivan, M.E.; Komotar, R.J.; Levi, A.D. Letter: Academic Neurosurgery Department Response to COVID-19 Pandemic: The University of Miami/Jackson Memorial Hospital Model. Neurosurgery 2020, 87, E63–E65. [Google Scholar] [CrossRef] [PubMed]
- Chae, J.K.; Haghdel, A.; Guadix, S.W.; Winston, G.M.; Younus, I.; Radwanski, R.; Schwartz, T.H.; Greenfield, J.P.; Apuzzo, M.L.J.; Pannullo, S.C. Letter: COVID-19 Impact on the Medical Student Path to Neurosurgery. Neurosurgery 2020, 87, nyaa187. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.G.; Pierson, L.; Doernberg, S. The Role of Medical Students During the COVID-19 Pandemic. Ann. Intern. Med. 2020, 173, 145–146. [Google Scholar] [CrossRef] [Green Version]
- Mohile, N.A.; Blakeley, J.O.; Gatson, N.T.N.; Hottinger, A.F.; Lassman, A.B.; Ney, D.E.; Olar, A.; Schiff, D.; Shih, H.A.; Strowd, R.; et al. Urgent Considerations for the Neuro-oncologic Treatment of Patients with Gliomas During the COVID-19 Pandemic. Neuro-Oncology 2020, 22, 912–917. [Google Scholar] [CrossRef] [Green Version]
- Association of American Medical Colleges. Interim Guidance on Medical Students’ Participation in Direct Patient Contact Activities; AAMC: Washington, DC, USA, 2020. [Google Scholar]
- Zuckerman, S.L.; Mistry, A.M.; Hanif, R.; Chambless, L.B.; Neimat, J.S.; Wellons, J.C.; Mocco, J.; Sills, A.K.; McGirt, M.J.; Thompson, R.C. Neurosurgery Elective for Preclinical Medical Students: Early Exposure and Changing Attitudes. World Neurosurg. 2016, 86, 120–126. [Google Scholar] [CrossRef]
- Garcia, R.M.; Reynolds, R.A.; Weiss, H.K.; Chambless, L.B.; Lam, S.; Dahdaleh, N.S.; Rosseau, G. Letter: Preliminary National Survey Results Evaluating the Impact of COVID-19 Pandemic on Medical Students Pursuing Careers in Neurosurgery. Neurosurgery 2020, 87, nyaa214. [Google Scholar] [CrossRef] [PubMed]
- Association of American Medical Colleges; AAMC: Washington, DC, USA, 2016.
- Listing of AANS Medical Student Chapters; American Association of Neurological Surgeons: Rolling Meadows, IL, USA, 2020.
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Census Regions and Divisions of the United States; U.S. Census Bureau: Washington, DC, USA, 2020.
- Sizdahkhani, S.; Purger, D.; Cohen-Gadol, A. Applying to Neurosurgery. In Neurosurgical Atlas; Neurosurgical Atlas Inc.: Indianapolis, IN, USA, 2017. [Google Scholar]
- Liang, Z.C.; Ooi, S.B.S.; Wang, W. Pandemics and Their Impact on Medical Training: Lessons From Singapore. Acad. Med. J. Assoc. Am. Med. Coll. 2020, 95, 1359–1361. [Google Scholar] [CrossRef]
- Leschke, J.M.; Hunt, M.A. Electronic Residency Application Service Application Characteristics Associated with Successful Residency Matching in Neurosurgery in 2009–2016. World Neurosurg. 2018, 113, e529–e534. [Google Scholar] [CrossRef] [PubMed]
- Advance Data Tables 2020 Main Residency Match; National Resident Matching Program: Washington, DC, USA, 2020.
- National Resident Matching Program. Charting Outcomes in the Match: International Medical Graduates, 2nd ed.; NRMP: Washington, DC, USA, 2018. [Google Scholar]
- National Resident Matching Program. Charting Outcomes in the Match: U.S. Allopathic Seniors; NRMP: Washington, DC, USA, 2018. [Google Scholar]
- Renfrow, J.J.; Rodriguez, A.; Liu, A.; Pilitsis, J.G.; Samadani, U.; Ganju, A.; Germano, I.M.; Benzil, D.L.; Wolfe, S.Q. Positive trends in neurosurgery enrollment and attrition: Analysis of the 2000–2009 female neurosurgery resident cohort. J. Neurosurg. 2016, 124, 834–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kozar, R.A.; Lucci, A.; Miller, C.C.; Azizzadeh, A.; Cocanour, C.S.; Potts, J.R.; Fischer, C.P.; Brundage, S.I. Brief intervention by surgeons can influence students toward a career in surgery. J. Surg. Res. 2003, 111, 166–169. [Google Scholar] [CrossRef]
- Campbell, P.G.; Awe, O.O.; Maltenfort, M.G.; Moshfeghi, D.M.; Leng, T.; Moshfeghi, A.A.; Ratliff, J.K. Medical school and residency influence on choice of an academic career and academic productivity among neurosurgery faculty in the United States. J. Neurosurg. 2011, 115, 380–386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansell, M.W.; Ungerleider, R.M.; Brooks, C.A.; Knudson, M.P.; Kirk, J.K.; Ungerleider, J.D. Temporal Trends in Medical Student Burnout. Fam. Med. 2019, 51, 399–404. [Google Scholar] [CrossRef] [Green Version]
- Wadhwa, H.; Shah, S.S.; Shan, J.; Cheng, J.; Beniwal, A.S.; Chen, J.-S.; Gill, S.A.; Mummaneni, N.; McDermott, M.W.; Berger, M.S.; et al. The neurosurgery applicant’s “arms race”: Analysis of medical student publication in the Neurosurgery Residency Match. J. Neurosurg. 2019, 133, 1–9. [Google Scholar] [CrossRef]
- Frieden, J. Trying to Fix the Hyper-Competitive Residency Match. MedPage Today, 8 July 2019. [Google Scholar]
- Al Khalili, K.; Chalouhi, N.; Tjoumakaris, S.; Gonzalez, L.F.; Starke, R.M.; Rosenwasser, R.; Jabbour, P. Programs selection criteria for neurological surgery applicants in the United States: A national survey for neurological surgery program directors. World Neurosurg. 2014, 81, 473–477.e2. [Google Scholar] [CrossRef]
- Results of the 2019 NRMP Applicant Survey by Preferred Specialty and Applicant Type; National Resident Matching Program: Washington, DC, USA, 2019.
- Maurer, R. Use of Video for Recruiting Continues to Grow; SHRM Society for Human Resource Management: Alexandria, VA, USA, 2015. [Google Scholar]
- Agarwal, N.; Choi, P.A.; Okonkwo, D.O.; Barrow, D.L.; Friedlander, R.M. Financial burden associated with the residency match in neurological surgery. J. Neurosurg. 2017, 126, 184–190. [Google Scholar] [CrossRef] [Green Version]
- Patel, V.; Nolan, I.T.; Morrison, S.D.; Fosnot, J. Visiting Subinternships in Wake of the COVID-19 Crisis: An Opportunity for Improvement. Ann. Plast. Surg. 2020, 85, S153–S154. [Google Scholar] [CrossRef]
- Aiyer, A.A.; Granger, C.J.; McCormick, K.L.; Cipriano, C.A.; Kaplan, J.R.; Varacallo, M.A.; Dodds, S.D.; Levine, W.N. The Impact of COVID-19 on the Orthopaedic Surgery Residency Application Process. J. Am. Acad. Orthop. Surg. 2020. [Google Scholar] [CrossRef]
- Boyd, C.J.; Inglesby, D.C.; Corey, B.; Greene, B.J.; Harrington, M.A.; Johnson, M.D.; King, T.W.; Rais-Bahrami, S.; Tavana, M.L. Impact of COVID-19 on away rotations in surgical fields. J. Surg. Res. 2020, 255, 96–98. [Google Scholar] [CrossRef] [PubMed]
- Sell, N.M.; Qadan, M.; Delman, K.A.; Roggin, K.K.; Spain, D.A.; Phitayakorn, R.; Lillemoe, K.D.; Mullen, J.T. Implications of COVID-19 on the General Surgery Match. Ann. Surg. 2020, 272, e155. [Google Scholar] [CrossRef]
- Bird, S.B.; Hern, H.G.; Blomkalns, A.; Deiorio, N.M.; Haywood, Y.; Hiller, K.M.; Dunleavy, D.; Dowd, K. Innovation in Residency Selection: The AAMC Standardized Video Interview. Acad. Med. J. Assoc. Am. Med. Coll. 2019, 94, 1489–1497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Field, N.C.; Gullick, M.M.; German, J.W. Selection of Neurological Surgery Applicants and the Value of Standardized Letters of Evaluation: A Survey of United States Program Directors. World Neurosurg. 2020, 136, e342–e346. [Google Scholar] [CrossRef] [PubMed]
- Nicolosi, F.; Rossini, Z.; Zaed, I.; Kolias, A.G.; Fornari, M.; Servadei, F. Neurosurgical digital teaching in low-middle income countries: Beyond the frontiers of traditional education. Neurosurg. Focus 2018, 45, E17. [Google Scholar] [CrossRef] [Green Version]
- Blankstein, U.; Dakurah, T.; Bagan, M.; Hodaie, M. Structured online neurosurgical education as a novel method of education delivery in the developing world. World Neurosurg. 2011, 76, 224–230. [Google Scholar] [CrossRef]
- Bagan, M. The Foundation For International Education in Neurological Surgery. World Neurosurg. 2010, 73, 289. [Google Scholar] [CrossRef]
- Abi-Rafeh, J.; Azzi, A.J. Emerging Role of Online Virtual Teaching Resources for Medical Student Education in Plastic Surgery: COVID-19 Pandemic and Beyond. J. Plast. Reconstr. Aesthetic Surg. 2020, 73, 1575. [Google Scholar] [CrossRef]
- Moszkowicz, D.; Duboc, H.; Dubertret, C.; Roux, D.; Bretagnol, F. Daily medical education for confined students during COVID-19 pandemic: A simple videoconference solution. Clin. Anat. 2020, 33, 927–928. [Google Scholar] [CrossRef] [PubMed]
- Chao, T.N.; Frost, A.S.; Brody, R.M.; Byrnes, Y.M.; Cannady, S.B.; Luu, N.N.; Rajasekaran, K.; Shanti, R.M.; Silberthau, K.R.; Triantafillou, V. Creation of an Interactive Virtual Surgical Rotation for Undergraduate Medical Education During the COVID-19 Pandemic. J. Surg. Educ. 2020, 78, 346–350. [Google Scholar] [CrossRef]
- Kania, K.; Abu-Ghname, A.; Agrawal, N.; Maricevich, R.S. Four Strategies for Plastic Surgery Education amid the COVID-19 Pandemic. Plast. Reconstr. Surg. 2020, 146, 252e–253e. [Google Scholar] [CrossRef]
- Ebrahimi, A.; Ebrahimi, S.; Esfahani, S.A. How COVID-19 pandemic can lead to promotion of remote medical education and democratization of education? J. Adv. Med. Educ. Prof. 2020, 8, 144. [Google Scholar] [PubMed]
- Ruthberg, J.S.; Quereshy, H.A.; Ahmadmehrabi, S.; Trudeau, S.; Chaudry, E.; Hair, B.; Kominsky, A.; Otteson, T.D.; Bryson, P.C.; Mowry, S.E. A Multimodal Multi-Institutional Solution to Remote Medical Student Education for Otolaryngology During COVID-19. Otolaryngol.—Head Neck Surg. 2020, 163, 707–709. [Google Scholar] [CrossRef] [PubMed]
- Hew, K.F.; Lo, C.K. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med. Educ. 2018, 18, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | n = 379 | % |
|---|---|---|
| What region of the United States is your medical school located in? (n, %) | ||
| Midwest | 91 | 24.0 |
| Northeast | 84 | 22.2 |
| South | 138 | 36.4 |
| West | 37 | 9.8 |
| Prefer not to say | 6 | 1.6 |
| Outside United States | 23 | 6.1 |
| Sex (n, %) | ||
| Female | 140 | 36.9 |
| Male | 238 | 62.8 |
| Prefer not to say | 1 | 0.3 |
| Age (mean +/standard error, range) | 25.6 (0.1) | 19–37 |
| What year are you currently completing? (n, %) | ||
| First year (MS1 a) | 94 | 24.8 |
| Second year (MS2) | 81 | 21.4 |
| Third year (MS3) | 121 | 31.9 |
| Fourth year (MS4) | 54 | 14.2 |
| Foreign Medical Graduate | 29 | 7.7 |
| Are you in a combined, dual degree program? (n, %) | ||
| No | 315 | 83.1 |
| Yes | 63 | 16.6 |
| Additional graduate degree type. (n, %) | ||
| Not applicable | 290 | 81.9 |
| PhD | 36 | 10.2 |
| MA/MS/MPH | 24 | 6.8 |
| MBA | 3 | 0.8 |
| JD | 1 | 0.3 |
| I am currently under a ‘Stay at Home’ order by my medical school (n, %) | ||
| False | 24 | 6.4 |
| True | 353 | 93.6 |
| Do you have a neurosurgery program at your home institution? (n, %) | ||
| No | 62 | 16.5 |
| Yes | 314 | 83.5 |
| Does your institution have a neurosurgery rotation for medical students? (n, %) | ||
| No, we do not have a neurosurgery rotation for students | 49 | 13 |
| Yes, it is optional for students | 314 | 83.3 |
| Yes, it is required for all students to graduate | 14 | 3.7 |
| Regarding the neurosurgery rotations at your home institution, are they elective, mandatory, or not available? | ||
| Elective | 317 | 85.0 |
| Mandatory | 14 | 3.8 |
| Not applicable | 42 | 11.3 |
| Neurosurgery rotation offered multiple years (n, %) | ||
| Single year | 104 | 27.4 |
| Multiple | 224 | 59.1 |
| Not applicable | 51 | 13.5 |
| Frequency of neurosurgery rotations by medical school year (n) | ||
| Year 1 | 3 | - |
| Year 2 | 28 | - |
| Year 3 | 252 | - |
| Year 4 | 290 | - |
| Does your university have an AANS b Medical Student Chapter or other neurosurgery interest group for medical students? (n, %) | ||
| Yes, AANS | 46 | 12.1 |
| Yes, interest group | 264 | 69.7 |
| No | 12 | 3.2 |
| Do not know | 56 | 14.8 |
| Priority | MS1 a n = 94 | MS2 n = 81 | MS3 n = 121 | MS4 n = 54 | FMG b n = 29 | Total n = 379 | Overall Rank |
|---|---|---|---|---|---|---|---|
| Student-focused educational webinars | 62 (2) | 19 (2) | 78 (3) | 33 (1) | 22 (1) | 217 | 1 |
| Focused medical student sessions at upcoming neurosurgical conferences | 63 (1) | 49 (1) | 28 (2) | 22 (1) | 226 | 2 | |
| Additional away sub-internship spots at programs in 2021 | 40 (3) | 49 (1) | 14 (2) | 177 | 3 | ||
| Additional away sub-internship spots at programs later in 2020 | 90 (1) | 19 (3) | 176 | 4 | |||
| Delay the match process to allow for away sub-internships | 80 (2) | 164 | 5 | ||||
| Be part of a “Future Neurosurgeons” listserv | 3 | 6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garcia, R.M.; Reynolds, R.A.; Weiss, H.K.; Shlobin, N.A.; Chambless, L.B.; Lam, S.; Dahdaleh, N.S.; Rosseau, G. A National Survey Evaluating the Impact of the COVID-19 Pandemic on Students Pursuing Careers in Neurosurgery. NeuroSci 2021, 2, 320-333. https://doi.org/10.3390/neurosci2040023
Garcia RM, Reynolds RA, Weiss HK, Shlobin NA, Chambless LB, Lam S, Dahdaleh NS, Rosseau G. A National Survey Evaluating the Impact of the COVID-19 Pandemic on Students Pursuing Careers in Neurosurgery. NeuroSci. 2021; 2(4):320-333. https://doi.org/10.3390/neurosci2040023
Chicago/Turabian StyleGarcia, Roxanna M., Rebecca A. Reynolds, Hannah K. Weiss, Nathan A. Shlobin, Lola B. Chambless, Sandi Lam, Nader S. Dahdaleh, and Gail Rosseau. 2021. "A National Survey Evaluating the Impact of the COVID-19 Pandemic on Students Pursuing Careers in Neurosurgery" NeuroSci 2, no. 4: 320-333. https://doi.org/10.3390/neurosci2040023
APA StyleGarcia, R. M., Reynolds, R. A., Weiss, H. K., Shlobin, N. A., Chambless, L. B., Lam, S., Dahdaleh, N. S., & Rosseau, G. (2021). A National Survey Evaluating the Impact of the COVID-19 Pandemic on Students Pursuing Careers in Neurosurgery. NeuroSci, 2(4), 320-333. https://doi.org/10.3390/neurosci2040023






