1. Introduction
There are many factors that influence an individual’s perception of pain. The literature suggests that personality type may affect perceptions of pain; however, it is an often-overlooked attribute. The purpose of this review is to discuss one of the most common medical conditions reported in industrialized society, low back pain (LBP), and factors that contribute to the pain experience, as well as personality attributes that may influence outcomes. In addition, this paper will explore personality inventories and how they may be interpreted. The information may help clinicians to determine if personality characteristics will influence perceptions of pain and therefore assist in developing a unique plan of care.
In the United States, an estimated 20% of adults live with chronic pain [
1]. LBP is one of the most common types of pain, being reported among 13.2% of American adults aged 20–69 [
2]. Despite its high prevalence, LBP is still a complicated and poorly understood affliction with a multitude of causes [
3]. Billions of dollars a year are attributed to direct and indirect costs associated with LBP. Kim et al. [
4] tracked 2.5 million patients with LBP and found that these individuals spent over USD 2.6 billion in health care costs. Up to 12.8% of patients with chronic LBP collect disability payments, compared to only 4.6% of Americans suffering from chronic pain elsewhere in the body [
2]. Many (35%) patients with LBP are referred for expensive imaging studies rather than more cost-effective conservative treatment options first [
4].
2. Demographic Factors Contributing to the Pain Experience
There are many factors in addition to tissue damage that contribute to a patient’s pain experience, which makes the understanding of pain complicated. Researchers have found similar correlations between job position, socioeconomic status, and education and chronic pain. Fliesser et al. [
5] conducted a longitudinal study that followed 352 individuals in order to identify factors that predicted chronic LBP. They found that a person’s employment and socioeconomic status was highly associated with the development of LBP [
5]. A study by Tong Yu et al. [
6] found similar correlations in a sample of 18,316 people from the 2008 Chinese Suboptimal Health Study. They found that individuals with a lower socioeconomic status and level of education were more likely to have chronic pain when compared to individuals with higher levels of education and income.
In the United States, the National Center of Health Statistics (NCHS) conducted the cross-sectional National Health Interview Survey (NHIS) to help find factors that may contribute to both chronic pain and high-impact chronic pain [
1]. Unlike chronic pain, high-impact chronic pain is associated with significant decreases in a person’s ability to carry out activities of daily living, such as work, recreational, social, and self-care activities such as bathing, cleaning, dressing, and cooking [
1]. High-impact chronic pain, in one study, was strongly correlated with individuals who previously worked but were not currently employed, individuals with low socioeconomic status, and rural residents [
1]. Similar to other studies, the authors reported that holding at least a Bachelor’s degree significantly decreased an individual’s likelihood of having high-impact chronic pain.
The evidence consistently reports socioeconomic status, job position, and education level as major predictors of chronic pain in adults. Results have been replicated throughout a variety of nations with different cultural backgrounds. It is important to account for this when exploring the causes of pain, because these correlations can be directly tied to depression which is another major factor surrounding the chronic pain experience [
7].
3. Depression and Its Contribution to Recovery
Psychological factors can influence the severity of pain felt by a patient, and this can potentially impact the prognosis of these patients as well as their behaviors. Of those who have LBP living in America, one in three are also depressed, as opposed to only one in five among the pain free population [
2].
Analysis of a prospective cohort of patients by George et al. [
8] studied a population of 111 individuals undergoing outpatient physical therapy for LBP using the STarT Back Screening Tool (SBT). The SBT is a 9-item prognostic tool that helps to determine the likelihood of recovery for individuals with LBP, with a score of over 4 being considered “high-risk” of poor recovery. They found that a co-occurrence of depression with high pain intensity and “high-risk” SBT scores was a predictive factor for patients not recovering from their pain within 6 months of outpatient physical therapy [
8].
Several other studies have found correlations between depression and behavioral changes leading to heightened kinesiophobia, fear-avoidance behaviors, anxiety, and LBP. A cross-sectional study by Antunes et al. [
9] in 2013 used the Tampa Scale of Kinesphobia (TSK), McGill Questionnaire (for pain), Medical Outcome Study 36 (for quality of life), and the Beck Depression Inventory to assess 193 individuals with LBP. They found that the 32.1% of individuals with depression also had higher perceived pain levels as well as higher fear of movement (kinesiophobia), and decreased quality of life when compared to the other individuals with LBP that did not suffer from depression [
9]. Another study by Trocoli et al. [
10] used the same Beck Depression inventory and TSK when assessing organic (musculoskeletal cause), non-organic (no musculoskeletal cause), and amplified organic LBP and found that across groups, there was little variation in scores on the different outcome measures. Over 66% of individuals fell under the category of “mild depression”, with an additional 33.8% falling under both moderate and severe [
10]. They also found that each group had a moderate amount of kinesiophobia, with no significant difference between groups. Several of these findings were again replicated by Oliveria et al. [
11]. Using the Hospital Anxiety and Depression Scale (HADS), Brief Pain Inventory (BPI), and the Shortened Treatment Outcomes in Pain Survey (S-TOPS), they screened patients at study initiation and followed up one year later. They found that individuals with heightened levels of depression and anxiety had significantly higher levels of pain interference at the one-year follow-up when compared to individuals with lower levels of these two behaviors [
11]. Higher levels of pain interference influence the rate of recovery in patients with LBP.
These findings confirm that depression can have an impact on the outcomes of patients and influence perceptions of pain and disability regardless of the type of LBP. Characteristics associated with depression are found in varying degrees within this population, manifesting as fear-avoidance behaviors and kinesiophobia, which can affect recovery and influence prognosis.
4. Anxiety, Depression, and Its Ties to Central Sensitization
Anxiety and its correlation with chronic pain has been studied extensively. There is preliminary evidence to suggest that in many cases, the development of an anxiety disorder precedes the development of chronic pain symptoms [
12]. Co-occurrence of anxiety is associated with more negative outcomes for pain patients, and highly anxious patients are more likely to develop central sensitization [
13]. In another study by Neblett et al. [
14], researchers looked at the correlation between major depressive disorders, pain-related anxiety, a population of 763 patients diagnosed with LBP and central sensitization syndromes (CSS). Briefly, CSS is a condition whereby patients have a heightened pain perception that is thought to occur from a processing dysfunction of the central nervous system. In the aforementioned study, the authors reported a strong association between heightened severity of CSS and major depressive disorders as well as anxiety, perceived disability, sleep disturbances, and pain intensity [
14]. These findings confirm that anxiety, depression, and similar behaviors contribute to the chronic pain experience, as well as the perception of pain with central sensitization. Heightened central sensitivity may increase kinesiophobia, fear-avoidance, and pain catastrophizing behaviors, further stunting recovery due to the complexity of central sensitization and the difficulty in shaping a treatment plan that can adequately address it [
15]. As most of the studies assessing the relation between mental health features and pain are cross-sectional, we may only speculate that this is a bidirectional relationship—mental health influences the pain perception, but pain also influences mental health.
5. Personality and Pain Correlation
Personality is a manner by which to describe how individuals perceive, relate, and think about the environment. Furthermore, this construct may be influenced by traumatic effects [
16], which may include depression or anxiety. Anxiety can be defined as state anxiety or trait anxiety. State anxiety is generally temporary and may be reflected by thoughts or feelings at a particular moment in time. However, trait anxiety is a more enduring characteristic that is present over a period of time and reflects a long-standing pattern or behavior. Several different behaviors and traits can alter the perception of pain, disability, and quality of life. Several of these behaviors can be found in various personality types and influence the development of chronic pain.
George and Beneciuk [
8] identified a co-occurrence of depression with high pain intensity that was a predictive factor in patients not recovering from their pain within 6 months. The authors sought to better understand psychosocial factors, psychological constructs, pain-related fears, and self-reporting recovery as variables in understanding of depression as it relates to pain and outcomes. The authors’ findings suggest that patients who are at high risk related to multidimensional psychosocial factors in conjunction with higher depressive symptoms and pain intensity are predictive of not recovering at the six-month mark. Of note, only 14 of the 111 participants recovered [
8]. The authors attributed their recovery to the lack of pain intensity. A study by Sliwka et al. [
17] corroborated these findings. Sliwka et al. [
17] also found that mental disorders were more prevalent in those with chronic disease. The authors suggest that this increase in prevalence related to chronically ill patients is a possible result of patients’ own psychological challenges. Overall, Bergstrom et al. [
18] summed up the notion that treatment of LBP is multifactorial and influenced by time of intervention, duration of symptoms, low levels of physical activity, psychological challenges and poor self-rated health [
18]. There is even preliminary evidence to suggest that in many cases, the development of an anxiety disorder precedes the development of chronic pain symptoms across multiple studies [
12]. It is known that chronic pain is understood as a lack of an adaptive response to persistent stimuli, which wanes on patients’ physical and emotional health. In a healthy study of 85,088 participants, those suffering from neck or back pain had a higher 12-month incidence of panic disorder, agoraphobia, social anxiety disorder, generalized anxiety disorder and even post-traumatic stress disorder (PTSD) [
19], lending to the notion that there is a possibility that persistent pain draws on patient’s mental health over time. Asmundson and Katz [
12] reported that, as pain intensity decreases, emotional numbness increases. This suggests that emotional numbness may be correlated with developing a persistent pain disability. In the study by Asmundson and Katz [
12], it was noted that PTSD and chronic musculoskeletal pain share multiple characteristics [
12]. Somatic hypervigilance, attention to threatening stimulus, heightened startle reaction, emotional numbness, avoidance, and dysregulation in the stress response are seen in response to PTSD and chronic musculoskeletal pain [
12]. This highlights the fact that chronic musculoskeletal pain is associated with hyperarousal/a highly anxious state. The literature consistently reports that dysregulation of the autonomic nervous system leads to hyperalgesia through this systematic response of cognitive, behavioral, and physiological numbness resulting from increased anxiety.
Anxiety is also associated with negative outcomes for patients with pain and highly anxious patients are more likely to develop central sensitization [
13]. This study essentially utilized a four-trait sensory profile used to understand nonspecific LBP patients, classifying them as high anxious, defensive high anxious, low anxious and repressor. As previously mentioned by Clark et al. [
13] in 2019, this cross-sectional observational study used eight physiotherapy and pain clinics to recruit 165 patients who had been identified by their physiotherapist as having nonspecific LBP [
13]. Participants were split up into two groups: participants who scored above 40 points (
n = 129) or below (
n = 36) 40 points on the Central Sensitization Inventory. It was noted that those who scored the highest (>40) had elevated results related to sensory sensitivity and a sensation avoidance profile. Breaking down all of the participants who had nonspecific LBP and central sensitization, analysis found that 75 participants (45%) were defensive high anxious [
13]. It was suggested that those who score high on the Central Sensitization Inventory are correlated with having a higher chance of experiencing nonspecific LBP and central sensitization due to a possible low neurological threshold related to sensory stimulation. This suggests that personality type may influence a patient’s response to pain [
13].
Yang and Bateer [
20] recruited 59 university students to receive painful stimuli in the dorsum of the left hand via two electrodes and looked at self-reported measures (Fear of Pain Questionnaire, Anxiety Sensitivity Index, STAI-T) in relation to their pain experience [
20]. The researchers concluded that high fear of pain groups reported higher pain intensity in conjunction with higher anxiety levels when compared to the low fear of pain groups. The authors found that threat appraisal of pain played an important role in the association between pain-related fear and pain perceptual biases [
20].
Validated outcome measures with psychosocial components, as well as personality inventories, have already been shown to have predictive value when it comes to prognosis in patients with chronic pain. For instance, the Temperament and Character Inventory (TCI-R) identifies traits such as harm avoidance and self-directedness. Patients who scored high on harm avoidance and low on self-directedness were more likely to have pain persist beyond the acute phase and become chronic [
21]. Additionally, the Minnesota Multiphasic Personality Inventory (MMPI) has also been studied extensively in multiple populations [
22,
23,
24]. Riley et al. [
24] sought to evaluate the clinical utility of the MMPI. They were able to replicate cluster profile groups in patients with chronic back pain. However, Pheasant et al. [
23] evaluated the MMPI as a predictor of outcome for individuals that undergo low back surgery and were not able to identify profiles that were predictive of outcomes. This suggests that the clinical utility for individuals suffering from low back pain be limited particularly when evaluating specific chronic conditions, particularly those that are considering surgery. A study by Bradley et al. [
22] suggested that MMPI profiles may be one of many factors that can contribute to profile subgroups. The authors report pain-related behavioral attributes that are unique with different subgroups which may be associated with different subgroups.
6. Eysenck’s Personality Inventory
While there are many personality assessments available, Eysenck’s Personality Inventory (EPI) has the ability to relate personality traits and traumatic accidents. Therefore, it is an ideal tool to understand personality traits in relation to LBP. Uses for the EPI include industrial applications (such as market research), educational guidance and counseling, clinical diagnosis, and experimental applications.
Studies examining Eysenck’s Personality Inventory (EPI) and the Neo-Personality Inventory found a relationship between neuroticism and pain, especially in the adjustment to pain symptoms of those with chronic pain [
21]. The authors described neurotics as those with tendencies towards being anxious, irritable and having low self-esteem [
21]. These characteristics are demonstrative of emotional reactivity and vulnerability to stress. This lends our ears to the fact that some research has suggested that neuroticism is likely related to chronic pain [
21]. There have been some confounding variables that have made it difficult to draw solid conclusions on these findings that Naylor et al. [
21] described. Anxiety and depression are very difficult variables to control, and thus make it difficult to conclusively state that neuroticism is linked to chronic pain. It has been suggested that the vulnerability of one’s personality might allow a person to feel threatened by pain and in the end try and avoid any type of pain [
21].
Understanding the premise of pain and the multitude of contributing factors is not an easy task as described in the above literature. Although Eysenck’s Personality Inventory is an older personality questionnaire, it provides a succinct understanding of one’s personality inventory.
The EPI was proposed by Eysenck and Eysenck as an update to the Maudsley Personality Instrument (MPI). A noted difference between the EPI and the MPI is that the EPI incorporates a “Lie Scale”. This “Lie Scale” was included in the EPI to understand the test-taking behavior of an individual, i.e., “faking good” or how “socially desirable” an answer may be perceived [
25]. The purpose of the EPI was to identify extraversion (e.g., seeking external gratification outside oneself) and neuroticism (disposition to experience negative affects), as two key primary personalities in the grand construct of personality [
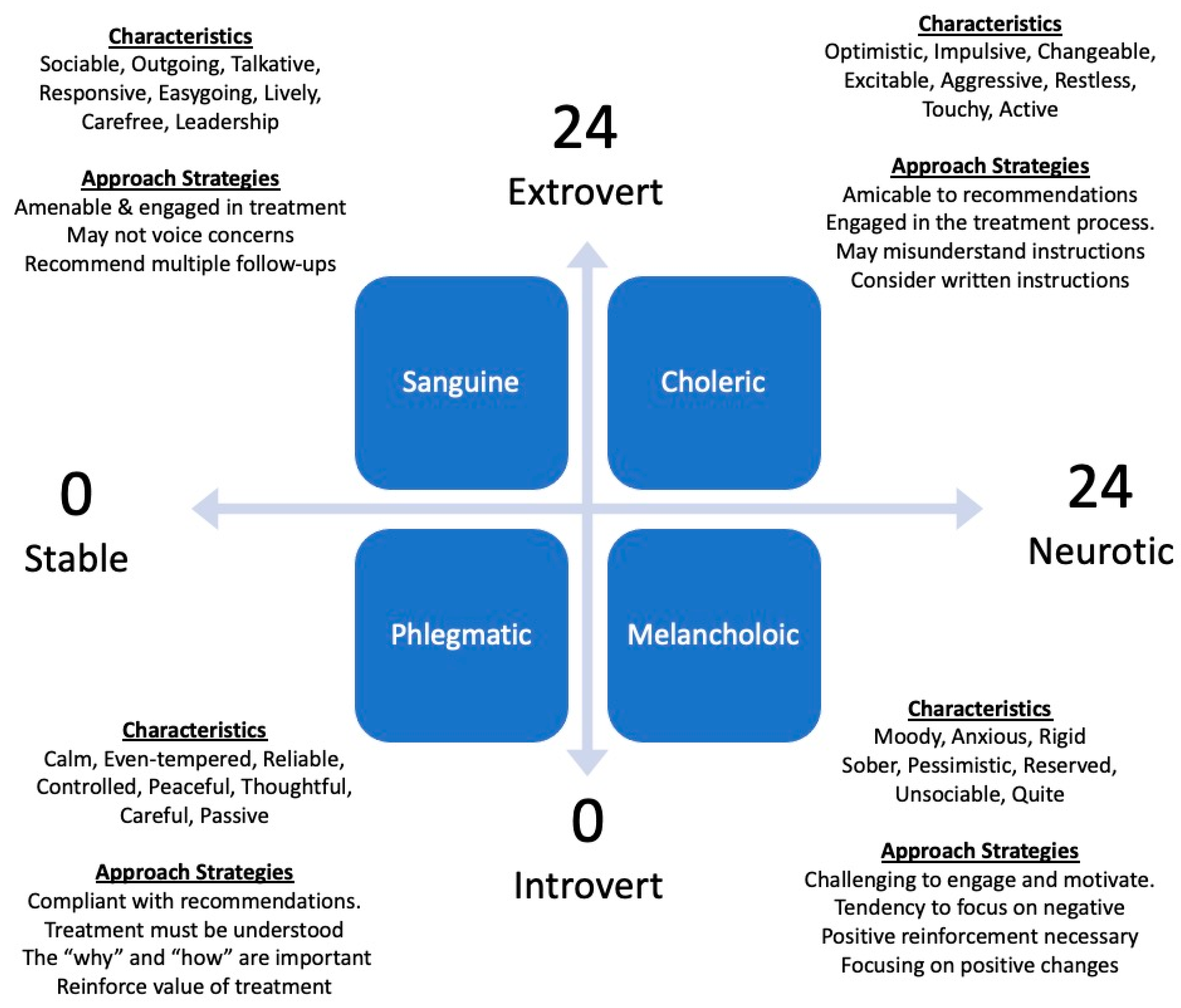
26]. The EPI is a 57-item dichotomous questionnaire, where 24 questions are related to neuroticism, 24 questions are related to extraversion, and nine questions are related to lying. Envision four quadrants in the form of a graph, with the origin being 12,12 (
Figure 1). On the Y-axis, 24 is extrovert and 0 is introvert. On the X-axis, 24 is neurotic and 0 is stable.
In the first quadrant, or the 12,12 to 24,24 range, lies the choleric personality. Choleric characteristics include, but are not limited to; optimistic, impulsive, and excitable. In quadrant II, or the 12,12 to 0,24 range, lies the sanguine category. The sanguine characteristics include, but are not limited to; sociable, outgoing, easygoing, and leadership. Quadrant III, or the plots 12,12 to 0,0, incorporates the phlegmatic personality. The phlegmatic characteristics include, but are not limited to calm, passive, peaceful, thoughtful, and reliable. Quadrant IV, or the plots of 12,12 to 24,0, incorporates the melancholic characteristic. The melancholic characteristics include, but are not limited to; moody, unsociable, pessimistic, and anxious.
7. Eysenck Personality Inventory Reliability & Validity
The reliability of the EPI ranges from 0.81 to 0.97 for test–retest reliability and 0.74 to 0.91 for split-half reliability [
26]. A study by Gabrys [
28] in 1982 conducted an in-depth study of the EPI with 274 females and 303 males [
28]. These participants were out-patients at a mental health center, and this test was conducted ultimately to understand the EPI as a research tool for psychological outpatients. Measures of extraversion were concluded to be 0.89 for males and 0.91 for females, while measures of neuroticism were 0.92 for males and 0.93 for females. The lie scale correlations between females and males were found to be 0.79 and 0.68, respectively. All statistics above had a
p-value of <0.01. Internal consistency was found to be 0.89 for extraversion, 0.92 for neuroticism, and 0.78 for the lie section. The author also stated that the validity and reliability found with this study was consistent with other published randomized samples during this time, although the author never went into depth about what those published findings were [
28].
Understanding the EPI can pose a challenge. Since its introduction in 1964, it has been updated into short forms, longer forms and tweaked to directly affect certain aspects of personality understanding, but the tool still has a solid foundation. The newer versions, as described by Bodling and Martin [
26], are a result of improving the understanding of certain personal characteristics. For instance, in 1975, the Eysenck Personality Questionnaire was adjusted to assess psychoticism.
8. Eysenck Personality Inventory and Research
A scant amount of research is noted when searching for EPI and LBP. A study by Gilchrist [
29] identified personality traits, utilizing the EPI, in patients with acute LBP, and found that they were similar to those of a control population [
29]. The author was a general practitioner at a health center, where he recruited patients who presented with LBP. The control group had 73 patients (27 in musculoskeletal and 46 in other), while 70 were in the LBP group. The author concluded that there were no significant differences in relation to neuroticism and the lie scale, but there was a notable difference in relation to the extraversion/introversion. The LBP group scored 12.70 (SD: 4.46), whereas the control group had a score of 10.50 (SD: 4.27). The author concluded that this statistical finding could be related to the fact that the more active a person is, the more likely they are to be extroverted. Ultimately, this article found inconclusive evidence of LBP and psychological findings [
29].
Lin et al. [
30] evaluated the correlations between quality of life and psychological factors in patients with chronic neck pain. Using 51 participants for the study, the study started off by completing a number of questionnaires: Chinese Health Questionnaire, Eysenck Personality Inventory, Beck Anxiety Index, SF-36 Taiwan version (for demographics). After completion of these questionnaires, the participants were then evaluated and treated for their chronic neck pain. For scores relating to the neuroticism domain and the extraversion domain, the average scores were 5.7 ± 2.7 and 7.1 ± 2.9, respectively. To break this down further for the neuroticism domain, 11.8% scored 0–2, 31.4% scored 3–5, 37.3% scored 6–8, 19.6% scored 9–11 and nobody scored 12–13. As it relates to the extraversion domain, 3.9% scored 0–2, 27.5% scored 3–5, 31.4% of patients scored both 6–8 and 9–11, and 5.9% scored 12–13. It was then concluded at the end of the study that mental health has a strong association with several psychological factors that were pronounced by the psychological measures in this study, such as the Eysenck Personality Questionnaire [
30]. The study concluded that psychiatric distress and neurotic personality are important factors associated with chronic pain [
30].
Personality has been described as a way of perceiving, relating and thinking about the environment, and may be influenced by traumatic effects [
16]. While the authors look at Eysenck’s personality dimensions and their relationships between breast cancer survivors and the general population, it has been understood that neuroticism and psychoticism are applicable with regard to depression, quality of life and fatigability, which are key aspects of LBP. The conclusion from this case–control study states that there were lower scores related to extraversion and higher scores related to neuroticism. The survivor group, when it came to extraversion, was 49.23 ± 9.35, and the control was 50.46 ± 9.04. The survivor group, when it came to neuroticism, was 46.73 ± 9.57, and the control was 43.36 ± 10.68 [
16]. It is also important to note that the other personality variables included based on the Eysenck Personality Inventory-Revised were psychoticism and a sincerity/compliance component. Both sincerity/compliance and psychoticism were scored higher in the survivor group. Psychoticism was the only statistical difference concluded out of the four psychological factors [
16]. This article sheds some interesting light on persons diagnosed with cancer and the possibility of subsequent psychological strategies that are employed as a result of sheer will to improve survivability and quality of life. The inclusion of the study is intended to better understand possible psychological traits for those looking to increase quality of life and return to prior level of function.
9. Conclusions and Implications for Treatment
LBP is a complicated multifactorial disorder with overlapping influences arising from various environmental, psychosocial, and biological factors. As discussed, the economic toll of LBP contributes to billions of dollars in healthcare costs, and increased likelihood of future disability, leading to the need for government support [
8,
11,
31,
32]. Chronic LBP leads to increased levels of disability limiting individuals’ ability to perform activities of daily living needed. Several studies have found correlations between job position, socioeconomic status, education level, and cLBP [
8,
11,
31,
32].
Numerous studies have used different outcome measures such as the TSK, RMQ, FABQ, SBT, NPRS, McGill Pain questionnaire, Beck Depression questionnaire, and the PCS to measure varying behavioral characteristics and traits in LBP patients to determine the effects depression had on overall recovery and its association with other relevant characteristics. Patients with higher levels of depression and anxiety tend to have higher levels of fear-avoidance, pain catastrophizing, perceived pain, and disability than other individuals with lower levels of depression on various questionnaires [
10,
14,
28,
33,
34]. All of these listed traits and behaviors have direct connections to different personalities that have been studied in the field of psychology for several decades, but currently there are very few studies that look at ties of personality to these different outcome measures and behaviors.
There are several personality inventories currently used in the field of psychology but, several have costs associated with training and access to their forms. For this reason, the EPI may be a better choice for clinicians due to its accessibility, reliability, and consistency. The EPI has been used in a wide range of research studies, and is an easily accessible questionnaire. One of the benefits of this particular measure is that it helps to separate individuals into different categories based on their responses to questions that have been rigorously studied within different populations. Some previous medical studies have used it to help to assess the correlation between neck pain and neuroticism, while others have used it to look at cancer patients and the correlation between pain and neuroticism, showing its versatility [
16]. Clinicians may consider utilizing the results of the EPI to assist with clinical decision making.
Choleric characteristics include being optimistic, impulsive, and excitable. These patients are generally amicable to recommendations and are engaged in the treatment process. However, due to their impulsive tendencies, they may initiate recommendations before they completely understand the instructions, which may lead to errors or misunderstandings. Clinicians should consider written instructions and multiple follow ups to ensure they are adhering recommendations properly.
The sanguine characteristics include being sociable, outgoing, easygoing, and demonstrating leadership qualities. Patients with a sanguine personality are amenable and engaged in their treatment. However, they tend to be easygoing or agreeable, and therefore may not voice concerns or objections. Clinicians are encouraged to follow up with patients to ensure that their concerns have been identified and the treatment plan is addressing those concerns.
The phlegmatic characteristics include being calm, passive, peaceful, thoughtful, and reliable. These patients have a tendency to follow instructions and are compliant with recommendations. However, they also tend to be thoughtful and therefore, treatment approaches must be understood by the patient. The “why” and “how” of treatment approaches become particularly important for patients classified with a phlegmatic type of personality. Clinicians are encouraged to spend more time with these patients to ensure that they understand the value and purpose of the recommended treatment approach.
The melancholic characteristics include being moody, unsociable, pessimistic, and anxious. These patients tend to be more challenging to engage and motivate. They have a tendency to focus on negative characteristics of treatment and their condition. Therefore, clinicians are encouraged to provide positive reinforcement and constantly point out improved changes in outcomes. Focusing on positive changes in the condition will have significant value for these patients.
The 57 questions in the EPI are interlaced with the neurotic, extroversion and lie questions [
26]. The test taker starts with a score of 0, and if they answer the question correctly, points add up. This is the same philosophy as with the EPI. As stated above, certain questions relate to the three question categories. So, if a participant was not answering questions correctly, the participant would score a 0.0 and be categorized as phlegmatic. The scoring only relates to the neurotic and extroversion questions, whereas the 9 lie questions (9 + 48 = 57) are used to see how honest a participant’s responses are.
Using the EPI, several different character categories can be examined, including: extroversion, introversion, neuroticism, and stability. Each of these has associated trait quadrants ranging from phlegmatic to choleric, melancholic, and sanguine that each include several more descriptors linked to the questions given to the participant. Ultimately, treatment of chronic pain can be a challenge. In the case of persistent and apparently unexplained pain, patients should be psychologically assessed in a multidisciplinary approach.